Abstract
Purpose
The purpose of this study was to evaluate a novel online education and coaching program to promote self-care among patients with heart failure. In this program, education and coaching content is automatically tailored to the knowledge and behavior of the patient.
Patients and methods
The evaluation of the program took place within the scope of the HeartCycle study. This multi-center, observational study examined the ability of a third generation telehealth system to enhance the management of patients recently (<60 days) admitted to the hospital for worsening heart failure or outpatients with persistent New York Heart Association (NYHA) Functional Classification III/IV symptoms. Self-reported self-care behavior was assessed at baseline and study-end by means of the 9-item European Heart Failure Self-care Behavior scale. Adherence to daily weighing, blood pressure monitoring, and reporting of symptoms was determined by analyzing the system’s database.
Results
Of 123 patients enrolled, the mean age was 66±12 years, 66% were in NYHA III and 79% were men. Self-reported self-care behavior scores (n=101) improved during the study for daily weighing, low-salt diet, physical activity (P<0.001), and fluid restriction (P<0.05). Average adherence (n=120) to measuring weight was 90%±16%, to measuring blood pressure was 89%±17% and to symptom reporting was 66%±32%.
Conclusion
Self-reported self-care behavior scores improved significantly during the period of observation, and the objective evidence of adherence to daily weight and blood pressure measurements was high and remained stable over time. However, adherence to daily reporting of symptoms was lower and declined in the long-term.
Keywords: lifestyle, patient adherence, telehealth, e-coaching
Introduction
Heart failure (HF) is highly prevalent and linked to increased incidence of hospital readmissions, poor quality of life, and mortality.1 Management of HF is challenging and resource intensive. Encouraging patients and their caregivers to play a more active role in the management of the condition may be a cost-effective solution.2 There is growing support for the concept and value of key self-care behaviors in HF, namely taking medication as prescribed, engaging in physical activity and exercise, monitoring signs and symptoms, and, where appropriate, following a low-salt diet and restricting fluid intake.1 Effective self-care is associated with lower readmission and mortality rates.3 It follows therefore that the promotion of self-care behaviors should benefit patients and health care systems alike.
To promote active participation in self-care management, patients and their caregivers should be provided with education on HF and ways to manage their condition themselves.4 Education can be delivered in several settings: during the hospital stay, in outpatient clinics, in primary care, or at home. Usually, this is carried out in face-to-face sessions by health care professionals supported by leaflets or digital resources (eg, CD-ROM,5 websites,6 telehealth systems,7 and tablet computers8).
Nevertheless adherence to self-care behaviors in HF is low.9,10 There are several factors that may account for this. First, despite current guidelines, hospital/service provision of training and staff for HF education is insufficient to meet demands.11–13 Second, many patients with HF may have impaired cognitive function.1,14,15 This makes learning new self-care skills problematic.16 Third, some patients with HF are clinically depressed or experience depressive symptoms17 that can undermine their motivation and ability to adopt new self-care routines.1 Fourth, knowledge itself may not provide enough impetus and support to negotiate the considerable challenges of initiating and maintaining health behavior change.18,19
The aim of the HeartCycle project funded by the European Commission Seventh Framework program was to examine how telehealth systems can be employed to increase adherence to self-care behaviors in HF. The first stage of the HeartCycle project surveyed the provision of support for self-care among patients with HF. This revealed that, although education is often provided, there is little follow-up to support implementation of self-care skills. The main thrust of tele-health systems has been the monitoring of vital signs rather than patient motivation. Although some systems provided education,20 no system incorporated a coaching program to support behavior change actively. Counseling of patients via telephone increases adherence but is time-consuming and may not be cost effective.21–23
With the aim of producing a less resource intensive approach, the HeartCycle project developed an innovative automated education and coaching (E&C) program integrated within a telehealth system. The rationale behind the program was to tailor the provision of information to the needs of the patient and offer an interactive coaching program to support them in the choice, adoption and maintenance of self-care behavior, and freeing the health care professional to deal with more complex issues arising from HF.
In this paper, we report the results of the component dealing with adherence to self-care behaviors and symptom reporting among HF patients using the HeartCycle E&C program in a multi-center observational study.
Patients and methods
Program summary
A detailed description of the E&C program has been published previously.24 Briefly, based on the 2008 guidelines for the diagnosis and treatment of HF from the European Society of Cardiology,25 we chose to offer education and coaching for daily monitoring of signs, physical activity, fluid restriction, low-salt diet, and medication intake. Other topics were addressed by education only (eg, alcohol consumption) or were left out of the program (eg, sexual activity and prognosis).
The program was offered to the patients via the Motiva Telehealth System (Philips, Böblingen, Germany). This system enables patients to measure vital signs (weight, blood pressure, heart rate), to answer symptoms questions, and to view trend-charts of vital signs and educational videos on their TV. Via a secure Internet connection, data are made available to the HF nurses, who assisted by decision support software, may adapt the care plan or call the patient.
The program’s behavior change model was based on the Heart Manual, a well-established, face-to-face, home-based cardiac rehabilitation approach.26,27 In this model, education and coaching are tailored to the knowledge and behavior of the individual patient. Coaching is offered for the self-care behaviors the patient is not engaged in, and education is provided when the patient has little knowledge of these behaviors. Coaching starts with assessing the patient’s readiness for change by letting the patient express how important self-care behaviors are, and how confident he or she is to engage in these behaviors. Patients are then guided through a goal-setting process that they conduct at their own pace through the support of the system. To raise commitment, patients set their own goals and make their own action plans. They report their progress in an electronic diary, allowing the system to provide appropriate weekly feedback. Only when patients repeatedly fail in adopting self-care behaviors do HF nurses intervene to offer help.
Coaching for daily monitoring of signs and symptoms was further tailored to the characteristics of these self-care behaviors. In particular, assessing the patient’s readiness for change was deemed not necessary since, based on previous experience with the Motiva system, adoption of these daily tasks was expected to be relatively easy. Furthermore, the goals of these behaviors were predefined: the patients were asked to measure weight and blood pressure and to answer a short questionnaire on breathlessness and edema every day. Finally, the patients did not need to self-report their progress on these behaviors in an electronic diary, since signs and symptoms data were stored automatically in the telehealth system.
Eligibility and study design
The E&C program was evaluated within the scope of the HeartCycle study that took place at three hospitals in the United Kingdom, Germany, and Spain. The aim of this multi-center, observational study was to investigate whether the management of patients with HF can be enhanced by a third generation telehealth system. Target doses of medicines were based on European Society of Cardiology guidelines, modified for the individual patient by an experienced clinician if necessary, after taking into account blood pressure, serum potassium, and renal function. Details of the phases of the study have been published elsewhere24 but are not relevant to this report on self-care adherence.
The inclusion and exclusion criteria are shown in Table 1. Patients had been recently (<60 days) admitted for HF or were outpatients with persistent New York Heart Association (NYHA) III/IV symptoms. We did not formally screen for depression or cognitive dysfunction but as patients had to consent to participate in a relatively complex clinical study, patients with marked depression or obvious cognitive dysfunction will have been excluded. Moreover, patients were excluded from the study if in the investigators’ opinion, they were unable to operate or comply with the telehealth system.
Table 1.
Inclusion and exclusion criteria for the HeartCycle study
| Inclusion criteria |
| • A clinical diagnosis of heart failure |
| ο Cause of heart failure may be for any reason other than those that are rapidly reversible (see exclusion criteria) |
| ο May include patients with and without a low left ventricular ejection fraction or with valve disease |
| • Requiring treatment with at least 40 mg/day of furosemide or equivalent (1 mg of bumetanide or 10 mg of torasemide) |
| • Evidence of advanced or unstable disease |
| ο Admission to hospital for or complicated by heart failure currently or within the previous 60 days |
| ο Or outpatients with persistent NYHA III/IV symptoms |
| • An elevated NT-proBNP value (within the 3 months prior to enrollment) |
| ο ≥1,000 pg/mL if in sinus rhythm, including atrio-biventricular pacing |
| ο ≥2,000 pg/mL if not in sinus rhythm |
| Exclusion criteria |
| • Unwilling to comply with the protocol. Patients should be willing and able to make daily measurements at home throughout Phase II |
| • Rapidly reversible causes of heart failure such as severe anemia (defined as the need for a blood transfusion), thyrotoxicosis, admission with rapid (>120 bpm) atrial fibrillation with good ventricular function |
| • Inability, in the investigators’ opinion, to operate or comply with the telehealth system, even with available support from carers and health volunteers if available |
| • Patients who are unable to communicate directly or indirectly in the local language (English in the United Kingdom, German in Germany, and Spanish in Spain) cannot participate |
Abbreviations: NYHA, New York Heart Association; NT-proBNP, N-terminal pro b-type natriuretic peptide.
The protocol was reviewed and approved by the ethics committee of each participating center. All patients provided written voluntary informed consent.
Data collection, instruments
Self-care behavior was measured at baseline and study end with the 9-item European Heart Failure Self-care Behavior Scale (EHFScB-9), which is a reliable and valid scale to measure self-care behavior.28,29 The items are rated on a 5-point scale between 1 (“I completely agree”) and 5 (“I completely disagree”).
Adherence to the three daily tasks (measuring weight, measuring blood pressure, and reporting of breathlessness, and edema) was determined by analyzing a de-identified copy of the telehealth system database. If patients measured their weight (or blood pressure) more than once per day, only one of these measurements was counted. The symptom questionnaire could be answered only once per day. The official enrollment and closure dates were used to determine the start and end of the patient’s monitoring period.
Statistical methods
The EHFScB-9 scores at baseline and study end were analyzed at an item level using a paired Student’s t-test. For each item, patients who answered “I completely agree” or “I agree” were considered adherent.30
For each daily task, the objectively measured adherence was calculated as follows:
The number of expected data elements has been corrected for death, hospitalization, and other absence from home (eg, holidays). The overall adherence of all patients during the entire study was obtained by dividing the total number of received data elements (of all patients) by the total number of expected data elements (of all patients). For each patient, we calculated the adherence of the entire monitoring period, and per month. In the latter case, for each month, we used the number of received data elements in that month and the number of expected data elements in that month in the above formula.
Matlab 2013a and R version 3.1.2 were used for statistics and making illustrations.
Results
Patients’ characteristics
Of 123 patients enrolled (mean age 66±12 years, 79% men) (Table 2), most (66%) were in NYHA class III, indicating that they had marked limitation of physical activity.
Table 2.
Baseline characteristics of the study population
| Total number of patients =123 | n (%) or mean ± SD |
|---|---|
| Men | 97 (79) |
| Mean age (years) | 66.2±11.8 |
| Age >70 years | 49 (40) |
| BMI (kg/m2) | |
| Underweight <18.5 | 2 (2) |
| Normal 18.5–25.0 | 37 (30) |
| Overweight 25.0–30.0 | 45 (37) |
| Obese ≥30.0 | 39 (32) |
| Cardiovascular history | |
| Myocardial infarction | 58 (47) |
| Revascularization | 52 (42) |
| Valve surgery | 11 (9) |
| Co-morbidities | |
| Cancer | 16 (13) |
| Diabetes | 53 (43) |
| NYHA class and symptoms | |
| NYHA II | 42 (34) |
| NYHA III | 81 (66) |
| Angina | 18 (15) |
| Peripheral edema | 41 (33) |
Note: Values are presented as n (%) or as mean ± SD.
Abbreviations: BMI, body mass index; NYHA, New York Heart Association.
Measured system usage
The patients were enrolled between January 2012 and March 2013. They were asked to use the system until the end of the study (June 30, 2013). Hence, patients enrolled in January 2012 could use the system for 18 months, but those enrolled in March 2013 only for 4 months.
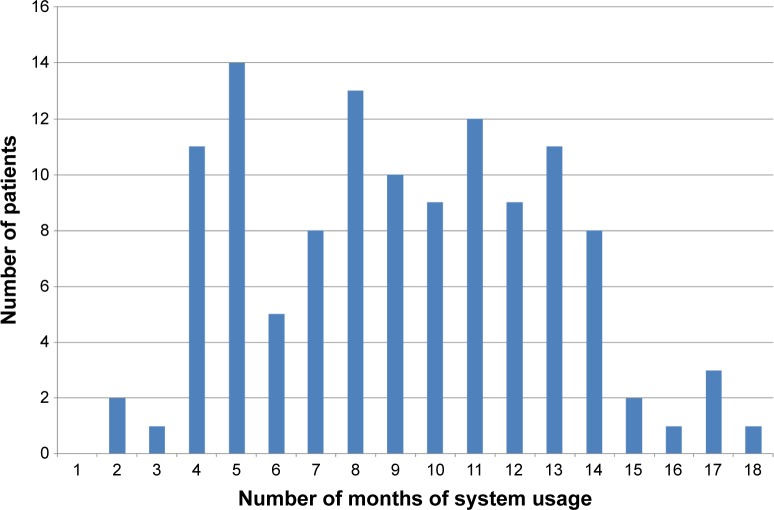
Of the 123 patients enrolled, three did not activate the system. The remaining 120 patients used the system for 9 months on average with a range of 2 to 18 months (Figure 1) with a total system usage of 1,101 patient-months. Ninety-seven patients used the system until the end of the study, and 23 patients discontinued before the end of the study due to death, increasing debility, or loss of interest.
Figure 1.
The number of patients per number of months of system usage.
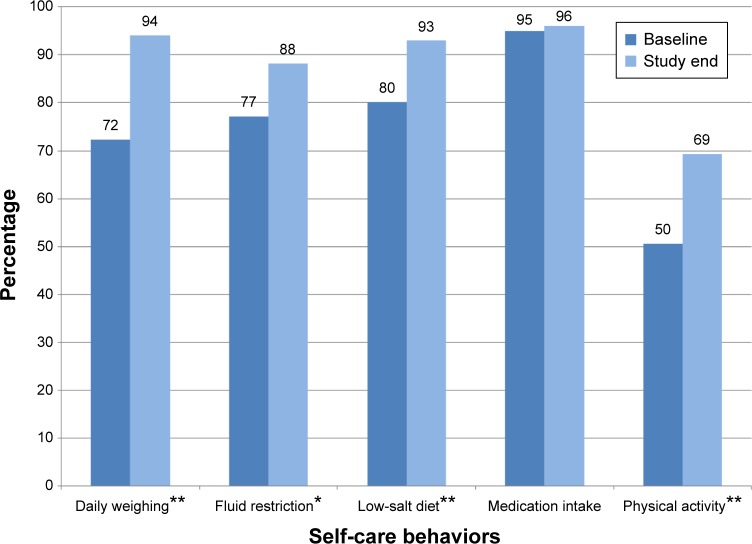
Self-reported self-care behavior at baseline and study end
Data from the 101 patients with paired data from the EHFScB-9 questionnaire at baseline and study end showed improved adherence of all self-care behaviors except for medication intake (Figure 2). The relative increase of adherence was 31% for daily weighing, 14% for fluid restriction, 16% for low-salt diet, and 38% for physical activity but only 1% for medication intake.
Figure 2.
Percentage of adherent patients in the EHFScB-9 self-care behavior scale at baseline and study end (n=101).
Notes: *P<0.05, **P<0.001.
Abbreviation: EHFScB-9, 9-item European Heart Failure Self-care Behavior Scale.
Differences in responses at baseline and study end per individual patient are shown in Table 3. For example, for daily weighing, 30 patients showed an adherence improvement from baseline to study end, the adherence of 61 patients remained the same, five patients showed a decline in adherence, and five patients gave an invalid answer at baseline or study end. All 61 patients who gave the same answer at baseline and study end for daily weighing, were adherent at both moments.
Table 3.
Differences between the answers at baseline and study end for self-care behaviors measured with the EHFScB-9 scale (n=101)
| Self-care behavior | Number of patients showing an improvement | Number of patients remaining the same (remaining adherent) | Number of patients showing a decline | Number of patients with invalid answer(s) |
|---|---|---|---|---|
| Daily weighing | 30 | 61 (61) | 5 | 5 |
| Fluid restriction | 17 | 70 (68) | 10 | 4 |
| Low-salt diet | 25 | 65 (62) | 8 | 3 |
| Medication intake | 4 | 91 (91) | 2 | 4 |
| Physical activity | 44 | 35 (28) | 19 | 3 |
Notes: EHFScB-9 scores range from 1 (“I completely agree”) to 5 (“I completely disagree”). A patient shows an improvement for a behavior if the score at study end is lower than the score at baseline. A patient remains the same for a behavior if the score at study end equals the score at baseline, and remains adherent if the scores for a behavior at study end and at baseline both are 1 (“I completely agree”) or 2 (“I agree”).
Abbreviation: EHFScB-9, 9-item European Heart Failure Self-care Behavior Scale.
Measured adherence to daily tasks
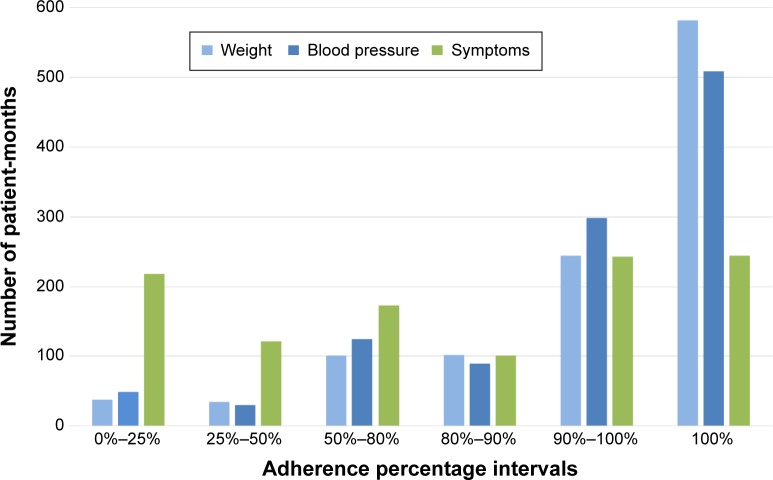
The overall and the average adherence of measuring weight and blood pressure was about 90% (Table 4). For daily reporting of symptoms, the overall and the average adherence was about 67%. The percentage of patients performing the daily task on ≥80% of the expected days was 88% for measuring weight, 85% for measuring blood pressure, and 50% for symptoms reporting.
Table 4.
Objectively measured adherence per daily task (n=120)
| Daily task | Overall adherence percentage | Average adherence percentage (SD) | Percentage of patients performing daily task on ≥80% of expected days |
|---|---|---|---|
| Measure weight | 91 | 90 (16) | 88 |
| Measure blood pressure | 90 | 89 (17) | 85 |
| Report symptoms | 68 | 66 (32) | 50 |
Notes: The overall adherence is the total number of received data elements (of all patients) divided by the total number of expected data elements (of all patients). The average adherence is the average of the 120 individual adherence numbers.
Abbreviation: SD, standard deviation.
For measuring weight, adherence was 100% in 582 (of the 1,101) patient-months and between 90% and 100% in a further 244 patient-months (Figure 3). For symptoms reporting, adherence was 100% in 244 patient-months, but between 0% and 25% in 218 patient-months.
Figure 3.
Number of patient-months per adherence percentage interval (total number of patient-months =1,101).
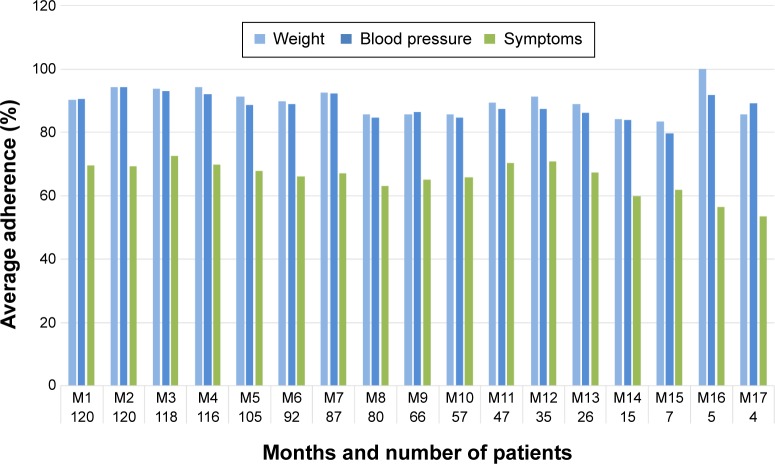
Figure 4 shows the average adherence over time of the three daily tasks. For example, 120 patients used the system for at least 1 month. The average adherence of measuring weight and blood pressure in the first month was 90%. For symptoms reporting the average adherence in the first month was 70%. A total of 92 patients used the system for at least 6 months. The average adherence percentage for measuring weight and blood pressure in month 6 was still about 90% but for symptoms reporting at month 6 this had dropped slightly to 66%.
Figure 4.
Average adherence over time for weight, blood pressure, and symptoms reporting. The numbers at the horizontal axis denote the number of patients who were using the system in that month. Since month M18 had only one patient, this month has been excluded from the figure.
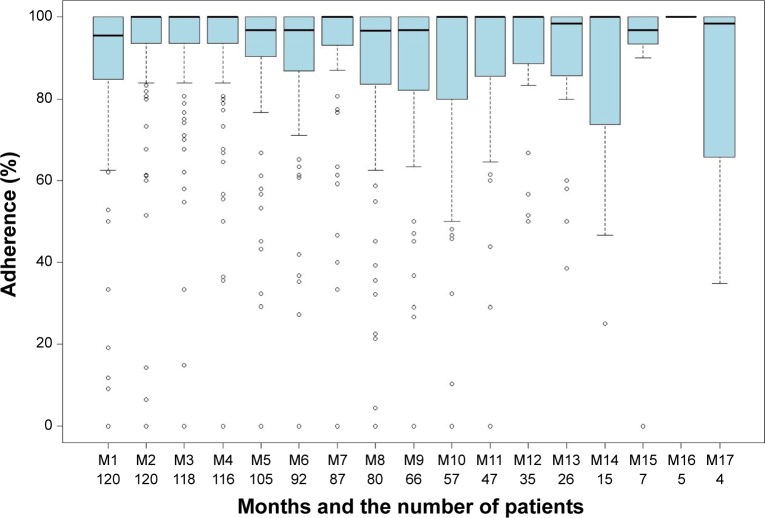
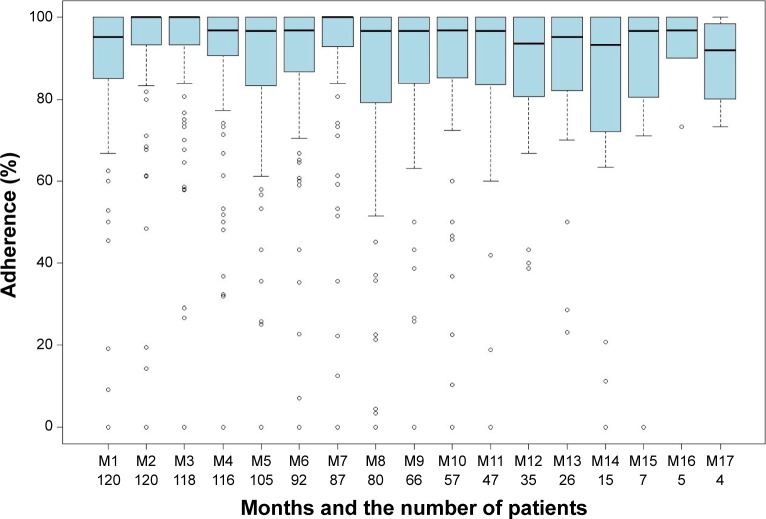
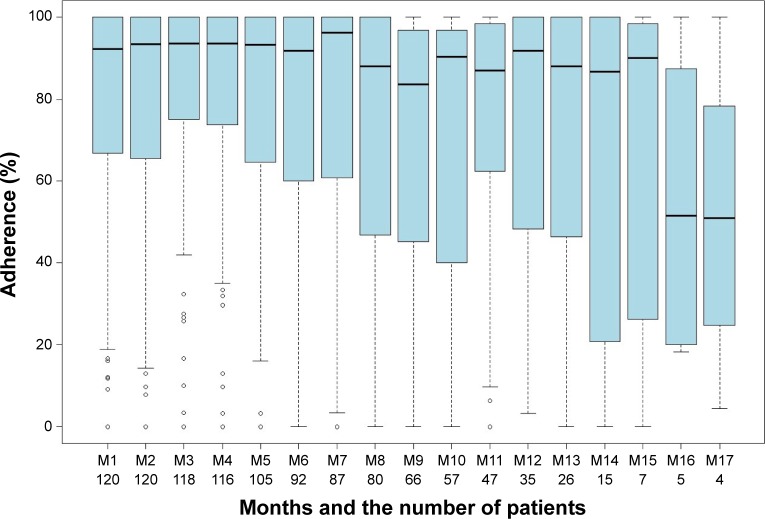
For measuring weight and blood pressure, adherence remained stable over time (Figures 5 and 6; the percentile details can be found in Table S1). For symptoms reporting, adherence was stable for 6 months with a median of about 93%, and then started to decline (Figure 7). After half a year, the variability for symptoms reporting became wider compared to both the variability in the preceding months and the variability for measuring weight and blood pressure.
Figure 5.
Box-and-whisker plot for measuring weight. Vertical axis shows adherence. Horizontal axis shows the months and the number of patients who were using the system in that month. Month M18 has been excluded from the figure since only one patient was using the system for 18 months.
Figure 6.
Box-and-whisker plot for measuring blood pressure. Vertical axis shows adherence. Horizontal axis shows the months and the number of patients who were using the system in that month. Month M18 has been excluded from the figure since only one patient was using the system for 18 months.
Figure 7.
Box-and-whisker plot for symptoms reporting. Vertical axis shows adherence. Horizontal axis shows the months and the number of patients who were using the system in that month. Month M18 has been excluded from the figure since only one patient was using the system for 18 months.
Discussion
For all self-care behaviors except medication intake, self-reported, and self-care behavior scores improved significantly from baseline to study end (n=101). We assume that the automated coaching was the likely mechanism for this improvement; proof of this assumption in a randomized trial is the logical next step. The results are promising, especially when taking into account that most patients already received substantial conventional education preceding enrollment in the HeartCycle study, and that self-reported adherence of daily weighing, fluid restriction, and low-salt diet was already high at baseline (72%, 77%, and 80%, respectively).
Adherence to medication intake was very high in our study. This is in line with other studies that use self-report as a measure of medication adherence. Depending on the way of measurement, adherence levels for medication intake can vary between 10% and 98%.10 More sensitive scales such as ProMAS31 or medication event monitoring systems32 may be used.
The objectively measured adherence of weight and blood pressure measurements is very high. It is encouraging that of the 1,101 patient-months of system usage, about half showed an adherence of 100% for weight and blood pressure monitoring.
Adherence to symptoms monitoring was lower compared to monitoring of weight and blood pressure, and started to decline after half a year. We did not systematically investigate the reasons for this. However, feedback provided by the study nurses revealed that some patients did not see the point in answering the short questionnaire on breathlessness and edema every day, especially when the intensity of their symptoms had not changed. Another reason could be that our program did not emphasize the value of symptoms reporting sufficiently and that patients perceived that there was no benefit in making the effort. When measuring weight or blood pressure, the system gives immediate feedback by providing information that the patient does not know yet. However, when reporting on symptoms, the patient has to enter information that he or she already knows into the system, but does not receive feedback on this. Receiving (personalized) feedback is essential in changing health behavior.33
For daily weighing self-reported adherence at study end (94%) is only slightly higher than the objectively measured adherence. It should be noted that we used a conservative approach to determine the objectively measured adherence. In particular, we used the official enrollment and closure dates to determine the start and end of the monitoring period. However, in practice some patients started a few days later, or stopped a few days earlier. Three of our 123 patients (2.4%) did not activate the system. This is a considerably lower proportion of non-participation than reported in previous studies; for example in the Tele-HF study 14.4% of the patients never used the telemonitoring system.34
In our study, 66% of the patients were in NYHA class III and 34% in NYHA class II. Since daily monitoring of signs and symptoms allows for the early detection of deterioration, it can be expected that with this program patients in NYHA class IV would show similar adherence to signs and symptoms monitoring. For the other self-care behaviors, it can be expected that the effectiveness of our program for class IV patients depends on the behavior. For example, since NYHA class IV patients have severe limitations with physical activity and are mostly bedbound, it can be expected that for these patients it will be difficult to increase their physical activity level.
Only a few studies have used the EHFScB-9 to study the effect of telehealth interventions on self-care behavior.20,35,36 Two of these studies used the Motiva telehealth system offering vital signs monitoring, education, and motivational messages, but without the coaching program as described in this paper. The first study, with 214 patients and a mean follow-up of 288 days, found no differences in self-care behavior between the control group and the intervention group.20 The RECAP study, in which 108 patients used the Motiva system during 42 days, found a significant difference between the EHFScB-9 total score at baseline and after 42 days.35 For the individual items, significant differences were found for daily weighing, fluid restriction, and low-salt diet, but not for medication intake and physical activity. The TEHAF study investigated the effects of a telemonitoring system that offered dialogues and questions with variable emphasis on symptoms, knowledge, and behavior.36 After 12 months, the total score of the intervention group had improved whereas the control group remained at the same level, which was a significant difference.
Several studies have reported on HF signs and symptoms monitoring adherence based on objective data collected by a telehealth system. Unfortunately, these studies use different adherence criteria. The TEMA-HF 1 study only reported overall adherence: 86% for measuring weight and 82% for measuring blood pressure on a daily basis.37 In our study, these were 91% and 90%, respectively.
Most studies report an average adherence to a standard deviation (Table 5).38–42 For example, the TIM-HF study found an average adherence of 90.6% for blood pressure monitoring and 88.0% for symptoms reporting.38 Another approach is to mention the percentage of patients monitoring signs or symptoms at least x% of the time. For example, in the CARME study 52.2% and 44.4% of the patients monitored weight and blood pressure respectively at least 80% of the time.39 In both cases, the HeartCycle results are among the highest adherence percentages of measuring weight and blood pressure.
Table 5.
Studies reporting on HF signs and symptoms monitoring adherence using telehealth system data
| Number of months in study | Average (SD) adherence percentage
|
Percentage of patients monitoring at least ×% of the time
|
||||||
|---|---|---|---|---|---|---|---|---|
| Weight | Blood pressure | Symptoms | × | Weight | Blood pressure | Symptoms | ||
| Signs and symptoms reported separately | ||||||||
| HeartCycle | 9 (average) | 89.7 (16.2) | 88.6 (16.9) | 66.0 (32.0) | 80 | 87.5 | 84.2 | 50.0 |
| Prescher et al38 (TIM-HF) | 22 (average) | – | 90.6 (15.1) | 88.0 (15.6) | – | – | – | – |
| Domingo et al39 (CARME) | 12 | 76.4 (19.6) | 71.8 (22.1) | – | 80 | 52.2 | 44.4 | – |
| Ledwidge et al40 | 5 (average) | 90.6 (13.6) | – | – | 85 | 77.0 | – | – |
| Lyngå et al41 (WISH) | 12 | 75 | – | – | – | – | – | – |
| de Lusignan et al42 | 12 | 73.7 (19.9) | 89.0 (6.7) | – | – | – | – | – |
| Signs and symptoms reported together | ||||||||
| Prescher et al38 (TIM-HF) | 22 (average) | 88.9 (21.5) [P] and 81.8 (22.8) [A] | 80 | 87.3 [P] and 85.1 [A] | ||||
| Seto et al43 | 6 | 79* | 80 | 66 | ||||
| Chaudhry et al34 (Tele-HF) | 6 | – | 43** | 90.2 (week 1) to 55.1 (week 26) | ||||
| Cleland et al44 (TEN-HMS) | 16 (median) | – | 80 | 81 [P] and 55 [A] | ||||
Notes: [P] means partial adherence (ie, at least one measurement done), [A] means absolute adherence (ie, all measurements done). The percentage 79* has been derived from the sentence “Patients completed their required measurements on average between 5 and 6 days per week”.43 The value 43** is based on at least three calls a week (a cutoff point representing approximately half the expected usage).34
Abbreviations: HF, heart failure; SD, standard deviation.
Four studies report on the combination of signs and symptoms monitoring.34,38,43,44 In the TEN-HMS study, where patients were asked to measure weight and blood pressure twice per day, 81% of the patients using the telehealth system had >80% adherence to at least one daily measurement (weight or blood pressure), and 55% had >80% adherence to twice daily measurements.44 Worth mentioning is that in the Tele-HF study, by week 26 only 55% of the patients were still using the system at least three times per week (ie, 43% of the time).34
The HeartCycle program is characterized by the fact that it provides automated coaching in the home context. Patients receive not only education about self-care behaviors, but also explicit support in adopting these behaviors. Furthermore, the HeartCycle program takes into account the dynamics of health behavior change by specifically addressing relapse. Patients who have relapsed are offered the opportunity to do the coaching program again.
So far, remarkably few programs offering automated coaching of HF self-care behaviors have been developed. We believe only one other study (CHF-CePPORT) designs and evaluates an e-platform for behavioral counseling and education to facilitate long-term adherence to self-care among patients with HF.45 Similar to our program, it is based on motivational interviewing and cognitive-behavioral therapy.
Study limitations
This study has several limitations. HeartCycle was primarily designed to develop a novel telehealth system in collaboration with patients and a multi-disciplinary team of engineers and clinicians rather than to run a large randomized controlled trial. Development and evaluation of the education and coaching program was not the only objective of the study but this was also considered an iterative learning process followed by a pilot concept observational study that did not have a control group. Ideally, a control group receiving usual education on self-care should be compared with a group receiving only online education, and a group receiving both online education and coaching. The sample size for the HeartCycle study was calculated based on the number of patients required for one of the study phases.24 Using three groups would require additional participants, which was beyond the available budget.
Second, this study did not assess whether the observed improvement in self-care adherence translated into improved outcome. This would require a larger randomized controlled trial.
Another limitation is that the patients were in the study for varying lengths of time. In particular, the time between the EHFScB-9 assessments at baseline and study end varied between 3 and 18 months.
Conclusion
Self-reported self-care behavior scores improved significantly from baseline to study end. Objectively measured adherence of daily weight and blood pressure measurements was very high and remained stable over time. Adherence to daily reporting of symptoms was lower and declined in the long-term.
The findings demonstrate that an automated education and coaching program, which is more scalable than human coaching, can be effective in improving self-care. A suggested next step is to compare this program with a control group receiving usual self-care education and a group receiving online education only, and to study the effect on clinical outcomes.
Supplementary material
Table S1.
| Month | M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 | M9 | M10 | M11 | M12 | M13 | M14 | M15 | M16 | M17 | M18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 120 | 120 | 118 | 116 | 105 | 92 | 87 | 80 | 66 | 57 | 47 | 35 | 26 | 15 | 7 | 5 | 4 | 1 |
| Weight | ||||||||||||||||||
| Max | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| 75th | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Median | 95.5 | 100.0 | 100.0 | 100.0 | 96.8 | 96.8 | 100.0 | 96.7 | 96.8 | 100.0 | 100.0 | 100.0 | 98.4 | 100.0 | 96.8 | 100.0 | 98.3 | 100.0 |
| 25th | 85.3 | 93.5 | 93.5 | 93.5 | 90.3 | 87.0 | 93.1 | 83.7 | 82.1 | 80.0 | 85.5 | 88.7 | 86.1 | 73.7 | 93.3 | 100.0 | 81.2 | 100.0 |
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 50.0 | 38.5 | 25.0 | 0.0 | 100.0 | 34.8 | 100.0 |
| Blood pressure | ||||||||||||||||||
| Max | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 76.7 |
| 75th | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 97.6 | 76.7 |
| Median | 95.1 | 100.0 | 100.0 | 96.8 | 96.7 | 96.8 | 100.0 | 96.7 | 96.7 | 96.8 | 96.7 | 93.5 | 95.2 | 93.3 | 96.7 | 96.8 | 91.9 | 76.7 |
| 25th | 85.4 | 93.3 | 93.3 | 90.8 | 83.3 | 86.7 | 92.7 | 79.6 | 83.9 | 85.2 | 83.6 | 80.6 | 82.4 | 72.1 | 80.5 | 90.0 | 83.6 | 76.7 |
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 38.7 | 23.1 | 0.0 | 0.0 | 73.3 | 73.3 | 76.7 |
| Symptoms | ||||||||||||||||||
| Max | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 13.3 |
| 75th | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 96.8 | 96.8 | 98.4 | 100.0 | 100.0 | 100.0 | 98.4 | 87.5 | 67.5 | 13.3 |
| Median | 92.2 | 93.4 | 93.5 | 93.5 | 93.3 | 91.8 | 96.2 | 88.0 | 83.6 | 90.3 | 87.1 | 91.7 | 88.0 | 86.7 | 90.0 | 51.6 | 50.9 | 13.3 |
| 25th | 66.7 | 66.6 | 75.0 | 74.0 | 64.5 | 60.0 | 60.6 | 47.6 | 45.5 | 40.0 | 62.4 | 48.3 | 47.3 | 20.8 | 26.3 | 20.0 | 35.0 | 13.3 |
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 3.2 | 0.0 | 0.0 | 0.0 | 18.2 | 4.3 | 13.3 |
Notes: For measuring weight, blood pressure, and symptoms reporting the maximum adherence, the 75th percentile, the median, the 25th percentile, and the minimum adherence per month are shown. The number of patients per month is indicated by n.
Acknowledgments
The authors gratefully thank W Armitage and M Clark for their contribution to the design of the program; B Schulte, K van Gelder, M Spanbroek, M van de Kamp, M Allmark, and A Tesanovic for the implementation of the program; and K Slottje, R Flockton, C Whitehead, P Atkin, P Gastelurrutia, M Domingo, and B Gonzalez Fernandez for performing the study. The authors thank H Reiter, C Westerteicher, A Bruege, U Goldbach, NK Bui, GJ de Vries, and A Rigby for their assistance. This research was supported by the European Commission under grant FP7-216695.
Footnotes
Disclosure
WS is employed by Philips. JGC has received research funding and honoraria for advice from Philips. CD and TJ report no conflicts of interest in this work.
References
- 1.Riegel B, Moser DK, Anker SD, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120(12):1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 2.Cleland JG, Ekman I. Enlisting the help of the largest health care workforce – patients. JAMA. 2010;304(12):1383–1384. doi: 10.1001/jama.2010.1387. [DOI] [PubMed] [Google Scholar]
- 3.Lee CS, Moser DK, Lennie TA, Riegel B. Event-free survival in adults with heart failure who engage in self-care management. Heart Lung. 2011;40(1):12–20. doi: 10.1016/j.hrtlng.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonagh TA, Blue L, Clark AL, et al. European Society of Cardiology Heart Failure Association Standards for delivering heart failure care. Eur J Heart Fail. 2011;13(3):235–241. doi: 10.1093/eurjhf/hfq221. [DOI] [PubMed] [Google Scholar]
- 5.Strömberg A, Ahlen H, Fridlund B, Dahlström U. Interactive education on CD-ROM – a new tool in the education of heart failure patients. Patient Educ Couns. 2002;46(1):75–81. doi: 10.1016/s0738-3991(01)00151-3. [DOI] [PubMed] [Google Scholar]
- 6.Orlowski JL, Oermann MH, Shaw-Kokot J. Evaluation of heart failure websites for patient education. Adv Emerg Nurs J. 2013;35(3):240–246. doi: 10.1097/TME.0b013e318296469b. [DOI] [PubMed] [Google Scholar]
- 7.Inglis SC, Clark RA, McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010;8:CD007228. doi: 10.1002/14651858.CD007228.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Oosterom-Calo R, Abma TA, Visse MA, Stut W, Te Velde SJ, Brug J. An interactive-technology health behavior promotion program for heart failure patients: Experiences and needs of patients and nurses in the hospital setting. JMIR Res Protoc. 2014;3(2):e32. doi: 10.2196/resprot.3188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaarsma T, Strömberg A, Ben Gal T, et al. Comparison of self-care behaviors of heart failure patients in 15 countries worldwide. Patient Educ Couns. 2013;92(1):114–120. doi: 10.1016/j.pec.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 10.van der Wal MH, Jaarsma T. Adherence in heart failure in the elderly: problem and possible solutions. Int J Cardiol. 2008;125(2):203–208. doi: 10.1016/j.ijcard.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Jaarsma T, Strömberg A, De Geest S, et al. Heart failure management programmes in Europe. Eur J Cardiovasc Nurs. 2006;5(3):197–205. doi: 10.1016/j.ejcnurse.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Cawthon C, Walia S, Osborn C, Niesner KJ, Schnipper JL, Kripalani S. Improving care transitions: the patient perspective. J Health Commun. 2012;17(Suppl 3):312–324. doi: 10.1080/10810730.2012.712619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manning S. Bridging the gap between hospital and home: a new model of care for reducing readmission rates in chronic heart failure. J Car-diovasc Nurs. 2011;26(5):368–376. doi: 10.1097/JCN.0b013e318202b15c. [DOI] [PubMed] [Google Scholar]
- 14.Sauvé MJ, Lewis WR, Blankenbiller M, Rickabaugh B, Pressler SJ. Cognitive impairments in chronic heart failure: a case controlled study. J Card Fail. 2009;15(1):1–10. doi: 10.1016/j.cardfail.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Harkness K, Heckman GA, Akhtar-Danesh N, Demers C, Gunn E, McKelvie RS. Cognitive function and self-care management in older patients with heart failure. Eur J Cardiovasc Nurs. 2014;13(3):277–284. doi: 10.1177/1474515113492603. [DOI] [PubMed] [Google Scholar]
- 16.Paul S. Hospital discharge education for patients with heart failure: What really works and what is the evidence? Crit Care Nurse. 2008;28:66–82. [PubMed] [Google Scholar]
- 17.Freedland KE, Rich MW, Skala JA, Carney RM, Dávila-Román VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med. 2003;65(1):119–128. doi: 10.1097/01.psy.0000038938.67401.85. [DOI] [PubMed] [Google Scholar]
- 18.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York: Guilford Press; 2002. [Google Scholar]
- 19.Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:69–119. [Google Scholar]
- 20.Balk AH, Davidse W, Dommelen Pv, et al. Tele-guidance of chronic heart failure patients enhances knowledge about the disease. A multi-centre, randomised controlled study. Eur J Heart Fail. 2008;10(11):1136–1142. doi: 10.1016/j.ejheart.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Grancelli H, Varini S, Ferrante D, et al. Randomized Study of Telephone Intervention in Chronic Heart Failure (DIAL): study design and preliminary observations. J Card Fail. 2003;9(3):172–179. doi: 10.1054/jcaf.2003.33. [DOI] [PubMed] [Google Scholar]
- 22.Dunagan WC, Littenberg B, Ewald GA, et al. Randomized study of a nurse-administered, telephone-based disease management program for patients with heart failure. J Card Fail. 2005;11(5):358–365. doi: 10.1016/j.cardfail.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K. Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled study to determine the effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc. 2009;57(3):395–402. doi: 10.1111/j.1532-5415.2009.02138.x. [DOI] [PubMed] [Google Scholar]
- 24.Stut W, Deighan C, Armitage W, Clark M, Cleland JG, Jaarsma T. Design and usage of the HeartCycle Education and Coaching Program for patients with heart failure. JMIR Res Protoc. 2014;3(4):e72. doi: 10.2196/resprot.3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Eur Heart J. 2008;29(19):2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 26.Lewin B, Robertson IH, Cay EL, Irving JB, Campbell M. Effects of self-help post-myocardial-infarction rehabilitation on psychological adjustment and use of health services. Lancet. 1992;339(8800):1036–1040. doi: 10.1016/0140-6736(92)90547-g. [DOI] [PubMed] [Google Scholar]
- 27.Clark M, Kelly T, Deighan C. A systematic review of the heart manual literature. Eur J Cardiovasc Nurs. 2011;10(1):3–13. doi: 10.1016/j.ejcnurse.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Jaarsma T, Strömberg A, Mårtensson J, Dracup K. Development and testing of the European Heart Failure Self-Care Behavior Scale. Eur J Heart Fail. 2003;5(3):363–370. doi: 10.1016/s1388-9842(02)00253-2. [DOI] [PubMed] [Google Scholar]
- 29.Jaarsma T, Arestedt KF, Mårtensson J, Dracup K, Strömberg A. The European Heart Failure Self-care Behaviour scale revised into a nine-item scale (EHFScB-9): a reliable and valid international instrument. Eur J Heart Fail. 2009;11(1):99–105. doi: 10.1093/eurjhf/hfn007. [DOI] [PubMed] [Google Scholar]
- 30.Uchmanowicz I, Loboz-Rudnicka M, Jaarsma T, Loboz-Grudzień K. Cross-cultural adaptation and reliability testing of Polish adaptation of the European Heart Failure Self-care Behavior Scale (EHFScBS) Patient Prefer Adherence. 2014;8:1521–1526. doi: 10.2147/PPA.S65890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kleppe M, Lacroix J, Ham J, Midden C. The development of the ProMAS: a Probabilistic Medication Adherence Scale. Patient Prefer Adherence. 2015;9:355–367. doi: 10.2147/PPA.S76749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nieuwenhuis MM, Jaarsma T, van Veldhuisen DJ, van der Wal MH. Self-reported versus ‘true’ adherence in heart failure patients: a study using the Medication Event Monitoring System. Neth Heart J. 2012;20(7–8):313–319. doi: 10.1007/s12471-012-0283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DiClemente CC, Marinilli AS, Singh M, Bellino LE. The role of feedback in the process of health behavior change. Am J Health Behav. 2001;25(3):217–227. doi: 10.5993/ajhb.25.3.8. [DOI] [PubMed] [Google Scholar]
- 34.Chaudhry SI, Mattera JA, Curtis JP, et al. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363(24):2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Varon C, Alao M, Minter J. Effect of telehealth on self-care behavior of heart failure patients. Comput Cardiol. 2014;41:473–476. [Google Scholar]
- 36.Boyne JJ, Vrijhoef HJ, Spreeuwenberg M, et al. Effects of tailored telemonitoring on heart failure patients’ knowledge, self-care, self-efficacy and adherence: a randomized controlled study. Eur J Cardiovasc Nurs. 2014;13(3):243–252. doi: 10.1177/1474515113487464. [DOI] [PubMed] [Google Scholar]
- 37.Dendale P, De Keulenaer G, Troisfontaines P, et al. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail. 2012;14(3):333–340. doi: 10.1093/eurjhf/hfr144. [DOI] [PubMed] [Google Scholar]
- 38.Prescher S, Deckwart O, Koehler K, et al. Will telemonitoring be adopted by patients with chronic heart failure? Dtsch Med Wochenschr. 2014;139(16):829–834. doi: 10.1055/s-0034-1369849. German. [DOI] [PubMed] [Google Scholar]
- 39.Domingo M, Lupón J, González B, et al. Evaluation of a telemedicine system for heart failure patients: feasibility, acceptance rate, satisfaction and changes in patient behavior: results from the CARME (CAtalan Remote Management Evaluation) study. Eur J Cardiovasc Nurs. 2012;11(4):410–418. doi: 10.1016/j.ejcnurse.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 40.Ledwidge MT, O’Hanlon R, Lalor L, et al. Can individualized weight monitoring using the HeartPhone algorithm improve sensitivity for clinical deterioration of heart failure? Eur J Heart Fail. 2013;15(4):447–455. doi: 10.1093/eurjhf/hfs186. [DOI] [PubMed] [Google Scholar]
- 41.Lyngå P, Persson H, Hägg-Martinell A, et al. Weight monitoring in patients with severe heart failure (WISH). A randomized controlled study. Eur J Heart Fail. 2012;14(4):438–444. doi: 10.1093/eurjhf/hfs023. [DOI] [PubMed] [Google Scholar]
- 42.de Lusignan S, Wells S, Johnson P, Meredith K, Leatham E. Compliance and effectiveness of 1 year’s home telemonitoring. The report of a pilot study of patients with chronic heart failure. Eur J Heart Fail. 2001;3(6):723–730. doi: 10.1016/s1388-9842(01)00190-8. [DOI] [PubMed] [Google Scholar]
- 43.Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Mobile phone-based telemonitoring for heart failure management: a randomized controlled study. J Med Internet Res. 2012;14(1):e31. doi: 10.2196/jmir.1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cleland JG, Louis AA, Rigby AS, Janssens U, Balk AH. Noninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the Trans-European Network-Home-Care Management System (TEN-HMS) study. J Am Coll Cardiol. 2005;45(10):1654–1664. doi: 10.1016/j.jacc.2005.01.050. [DOI] [PubMed] [Google Scholar]
- 45.Nolan RP, Payne AYM, Ross H, et al. An Internet-based counseling intervention with email reminders that promotes self-care in adults with chronic heart failure: randomized controlled study protocol. JMIR Res Protoc. 2014;3(1):e5. doi: 10.2196/resprot.2957. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
| Month | M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 | M9 | M10 | M11 | M12 | M13 | M14 | M15 | M16 | M17 | M18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 120 | 120 | 118 | 116 | 105 | 92 | 87 | 80 | 66 | 57 | 47 | 35 | 26 | 15 | 7 | 5 | 4 | 1 |
| Weight | ||||||||||||||||||
| Max | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| 75th | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Median | 95.5 | 100.0 | 100.0 | 100.0 | 96.8 | 96.8 | 100.0 | 96.7 | 96.8 | 100.0 | 100.0 | 100.0 | 98.4 | 100.0 | 96.8 | 100.0 | 98.3 | 100.0 |
| 25th | 85.3 | 93.5 | 93.5 | 93.5 | 90.3 | 87.0 | 93.1 | 83.7 | 82.1 | 80.0 | 85.5 | 88.7 | 86.1 | 73.7 | 93.3 | 100.0 | 81.2 | 100.0 |
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 50.0 | 38.5 | 25.0 | 0.0 | 100.0 | 34.8 | 100.0 |
| Blood pressure | ||||||||||||||||||
| Max | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 76.7 |
| 75th | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 97.6 | 76.7 |
| Median | 95.1 | 100.0 | 100.0 | 96.8 | 96.7 | 96.8 | 100.0 | 96.7 | 96.7 | 96.8 | 96.7 | 93.5 | 95.2 | 93.3 | 96.7 | 96.8 | 91.9 | 76.7 |
| 25th | 85.4 | 93.3 | 93.3 | 90.8 | 83.3 | 86.7 | 92.7 | 79.6 | 83.9 | 85.2 | 83.6 | 80.6 | 82.4 | 72.1 | 80.5 | 90.0 | 83.6 | 76.7 |
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 38.7 | 23.1 | 0.0 | 0.0 | 73.3 | 73.3 | 76.7 |
| Symptoms | ||||||||||||||||||
| Max | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 13.3 |
| 75th | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 96.8 | 96.8 | 98.4 | 100.0 | 100.0 | 100.0 | 98.4 | 87.5 | 67.5 | 13.3 |
| Median | 92.2 | 93.4 | 93.5 | 93.5 | 93.3 | 91.8 | 96.2 | 88.0 | 83.6 | 90.3 | 87.1 | 91.7 | 88.0 | 86.7 | 90.0 | 51.6 | 50.9 | 13.3 |
| 25th | 66.7 | 66.6 | 75.0 | 74.0 | 64.5 | 60.0 | 60.6 | 47.6 | 45.5 | 40.0 | 62.4 | 48.3 | 47.3 | 20.8 | 26.3 | 20.0 | 35.0 | 13.3 |
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 3.2 | 0.0 | 0.0 | 0.0 | 18.2 | 4.3 | 13.3 |
Notes: For measuring weight, blood pressure, and symptoms reporting the maximum adherence, the 75th percentile, the median, the 25th percentile, and the minimum adherence per month are shown. The number of patients per month is indicated by n.