Abstract
Background
Orthostatic tremor (OT) is defined by the presence of a high-frequency (13–18 Hz) tremor of the legs upon standing associated with a feeling of unsteadiness. However, some patients have discharge frequencies of <13 Hz, so-called “slow OT”. The aim of this study was to characterize patients with unsteadiness upon standing found to have <13 Hz tremor discharges on neurophysiologic testing.
Methods
A retrospective review was performed on all subjects with a diagnosis of OT who were referred to the Mayo Clinic, Scottsdale, AZ, between 1999 and 2013 for confirmation using neurophysiology.
Results
Fourteen of 28 subjects (50%) had OT discharges of <13 Hz, of whom eight had frequencies of <10 Hz and six had frequencies of 10–13 Hz. Lower frequency discharges tended to have a broader spectral peak, greater variability in discharge duration, and lower inter-muscular coherence. Subjects with <13 Hz OT had shorter mean disease duration at time of neurophysiology testing (2.00 years in <10 Hz group, 7.96 years 10–13 Hz group, and 11.43 years >13 Hz; p = 0.002). The proportion of subjects who experienced gait unsteadiness (85.7% vs. 66.6% vs. 21.4%; p = 0.016), falls (37.5% vs. 50% vs. 0%; p = 0.010), and had abnormal gait on examination (71.4% vs. 66.0% vs. 14.3%; p = 0.017) was greater in those with low and intermediate frequencies.
Discussion
Slow tremor electromyography frequencies (<13 Hz) may characterize a substantial proportion of patients labeled as OT. These subjects may have greater gait involvement and higher likelihood of falls leading to earlier presentation to subspecialty care.
Keywords: Orthostatic tremor, neurophysiology
Introduction
Orthostatic tremor (OT) causes unsteadiness with standing and is often a source of considerable disability and distress in those affected. High frequency electromyography (EMG) discharges (13–18 Hz) are typical and part of the criteria established by the Movement Disorders Society (MDS),1 although some reports use frequencies as low as 10 Hz as the lower limit for defining OT.2–4 Neurophysiologic testing in classic OT characteristically shows brief, highly rhythmic discharges that demonstrate high inter-muscular coherence.5,6 It is unknown where in the nervous system the tremor discharges are generated. A central nervous system source associated with stance mechanisms in brainstem–cerebellum circuits is often cited.7,8 However, a recent cortico-muscular coherence study suggests that more widespread networks are involved.9 Both the uncertainty of the source mechanism and the heterogeneous characteristics of OT cases contribute to disagreement about phenomenology of OT in general.7
Some patients with unsteadiness upon standing are found to have slow tremor discharges on neurophysiologic testing. The term “slow OT” has been widely used in the literature although some discourage this term.7 So-called “slow OT” was first described in 1986 in a family with essential tremor.10 It has since been documented in case reports and small case series with the term applied to frequencies as low as 4 Hz11 and as high as 10–11 Hz.12 Most cases of “slow OT” have been reported in the setting of an underlying disorder, including Grave’s disease,13 multiple sclerosis,11 suspected paraneoplastic syndrome,14 cerebellar ataxia,15,16 and Parkinson’s disease.17,18 Rare cases of “slow OT” as an idiopathic condition not associated with any underlying neurologic disease have also been described.12,19 Although the clinical and neurophysiologic features of patients with classic or “fast” OT have been reported in several large case series,3,4,20,21 little is known about the characteristics of <13 Hz cases and the literature is limited to case reports and short case series. The main objective of this study was to describe the characteristics of patients with clinical suspicion of OT who were referred to our Movement Neurophysiology Laboratory and found to have <13 Hz EMG tremor discharges on neurophysiologic testing.
Methods
A retrospective review of cases was performed on all subjects with a clinical diagnosis of OT who were referred to the Mayo Clinic Arizona, Neurology Clinic, between 1999 and 2013 for confirmation using neurophysiology. All patients were evaluated by a Mayo Clinic staff neurologist and met the MDS clinical criteria for OT.
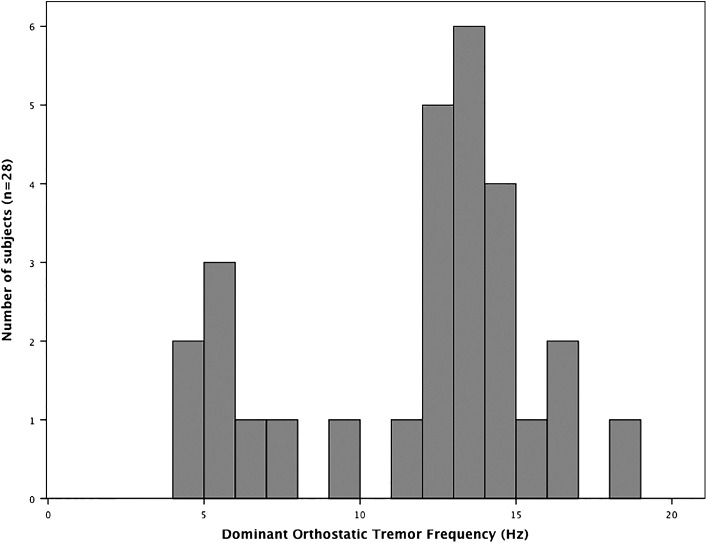
Demographic and clinical features were collected from the charts. The Neuroscan System (Compumedics Neuroscan, Charlotte, NC, USA) was used to collect neurophysiologic data on all subjects. Surface EMG recordings were collected at 1,000 Hz (1–200 Hz bandpass) with the patient sitting comfortably in a chair, during postural activation with wrist extension and/or arms outstretched, during various functional maneuvers (finger-to-nose testing, handwriting), standing, and in some cases leaning against an object from a standing position. Neurophysiologic information was extracted from the neurophysiology reports and from systematic analysis of the stored EMG data. The predominant frequency of tremor was determined by spectral analysis and confirmed to be consistent with visual inspection of the number of bursts per second in all cases. The lower frequency OT group (<13 Hz) was subdivided into two groups, intermediate (10–13 Hz) and low frequency (<10Hz), based on clustering seen on the histogram analysis (Figure 1).
Figure 1. Histogram Analysis Showing the Distribution of Dominant Tremor Frequencies.
For inter-muscular coherence analysis, the data were processed off-line with EMG rectification, creation of 4,096-point epochs for a frequency resolution of 0.2444 Hz, artifact rejection, and inspection for right wrist extensor EMG activation during artifact-free epochs. The 4,096-point epochs were consecutive and non-overlapping. Individual files yielded 60–80 epochs. These epochs were then used to perform fast Fourier transform and coherence analysis for all electrode pairs up to 200 Hz. For consistency, the coherence results reported are between the right and the left anterior tibialis leg muscles, and the dominant frequency was used to determine coherence values. To assess variability in EMG burst interval duration, we measured the width of the frequency peak at half the peak amplitude. The mean values for each of the three groups were calculated.
A descriptive analysis of neurophysiologic and clinical variables was performed using SPSS v.21 (IBM Corp., Armonk, NY, USA). Continuous variables were analyzed using one-way analysis of variance when normally distributed and using the Kruskal–Wallis test when not normally distributed. Categorical variables were analyzed using the Fisher exact test. A p-value of <0.05 was considered significant. The Mayo Clinic Institutional Review Board approved this study.
Results
Neurophysiologic and clinical data were available in 28 subjects from 1999 to 2013. There were 14 patients with fast OT in the range of >13 Hz and 14 with frequencies of <13 Hz (Figure 1). Those with <13 Hz OT were further subdivided into a low-frequency group (<10 Hz) consisting of eight patients and an intermediate frequency group (10–13 Hz) consisting of six patients.
The EMG phase relationship between ipsilateral antagonist leg muscles varied among subjects (Table 1). The mean coherence was lowest in the <10 Hz group and highest in the >13 Hz group (mean 0.53, 0.74, and 0.91) with a statistically significant difference between each group using multiple comparisons with Tukey correction (all p<0.01) (Table 1).
Table 1. Neurophysiologic Features.
| <10 Hz (n = 8) | 10–13 Hz (n = 6) | >13 Hz (n = 14) | |
|---|---|---|---|
| Phase relationship1 | |||
| Mixed | 3 | 1 | 9 |
| Alternating | 2 | 3 | 2 |
| Co-contraction | 3 | 2 | 3 |
| Mean inter-muscular coherence (95% CI)2 | 0.53 (0.43–0.63) | 0.74 (0.60–0.89) | 0.91 (0.88–0.94) |
| Mean width in Hz of dominant frequency peak at half peak amplitude (95% CI) | 1.51 (1.24–1.79) | 1.00 (0.65–1.35) | 0.66 (0.59–0.72) |
| Arm tremor leaning3 | 3/3 (all <10 Hz) | 1/1 (12.45 Hz) | 8/8 (all 13–19Hz) |
| Arm tremor with postural activation (n, %) | 6 (75) | 2 (33.3) | 9 (64.2) |
| Arm tremor discharges 13–18 Hz | 0 | 0 | 5 |
| Arm tremor discharges 10–13 Hz | 2 | 2 | 0 |
| Arm tremor discharges <10 Hz | 4 | 0 | 4 |
Between ipsilateral antagonist leg muscles on standing.
Between right and left tibialis anterior muscles on standing.
Maneuver performed by the number of patients indicated in the denominator.
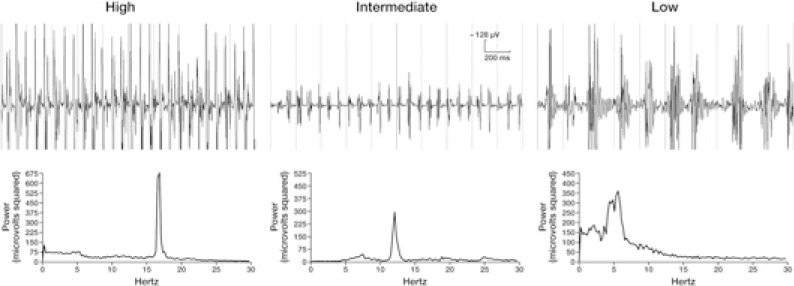
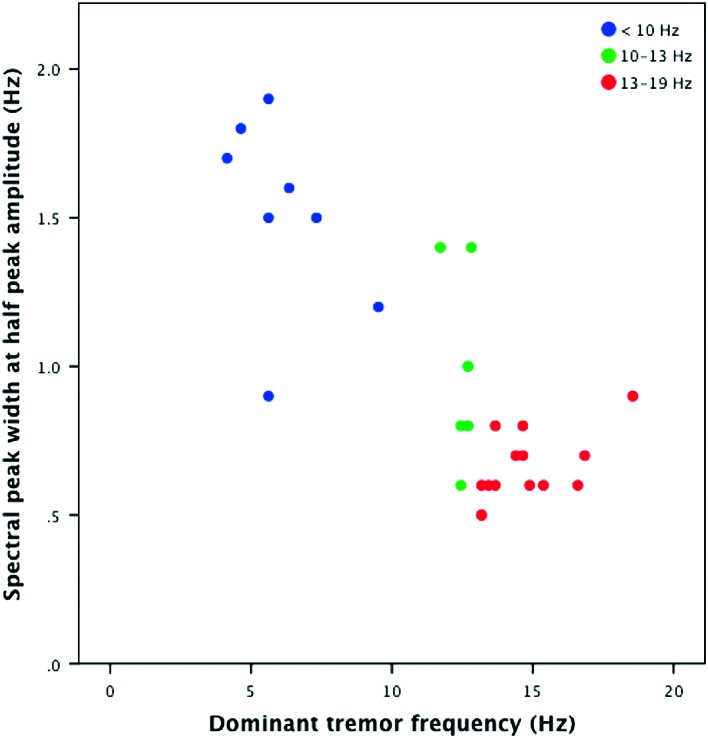
Those with classic orthostatic leg tremor (>13 Hz) had uniformly brief discharges based on visual inspection of individual surface EMG tracings (Figure 2). Cases with 10–13 Hz frequency tremor also had a high proportion of short-duration discharges whereas those in the <10 Hz group had longer-duration discharges with a low proportion of short-duration discharges. The variability in EMG burst interval duration also differed between groups as calculated by the mean spectral peak width at half of the peak amplitude. This mean value was largest in the <10 Hz group and smallest in the >13 Hz group (mean 1.51, 1.00, and 0.66 Hz) with a statistically significant difference between each group using multiple comparisons with Tukey correction (all p<0.05) (Table 1). Clustering of subjects by tremor frequency is shown in Figure 3.
Figure 2. Surface Electromyography Tracings and Spectral Analysis in Patients with High-, Intermediate-, and Low-Frequency Orthostatic Tremor.
Figure 3. Dominant Tremor Frequency vs. Spectral Peak Width at Half Peak Amplitude for Each Patient (blue <10 Hz; green 10–13 Hz; red 13–19 Hz)..
Arm tremor was present with weight bearing by leaning forward in all patients in whom this maneuver was performed (Table 1). In each case, the tremor frequency in the arms was similar to the orthostatic frequency in the legs. Postural arm tremor across a spectrum of frequencies was seen in some patients of all three groups (Table 1).
The clinical features are detailed in Table 2. The groups did not differ with respect to age at the time of neurophysiologic assessment or gender. Mean disease duration was significantly shorter in the <10 Hz group. All patients in this study reported unsteadiness upon standing but unsteadiness with walking, abnormal gait on examination, and falls were more common in the lower frequency groups. Only half the patients in the <10 Hz group had a feeling of tremor whereas symptomatic tremor was reported by all but one subject with tremor of >10 Hz frequency.
Table 2. Demographic and Clinical Information.
| <10 Hz (n = 8) | 10–13 Hz (n = 6) | >13 Hz (n = 14) | p-value | |
|---|---|---|---|---|
| Mean age (years) | 75 | 69.5 | 71.21 | 0.690 |
| Gender female/male (% female) | 7/1 (87.5) | 2/4 (33.3) | 8/6 (57.1) | 0.122 |
| Mean disease duration (years) | 2.00 | 7.96 | 11.43 | 0.002 |
| Mean age at disease onset (years) | 72.88 | 61.3 | 59.71 | 0.093 |
| Symptoms1 | ||||
| Feeling of tremor | 4 (50) | 6 (100) | 13 (92.8) | 0.032 |
| Unsteadiness with standing | 8 (100) | 6 (100) | 14 (100) | |
| Unsteadiness with walking | 6/7 (85.7) | 4 (66.6) | 3 (21.4) | 0.016 |
| Documented falls | 3 (37.5) | 3 (50) | 0 (0.00) | 0.010 |
| Examination | ||||
| Leg tremor | 5 (62.5) | 5 (83.3) | 12 (85.7) | 0.493 |
| Abnormal gait | 5/7 (71.4) | 4 (66) | 2 (14.3) | 0.017 |
| Family history of tremor | 3 (37.5) | 0 (0) | 3 (21.4) | 0.145 |
Data presented as n (%).
The rows containing significant p-values are in bold
Five out of 14 patients with <13 Hz OT (all in the intermediate range) had an underlying neurologic disease: one had a spinal dural atriovenous fistula, one had cerebellar degeneration of unknown cause, one had suspected autoimmune autonomic dysfunction with elevated PQ-type calcium channel antibodies, one had a peripheral neuropathy, and one had a myelopathy. None of the patients with OT across the range of frequencies had parkinsonism.
Various medications were used to treat OT with at least partial response seen in some patients to clonazepam, gabapentin, primidone, and propranolol (Table 3). No benefit was seen in the few subjects treated with topiramate, valproic acid, levodopa, pramipexole, or alprazolam.
Table 3. Proportion of Patients Experiencing at Least Partial Benefit from Medication.
| <10 Hz | 10–13 Hz | >13 Hz | |
|---|---|---|---|
| Clonazepam | 1/1 | 2/3 | 1/5 |
| Gabapentin | 2/2 | 1/2 | 4/9 |
| Primidone | 1/3 | – | 1/6 |
| Propanolol | – | – | 1/2 |
| Topiramate | – | – | 0/4 |
| Valproic acid | – | – | 0/2 |
| Levodopa | – | – | 0/2 |
| Pramipexole | – | – | 0/1 |
| Alprazolam | – | – | 0/2 |
Discussion
Fifty percent of the cases in this series had tremor frequencies below the 13–18 Hz criteria for OT established by the MDS.1 This relatively high occurrence of lower frequencies may be due to a referral bias at our laboratory in which “classic OT” is often not referred for neurophysiology testing. Nevertheless, our results suggest that lower frequencies characterize a substantial proportion of cases that have at least partial clinical overlap with classically defined >13 Hz OT. Despite MDS criteria, both confusion and disagreement exist with regard to when the term “slow OT” should be used or whether it should be used at all. Erro and colleagues7 nicely outline this dilemma and point out many knowledge gaps that exist about OT. These authors maintain that EMG frequency is critical for diagnosing OT. However, the expertise and/or opportunity may not be available in many cases. Even so, EMG frequency, perhaps supplemented by inter-muscular coherence, seems to be the best available testing to confirm classic OT. A major finding in our study was that the group with EMG frequency in the 10–13 Hz range seemed quite close in many respects to the >13 Hz group, both clinically and electrophysiologically. The 10–13 Hz group had high inter-muscular coherence, although not quite as high as the >13 Hz group. Indeed, one recent article used cases as low as 10 Hz.4 However, our low frequency group (<10 Hz) had greater differences, both clinically and electrophysiologically, from the classically defined >13 Hz cases. This supports the general feeling in the literature that such slow cases bear little resemblance to higher frequency cases and maybe should not be labeled OT at all.7
It is interesting that besides EMG frequency, other physiologic differences may characterize these groups. A neurophysiologic pattern emerges in this study in which those with fast discharges (13–19 Hz) had brief, highly rhythmic, often synchronous discharges whereas longer and more varied burst interval lengths were seen in those with intermediate and low frequency OT. The physiologic meaning of this relatively small but statistically significant frequency peak width difference is unknown, but the value seems to characteristically increase as OT frequency decreases. Furthermore, there is lower coherence (i.e., less constant phase difference at a given frequency between homologous leg muscles) in those with lower-frequency discharges. Others have observed the same neurophysiologic hallmarks of fast and slow OT.18 The term orthostatic myoclonus (OM) has been applied in three case series in recent years2,18,22 and has been distinguished from “slow OT” by the presence of clinical myoclonus, uniformly shorter burst durations (30–100 ms), lack of right/left burst synchrony, and the irregularity of the discharges.18 This raises the question of whether, at least in some cases, different terminologies are being used for the same disorder. We feel that our cases do not represent OM because they demonstrated a low percentage of short-duration discharges (Figure 2) and exhibited some coherence even at lower discharge frequencies. Moreover, the strong frequency peak supports OT even in the lower-frequency cases.
Gait involvement was present in the majority of patients with <13 Hz OT in this study and has been documented in some case reports14,15 but not others.10–12,19 Others have also found gait impairment and falls to be relatively infrequent in patients with fast OT. Falls were reported in only four of 26 patients with fast OT in one study,3 and gait impairment felt to be secondary to OT in only two of 26 patients in another study.21 Disease duration at the time of the movement neurophysiology test was shorter in those with slow OT, particularly in the group with <10 Hz frequency. Although precise disability comparisons were not possible in this retrospective analysis, the association between <13 Hz OT and gait difficulties/falls may have led to earlier specialty consultation due to greater impairment of function. Whether <13 Hz OT progresses at a different rate from >13 Hz OT is unknown.
Postural arm tremor is common in classic OT and was seen in five out of 14 cases of fast OT but none of those with slow OT. Arm tremor was present with weight bearing by leaning forward in patients from all three groups. In each case, the tremor frequency in the arms was similar to the orthostatic frequency in the legs. This phenomenon was observed in 27 out of 30 patients with OT in one study,23 and in all eight patients with OT in another.2
Although the etiology of OT is unknown, it is commonly reported in the setting of underlying neurologic disease. In one of the largest series of OT, 10 out of 41 patients had additional neurologic features (termed OT-plus) including six with parkinsonism.20 “Slow OT” is commonly reported as symptomatic of another condition. Five out of 14 patients with <13 Hz OT in this study had an underlying neurologic disease. It is unclear whether the neurologic disorders present in the patients we describe had any relationship to the co-existing OT and most cases in this study appear to be idiopathic.
Response to medication in fast OT is often unsatisfactory, with many patients failing to achieve lasting benefit. Our findings are in line with others who have reported a proportion of patients with at least partial response to clonazepam, gabapentin, primidone, and propranolol.3,4,20,21 Numbers in the lower-frequency OT groups are too few to make any firm conclusions about medication responsiveness, but there is a suggestion that the same drugs used in classic OT may be effective in some patients with lower-frequency OT as well.
Despite some clinical and neurophysiologic overlap found here and pointed out sporadically in the literature, “slow OT” would seem to represent a different clinical entity than classic “fast OT” with more heterogeneous clinical and neurophysiologic features. Slower frequency tremor discharges tended to have a broader spectral peak with greater variability in discharge duration. These subjects may have greater gait involvement and higher likelihood of falls leading to earlier presentation to subspecialty care. It is possible that the 10–13 Hz group has a closer relationship to the classic >13 Hz group than to the <10 Hz group but this speculation arising from our results needs further study. We recommend that orthostatic movement problems be studied in the neurophysiology laboratory when uncertainty exists about the nature of the disorder. Further study is warranted to determine differences in underlying pathophysiology and etiology of cases along the frequency spectrum of clinical tremor and shaking induced by standing.
Footnotes
Funding: None.
Financial Disclosures: J.C. has received research funding from Amarin Pharmaceuticals, the Michael J. Fox Foundation, the National Institutes of Health, and the Arizona Biomedical Research Foundation, and received consulting fees from Teva.
Conflicts of Interest: The authors report no conflict of interest.
References
- 1.Deuschl G, Bain P, Brin M. Consensus statement of the Movement Disorder Society on Tremor. Ad Hoc Scientific Committee. Mov Disord. 1998;13:2–23. doi: 10.1002/mds.870131303. [DOI] [PubMed] [Google Scholar]
- 2.van Gerpen JA. A retrospective study of the clinical and electrophysiological characteristics of 32 patients with orthostatic myoclonus. Parkinsonism Relat Disord. 2014;20:889–893. doi: 10.1016/j.parkreldis.2014.05.006. doi: http://dx.doi.org/10.1016/j.parkreldis.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piboolnurak P, Yu QP, Pullman SL. Clinical and neurophysiologic spectrum of orthostatic tremor: Case series of 26 subjects. Mov Disord. 2005;20:1455–1461. doi: 10.1002/mds.20588. doi: http://dx.doi.org/10.1002/mds.20588. [DOI] [PubMed] [Google Scholar]
- 4.Yaltho TC, Ondo WG. Orthostatic tremor: A review of 45 cases. Parkinsonism Relat Disord. 2014;20:723–725. doi: 10.1016/j.parkreldis.2014.03.013. doi: http://dx.doi.org/10.1016/j.parkreldis.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Britton TC, Thompson PD, van der Kamp W, et al. Primary orthostatic tremor: Further observations in six cases. J Neurol. 1992;239:209–217. doi: 10.1007/BF00839142. doi: http://dx.doi.org/10.1007/BF00839142. [DOI] [PubMed] [Google Scholar]
- 6.Köster B, Lauk M, Timmer J, et al. Involvement of cranial muscles and high intermuscular coherence in orthostatic tremor. Ann Neurol. 1999;45:384–388. doi: 10.1002/1531-8249(199903)45:3<384::aid-ana15>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 7.Erro R, Bhatia K, Cordivari C. Shaking on standing: A critical review. Mov Disord Clin Pract. 2014;1:172–179. doi: 10.1002/mdc3.12053. doi: http://dx.doi.org/10.1002/mdc3.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wills AJ, Thompson PD, Findley LJ, Brooks DJ. A positron emission tomography study of primary orthostatic tremor. Neurology. 1996;46:747–752. doi: 10.1212/wnl.46.3.747. doi: http://dx.doi.org/10.1212/WNL.46.3.747. [DOI] [PubMed] [Google Scholar]
- 9.Muthuraman M, Hellriegel H, Paschen S, et al. The central oscillatory network of orthostatic tremor. Mov Disord. 2013;28:1424–1430. doi: 10.1002/mds.25616. doi: http://dx.doi.org/10.1002/mds.25616. [DOI] [PubMed] [Google Scholar]
- 10.Wee AS, Subramony SH, Currier RD. ‘Orthostatic tremor’ in familial-essential tremor. Neurology. 1986;36:1241–1245. doi: 10.1212/wnl.36.9.1241. doi: http://dx.doi.org/10.1212/WNL.36.9.1241. [DOI] [PubMed] [Google Scholar]
- 11.Baker M, Fisher K, Lai M, Duddy M, Baker S. Slow orthostatic tremor in multiple sclerosis. Mov Disord. 2009;24:1550–1553. doi: 10.1002/mds.22630. doi: http://dx.doi.org/10.1002/mds.22630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coffeng SM, Hoff JI, Tromp SC. A slow orthostatic tremor of primary origin. Tremor Other Hyperkinet Mov (NY) 2013;3:1–3. doi: 10.7916/D8057DNW. http://www.tremorjournal.org/article/view/147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin FC, Wu MN, Chen CH, Huang P. Slow orthostatic tremor as the first manifestation of Grave’s disease. Mov Disord. 2013;28:1158–1159. doi: 10.1002/mds.25313. doi: http://dx.doi.org/10.1002/mds.25313. [DOI] [PubMed] [Google Scholar]
- 14.Hegde M, Glass GA, Dalmau J, Christine CW. A case of slow orthostatic tremor, responsive to intravenous immunoglobulin. Mov Disord. 2011;26:1563–1565. doi: 10.1002/mds.23610. doi: http://dx.doi.org/10.1002/mds.23610. [DOI] [PubMed] [Google Scholar]
- 15.Williams ER, Jones RE, Baker SN, Baker MR. Slow orthostatic tremor can persist when walking backward. Mov Disord. 2010;25:795–797. doi: 10.1002/mds.23024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Setta F, Jacquy J, Hildebrand J, Manto MU. Orthostatic tremor associated with cerebellar ataxia. J Neurol. 1998;245:299–302. doi: 10.1007/s004150050222. doi: http://dx.doi.org/10.1007/s004150050222. [DOI] [PubMed] [Google Scholar]
- 17.Kim JS, Lee MC. Leg tremor mimicking orthostatic tremor as an initial manifestation of Parkinson’s disease. Mov Disord. 1993;8:397–398. doi: 10.1002/mds.870080331. doi: http://dx.doi.org/10.1002/mds.870080331. [DOI] [PubMed] [Google Scholar]
- 18.Leu-Semenescu S, Roze E, Vidailhet M, et al. Myoclonus or tremor in orthostatism: An under-recognized cause of unsteadiness in Parkinson's disease. Mov Disord. 2007;22:2063–2069. doi: 10.1002/mds.21651. [DOI] [PubMed] [Google Scholar]
- 19.Uncini A, Onofrj M, Basciani M, Cutarella R, Gambi D. Orthostatic tremor: Report of two cases and an electrophysiological study. Acta Neurol Scand. 1989;79:119–122. doi: 10.1111/j.1600-0404.1989.tb03722.x. doi: http://dx.doi.org/10.1111/j.1600-0404.1989.tb03722.x. [DOI] [PubMed] [Google Scholar]
- 20.Gerschlager W, Brown P. Orthostatic tremor – A review. Handb Clin Neurol. 2011;100:457–462. doi: 10.1016/B978-0-444-52014-2.00035-5. doi: http://dx.doi.org/10.1016/B978-0-444-52014-2.00035-5. [DOI] [PubMed] [Google Scholar]
- 21.Mestre TA, Lang AE, Ferreira JJ, et al. Associated movement disorders in orthostatic tremor. J Neurol Neurosurg Psychiatry. 2012;83:725–729. doi: 10.1136/jnnp-2012-302436. doi: http://dx.doi.org/10.1136/jnnp-2012-302436. [DOI] [PubMed] [Google Scholar]
- 22.Glass GA, Ahlskog JE, Matsumoto JY. Orthostatic myoclonus: A contributor to gait decline in selected elderly. Neurology. 2007;68:1826–1830. doi: 10.1212/01.wnl.0000260225.46732.af. [DOI] [PubMed] [Google Scholar]
- 23.McManis PG, Sharbrough FW. Orthostatic tremor: Clinical and electrophysiologic characteristics. Muscle Nerve. 1993;16:1254–1260. doi: 10.1002/mus.880161117. [DOI] [PubMed] [Google Scholar]