Abstract
Background:
Corticosteroids, delivered systemically and by inhalation, are widely used for the treatment of multiple acute respiratory illnesses in children. However, the level of evidence to support the utility of this therapy varies between these different acute respiratory illnesses.
Objective:
To summarize the evidence regarding the utility of corticosteroids in the management of common acute pediatric respiratory conditions and to highlights the controversies regarding their use.
Methods:
Literature search of manuscripts describing the evidence regarding the efficacy of corticosteroids (systemic and inhaled) in the management of: acute asthma exacerbation among school age children, acute episodic wheeze among preschool children, viral croup, and acute viral bronchiolitis.
Results:
Current evidence indicates that systemic corticosteroids provide benefits for the treatment of acute asthma exacerbations in school age children, mainly in the acute care setting. In addition, high dose inhaled corticosteroid therapy administered in the Emergency Department appears to have comparable effect for the prevention of asthma-related hospital admission as systemic corticosteroids in this age group. In contrast, most available studies have not shown benefit for systemic corticosteroids during acute wheezing episodes in preschool children. Systemic corticosteroids decrease symptoms and the rate of hospital admissions in patients with severe croup; however, corticosteroids have no role in the treatment of acute bronchiolitis and their use in this condition should be discouraged.
Conclusion:
Corticosteroids treatment response varies between the acute respiratory illnesses presented in this review. Future research should aim to fill the current gaps-of-knowledge regarding the utility this intervention such as the identification of specific wheezing phenotypes among preschool children which might benefit from systemic corticosteroids as a treatment for acute viral wheeze.
Keywords: Corticosteroids, asthma, wheezing, croup, bronchiolitis, children
Both systemic and inhaled corticosteroids (ICSs) have been widely used for the treatment of numerous acute respiratory illnesses associated with airway inflammation. The goal of this review is to present the evidence regarding the utility of this treatment in the management of common acute pediatric respiratory conditions: acute asthma exacerbation among school age children, acute episodic wheeze among preschool children, viral croup, and acute viral bronchiolitis. In addition, this review highlights the substantial controversies regarding the use of corticosteroids for some of these acute conditions.
GENERAL CONCEPTS REGARDING THE MECHANISM OF ACTION OF CORTICOSTEROIDS
The antiinflammatory effects of corticosteroids are mediated by both genomic and nongenomic effect, which have been well-described elsewhere.1,2 Glucocorticoids interact with the intracellular glucocorticoid receptor leading to alterations in gene expression and transcription. Corticosteroids also block the activity of nuclear factor κB, which stimulates the transcription of cytokines, chemokines, adhesion molecules, and the attendant receptors for these molecules. The nongenomic effects include glucocorticoid signaling through membrane-associated receptors and second message receptors. The effects related to pulmonary disease include accelerated eosinophil death (apoptosis) and prolonged lifespan of neutrophils by inhibiting apoptosis. The number of mast cells in the airway wall has also been shown to decrease with regular inhaled glucocorticoid treatment. Corticosteroids have vasoconstrictive effects that may contribute to their clinical actions by resulting in reduced airway edema and less microvascular leakage. In addition corticosteroids reduce airway mucus production.
The onset of corticosteroid effects in vivo varies due to the multiple pathways of corticosteroid action. Although the genomic effects of glucocorticoids on gene expression occur over hours to days, the vasoconstrictive effect has an onset of action within four hours of administration, resulting in more rapid improvement of airway edema, and corticosteroid-driven improvement in β-agonist responsiveness is detectable within 12 hours.
ACUTE ASTHMA IN SCHOOL-AGE CHILDREN
Systemic Corticosteroids
The combined available evidence indicates that the administration of systemic corticosteroids hasten the resolution of acute exacerbations of asthma, particularly in the emergency department (ED) and hospital settings. Children with acute asthma episodes who receive systemic corticosteroids in the ED experience lower admission rates for asthma3 and shorter lengths of stay in hospital. Two randomized controlled studies of parental administration of prednisolone at home among preschool and school age children provide inconsistent results, with one trial showing no difference in outpatient visits for acute asthma among children 2–14 years of age,4 whereas a study including children 5–12 years of age demonstrated modest benefit in symptom scores, health care use, and school absences among children treated with prednisolone 1 mg/kg per day for three days relative to placebo.5 Dosing recommendations for systemic corticosteroids in acute asthma are based upon a limited number of studies comparing various dosing regimens6 and indicate a minimal dose response relationship in daily prednisone/prednisolone dosing and clinical improvement. A trial including 98 children, 1–15 years of age hospitalized with acute asthma demonstrated no difference in patterns of recovery between groups receiving prednisolone 0.5, 1, and 2 mg/kg per day in addition to inhaled bronchodilators.7 Kayani and Shannon8 demonstrated comparable efficacy between 1- and 2-mg/kg per day dosing regimens of prednisone for five days among 86 children with asthma exacerbations, although the 2-mg/kg per day group experienced higher rates of behavioral side effects (e.g., anxiety) and aggressive behavior. The National Asthma Education and Prevention Program (NAEPP) Guidelines9 recommend a dosing regimen of 1–2 mg/kg per day (maximum 60 mg per day) for the treatment of asthma exacerbation in children. Until additional dose ranging trials are conducted in children, we suggest using the NAEPP-recommended dosing approach. Once-daily and multiple daily dosing approaches are comparable in clinical outcomes.10 Although studies are limited in number, there appears to be no significant difference in the efficacy of oral corticosteroids (OCSs) or parenteral corticosteroids on the length of hospital stay in children with acute asthma exacerbations,11 although parenteral administration may be preferred in the child who is unable to tolerate oral medications due to vomiting. Given its longer biologic duration of action and thus potential for shorter courses of therapy, dexamethasone has also been studied in ED management of acute asthma. A recent metaanalysis concluded there was no difference in the relative risk of relapse between dexamethasone (intramuscular or oral, one or two doses) and prednisone/prednisolone (oral for five days) and that children treated with dexamethasone were less likely to experience emesis.12
Given the well-described side effect profile of repeated or continuous use of systemic corticosteroids, frequency of OCS courses should always be minimized. There is no evidence for clinically significant hypothalamic–pituitary–adrenal axis suppression after short “bursts” of systemic corticosteroids for acute exacerbations of asthma,13 and tapering is not required with courses of 10 days or less in duration. However, tapering may be considered if doses that are greater than the NAEPP-recommended dosing are given in this period of time. Furthermore, there is no evidence for increased susceptibility to common acute infections.14
When systemic corticosteroids are administered for asthma exacerbations, the child should be continue to receive maintenance ICS to reinforce the importance of this medication, although no literature has addressed the clinical utility of this practice.
Inhaled Corticosteroids
Given their established efficacy in the chronic management of asthma, along with a favorable adverse effect profile, many studies have examined the potential role of high-dose ICS in children presenting with acute asthma exacerbations. Interpretation of these studies is complicated by use of different ICS medications, delivery devices, and dosing regimens along with methodological limitations. Despite these challenges, two recent metaanalyses were consistent in their conclusions that high-dose ICS therapy administered in the ED to children with acute asthma resulted in comparable hospital admission rates as children treated with systemic corticosteroids,15,16 as well as comparable rates of unscheduled visits for asthma and need for additional OCSs.16 High-dose ICS therapy in the ED was superior to placebo in reducing the rate of hospitalization.15 However, two studies demonstrated that improvement in measures of pulmonary function was more rapid among children who receive systemic corticosteroids.17,18 Although these metaanalyses15,16 indicate no evidence of difference in the clinical efficacies of systemic and ICSs, limitations of the studies which comprise the metaanalyses, predominantly relatively small sample sizes, temper these findings and provide insufficient evidence at the present time to recommend the routine use of high-dose ICS as an alternative to systemic corticosteroids in children presenting to ED with acute exacerbations of asthma. However, in milder episodes, high-dose ICS therapy may be an acceptable alternative to systemic corticosteroids. Finally, a recent metaanalysis19 that included three trials in 909 patients (mostly adults) concluded that there is insufficient evidence that ICS therapy provides additional benefit when used in combination with standard systemic corticosteroid therapy upon ED discharge for acute asthma.
ACUTE EPISODIC WHEEZE IN PRESCHOOL CHILDREN
Systemic Corticosteroids
Wheezing episodes during the preschool years, which are usually triggered by viral respiratory infections, are the most common presentation in the pathway of developing childhood asthma.20–22 Given the multitude of patterns of early childhood wheezing, with their differing pathophysiologies and natural histories,23,24 clinical trials that have evaluated corticosteroid response in this age group have included mixed populations of children with wheezing, both single-wheezing-episode and recurrent wheezing. In addition, many trials are comprised of populations that could be appropriately classified as experiencing episodic wheeze, whereas others may include those with both episodic wheeze and diagnosed asthma. Although OCSs are recommended by all asthma guidelines for acute asthma exacerbations that are not responsive to bronchodilators,9 these guidelines do not include age-specific (or preschool wheezing phenotype-specific) recommendations regarding OCSs use. Although acute episodic wheeze among preschool children has traditionally been treated with OCSs based on the established efficacy of this intervention among older children with asthma,25 a growing number of recent studies have questioned the utility of this intervention.
Two clinical trials investigated the utility of early parent-initiated OCSs at home among preschool children with recurrent wheeze. Participants in both studies had histories of at least one previous wheeze and/or asthma urgent visit. Oommen et al.26 randomized preschool children to parent-initiated prednisolone 20 mg per day for five days, whereas Grant et al.4 in a crossover trial, randomized children to treatment blocks of a single 2-mg/kg dose of prednisone, or placebo; the latter trial included preschool and school aged children, but reported the results of a subgroup analysis that included only children 2–5 years old. These studies both concluded that parent-initiated OCSs treatment at home did not prevent unscheduled clinic visits, ED visits, or hospital admissions. Moreover, Grant et al.4 actually reported a higher proportion of children requiring unscheduled clinic or ED visits among the children treated with OCSs compared with placebo (35% versus 14%, p = 0.04). The investigators could not identify any reason for this unexpected finding. We can speculate that children treated with OCS were seen in ED for reasons other than pure respiratory distress, including irritability triggered by the OCS. Additional stratification of the participants in the Oommen study26 by the level of eosinophilic priming (serum levels of eosinophilic cationic protein and eosinophilic protein X), as a predictor for future persistent atopic asthma, did not change the negative results of this study. Interpretation of this study is complicated by a high rate of noncompliance with the study protocol (∼70% of parents), reducing the external validity of its results.26 Two randomized double-blinded placebo-controlled trials investigated the efficacy of systemic corticosteroids in the ED setting with inconsistent results. Tal et al.27 randomized preschool children with histories of at least three wheezing episodes to receive a single dose of 4 mg/kg of intramuscular methylprednisolone or placebo and reported that corticosteroid treatment was associated with a significantly lower proportion of participants requiring admission (20% versus 43%, p < 0.05) and with a significant improvement in respiratory symptom scores. Csonka et al.28 randomized preschool children to receive oral prednisolone (2-mg/kg per day for three days) and found no difference in the proportions of admitted children (54% versus 53%; p = 0.88); OCSs treatment, among the children who were eventually hospitalized was associated with a numerically, but not statistically significant, shorter duration of hospital stay (two versus three days, p = 0.06). Patient characteristics in that study28 limit its external validity, because ∼40% of the participants had never been treated previously for wheezing.
Finally, Panickar et al.29 performed the largest clinical trial investigating the efficacy of OCSs treatment among 687 preschool children hospitalized due to acute viral wheeze. Participants were randomized to receive five days of oral prednisolone (10 mg per day for five days for children 24 months old and younger, or 20 mg per day for older children) or placebo. There was no significant difference in the primary outcome, the duration of hospitalization, between the prednisolone and placebo groups (median 11.0 versus 13.9 hours, respectively, p = 0.18). There were no significant differences between the groups in the secondary outcomes including: clinical symptom scores over the first day of admission, the mean seven-day symptom score assessed by the parents, and the number of hospital readmissions for wheezing within a month after discharge. Initial disease severity measured by symptom scores did not influence the primary outcome. In addition, the result of the primary analysis did not change once analyzed only in a subgroup of children who were at an increased risk for atopic asthma. This subgroup fulfilled the major criteria of the Asthma Predictive Index as suggested by Castro-Rodríguez et al.30: children with a history of four or more wheezing episodes who had a parent with asthma or who had physician-diagnosed eczema. The results of this study should be interpreted within the context of its study population characteristics: approximately one third of the participants did not have previous wheezing episodes, suggesting that many were experiencing viral bronchiolitis, a disease that is resistant to treatment with corticosteroids (see below). Moreover, the generally mild severity of episodes, evident by a short duration of hospitalization (less than 14 hours in the placebo group), might be an additional reason for the negative results.
Beigelman et al.31 recently performed a post hoc analysis in two independent outpatient cohorts of preschool children with episodic wheeze. The investigators evaluated symptom scores during more than 1500 respiratory tract illnesses over two clinical trials and concluded that OCSs treatment at home for acute lower-respiratory tract illnesses did not reduce symptom severity during these acute episodes and did not facilitate symptom resolution.31
Overall, the majority of published studies do not support the utility of OCSs treatment for preschool acute episodic wheeze. Lack of OCSs response in this age group might be related to the heterogeneity of wheezing phenotypes in early life and/or a lesser level of chronic eosinophilic airway inflammation, which is generally corticosteroid responsive, among most of these young children with episodic wheeze. Editorials on this topic have suggested reconsideration of OCSs use in preschool viral-associated wheeze, including reserving this treatment to the most seriously ill, hospitalized children.32,33 However, it remains uncertain whether OCSs might be effective in selected subgroups of atopic preschool children with more persistent, rather than episodic, asthma symptoms. In addition, as the currently available trials have substantial limitations, additional prospective randomized controlled trials are required to fully define the place of OCS in preschool wheezing illnesses before abandoning this longstanding therapy.
Inhaled Corticosteroids
As noted above, two metaanalyses revealed that high-dose ICS therapy administered in the ED to children (mainly older school aged children) with acute asthma resulted in comparable hospital admission rates as in children treated with systemic corticosteroids.15,16 Among the studies reviewed in these metaanalyses, only one study included preschool predominant populations. Milani et al. reported that compared with placebo, treatment with 2 mg of inhaled budesonide given in the ED did not result in a faster improvement of clinical score.34 However, only one participant in this study34 was admitted, so it was not possible to evaluate the efficacy of the intervention to prevent admissions. Given the limited data available, and the uncertainty regarding the efficacy of systemic corticosteroids in this age group, it is not possible to draw a firm conclusion regarding the role of high-dose ICS treatment for acute exacerbation among young preschool children.
CROUP
Croup (laryngotracheitis) usually occurs in children between six months and six years of age. Prodromal symptoms include coryza and fever, which may progress to severe and typically nocturnal respiratory distress.35,36 The most common agents include parainfluenza virus and rhinovirus. Other viruses such as enterovirus, respiratory syncytial virus, influenza virus, and human bocavirus have been identified.37 Midautumn is the peak time for onset of this illness. The illness is usually handled well as an outpatient with less than 10% of patients requiring hospital admission. Supportive treatment alone is effective in most children and includes hydration and increased inspired humidity. In more significantly affected children, the vasoconstrictive effect of L-epinephrine (1:1000) and racemic epinephrine (2.25%) may lead to a rapid, albeit transient, decrease in central airway resistance and alleviate increased work of breathing.38 Given the inflammatory nature of the illness, corticosteroids (oral, parenteral, and inhaled) have been studied in the management of croup. The overall evidence suggests that the oral delivery of dexamethasone at a dose of 0.3 mg/kg for moderate croup up to 0.6 mg/kg for severe croup as a single dose is helpful in decreasing symptoms at 6, 12, and 24 hours after treatment, decreasing the need to use nebulized epinephrine, reducing the length of stay in the ED and resulting in fewer hospital admissions.36,39,40 The onset of action of dexamethasone may be clinically apparent as soon as 30 minutes after its administration.41 In a patient who is not vomiting, there is little evidence to suggest that parenteral administration is superior to oral administration.42 In children with mild-moderate croup seeking outpatient (but not ED care), oral treatment with prednisolone 2 mg/kg daily for three days and dexamethasone 0.6 mg/kg for 1 day followed by two days of placebo did not differ in terms of need for additional health care, or symptom reduction.43 Although one study demonstrated that prednisone 1 mg/kg daily has been shown to be equally effective to dexamethasone, a recent study suggests that there is a higher rate of return to the ED for a second visit if prednisone is used as opposed to dexamethasone.35,43 In an effort to reduce systemic exposure to corticosteroids, high ICS have also been examined in acute viral croup. A single dose of inhaled budesonide 2 mg in children with mild-moderate croup requiring ED care was superior to placebo in terms of symptom score reduction, time in the ED, and use of systemic corticosteroids after the ED visit.44 However, in a direct comparative trial, dexamethasone 0.6 mg/kg intramuscularly was superior to inhaled budesonide 4 mg in terms of more rapid clinical improvement in children seen in the ED for moderately severe croup.45 The onset of action is apparent within one to two hours after nebulization. There is no evidence that patients receive adjunctive benefit from both nebulized and either OCS or parenteral corticosteroid. The weight of the evidence suggests that the oral or parenteral route is preferred for ease of administration and cost effectiveness. Patients may be discharged from the ED once one dose of corticosteroid has been given and once the patient has been observed for at least two to four hours after nebulized epinephrine has been administered.
ACUTE BRONCHIOLITIS
The current American Academy of Pediatrics bronchiolitis guidelines recommend that “clinicians should not administer systemic corticosteroids to infants with a diagnosis of bronchiolitis in any setting.”46 This recommendation is supported by a recent metaanalysis that included 17 trials (2596 participants) comparing systemic or ICS with placebo, which concluded that corticosteroid treatment does not prevent admissions (risk ratio = 0.92; 95% confidence interval, 0.78–1.08), shorten the duration of hospitalization (mean difference = −0.18 days; 95% confidence interval −0.39 to 0.04), or have any relevant effects on the secondary outcomes.47 One of the trials included in this metaanalysis found that the combination of nebulized epinephrine with oral dexamethasone administered in the ED was superior to placebo in preventing hospital admission.48 However, there was no clinical benefit for nebulized epinephrine or oral dexamethasone given alone, and the effect of the combined intervention became nonstatistically significant after adjustment for multiple comparisons. Finally, oral dexamethasone (1 mg/kg on day 1, followed by 0.6 mg/kg for four additional days) given to hospitalized bronchiolitis patients who have eczema or a first degree family member with asthma shortened the duration of the hospitalization.49 The results of these studies must be confirmed in additional trials before any change to the recommendation to not administer corticosteroids for viral bronchiolitis is considered.
SUMMARY AND AREAS OF UNCERTAINTY/GAPS OF KNOWLEDGE
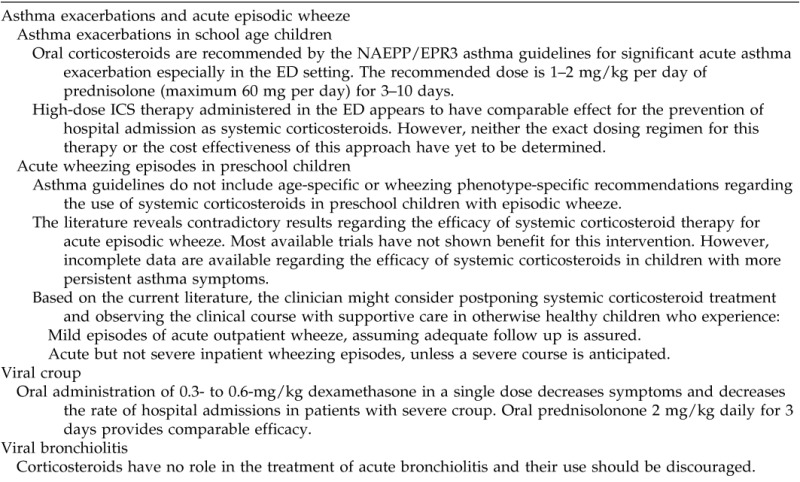
Given their broad antiinflammatory actions, corticosteroids have been used widely for acute respiratory illnesses associated with an inflammatory trigger, most often acute viral infection. The current evidence regarding the use of corticosteroids in these acute pediatric respiratory disorders is summarized in Table 1. Although patients with several disease states, such as asthma and viral croup, have been consistently found to benefit from corticosteroid therapy, other conditions are less predictably responsive. The reasons for these differences remain incompletely understood and deserve further examination. Furthermore, clinical trials in these conditions have been complicated by heterogeneous patient populations, likely representing different disease processes and thus a wide range of therapeutic responses. Future research should include adequately powered clinical trials focused on distinct and well-defined disease phenotypes, use pharmacologically sufficient doses of corticosteroids, include robust and clinically relevant outcome measures, and strive to identify patient and infectious factors which may influence outcomes.
Table 1.
Summary of the evidence regarding the use of corticosteroids in acute pediatric respiratory disorders
Footnotes
A. Beigelman is supported by research grants from the National Heart, Lung, and Blood Institute and the National Institute of Allergic and Infectious Diseases/National Institutes of Health. L.B. Bacharier is supported by research grants from the National Heart, Lung, and Blood Institute and the National Institute of Allergic and Infectious Diseases/National Institutes of Health
B.E. Chipps is on the Speaker's Bureau for AstraZeneca, Boehringer Ingelheim, Genentech, Meda, Merck, and Novartis and advisor for consult for AstraZeneca, Genentech, Meda, Merck, and Novartis. L.B. Bacharier is an advisor consult for Aerocrine, GlaxoSmithKline, Genentech/Novartis, Merck, Schering, Cephalon, DBV Technologies, and Teva and is on the Speaker's Bureau for Aerocrine, AstraZeneca, Genentech/Novartis, GlaxoSmithKline, Merck, Schering, and Teva.
REFERENCES
- 1. Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids–new mechanisms for old drugs. N Engl J Med 353:1711–1723, 2005. [DOI] [PubMed] [Google Scholar]
- 2. de Benedictis FM, Bush A. Corticosteroids in respiratory diseases in children. Am J Respir Crit Care Med 185:12–23, 2012. [DOI] [PubMed] [Google Scholar]
- 3. Scarfone RJ, Fuchs SM, Nager AL, Shane SA. Controlled trial of oral prednisone in the emergency department treatment of children with acute asthma. Pediatrics 92:513–518, 1993. [PubMed] [Google Scholar]
- 4. Grant CC, Duggan AK, DeAngelis C. Independent parental administration of prednisone in acute asthma: A double-blind, placebo-controlled, crossover study. Pediatrics 96:224–229, 1995. [PubMed] [Google Scholar]
- 5. Vuillermin P, South M, Robertson C. Parent-initiated oral corticosteroid therapy for intermittent wheezing illnesses in children. Cochrane Database Syst Rev CD005311, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang L, Mendoza RA. Doses of systemic corticosteroids in hospitalised children with acute asthma: A systematic review. J Paediatr Child Health 42:179–183, 2006. [DOI] [PubMed] [Google Scholar]
- 7. Langton Hewer S, Hobbs J, Reid F, Lenney W. Prednisolone in acute childhood asthma: Clinical responses to three dosages. Respir Med 92:541–546, 1998. [DOI] [PubMed] [Google Scholar]
- 8. Kayani S, Shannon DC. Adverse behavioral effects of treatment for acute exacerbation of asthma in children: A comparison of two doses of oral steroids. Chest 122:624–628, 2002. [DOI] [PubMed] [Google Scholar]
- 9. National Asthma Education and Prevention Program. Expert Panel Report III: Guidelines for the diagnosis and management of asthma. Bethesda, MD: US Department of Health and Human Services; 2007. [Google Scholar]
- 10. Kelly HW. What is the dose of systemic corticosteroids for severe asthma exacerbations in children? Pediatr Asthma Allergy Immunol 22:75–80, 2009. [Google Scholar]
- 11. Becker JM, Arora A, Scarfone RJ, et al. Oral versus intravenous corticosteroids in children hospitalized with asthma. J Allergy Clin Immunol 103:586–590, 1999. [DOI] [PubMed] [Google Scholar]
- 12. Keeney GE, Gray MP, Morrison AK, et al. Dexamethasone for acute asthma exacerbations in children: A meta-analysis. Pediatrics 133:493–499, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ducharme FM, Chabot G, Polychronakos C, et al. Safety profile of frequent short courses of oral glucocorticoids in acute pediatric asthma: Impact on bone metabolism, bone density, and adrenal function. Pediatrics 111:376–383, 2003. [DOI] [PubMed] [Google Scholar]
- 14. Grant CC, Duggan AK, Santosham M, DeAngelis C. Oral prednisone as a risk factor for infections in children with asthma. Arch Pediatr Adolesc Med 150:58–63, 1996. [DOI] [PubMed] [Google Scholar]
- 15. Su XM, Yu N, Kong LF, Kang J. Effectiveness of inhaled corticosteroids in the treatment of acute asthma in children in the emergency department: A meta-analysis. Ann Med 46:24–30, 2014. [DOI] [PubMed] [Google Scholar]
- 16. Beckhaus AA, Riutort MC, Castro-Rodriguez JA. Inhaled versus systemic corticosteroids for acute asthma in children. A systematic review. Pediatr Pulmonol 49:326–334, 2014. [DOI] [PubMed] [Google Scholar]
- 17. Schuh S, Dick PT, Stephens D, et al. High-dose inhaled fluticasone does not replace oral prednisolone in children with mild to moderate acute asthma. Pediatrics 118:644–650, 2006. [DOI] [PubMed] [Google Scholar]
- 18. Schuh S, Reisman J, Alshehri M, et al. A comparison of inhaled fluticasone and oral prednisone for children with severe acute asthma. N Engl J Med 343:689–694, 2000. [DOI] [PubMed] [Google Scholar]
- 19. Edmonds ML, Milan SJ, Brenner BE, et al. Inhaled steroids for acute asthma following emergency department discharge. Cochrane Database Syst Rev 12:CD002316, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bacharier LB, Guilbert TW. Diagnosis and management of early asthma in preschool-aged children. J Allergy Clin Immunol 130:287–296; quiz 97–98, 2012. [DOI] [PubMed] [Google Scholar]
- 21. Beigelman A, Bacharier LB. Infection-induced wheezing in young children. J Allergy Clin Immunol 133:603–604 e4, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ducharme FM, Tse SM, Chauhan B. Diagnosis, management, and prognosis of preschool wheeze. Lancet 383:1593–1604, 2014. [DOI] [PubMed] [Google Scholar]
- 23. Savenije OE, Granell R, Caudri D, et al. Comparison of childhood wheezing phenotypes in 2 birth cohorts: ALSPAC and PIAMA. J Allergy Clin Immunol 127:1505–1512 e14, 2011. [DOI] [PubMed] [Google Scholar]
- 24. Martinez FD, Wright AL, Taussig LM, et al. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med 332:133–138, 1995. [DOI] [PubMed] [Google Scholar]
- 25. Rowe BH, Spooner CH, Ducharme FM, et al. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev CD000195, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Oommen A, Lambert PC, Grigg J. Efficacy of a short course of parent-initiated oral prednisolone for viral wheeze in children aged 1–5 years: Randomised controlled trial. Lancet 362:1433–1438, 2003. [DOI] [PubMed] [Google Scholar]
- 27. Tal A, Levy N, Bearman JE. Methylprednisolone therapy for acute asthma in infants and toddlers: A controlled clinical trial. Pediatrics 86:350–356, 1990. [PubMed] [Google Scholar]
- 28. Csonka P, Kaila M, Laippala P, et al. Oral prednisolone in the acute management of children age 6 to 35 months with viral respiratory infection-induced lower airway disease: A randomized, placebo-controlled trial. J Pediatr 143:725–730, 2003. [DOI] [PubMed] [Google Scholar]
- 29. Panickar J, Lakhanpaul M, Lambert PC, et al. Oral prednisolone for preschool children with acute virus-induced wheezing. N Engl J Med 360:329–338, 2009. [DOI] [PubMed] [Google Scholar]
- 30. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med 162:1403–1406, 2000. [DOI] [PubMed] [Google Scholar]
- 31. Beigelman A, King TS, Mauger D, et al. Do oral corticosteroids reduce the severity of acute lower respiratory tract illnesses in preschool children with recurrent wheezing? J Allergy Clin Immunol 131:1518–1525, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bush A. Practice imperfect–treatment for wheezing in preschoolers. N Engl J Med 360:409–410, 2009. [DOI] [PubMed] [Google Scholar]
- 33. Grigg J. Role of systemic steroids in acute preschool wheeze. Arch Dis Child 95:491–492, 2010. [DOI] [PubMed] [Google Scholar]
- 34. Milani GK, Rosario Filho NA, et al. Nebulized budesonide to treat acute asthma in children. J Pediatr (Rio J) 80:106–112, 2004. [PubMed] [Google Scholar]
- 35. Petrocheilou A, Tanou K, Kalampouka E, et al. Viral croup: Diagnosis and a treatment algorithm. Pediatr Pulmonol 49:421–429, 2014. [DOI] [PubMed] [Google Scholar]
- 36. Cherry JD. Clinical practice. Croup. N Engl J Med 358:384–391, 2008. [DOI] [PubMed] [Google Scholar]
- 37. Rihkanen H, Ronkko E, Nieminen T, et al. Respiratory viruses in laryngeal croup of young children. J Pediatr 152:661–665, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Waisman Y, Klein BL, Boenning DA, et al. Prospective randomized double-blind study comparing L-epinephrine and racemic epinephrine aerosols in the treatment of laryngotracheitis (croup). Pediatrics 89:302–306, 1992. [PubMed] [Google Scholar]
- 39. Bjornson CL, Klassen TP, Williamson J, et al. A randomized trial of a single dose of oral dexamethasone for mild croup. N Engl J Med 351:1306–1313, 2004. [DOI] [PubMed] [Google Scholar]
- 40. Russell KF, Liang Y, O'Gorman K, et al. Glucocorticoids for croup. Cochrane Database Syst Rev CD001955, 2011. [DOI] [PubMed] [Google Scholar]
- 41. Dobrovoljac M, Geelhoed GC. How fast does oral dexamethasone work in mild to moderately severe croup? A randomized double-blinded clinical trial. Emerg Med Australas 24:79–85, 2012. [DOI] [PubMed] [Google Scholar]
- 42. Rittichier KK, Ledwith CA. Outpatient treatment of moderate croup with dexamethasone: Intramuscular versus oral dosing. Pediatrics 106:1344–1348, 2000. [DOI] [PubMed] [Google Scholar]
- 43. Sparrow A, Geelhoed G. Prednisolone versus dexamethasone in croup: A randomised equivalence trial. Arch Dis Child 91:580–583, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Klassen TP, Feldman ME, Watters LK, et al. Nebulized budesonide for children with mild-to-moderate croup. N Engl J Med 331:285–289, 1994. [DOI] [PubMed] [Google Scholar]
- 45. Johnson DW, Jacobson S, Edney PC, et al. A comparison of nebulized budesonide, intramuscular dexamethasone, and placebo for moderately severe croup. N Engl J Med 339:498–503, 1998. [DOI] [PubMed] [Google Scholar]
- 46. Ralston SL, Lieberthal AS, Meissner HC, et al. Clinical practice guideline: The diagnosis, management, and prevention of bronchiolitis. Pediatrics 134:e1474–e1502, 2014. [DOI] [PubMed] [Google Scholar]
- 47. Fernandes RM, Bialy LM, Vandermeer B, et al. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev 6:CD004878, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Plint AC, Johnson DW, Patel H, et al. Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med 360:2079–2089, 2009. [DOI] [PubMed] [Google Scholar]
- 49. Alansari K, Sakran M, Davidson BL, et al. Oral dexamethasone for bronchiolitis: A randomized trial. Pediatrics 132:e810–e816, 2013. [DOI] [PubMed] [Google Scholar]


