Abstract
Background
Patient-centeredness (i.e., providing care that is responsive to individual patient preferences) is increasingly recognized as a crucial element of quality of care.
Methods
A six-item patient-centeredness questionnaire was devised to assess the self-perceived needs of essential tremor (ET) patients. A link to the questionnaire was included in the monthly e-newsletter of the International Essential Tremor Foundation. The questionnaires were completed online and data were available in electronic format.
Results
There were 1,418 respondents. One in three respondents (i.e., 31.4%) indicated that the doctor was not even “moderately well-educated” about ET. Only 11.8% of respondents were satisfied with their care. Respondents raised a multiplicity of issues that were not being addressed in their current care. The top items were psychological services and support (33.9%), physical or occupational therapy (28.6%), handling embarrassment and social effects of tremor (15.8%), feelings of not being in control (13.7%), a detailed report and a more quantitative way of assessing tremor and tracking progression (12.7%), better counseling about current treatment and medications (11.9%), empathy, compassion and a feeling of being heard (11.6%), a treatment approach other than just medications and surgery (11.2%), and a discussion of all symptoms aside from tremor (e.g., cognition, balance).
Discussion
Patients with ET identified a broad range of issues that they felt were not addressed in their treatment; indeed, only one in 10 patients reported that they were satisfied with their care. It is hoped that patient-centered approaches such as this will lead to improved models for the care of patients with this common chronic disease.
Keywords: Essential tremor, treatment, clinical, patient-centeredness
Introduction
Essential tremor (ET) is one of the most common neurological diseases, with an estimated seven million affected persons in the United States.1,2 The disease is both chronic and progressive.3,4 The proportion of affected persons who seek treatment is unclear, although several studies suggest this to be 19.3–21.3% in Western countries.5,6 Hence, a considerable number of patients with ET worldwide, and on the order of hundreds of thousands to millions in the United States alone, are under the care of a doctor. During the visit to the doctor, tremor is assessed and treated; quality of life is sometimes evaluated as well.7
Yet, the issues that doctors focus on are not necessarily what is important to patients,8 and there is often a disconnect. Patient-centeredness (i.e., providing care that is responsive to individual patient preferences) is increasingly recognized as a crucial yet often overlooked element of quality of care.8 Indeed, patient-centeredness is one of the Institute of Medicines’ six quality dimensions.8 With this in mind, one may ask: What is the perspective and clinical experience of ET patients? What are the self-perceived needs, both met and unmet, of ET patients? Though seemingly simple in nature, we are unaware of a study that has addressed these specific questions.
A related issue is that there is a national trend towards patient-centered as well as multidisciplinary care, both in neurology and in other branches of medicine.9 How would ET patients design the ideal patient-centered clinical treatment center?
In this study, we designed and piloted a questionnaire to assess the treatment needs of ET patients, and then administered it to more than 1,000 ET patients. The overarching goal was to identify the unmet self-identified needs of ET patients. Such efforts at consumer participation and feedback are expected to be a key ingredient for efforts that lead to improvements in chronic disease care.10
Methods
Questionnaire development
A patient-centeredness questionnaire was developed by one of the authors (E.D.L.), a senior movement disorder neurologist with longstanding and focused clinical and research interests in ET. During the development of the questionnaire, he consulted neurological colleagues about the formulation of questions. After an initial version of the questionnaire was developed, he consulted 20 consecutively seen ET patients in his clinical practice, and then made several changes. The final questionnaire comprised six questions (Appendix 1). Four of the questions (numbers 1, 3, 4, and 5) were designed for open-ended responses, rather than yes–no or multiple choice responses, so as to obtain the most detailed and individual-level responses. Two of the questions (numbers 3 and 6) asked for graded responses. All of the questions related to patient’s views on the quality of their treatment and what was lacking from that treatment. This process and the data collection were approved by the University Institutional Review Board.
Data collection
The monthly e-newsletter of the International Essential Tremor Foundation (IETF) included the following statement: “The IETF and Elan Louis MD….are partnering to gather information about the treatment needs of essential tremor patients. Please take a few minutes to fill out the brief survey below.” A link was provided to an electronic questionnaire. The questionnaire was posted online on October 20, 2014, and remained online until December 3, 2014.
Data analysis
The questionnaires were completed online; therefore, data were available in electronic format. Two of the authors reviewed the data, carefully assigning responses to discrete categories. Data were entered into SPSS (Version 21.0) for additional analyses.
Results
There were 1,418 responses, and a large majority of these were within the first 2 weeks of posting. Data on questions 2, 3, 4, and 6 were the most informative. Two of the open-ended questions (1 and 5) resulted in data that were less detailed, less informative, and often duplicated that provided by responses to the other questions; hence data on these two questions were not presented.
In question 2, respondents were asked, “If you were going to design a comprehensive approach/ideal clinical center for the treatment of tremor, which problems, aside from tremor, would you focus attention on?” The top 10 responses (Table 1) were psychological services/support (33.9%), physical or occupational therapy (i.e., help with self or personal care or personal hygiene) (28.6%), handling embarrassment and social effects of tremor (15.8%), discussion of more treatment options or alternative treatment options (8.7%), stigma reduction (7.9%), more individualized treatment (7.4%), anxiety (6.8%), depression (6.3%), patient education (5.1%), and support groups (4.9%). Sample responses may be found for each response item (Table 1), providing a more vivid portrayal of the nature of the response. In addition to these top issues, 20 other issues were raised (Table 1).
Table 1. Responses to Survey Question 2: “If You Were Going to Design a Comprehensive Approach/Ideal Clinical Center for the Treatment of Tremor, Which Problems, Aside from Tremor, Would You Focus Attention On?”.
| Response Category | Example (Sample Quotation from Respondents) | Number (%) of Patients Who Raised This Issue |
|---|---|---|
| Psychological services/support | “Aid in the mental and emotional feelings dealing with this disease.” | 396 (33.9) |
| Physical or occupational therapy. Help with self or personal care or personal hygiene | “Occupational therapy related to dealing with the effects of tremor on ADLs such as eating and speaking among other things.” “Feeding, preparing meals, bathing, dressing, applying makeup, fixing hair, walking, exercise, driving.” “Help with hygiene issues: clipping toenails, manicures, tweezing eyebrows etc.” |
334 (28.6) |
| Handling embarrassment and social effects of tremor | “Being social with tremor. How to deal with the shame and isolation due to tremor.” | 184 (15.8) |
| Don’t know | “Cannot say.” “Don’t know.” “I am not qualified to comment.” |
127 (10.9) |
| Doctor should discuss more treatment options or alternative treatment options | “Offering a wide range of treatment modalities.” “Better treatment besides brain surgery to control hand tremors.” “Medications, strategies, or alternate methods to improve functioning.” “Alternative treatment options.” |
102 (8.7) |
| Public education/stigma reduction | “A way for the public to not automatically think we have Alzheimer’s.” “Educate the public so there is not such a fear of embarrassment.” |
92 (7.9) |
| More individualized treatment | “A person-centered approach that starts with a full occupational interview, then builds the team from the needs identified from that. For instance, not everyone would be interested in a surgical approach or need a psychiatrist.” | 87 (7.4) |
| Anxiety | “Anxiety caused by dealing with tremor.” | 79 (6.8) |
| Depression | “Dealing with the depression associated with tremor.” | 73 (6.3) |
| Education for patients | “Assembly of a wide range of information resources that someone with essential tremors may consult.” | 59 (5.1) |
| Support groups | “Caring circles.” “Creating an area where people with ET can get together and talk.” |
57 (4.9) |
| Research | “Comprehensive research….Until the cause is identified, the treatments will be unsatisfactory.” | 53 (4.5) |
| Education and support for family members of patients | “Counseling should include the family members who are living with it as well, both as caregivers and potentially future patients.” | 49 (4.2) |
| Treat the whole person | “A health and wellness approach to lessen the tremors.” “Treat the entire person, physical, mental, emotional, etc.” |
46 (3.9) |
| Assistive devices or new technologies to lessen tremor | “Assistive devices which could be taken home and tried, like a computer mouse.” “Gadgets to help with eating and writing.” |
43 (3.7) |
| Better/more comprehensive assessments | “Methodology to analytically differentiate between ET and PD.” “Comprehensive diagnostics.” |
41 (3.5) |
| Speech therapy, help with voice tremors | “I would design some sort of approach on the throat or speech issue caused by this tremor.” | 39 (3.3) |
| Specific mention of stress reduction | “Relaxing techniques in stress situations.” “Stress and relaxation help. Sometimes that helps with the tremors.” “Stress reduction and its effects on tremor.” |
37 (3.2) |
| Dietary/nutrition counseling | “How to arrange my life so as to minimize tremor, e.g., no caffeine, fewer carbs.” | 35 (3.0) |
| Help with employment or workplace issues | “Dealing with employer’s misconceptions.” “Career counseling.” “Counseling for younger people in careers dealing with the problem.” |
29 (2.5) |
| Cognitive issues | “Cognitive functions as related to tremors.” “Cognitive and memory issues related to long term use of tremor meds.” |
26 (2.2) |
| Fewer barriers and better access to treatment | “Have more centers in all states making it easier for ET patients to get to.” | 22 (1.9) |
| Multidisciplinary care and coordinated care across specialties | “Build teams of specialists trained in the treatment of essential tremors.” “Communication between providers to discuss all of the patient’s unique medical needs.” |
22 (1.9) |
| Doctors who understand complex illness and who understand the complexity of ET | “A doctor who understands how different diseases or illnesses may affect the tremor and be understanding of the patient’s challenges.” “Health professionals who know about ET and a comprehensive interprofessional team.” |
22 (1.9) |
| More educated doctors | “Better training for clinicians and doctors to recognize essential tremor as an illness separate from other similar illnesses.” | 21 (1.8) |
| Specific alternative therapies or treatments (e.g., acupuncture, natural remedies, massage therapy) | “Alternative therapies such as acupuncture.” “Alternative medications (prescription and traditional alternative medication) for those of us who respond poorly to the traditionally prescribed meds.” |
15 (1.3) |
| Prognosis | “Examples of what you will and will not be able to do (as ET progresses.” “Preparkinson’s possibility.” “The stages of tremor.” |
14 (1.2) |
| Help for younger or pediatric patients | “Treating tremor in the younger population (under 50).” | 13 (1.1) |
| Social worker to help coordinate services | “A social worker or someone to work towards maintaining your independence.” “Counselor to talk about life needs (disability insurance).” |
13 (1.1) |
| Address sleep problems | “Insomnia…internal tremors that never let you feel relaxed.” “Sleep deprivation, fatigue.” |
11 (0.9) |
| Dealing with frustration | “Dealing with frustration.” “Frustration that stems from not being able to do ordinary tasks quickly and efficiently.” |
9 (0.8) |
ADLs, Activities of Daily Living; ET, Essential Tremor; PD, Parkinson’s Disease.
In question 3, respondents rated the importance of various specialists in their care (Tables 2 and 3). In order of importance, the five highest were the neurologist specializing in movement disorders, the clinical trials specialist, the gait and balance specialist, the physiatrist/physical therapist, and the neurosurgeon (Table 3). There were nine specialists who were considered to be important by at least one-half (i.e., 50%) of respondents. In addition to the five listed above, these included the dietician, speech pathologist, general neurologist, and psychiatrist (Table 3). The neurologist specializing in movement disorders was considered to be very important or essential by 91.0% of respondents vs. the general neurologist, who was considered as such by only 51.2% (Table 3).
Table 2. Respondents’ Ratings of the Potential Importance of Specialists in the Treatment of Patients with ET (Survey Question 3).
| Not Important | Only Slightly Important | Somewhat Important | Moderately Important | Very Important | Essential | |
|---|---|---|---|---|---|---|
| General neurologist | 45 (3.3) | 109 (7.9) | 233 (16.9) | 286 (20.7) | 403 (29.2) | 304 (22.0) |
| Neurologist specializing in movement disorders | 6 (0.4) | 16 (1.1) | 39 (2.8) | 67 (4.7) | 317 (22.4) | 971 (68.6) |
| Neurosurgeon | 43 (3.1) | 103 (7.4) | 168 (12.0) | 274 (19.6) | 388 (27.8) | 421 (30.1) |
| Psychiatrist | 79 (5.6) | 113 (8.0) | 228 (16.2) | 280 (19.9) | 389 (27.7) | 318 (22.6) |
| Hearing specialist | 291 (20.8) | 266 (19.0) | 291 (20.8) | 259 (18.5) | 198 (14.2) | 93 (6.7) |
| Someone who can evaluate you for memory problems | 169 (12.1) | 163 (11.7) | 243 (17.4) | 298 (21.3) | 332 (23.8) | 193 (13.8) |
| Physiatrist or physical therapist | 35 (2.5) | 83 (5.9) | 177 (12.5) | 249 (17.6) | 453 (32.0) | 421 (29.7) |
| Gait and balance specialist | 37 (2.6) | 77 (5.4) | 160 (11.3) | 258 (18.2) | 483 (34.1) | 402 (28.4) |
| Dietician | 67 (4.8) | 109 (7.8) | 184 (13.1) | 258 (18.4) | 433 (30.8) | 355 (25.3) |
| Speech pathologist | 95 (6.8) | 97 (7.0) | 193 (13.8) | 283 (20.3) | 412 (29.5) | 315 (22.6) |
| Social worker | 155 (11.1) | 159 (11.4) | 216 (15.5) | 279 (20.0) | 343 (24.6) | 244 (17.5) |
| Genetics counselor | 108 (7.7) | 180 (12.9) | 247 (17.7) | 305 (21.8) | 325 (23.3) | 233 (16.7) |
| Clinical trials specialist | 19 (1.4) | 66 (4.7) | 135 (9.6) | 222 (15.7) | 445 (31.5) | 524 (37.1) |
The number of respondents per row ranged from 1,380 to 1,418.
ET, Essential Tremor.
Table 3. Respondents’ Ratings of the Potential Importance of Specialists in the Treatment of Patients with ET (Survey Question 3).
| Not Important–Only Slightly– Somewhat Important | Moderately Important | Very Important–Essential | |
|---|---|---|---|
| Neurologist specializing in movement disorders | 61 (4.3) | 67 (4.7) | 1288 (91.0) |
| Clinical trials specialist | 220 (15.7) | 222 (15.7) | 969 (68.6) |
| Gait and balance specialist | 274 (19.3) | 258 (18.2) | 885 (62.5) |
| Physiatrist or physical therapist | 295 (20.9) | 249 (17.6) | 874 (61.7) |
| Neurosurgeon | 314 (22.5) | 274 (19.6) | 809 (57.9) |
| Dietician | 360 (25.7) | 258 (18.4) | 788 (56.1) |
| Speech pathologist | 385 (27.6) | 283 (20.3) | 727 (52.1) |
| General neurologist | 387 (28.1) | 286 (20.7) | 707 (51.2) |
| Psychiatrist | 420 (29.8) | 280 (19.9) | 707 (50.3) |
| Social worker | 530 (38.0) | 279 (20.0) | 587 (42.1) |
| Genetics counselor | 535 (38.3) | 305 (21.8) | 558 (40.0) |
| Someone who can evaluate you for memory problems | 575 (41.2) | 298 (21.3) | 525 (37.6) |
| Hearing specialist | 848 (60.6) | 259 (18.5) | 291 (20.9) |
The number of respondents per row ranged from 1,380 to 1,418.
In question 4, respondents were asked, “What do you find lacking in the treatment you receive for your tremor? What would you like to see happening during a doctor's visit that is not happening now?” The top 10 responses (Table 4) were a better educated doctor (16.4%), treatment is not effective enough (16.1%), need for more options and a feeling of being in control (13.7%), a detailed report and a more quantitative way of assessing tremor and tracking progression (12.7%), better counseling/management of current treatment and medications (11.9%), nothing is lacking from my ET treatment (11.8%), empathy, compassion and being heard (11.6%), a treatment approach other than just medications and surgery (11.2%), discussing and assessing all of my symptoms (mental, balance, etc.) aside from tremor (9.5%), and too rapid and/or superficial of an assessment (8.6%). A whole host of other issues were also raised (Table 4).
Table 4. Responses to Survey Question 4: “What Do You Find Lacking in the Treatment You Receive for Your Tremor? What Would You Like to See Happening during a Doctor's Visit That Is Not Happening Now?”.
| Response Category | Example (Sample Quotation from Respondents) | Number (%) of Patients Who Raised This Issue |
|---|---|---|
| A better educated doctor | “My experience has been that most primary care physicians seem to know very little about the condition.” | 201 (16.4) |
| Treatment is not effective enough | “A medication that reduced my tremor.” “Effective medicine.” |
198 (16.1) |
| Need for more options and a feeling of being in control | “I need more options about treatment and counseling.” | 168 (13.7) |
| A detailed report. A more quantitative way of assessing tremor and tracking progression | “I would have preferred a detailed report rather than 1 page with my diagnosis and meds.” “Method of quantitatively tracking progression of tremor and/or other ET symptoms.” “Some type of measurement or comparison to track progression.” “Objective measurement of tremor severity vs. last visit. Today, every measure is "subjective".” “Each time we see a doctor, we should be tested for worsening tremor, drawing lines, circles…” |
155 (12.7) |
| Better counseling/management of current treatment and medications | “Closer follow up and guidance when trying different meds.” | 146 (11.9) |
| Nothing is lacking from my ET treatment | “I receive good treatment at the university clinic from movement disorder specialists. I think they are doing all they can with the knowledge and treatments available.” “I’m happy with my neurologist. We have a very good team.” |
145 (11.8) |
| Empathy, compassion, being heard | “What do I think was lacking? Any real understanding of what it's like for the patient.” “Sympathetic discussion instead of 5 minute routine of what has happened since last visit.” “A true sense of caring, understanding.” |
142 (11.6) |
| A treatment approach other than just medications and surgery | “He did not talk to me about diet, research, other possible treatments (other than drugs & surgery).” “Discuss treatments for tremor rather just handing out pills.” |
138 (11.2) |
| Not currently receiving treatment | “I don’t receive treatment.” “No treatment at present.” |
131 (10.7) |
| Discussing and assessing all of my symptoms (mental, balance, etc.) aside from tremor | “Feeling less rushed and able to discuss all of the symptoms that are not being addressed…such as mental state, balance, hearing, memory, etc.” “The neurologists I have seen do not seem to have an adequate understanding of essential tremor. I would like to see a more complete diagnostic test—involving gait, tremor, memory—instead of the extremely basic tests used so far.” |
116 (9.5) |
| Too rapid and/or superficial of an assessment | “He does the ‘fly-by’ approach, hello, let me see your hands, raise them up, hold them out (you can’t tell much, I would rather he see me ‘actively’ hold something like a coffee mug) and then says see you again in six months.” “I am always asked to extend my hands and that is the basis for treatment. Would like to see a more extensive evaluation and treatment plan.” |
105 (8.6) |
| Better communication of knowledge to patient | “Education as my tremors increase. Knowledge reduces fear.” “Good communication between patient and doctor, questions asked and answered.” |
103 (8.4) |
| Better counseling of medication side effects. Side effects of treatment were not discussed | “Education on the side effects of taking additional medications.” | 72 (5.9) |
| Dealing with the psychological and emotional issues related to ET | “A deeper understanding of the emotional toll tremors have.” “More discussion to determine if the patient is depressed.” |
63 (5.1) |
| Prognostic information and dispelling fear for the future | “Information about what one can expect with ET.” “Hope for the future rather than fear.” “Explanation of what to expect in the future.” |
50 (4.1) |
| Movement disorders neurologist and/or a doctor with a specific interest in ET | “It took years to find the right medical team. A general neurologist should know when to quit and send the patient for proper assessment.” “MD's for the most part do not take it too seriously, but I finally got my Dr. to send a referral to a center for Movement disorders.” |
46 (3.7) |
| A doctor who gives advice | “A doctor who gives advice.” “More input from the doctor.” |
40 (3.3) |
| More information about new research findings | “No one seems to give me any information on new treatments or new research that has been done.” “Notification of emerging therapies.” |
38 (3.1) |
| A holistic approach to treatment | “Doctor relies on prescription drugs to mitigate ET challenges rather than alternatives such as acupuncture, massage, relaxation techniques.” “Right now we just monitor and medicate…I would like a holistic approach.” |
34 (2.8) |
| A better educated neurologist | “Currently, I am seeing a neurologist who doesn’t seem familiar with essential tremor.” “I have a general neurologist who doesn't seem to be able to answer my questions.” |
33 (2.7) |
| Physical therapy and help with balance and gait | “I wish a physical therapist had been part of the very frustrating and difficult process of calibration.” “It has never been suggested that I see someone about my balance or gait and I have fallen several times.” |
33 (2.7) |
| A list of services and coordinated care. Better coordination between primary care and neurological specialists | “Not totally familiar with the services offered by their department. A print out of services may have been helpful.” “Better coordination between primary care and neurological specialists.” “Would like to go to ONE doctor for everything or ONE place for everything. My neurologist treats the tremors with medication. I go to my regular MD to treat depression. I go to my eye doctor to treat the eye tremors. And I have nobody for the balance issues and the sleep issues.” |
29 (2.4) |
| Accuracy of diagnosis, second opinions | “I really have not been tested for tremors. Just had to draw a circle and then was told I have tremors. I would really like to know what I have.” “In this clinic, this condition does not seem to be recognized at all, although my doctor says it is ‘quite possible’ that my daughter, my sisters and I have a familial tremor. I would like a definite diagnosis.” |
29 (2.4) |
| Address dietary issues that relate to ET | “Ways to modify the diet to lessen tremor.” “Learning about how certain foods can affect tremors.” |
24 (2.0) |
| Social support and information about other people with ET, family support, support groups | “Acknowledgement that ‘you are not alone’.” “I would like to have doctors point out the tremor support groups that are available.” |
24 (2.0) |
| Help adjusting to work | “Understanding of how the tremor affects my work environment and responsibilities.” “Patients should receive a signed medical form/card that they may present to employers that explains what ET is with the endorsement of a doctor. This will help patients explain to employers that the tremor is not due to alcohol or other ominous reasons.” |
17 (1.4) |
| There is something wrong with the office/clinic environment | “Provide a place to rest after injections are given.” “Help filling in forms at front desk because of tremor!” “Drs. office is an artificial environment that doesn’t reproduce certain situations I experience.” |
16 (1.3) |
| More information about clinical trials and research that is currently recruiting | “I would like for the doctor to be more informed about any new ideas or clinical trials.” “Discuss knowledge of advances and clinical trials.” “A clinical trial specialist to inform me of any new treatments that are undergoing testing and where one can obtain the medication being tested.” |
16 (1.3) |
| Occupational therapy | “Occupational therapy, to assist in learning ways to cope.” “Something to help with writing, eating, or holding objects on bad days.” |
16 (1.3) |
| I feel pressure to have brain surgery | “My last appointment my Dr. simply asked if I was ready for brain surgery. He did not talk to me about diet, research, or other possible treatments.” | 15 (1.2) |
| Geographic constraints to accessing treatment | “I don’t even know who to see locally, and am too old with too many problems to travel far.” | 13 (1.1) |
| Speech therapy/help with voice tremors | “No one offered a speech pathologist and my voice is affected.” “Not only until recently did I realize that tremor was the likely cause of my speech struggles.” |
14 (1.1) |
| Confusion between ET and Parkinson’s disease or dystonia | “Separating Parkinson’s from ET.” “I have been frustrated because I have been diagnosed with ET and then dystonia, can’t get clear on what I have, and as a result can’t participate in clinical trials.” |
10 (0.9) |
| Dealing with problems with memory | “Primidone was ramped up until it about did me in. I ended up in a memory clinic.” “Memory problems.” |
11 (0.9) |
| Financial constraints to accessing treatment | “Tremors occur in common people, not only people with money, but the treatments seem to be out of reach for common people with average incomes.” “Ability to get a second opinion—this is an insurance problem.” |
11 (0.9) |
| Less of a “guessing game” (i.e., trial and error empiric approach to treatment) | “It seems to be a hit or miss attempt at ameliorating tremor.” “Try this one, then try that one.” |
8 (0.7) |
| Hearing problems | “No one has mentioned hearing problems to me—are/might they occur because of tremor?” | 5 (0.4) |
| Help for young patients | “My son has been to 3 different neurologists and because he is young, the neurologists just don’t seem to care about his quality of life or try different regimens.” | 5 (0.4) |
| Suggest products to buy that would help with tremor | “Information on assistive technology.” “Available items you can purchase to help you reduce your tremor.” |
2 (0.2) |
ET, Essential Tremor.
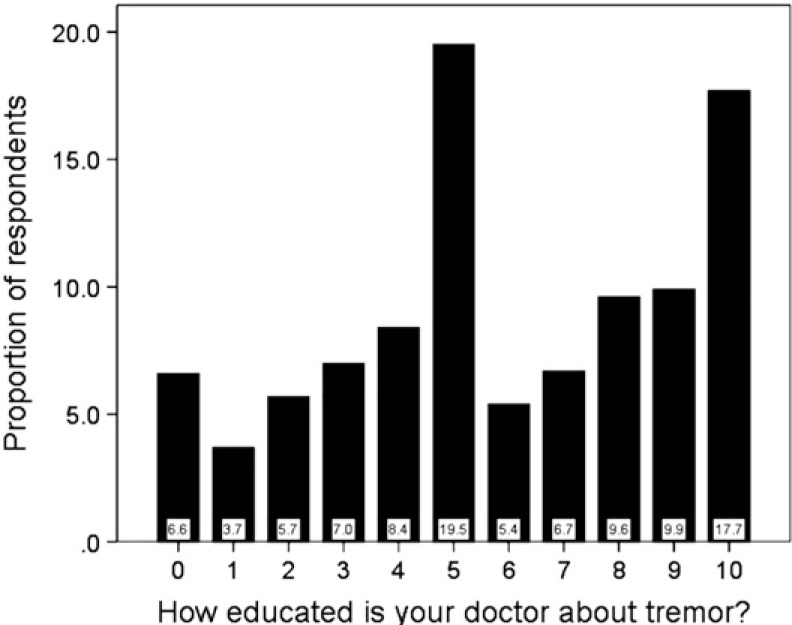
When asked how educated they felt their doctor was about tremor (i.e., question 6), 6.6% endorsed “not very well-educated”, 24.8% endorsed a value that was between “not very well-educated” and “moderately well-educated”, 19.5% endorsed “moderately well-educated”, 31.6% endorsed a value that was between “moderately educated” and “extremely well-educated”, and 17.7% endorsed “extremely well-educated” (Figure 1). Hence, 68.8% (approximately two in three) endorsed “moderately well-educated” or greater while 31.4% (approximately one in three) endorsed a response that was less than “moderately well-educated”.
Figure 1. Respondent’s Responses to the Question “How Educated Is Your Doctor about Tremor?” (Survey Question 6). Anchor points: 0 (not very well educated), 5 (moderately educated), 10 (extremely well educated).
Discussion
Patient-centered queries and their elicited feedback are expected to lead to improvements in the care of patients with chronic diseases.10 These efforts have been undertaken for patients with, for example, Parkinson’s disease (PD)8 or pediatric neurology patients.11 In this questionnaire, endorsed by more than 1,400 respondents with ET, we attempted to elicit and define the self-identified unmet needs and frustrations of ET patients. A number of revealing and useful responses were obtained.
When asked what they found lacking in their treatment (question 5), it is interesting to note that one of the top responses (16.1% of respondents) was that the current treatment (especially tremor medication) was not effective enough. This speaks to the limited efficacy of the currently available medications for ET and a reluctance of ET patients to undergo deep brain stimulation (DBS) surgery.12,13 The top response, endorsed by 16.4% of respondents, was that they wanted a more educated doctor. Indeed, when asked more specifically how educated they felt their doctor was about tremor (question 6), one in every three respondents (i.e., 31.4%) indicated that the doctor was not even “moderately well-educated”. This may reflect a low level of knowledge among general practitioners, internists, and even general neurologists about ET, its clinical nuances, and its associated features; the extraordinarily high level of misdiagnosis of ET (30–50% of cases)14,15 likely similarly reflects a general lack of knowledge about ET.
Many respondents indicated a desire to have a more detailed and quantitative assessment of their tremor during their visit to the doctor as well as a more stringent method for tracking its progression (Table 4). This was similar to the response that the assessment seemed too rapid, superficial and formulaic (Table 4). Indeed, although a number of rating scales exist to quantify tremor severity in patients with ET,16 at present, these are mainly used as research tools rather than metrics to track tremor in clinical practice.
Respondents raised a whole host of additional issues about their care (Tables 1 and 4), which speaks to the multiplicity of patient needs. Such a situation is optimally managed in a multidisciplinary care setting by physicians who are educated about and experienced in the issues that arise in the treatment of patients with ET. At present, specialty clinics exist for select neurological diseases (e.g., Huntington’s disease, ataxia), but not for tremor disorders as a group or more specifically for ET.
A large number of patients focused on the fact that the assessment was limited to a discussion of their tremor and that it did not delve into myriad other issues ranging from psychiatric problems to problems with gait and balance, to coping mechanisms (for performing daily activities). This in large measure reflects the more traditional view of ET, now challenged, that it is a monosymptomatic entity rather than a broad-spectrum clinical disorder characterized by a range of both motor and non-motor features.17 It further speaks to the notion, probably incorrect to some extent, that these additional issues in ET are mild or subclinical and therefore not meritorious of very much medical attention.
Respondents rated the importance of various specialists in their care, and the five highest were the neurologist specializing in movement disorders, the clinical trials specialist, the gait and balance specialist, the physiatrist/physical therapist and the neurosurgeon, yet there were nine specialists who were considered to be important by 50% or more respondents. Again, this speaks to the multiplicity of patient needs, many of which are unrecognized. When asked which problems aside from tremor would they focus attention on in an ideal clinical center, one in three respondents (i.e., 33.9%) asked for psychological services and support (Table 1) and a similar proportion (28.6%) requested occupational or physical therapy to aid in dealing with the effects of tremor on eating, preparing meals, and performing personal hygiene (Table 1).
This questionnaire may be used to begin to identify the different care aspects that are important to patients with ET. Such questionnaires, as has been the case in PD, may be used to identify areas for improved treatment; they may also serve as a useful metric to gauge patients’ satisfaction with their current treatment situation.8
These data, while unique, should be interpreted within the context of several limitations. First, one must consider the issue of ascertainment bias. The wording of the online posting was purposely designed as a general and somewhat non-specific request for information. A goal was to avoid enrolling only those patients who were under treatment yet dissatisfied with their treatment. Indeed, 11.8% of respondents were completely satisfied with their treatment (Table 4) and another 10.7% were not even under treatment (Table 4), suggesting that this strategy was somewhat successful. The second issue is whether the responses of this particular group of approximately 1,400 individuals are representative of all ET patients or of a group ascertained from another source. The fact that the sample size was so large and that there was such a heterogeneity of responses (e.g., a large number of categories of responses for several of the questions) suggests that a broad spectrum of opinions is represented. On the other hand, this was not a population-based sample either. However, the bulk of ET patients in the population do not seek treatment, so this is not a particularly relevant patient sample anyway. Third, we did not collect individual level data on age, gender, education, severity of tremor, and duration of tremor, so we are not able to determine the extent to which these factors influenced the results or correlated with the results. Future studies should examine these issues. Finally, we did not collect data on the psychometric properties of the questionnaire; indeed, we found that several of the questions elicited redundant responses. Therefore, there is room to improve the tool. It is possible that additional information could be elicited with a more refined version of this questionnaire.
In summary, patients with ET identified a broad range of issues that they felt were not being addressed in their current treatment situation, with only one in 10 patients reporting that they were satisfied with their current situation. It is hoped that efforts such as this, to obtain patient participation and feedback, will lead to improvements in the care of patients with this common and chronic neurological disease. In addition, future research would need to be performed to evaluate the feasibility and impact that such changes would have on the quality of care.
Appendix 1
Six-item essential tremor patient-centeredness questionnaire
What, in your opinion, are the major unmet needs in the treatment of patients with tremor?
If you were going to design a comprehensive approach/ideal clinical center for the treatment of tremor, which problems aside from tremor, would you focus attention on?
-
Please rate from 0 to 5 the potential importance of each of the following people in the treatment of patients with tremor:
(0 = not important, 1 = only slightly important, 2 = somewhat important, 3 = moderately important, 4 = very important, 5 = essential).- General Neurologist
- Neurologist Specializing in Movement Disorders
- Neurosurgeon—to inform you about surgical options for your tremor
- Psychiatrist or psychologist—to identify and/or treat depression or anxiety
- Hearing specialist—to evaluate your hearing
- Someone who can evaluate you for memory problems
- Physiatrist or physical therapist—to guide you about the available items you can purchase to help reduce your tremor (e.g., weighted spoons).
- A gait and balance specialist—to evaluate your walking and balance and to recommend exercises.
- Dietician—to provide guidance on ways to modify your diet to lessen your tremor.
- Speech pathologist - to discuss voice tremor.
- Social worker (someone who can help guide you with filling out disability paperwork.
- A genetics counselor—to discuss familial risks of tremor.
- A clinical trials specialist—to inform you of any new treatments that are undergoing testing.
What do you find lacking in the treatment you receive for your tremor? What would you like to see happening during a doctor’s visit that is not happening now?
What problems that tremor patients have that you feel are being ignored?
-
How well educated/informed is your doctor about tremor?
(Please rate from 0 to 10, with 0 = not very well educated, 5 = moderately well educated, 10 = extremely well informed).
Footnotes
Funding: E.D.L. has received research support from the National Institutes of Health: NINDS #R01 NS042859 (principal investigator), NINDS #R01 NS39422 (principal investigator), NINDS #R01 NS086736 (principal investigator), NINDS #R01 NS073872 (principal investigator), NINDS #R01 NS085136 (principal investigator), and NINDS #R01 NS088257 (principal investigator). This funding body played no role in the design of the study, the collection, analysis, and interpretation of data, or the writing of the manuscript.
Financial Disclosures: None.
Conflicts of Interest: The authors report no conflict of interest.
References
- 1.Louis ED, Ottman R. How many people in the USA have essential tremor? Deriving a population estimate based on epidemiological data. Tremor Other Hyperkinet Mov (NY) 2014;4:259. doi: 10.7916/D8TT4P4B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Louis ED, Ferreira JJ. How common is the most common adult movement disorder? Update on the worldwide prevalence of essential tremor. Mov Disord. 2010;25:534–541. doi: 10.1002/mds.22838. [DOI] [PubMed] [Google Scholar]
- 3.Putzke JD, Whaley NR, Baba Y, Wszolek ZK, Uitti RJ. Essential tremor: Predictors of disease progression in a clinical cohort. J Neurol Neurosurg Psychiatry. 2006;77:1235–1237. doi: 10.1136/jnnp.2006.086579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Louis ED, Agnew A, Gillman A, Gerbin M, Viner AS. Estimating annual rate of decline: Prospective, longitudinal data on arm tremor severity in two groups of essential tremor cases. J Neurol Neurosurg Psychiatry. 2011;82:761–765. doi: 10.1136/jnnp.2010.229740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rautakorpi I, Takala J, Marttila RJ, Sievers K, Rinne UK. Essential tremor in a Finnish population. Acta Neurol Scand. 1982;66:58–67. doi: 10.1111/j.1600-0404.1982.tb03129.x. [DOI] [PubMed] [Google Scholar]
- 6.Benito-León J, Bermejo-Pareja F, Morales JM, Vega S, Molina JA. Prevalence of essential tremor in three elderly populations of central Spain. Mov Disord. 2003;18:389–394. doi: 10.1002/mds.10376. [DOI] [PubMed] [Google Scholar]
- 7.Troster AI, Pahwa R, Fields JA, Tanner CM, Lyons KE. Quality of life in Essential Tremor Questionnaire (QUEST): Development and initial validation. Parkinsonism Relat Disord. 2005;11:367–373. doi: 10.1016/j.parkreldis.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 8.van der Eijk M, Faber MJ, Ummels I, Aarts JW, Munneke M, Bloem BR. Patient-centeredness in PD care: Development and validation of a patient experience questionnaire. Parkinsonism Relat Disord. 2012;18:1011–1016. doi: 10.1016/j.parkreldis.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 9.Galvin JE, Valois L, Zweig Y. Collaborative transdisciplinary team approach for dementia care. Neurodegener Dis Manag. 2014;4:455–469. doi: 10.2217/nmt.14.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fradgley EA, Paul CL, Bryant J, Roos IA, Henskens FA, Paul DJ. Consumer participation in quality improvements for chronic disease care: Development and evaluation of an interactive patient-centered survey to identify preferred service initiatives. J Med Internet Res. 2014;16:e292. doi: 10.2196/jmir.3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dooley JM, Gordon KE, Brna PM, et al. What do patients and families want from a child neurology consultation? J Child Neurol. 2014;29:1699–1703. doi: 10.1177/0883073813511857. [DOI] [PubMed] [Google Scholar]
- 12.Diaz NL, Louis ED. Survey of medication usage patterns among essential tremor patients: Movement disorder specialists vs. general neurologists. Parkinsonism Relat Disord. 2010;16:604–607. doi: 10.1016/j.parkreldis.2010.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Louis ED, Rios E, Henchcliffe C. How are we doing with the treatment of essential tremor (ET)? Persistence of patients with ET on medication: Data from 528 patients in three settings. Eur J Neurol. 2010;17:882–884. doi: 10.1111/j.1468-1331.2009.02926.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schrag A, Munchau A, Bhatia KP, Quinn NP, Marsden CD. Essential tremor: An overdiagnosed condition? J Neurol. 2000;247:955–959. doi: 10.1007/s004150070053. [DOI] [PubMed] [Google Scholar]
- 15.Jain S, Lo SE, Louis ED. Common misdiagnosis of a common neurological disorder: How are we misdiagnosing essential tremor? Arch Neurol. 2006;63:1100–1104. doi: 10.1001/archneur.63.8.1100. [DOI] [PubMed] [Google Scholar]
- 16.Elble R, Bain P, João Forjaz M, et al. Task force report: Scales for screening and evaluating tremor: Critique and recommendations. Mov Disord. 2013;28:1793–1800. doi: 10.1002/mds.25648. [DOI] [PubMed] [Google Scholar]
- 17.Benito-Leon J. Essential tremor: From a monosymptomatic disorder to a more complex entity. Neuroepidemiology. 2008;31:191–192. doi: 10.1159/000154933. [DOI] [PubMed] [Google Scholar]