Abstract
Purpose
We developed a method for quantifying intraoperative torsional forced ductions and validated the new test by comparing patients with oblique dysfunction and controls.
Design
Comparative case series
Subjects
We studied 33 eyes with oblique dysfunction (9 presumed congenital superior oblique palsy (SOP), 13 acquired SOP, 7 Brown syndrome, and 4 Inverted Brown syndrome) and 31 controls. We also studied maximal excyclorotation after superior oblique (SO) disinsertion in 6 eyes and maximal incyclorotation after inferior oblique (IO) disinsertion in 2 eyes.
Methods
Under deep general anesthesia, the 12 and 6 o’clock positions at the limbus were marked and the globe was maximally excyclorotated and incyclorotated without retroplacement until the first resistance was felt, and the angle of rotation (in degrees) was read on a Mendez ring by the surgeon. A photograph was taken in each position to be read by a masked observer.
Main outcome measures
Maximal excyclorotation and maximal incyclorotation in each oblique dysfunction and in controls, by both surgeon’s report and photographic assessment. We duplicated the photographs to evaluate test-retest reliability and to evaluate agreement between the surgeon’s assessments and photographic assessment.
Results
Surgeon’s assessment revealed greater maximal excyclorotation in presumed congenital SOP than controls (median, 40 degrees versus 30 degrees). Maximal excyclorotation in acquired SOP was similar to controls (30 degrees in both). Eyes with Brown syndrome and Inverted Brown syndrome had lower maximal excyclorotation than controls (10 degrees and 20 degrees versus 30 degrees, respectively). Maximal incyclorotation in inverted Brown syndrome was lower than controls (12.5 degrees versus 30 degrees) whereas it was similar to controls in presumed congenital SOP, acquired SOP and Brown syndrome (30 degrees in each condition). Median maximal excyclorotation after SO disinsertion was 62.5 degrees and maximal incyclorotation after IO disinsertion was 60 degrees. Photographic assessment yielded essentially identical findings to the surgeon’s report. Test-retest reliability of the photographic reading was excellent and agreement between the surgeon’s report and the photographic reading was also excellent (95% Limits of agreement; 4.4 and 11.6, Intraclass correlation coefficient; 0.97 and 0.82, respectively).
Conclusions
The new torsional forced duction test enables quantitative assessment of superior oblique and inferior oblique tightness and laxity.
Intraoperative assessment of tightness or laxity of the superior oblique tendon and inferior oblique muscle may be important for diagnosis and may provide essential information for surgical planning. In 1981, Guyton1 described a method for assessing superior oblique tightness during surgery and reported a grading system. Guyton’s method depends on the feeling of a ‘jump over the band’1 when rolling the globe back and forth over the stretched superior oblique tendon while gently pushing the globe into the orbit. Plager2 also described ‘traction testing in superior oblique laxity’, and also reported a grading scale.3 Nevertheless, both Guyton’s and Plager’s grading scales for tightness or laxity of oblique muscles are based on qualitative assessments and the scales are reported as ordinal values; 0 to +4 for superior oblique tightness,1 and −1 to −4 for superior oblique laxity.3 Kushner4 described comparing symmetry of excyclorotation and incyclorotation using a rotary forced duction test without quantification. Ludwig5, 6 described a torsional forced duction test estimating the amount of torsion but without describing a method of measurement.
We now describe a simple method to more precisely quantify superior and inferior oblique tightness or laxity by measuring the number of degrees of torsional movement possible during an intraoperative torsional forced duction test. In addition, we validated the new test by comparing the quantitative values obtained between patients with abnormal oblique muscles and controls.
Materials and Methods
Torsional Forced Duction Test
All measurements were performed under deep general anesthesia and before starting any surgical procedure. Nearly all patients (27 of 29 patients with abnormal oblique conditions and 21 of 31 control patients) received a short-acting depolarizing muscle relaxant (succinylcholine) and one control patient received a non-depolarizing muscle relaxant (rocuronium). If a short-acting depolarizing muscle relaxant was administered during induction, our test was performed at least 10 minutes after its administration when there should be no residual effect of a short-acting depolarizing muscle relaxant.7 A secondary analysis of controls with or without succinylcholine revealed essentially identical values (see below).
The 6 and 12 o’clock positions at the limbus were marked with a blue skin marking pen,8, 9 and a Mendez ring (Duckworth and Kent Ltd., Hertfordsire, UK, Product number 9-705R-1) was aligned with these reference marks and a photograph was taken (Fig 1A). The eye was then grasped at the limbus with 0.3 mm toothed forceps at the 2 and 8 o’clock positions (Fig 1A; Video clip 1) and the eye was excyclorotated while maintaining the natural anteroposterior axis without retropositioning the globe. When the first resistance was felt (which we defined as “maximal excyclorotation,” this angle was recorded by the surgeon (JMH) in degrees and a photograph was taken for later assessment by a masked reader (Fig 1B; Video clip 1). This procedure was repeated for maximal incyclorotation (Fig 1C; Video clip 1).
Figure 1. Torsional forced duction test illustrated in the left eye of a control patient.
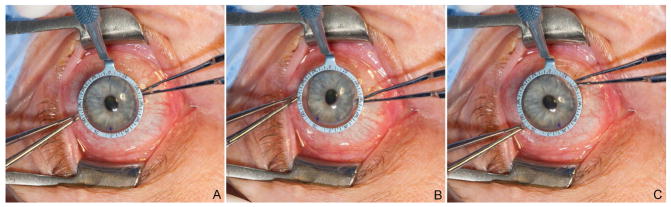
(A) Initial alignment of Mendez ring to limbal reference marks at 6 and 12 o’clock in the left eye (surgeon’s view). (B) Globe was maximally excyclorotated until the first resistance was felt, without replacement, and maximal excyclorotation was read as 30 degrees. (C) Globe was maximally incyclorotated until the first resistance was felt, without replacement, and maximal incyclorotation was read as 30 degrees.
Patients
We retrospectively studied patients with four abnormal oblique muscle conditions; 1) presumed congenital superior oblique palsy, 2) acquired superior oblique palsy, 3) Brown syndrome, and 4) suspected inverted Brown syndrome.10 Patients with a history of prior strabismus surgery, ocular trauma, or any restriction of the horizontal or vertical rectus muscles, based on standard intraoperative forced duction tests, were excluded, except for cases of suspected inverted Brown syndrome.
The four abnormal oblique muscle conditions were defined as follows. 1) presumed congenital superior oblique palsy (9 eyes from 9 patients, age 23 to 75 years) had a history of vertical strabismus or head tilt dating back to childhood with large vertical fusional amplitudes (>10 prism diopter). 2) acquired superior oblique palsy (13 eyes from 10 patients, age 62 to 82 years) had a history of severe head trauma (9 eyes from 6 patients), rheumatoid arthritis (1 eye from 1 patient), neuro-surgery (1 eye from 1 patient), or uncontrolled hypertension (2 eyes from 2 patients), and all had sudden onset of vertical or torsional double vision with normal fusion amplitudes and no evidence of pre-existing palsy. 3) Brown syndrome (7 eyes from 6 patients, age 29 to 78 years) had restriction of eye elevation in adduction and superior oblique tightness on intraoperative Guyton’s exaggerated forced duction test.1 4) suspected inverted Brown syndrome (4 eyes from 4 patients, age 70 to 73 years) had deficiency of depression particularly in adduction and positive inferior oblique tightness on intraoperative Guyton’s exaggerated forced duction test.10 Two of the patients with inverted Brown syndrome had a history of strabismus surgery; one patient had undergone superior oblique advancement for superior oblique palsy 13 years previously, and the other patient underwent superior rectus recession combined with inferior rectus resection 1 year previously.
We also evaluated thirty one patients as controls (age 8 to 77 years). These subjects had no restriction of any horizontal or vertical rectus muscles, had negative Guyton’s exaggerated forced duction tests for superior oblique or inferior oblique tightness or laxity, and were scheduled to undergo horizontal muscle surgery to correct purely horizontal strabismus. We randomly selected one eye from each control patient (n=31 eyes) for analysis.
We also measured maximal excyclorotation after complete superior oblique disinsertion, prior to reattachment, in 6 eyes (1 eye with presumed congenital superior oblique palsy, 1 eye with acquired superior oblique palsy, and 4 eyes with Brown syndrome). Finally, we also measured maximal incyclorotation after complete inferior oblique disinsertion, prior to reattachment, in 2 eyes (2 eyes with suspected inverted Brown syndrome).
Approval to conduct this retrospective study was obtained from the Institutional Review Board (IRB) of the Mayo Clinic. The study was conducted in a HIPPA-compliant manner, and the study conformed to the tenets of the Declaration of Helsinki. Since 2012, it has been our routine practice to perform the torsional forced duction test in every surgical patient as part of routine forced duction testing.
Analyses
We compared the median maximal excyclorotation of each oblique dysfunction conditions with controls, first based on the surgeon’s intraoperative report and second based on masked photographic assessment, where the reader of the photographs (JHJ) was unaware of the patient or control group. For the photographic assessments, maximal excyclorotation was calculated by subtracting the reading at baseline from the reading at the position of maximal excyclorotation. We similarly evaluated maximal incyclorotation.
All photographs were also duplicated and we evaluated test-retest reliability of the masked photographic assessment. In addition, we compared the surgeon’s intraoperative report with the photographic assessment, and evaluated agreement between the surgeon’s report and the photographic assessment. Only data from eyes with both surgeon’s intraoperative report and photographic assessments were used for the latter analysis, with unreadable or missing photographs excluded (n= 7 excluded of 120 possible pairs). Bland-Altman plots were constructed to analyze test-retest reliability of photographic assessment and agreement between surgeon’s report and photographic assessment. Half-width of the 95% limits of agreements (LOA) and intraclass correlation coefficients (ICC) were calculated.
Unpaired comparisons between groups were made using Wilcoxon rank sum tests, and paired comparisons were made using Wilcoxon signed-rank tests. Statistical analysis was performed using SAS program version 9.3 (SAS Institute, Cary, NC).
Results
Surgeon’s report
Patients with presumed congenital superior oblique palsy had greater maximal excyclorotation than controls (median, 40 degrees versus 30 degrees, p=0.003, Table 1, Fig 2A). Maximal excyclorotation in acquired superior oblique palsy was similar to controls (30 degrees in both, p=0.1, Table 1, Fig 2A). Patients with Brown syndrome and suspected inverted Brown syndrome had lower maximal excyclorotation than controls (10 degrees and 20 degrees versus 30 degrees, each p<0.002, Table 1, Fig 2A). Maximal excyclorotation after superior oblique disinsertion was greater than controls (62.5 versus 30 degrees, p<0.0001, Table 1, Fig 2A).
Table 1.
The surgeon’s intraoperative report and photographic assessment for oblique conditions and controls (median and quartile ranges, in degrees).
| Conditions | Maximal Excyclorotation | Maximal Incyclorotation | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Surgeon’s report | n | Photographic assessment | n | Surgeon’s report | n | Photographic assessment | n | |
| Controls | 30 (30–30) | 31 | 30 (25–30) | 26 | 30 (30–30) | 31 | 31 (28–36) | 29 |
| Presumed CSOP | *40 (30–40) | 9 | *34 (33–40) | 7 | 30 (30–30) | 8 | 30 (25–31) | 7 |
| Acquired SOP | 30 (30–30) | 13 | 29 (25–30) | 10 | *30 (30–30) | 13 | 30 (25–33) | 11 |
| Brown SD | *10 (10–20) | 7 | *10 (7–12) | 5 | *30 (15–30) | 5 | 30 (20–40) | 5 |
| Inverted Brown SD | *20 (12.5–27.5) | 4 | 24 (16–30) | 3 | *12.5 (10–20) | 4 | *21.5 (17.5–24) | 4 |
| SO-Dis | *62.5 (60–65) | 6 | *50 (50–56) | 3 | N/A | N/A | ||
| IO-Dis | N/A | N/A | *60 (60–60) | 2 | *58 (57–59) | 2 | ||
n: Number of eyes with available data, CSOP: Congenital superior oblique palsy, SOP: Superior oblique palsy, SO: Superior oblique, IO: Inferior oblique, N/A; Non applicable,
significantly different from controls (p<0.05) for the specific measurement in that condition.
Figure 2. Box plots of maximal excyclorotation and maximal incyclorotation in each oblique condition and controls based on surgeon’s report. Top and bottom of box represent upper and lower quartiles, and whiskers represented maximum and minimum values.

(A) Maximal excyclorotation was greater than controls in presumed congenital superior oblique palsy and superior oblique disinsertion, and lower than controls in Brown syndrome and inverted Brown syndrome. (B) Maximal incyclorotation was lower than controls in inverted Brown syndrome and greater than controls in inferior oblique disinsertion. In acquired SOP and Brown syndrome, the medians were the same as controls but the distributions were different. (*; Significantly different from controls (p<0.05), CSOP: Congenital superior oblique palsy, SOP: Superior oblique palsy, SO: superior oblique, IO: inferior oblique)
Regarding maximal incyclorotation, patients with suspected inverted Brown syndrome had lower maximal incyclorotation than controls (12.5 versus 30 degrees, p<0.0001, Table 1, Fig 2B), and maximal incyclorotation after inferior oblique disinsertion was greater than controls (60 versus 30 degrees, p=0.0002, Table 1, Fig 2B). Maximal incyclorotation of presumed congenital superior oblique palsy was similar to controls (30 degrees in both, p=0.09, Table 1, Fig 2B). Maximal incyclorotation in acquired superior oblique palsy and Brown syndrome were also similar to controls (median, 30 degrees in each, Table 1, Fig 2B), but the distributions were somewhat dissimilar yielding a statistical significant but clinically insignificant difference (p=0.03 and 0.008, Table 1, Fig 2B).
Regarding the effect of a short-acting depolarizing muscle relaxant (succinylcholine), maximal excyclorotation and maximal incyclorotation were similar in control patients who had, and who had not, received succinylcholine (medians, 30 versus 30 degrees and 30 versus 30 degrees, respectively).
Test-retest reliability of photographic assessment
Test-retest reliability of the photographic assessment represented on the Bland-Altman plots showed excellent test-retest reliability (Fig 3A). The mean difference (retest minus test) was −0.3 degrees, with half-width of the 95% limits of agreement of 4.4 degrees and intraclass correlation coefficient of 0.97 (95% confidence interval: 0.96 to 0.98).
Figure 3. Bland-Altman plots for test-retest reliability photographic assessment and agreement between surgeon’s intraoperative report and photographic assessment.
(A) Masked photographic assessment showed excellent test-retest reliability and similar variability for both large and small angles. Mean difference was −0.3 degrees and the half-width of the 95% limit of agreement was 4.4 degrees. (B) Agreement between surgeon’s intraoperative report and photographic assessment showed excellent test-retest reliability and similar variability for both large and small angles. Mean difference was −0.1 degrees and the half-width of the 95% limit of agreement was 11.6 degrees.
Comparison and agreement between surgeon’s report and photographic assessment
There was excellent agreement between surgeon’s report and photographic assessment. The mean difference (photographic assessment minus surgeon’s report) was −0.1 degree, with half width of the 95% limits of agreement of 11.6 degrees and intraclass correlation coefficient of 0.82 (95% confidence interval: 0.75 to 0.87, Fig 3B).
Photographic assessment
The findings of the photographic assessments were essentially identical to those of the surgeon’s assessment with greater maximal excyclorotation in cases of presumed congenital superior oblique palsy and superior oblique disinsertion, and reduced maximal excyclorotation in cases of Brown syndrome. Regarding maximal incyclorotation, the masked photographic readings were also essentially identical to the surgeon’s assessment. Maximal incyclorotation was lower than controls in suspected inverted Brown syndrome and greater than controls after inferior oblique disinsertion (Table 1).
Selected Case Example: Brown syndrome
A 78-year-old man underwent strabismus surgery for Brown syndrome in his right eye planning to recess the right superior oblique tendon. After deep general anesthesia, the new torsional forced duction test revealed only 8 degrees of the maximal excyclorotation in the right eye (Fig 4A and 4B). The right superior oblique was disinserted from the sclera, but maximal excyclorotation only improved to 30 degrees (Fig 4C) and Guyton’s exaggerated forced duction test suggested residual superior oblique fibers.1 Therefore, the superotemporal quadrant was re-explored, and a 1 mm band of residual posterior superior oblique tendon fibers were identified posteriorly (Fig 4D), which were then disinserted. The torsional forced duction test was repeated and maximal excyclorotation improved to almost 60 degrees (Fig 4E), which was consistent with an entirely disinserted superior oblique tendon. The Guyton’s exaggerated forced duction test at that time was entirely free, confirming disinsertion of the entire tendon. This case illustrated the clinical usefulness of our new torsional forced duction test.
Figure 4. Case example; Right Brown syndrome.
(A) Mendez ring was aligned to limbal reference marks in the right eye (surgeon’s view). (B) Torsional forced duction test showed markedly reduced excyclorotation compared with controls, measuring only 8 degrees. (C) In this case, the superior oblique tendon was isolated and disinserted from the sclera as part of a planned recession. Partial improvement in excyclorotation was observed, measuring 30 degrees (similar to controls), but we would have expected much greater maximal excyclorotation with a totally disinserted tendon. (D) The Superior temporal quadrant was re-explored and residual posterior fibers of the superior oblique tendon were identified still attached to the sclera (arrow). These residual fibers were then disinserted from sclera. (E) On disinsertion of all the superior oblique tendon fibers, the maximal excyclorotation increased to almost 60 degrees.
Discussion
Using our new quantitative torsional forced duction test, we found greater maximal excyclorotation in presumed congenital superior oblique palsy and lower maximal excyclorotation in Brown syndrome compared with controls. We also found reduced maximal incyclorotation in cases of suspected inverted Brown syndrome compared with controls. Photographic assessment showed excellent test-retest reliability and the surgeon’s report showed excellent agreement with photographic assessment.
Guyton’s exaggerated forced duction test has become an indispensable part of evaluating superior and inferior oblique tightness or laxity.1, 2 Nevertheless, quantification of Guyton’s test is based on a subjective feeling and is commonly represented as an ordinal scale from 0 to +4,1 or −1 to −4.3 In addition, the Guyton’s exaggerated forced duction test is not based on normal physiologic rotation, but it requires exaggerated retroplacement of the globe. In contrast, our new torsional forced duction test is quantitative, yielding a value in degrees and performed in a more physiologic field of rotation.
Kushner4 described a rotary forced duction test in the specific context of diagnosing superior oblique incarceration syndrome. He used symmetry or asymmetry between estimated maximal excyclorotation and maximal incyclorotation to establish the diagnosis of superior oblique incarceration. Nevertheless, Kushner did not specifically quantify his test or report normal values. In our quantitative test, values in one eye can be compared with control values and with values in the fellow eye. Our test also allows quantitative monitoring of stepwise effects during the surgical procedure, as described in our case example.
Ludwig and colleagues also studied maximal excyclorotation and maximal incyclorotation under general anesthesia.5,6 They reported that normal rotation in children was 60–70 degrees of excyclorotation and 60–70 degrees of incyclorotation, whereas in adults, both ranged from 20–60 degrees. Ludwig commented that decreased rotation in the torsional forced duction test may signify tightness of the oblique muscle or abnormal adhesion between extra- and intraconal tissues,5 and also reported that in patients with superior oblique weakness, the range of extorsion increased to 85–90 degrees.6 Nevertheless, they did not describe how they quantified the degree of rotation. In contrast to Ludwig’s test, our torsional forced duction test quantifies the amount of torsion using a Mendez ring and our test appeared to be much less variable in control subjects, with surgeon’s reported values ranging from 25 to 35 degrees of maximal excyclorotation and 30 to 35 degrees of maximal incyclorotation. One difference between our test and Ludwig’s test may be that the endpoint of our test is where the first resistance is felt.
Several previous investigators have developed methods to quantify the passive forced duction test for extraocular rectus muscles, in contrast to the oblique muscles.11–13 Stephens and Reinenke11 developed a perilimbal suction cup placed on the globe and attached to a force displacement transducer. Metz12 also developed a strain gauge force transducer, and Rosenbaum and Myer13 used spring dynamometer which measured the grams of force required to displace the eye from its rest position into the various fields of rotation of the globe. Nevertheless, these previous studies used custom-made instruments and were limited to evaluating rectus muscles. Our torsional forced duction test for obliques can be simply performed in the anesthetized patient using only a commercially available Mendez ring, 0.3 mm forceps, and a skin marking pen.
Our torsional forced duction test might be considered an extension of our previously reported method for monitoring intraoperative torsion using vertical limbal marks at 12 and 6 o’clock as described for vertical rectus transposition surgery strabismus surgery associated with thyroid eye disease.8, 9 McCall et al, 14 had also previously described monitoring torsion under general anesthesia based on 6 o’clock limbal mark.
From a practical clinical standpoint, our data suggests that the torsional forced duction test is useful in distinguishing between congenital superior oblique palsy and normal controls and between congenital superior oblique and acquired superior oblique palsy. Based on surgeon’s report, 5 of 9 (55.6%; 95% CI, 21.2% to 86.3%) cases of presumed congenital superior oblique palsy had a value of maximal excyclorotation above 35 degrees, which was the greatest value for controls or acquired superior oblique palsy. Nevertheless the test is not definitive for congenital SOP because not all cases of congenital SOP have a lax SO tendon. Our test is also helpful in establishing diagnosis of either Brown syndrome or inverted Brown syndrome. All 7 cases of Brown syndrome had lower maximal excyclorotation than the lowest values of excyclorotation for controls and all 4 cases of inverted Brown syndrome had lower maximal incyclorotation than the lowest values of incyclorotation for controls. Our data also support the use of our test to monitor the completeness of the intraoperative oblique muscles disinsertion from sclera, and as such, is a useful supplement to Guyton’s exaggerated forced duction test when confirming complete superior oblique or inferior oblique disinsertion. Our case illustration demonstrated the difference between partial superior oblique disinsertion and complete superior oblique disinsertion, which was critical for surgical success. In this way, our torsional forced duction test may help confirm the preoperative diagnosis and guide intraoperative surgical planning.
There are some limitations to our method. Although resistance to ocular torsion is usually determined by superior and/or inferior oblique muscle tightness or laxity, the test results can also be affected by rectus muscle tightness, and/or scarring around the muscles. Accordingly, our torsional forced duction test should be interpreted in the context of conventional forced duction tests of the rectus muscles, considering whether or not the rectus muscles are also tight and whether or not there is coexistent scarring. Anecdotally, we have found apparent superior oblique tightness in patients with thyroid eye disease associated with inferior rectus tightness, which may or may not revert to normal on disinsertion of the tight inferior rectus, depending on whether the superior oblique is also tight.8 In addition, we did not study test-retest reliability between two different surgeons performing the test on the same patient, and further study of this aspect of test-retest reliability is warranted. Nevertheless, agreement between surgeon’s intraoperative report and photographic assessment was excellent. Although we have used the term maximal rotation, it should be noted that the globe is rotated until the first resistance is felt, and not to the point of absolute maximal rotation.
Our torsional forced duction test is particularly useful in the diagnosis of congenital superior oblique palsy, Brown syndrome, inverted Brown syndrome and may guide intraoperative surgical planning in these conditions or when these conditions are suspected. Our torsional forced duction test is also useful in confirming complete or incomplete intraoperative disinsertion of the superior oblique tendon or inferior oblique muscle, and may help prevent unwanted surgical undercorrection when disinsertion or recession of the obliques are indicated.
Supplementary Material
Video of the torsional forced duction test performed in the right eye (surgeon’s view). The Mendez ring is initially aligned to limbal reference marks at 6 and 12 o’clock. The eye is grasped at the limbus with 0.3 mm toothed forceps, and the eye is excyclorotated while maintaining the natural anteroposterior position without pushing the eye into the orbit. When the first resistance is felt, the angle of maximal excyclorotation is recorded in degrees (30 degrees in this case). The test is repeated for maximal incyclorotation (35 degrees in this case).
Acknowledgments
Financial Support: Supported by National Institutes of Health Grant EY024333 (JMH), Research to Prevent Blindness, New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN. The funding organizations had no role in the design or conduct of this research.
Footnotes
Meeting Presentation: The work presented in this article was presented in parts as a paper presentation at the annual meeting of the American Association for Pediatric Ophthalmology and Strabismus in New Orleans, LA, March 28, 2015 and Association for Research in Vision and Ophthalmology in Denver, CO, May 4, 2015.
Conflict of Interest: The authors have no conflicts of interest to disclose other than grant support from the National Institutes of Health Grant EY024333 (JMH), Research to Prevent Blindness, New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Guyton DL. Exaggerated traction test for the oblique muscles. Ophthalmology. 1981;88:1035–40. doi: 10.1016/s0161-6420(81)80033-4. [DOI] [PubMed] [Google Scholar]
- 2.Plager DA. Traction testing in superior oblique palsy. J Pediatr Ophthalmol Strabismus. 1990;27:136–40. doi: 10.3928/0191-3913-19900501-08. [DOI] [PubMed] [Google Scholar]
- 3.Plager DA. Tendon laxity in superior oblique palsy. Ophthalmology. 1992;99:1032–8. doi: 10.1016/s0161-6420(92)31854-8. [DOI] [PubMed] [Google Scholar]
- 4.Kushner BJ. Superior oblique tendon incarceration syndrome. Arch Ophthalmol. 2007;125:1070–6. doi: 10.1001/archopht.125.8.1070. [DOI] [PubMed] [Google Scholar]
- 5.Ludwig IH. Principles and management of complex strabismus. In: Wilson ME, Saunders RA, Trivedi RH, editors. Pediatric Ophthalmology: Current Thought and a Practical Guide. Berlin: Springer; 2009. [Google Scholar]
- 6.Ludwig IH, Clark RA, Stager DR., Sr New strabismus surgical techniques. J AAPOS. 2013;17:79–88. doi: 10.1016/j.jaapos.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 7.Kopman AF, Zhaku B, Lai KS. The “intubating dose” of succinylcholine: the effect of decreasing doses on recovery time. Anesthesiology. 2003;99:1050–4. doi: 10.1097/00000542-200311000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Holmes JM, Hatt SR, Bradley EA. Identifying masked superior oblique involvement in thyroid eye disease to avoid postoperative A-pattern exotropia and intorsion. J AAPOS. 2012;16:280–5. doi: 10.1016/j.jaapos.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holmes JM, Hatt SR, Leske DA. Intraoperative monitoring of torsion to prevent vertical deviations during augmented vertical rectus transposition surgery. J AAPOS. 2012;16:136–40. doi: 10.1016/j.jaapos.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Awadein A, Pesheva M, Guyton DL. “Inverted Brown pattern”: a tight inferior oblique muscle masquerading as a superior oblique muscle underaction--clinical characteristics and surgical management. J AAPOS. 2006;10:565–72. doi: 10.1016/j.jaapos.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 11.Stephens KF, Reinecke RD. Quantitative forced duction. Transactions - American Academy of Ophthalmology & Otolaryngology. 1967;71:324–9. [PubMed] [Google Scholar]
- 12.Metz HS. Quantitative evaluation of the strabismus patient. Int Ophthalmol Clin. 1985;25:13–36. doi: 10.1097/00004397-198502540-00004. [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum AL, Myer JH. New instrument for the quantitative determination of passive forced traction. Ophthalmology. 1980;87:158–63. doi: 10.1016/s0161-6420(80)35265-2. [DOI] [PubMed] [Google Scholar]
- 14.McCall LC, Isenberg SJ, Apt L. The effect of torsional muscle dysfunction and surgery on eye position under general anesthesia. J Pediatr Ophthalmol Strabismus. 1993;30:154–6. doi: 10.3928/0191-3913-19930501-06. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video of the torsional forced duction test performed in the right eye (surgeon’s view). The Mendez ring is initially aligned to limbal reference marks at 6 and 12 o’clock. The eye is grasped at the limbus with 0.3 mm toothed forceps, and the eye is excyclorotated while maintaining the natural anteroposterior position without pushing the eye into the orbit. When the first resistance is felt, the angle of maximal excyclorotation is recorded in degrees (30 degrees in this case). The test is repeated for maximal incyclorotation (35 degrees in this case).




