Abstract
The Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007) is a self-report assessment of anxiety sensitivity, reflecting one’s tendency to misinterpret the meaning of anxiety-relevant sensations. Despite this construct being related to a wide array of clinically-significant smoking maintenance and relapse processes, the psychometric properties of scores on the ASI-3 have not yet been investigated for use among smokers. Therefore, the current study aimed to test the psychometric properties of the scores on the ASI-3 in a sample of cigarette smokers. Participants were treatment-seeking daily smokers who completed the ASI-3 at a pre-cessation visit (Time 1: n = 464) and three-months post-cessation attempt (Time 2: n = 137). Confirmatory factor analyses results of the scores on ASI-3 at Time 1 and Time 2 revealed the hypothesized three-factor model, including physical, social, and cognitive concerns. Additionally, the ASI-3 factor scores evidenced factor stability, test-retest reliability, internal consistency, convergent, discriminant, and predictive validity. The present study provides evidence in support of the validity and reliability of scores on the ASI-3 as a measure of anxiety sensitivity among treatment-seeking cigarette smokers.
Keywords: anxiety sensitivity, ASI-3, confirmatory factor analysis, cigarette smoking
The expectancy model of fear posits that, in the context of personal threat, anxiety sensitivity marks the extent to which one attends to, and perceives, anxiety-relevant sensations as harmful, dangerous, and indicative of catastrophic consequences across domains (physical, social, and cognitive concerns; Reiss & McNally, 1985). Anxiety sensitivity is a risk factor for the acquisition and maintenance of psychopathology, primarily anxiety and mood disorders (Olatunji & Wolitzky-Taylor, 2009).
Research over the past decade has convincingly indicated that this construct may serve as a central explanatory mechanism in substance use disorders; perhaps, best illustrated in the case of cigarette smoking (Leventhal & Zvolensky, in press). Anxiety sensitivity may be particularly relevant to smokers given that health consequences of smoking (e.g., Goodwin et al., 2012) may potentiate the salience of negative interoceptive experiences. Specifically, anxiety sensitivity is associated with affect-regulatory smoking expectancies and motives for use (e.g., Farris, Leventhal, Schmidt, & Zvolensky, in press) and various aspects characterized by psychological inflexibility (e.g., Zvolensky, Farris, Schmidt, & Smits, 2014). Anxiety sensitivity appears to also be related to increases in positive affect after cigarette use (Wong et al., 2013) and reductions in subjective anxiety after stressful experiences (Perkins, Karelitz, Giedgowd, Conklin, & Sayette, 2010). Moreover, anxiety sensitivity also impacts the process of quitting, including the experience of more severe nicotine withdrawal (e.g., Johnson, Stewart, Rosenfield, Steeves, & Zvolensky, 2012) and risk for cessation failure (Assayag, Bernstein, Zvolensky, Steeves, & Stewart, 2012).
The most recent published measure, the 18-item Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007), was designed, in part, based on previous measures of anxiety sensitivity (Reiss, Peterson, Gursky, & McNally, 1986; Taylor & Cox, 1998). Psychometric tests of the ASI-3 have consistently yielded a three-factor model of anxiety sensitivity, including physical, cognitive, and social concerns (Bernstein et al., 2010; Ebesutani, McLeish, Luberto, Young, & Maack, 2014; Stellman et al., 2008; Taylor et al., 2007). Although the ASI-3 has been validated among clinical (anxiety disordered) and non-clinical samples (Escocard, Fioravanti-Bastos, & Landeira-Fernandez, 2009; Kemper, Lutz, Bähr, Rüddel, & Hock, 2012; Osman et al., 2010; Wheaton, Deacon, McGrath, Berman, & Abramowitz, 2012), none of these past studies assessed for, or screened on the basis of, smoking behavior. Thus, the psychometric properties of scores on the ASI-3 have not yet been investigated for use among smokers. To address this matter, the current study examined the factor structure, factor structure stability, reliability, and validity of scores on the ASI-3 measure among treatment-seeking adult daily cigarette smokers.
Method
Participants and Procedure
Adult daily smokers (N = 464; 48.2% female; Mage = 37.4, SD = 13.40) were recruited from the community to participate in a larger randomized control trial examining the efficacy of two smoking cessation interventions (clinicaltrials.gov #NCT01753141). Participants eligible for inclusion in the current study were between 18–65 years old who reported smoking ≥ 8 cigarettes per day, with motivation to quit rated as at least 5 or higher on a 10-point scale. Individuals responding to study advertisements were scheduled for an in-person, baseline assessment. After providing written informed consent, participants were interviewed using the Structural Clinical Interview of DSM-IV Disorders (SCID-I/NP; First, Spitzer, Gibbon, & Williams, 2007) and completed a computerized battery of baseline (pre-treatment) self-report questionnaires. Eligible participants were then randomly assigned to one of two 4-session smoking cessation treatment programs (described elsewhere; Farris, Zvolensky, DiBello, & Schmidt, in press). Follow-up data were collected at various time points post-quit attempt. All participants provided written informed consent prior to participation and the study protocol was approved by the Institutional Review Boards at the University of Vermont and Florida State University, where the study was conducted. For the current psychometric investigation, data from two time points (Baseline/Time 1; Month 3 post-cessation attempt/Time 2) were utilized.
At baseline, 464 cases were retained for analyses at Time 1 (i.e., those who provided complete baseline data for variables in the current study, regardless of parent study eligibility). Of the 464 cases, 398 were deemed eligible and were randomized to treatment (Panic-Smoking Prevention Program [n = 223, 56.0%] and Smoking Cessation Program [n = 175, 44.0%]. Of those randomized, 137 provided complete data at Month 3 post-quit attempt (Time 2).1 At Time 1, the average daily smoking rate of this sample was 17.8 (SD = 9.60), with participants reporting regular daily smoking for 19.1 years (SD = 13.29); smoking heaviness index averaged 3.0 (SD = 1.41; possible range 0–6 on the Fagerström Test for Nicotine Dependence [FTND]). Self-reported tobacco-related medical problems were reported among 29.9% of the sample. Regarding Axis I psychopathology, 42.5% of the sample met criteria for a past year (current) diagnosis. At Time 2, the self-reported rate of smoking was 4.4 cigarettes per day (SD = 7.26; range 0–40), with a mean smoking heaviness index of 2.1 (SD = 1.22).
Measures
The Anxiety Sensitivity Index-3 (ASI-3; Taylor et al. 2007) is an 18-item self-report used to assess concern associated with possible negative consequences of anxiety-related symptoms (e.g., “It scares me when my heart beats rapidly”). The scale includes some items from the original ASI (Reiss et al., 1986). Responses are rated on a 5-point Likert scale ranging from 0 (very little) to 4 (very much) and summed to create total score.
Descriptive Measures
The Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-I/NP; First et al., 2007) is a clinician-administered structured diagnostic assessment of past year Axis I psychopathology. Assessments were administered by trained research assistants or doctoral level staff. The Smoking History Questionnaire (Brown, Kahler, Zvolensky, Lejuez, & Ramsey, 2001) is a self-report questionnaire used to assess smoking history (e.g., onset of regular daily smoking), pattern (e.g., number of cigarettes consumed per day), and quit history.
Convergent and Discriminant Validity
The Anxiety Sensitivity Index (ASI; Reiss et al., 1986) is the original 16-item measure of anxiety sensitivity; with five items that overlap with the ASI-3. The total sum score was used as a test of convergent validity (internal consistency of items was α = .93). The Body Vigilance Scale (BVS; Schmidt, Lerew, & Trakowski, 1997) is a four-item self-report measure of the extent to which one focuses on internal bodily sensations. Items are summed to derive a total score. This measure has strong psychometric properties (Schmidt et al., 1997); internal consistency of items was α = .81. The Inventory of Depression and Anxiety Symptoms (IDAS; Watson et al., 2007) is a 64-item self-report measure of symptoms of major depression and related anxiety symptoms, with strong psychometric properties (Watson et al., 2007). The Panic subscale (eight items) was used for a test of convergent validity, as this subscale taps anxious arousal, the tendency to experience physiological arousal associated with anxiety (Watson et al., 2007). The IDAS-Well-Being subscale (eight items) indexes positive affective states, which was used to assess discriminant validity. Internal consistency was α = .88 for the IDAS-Panic subscale items and α = .91 for the IDAS-Well-Being subscale items. The Positive and Negative Affect Scale (PANAS; Watson, Clark, & Tellegen, 1988) is a 20-item self-report measure of broad negative and positive affect. The PANAS has strong documented psychometric properties (Watson et al., 1988). The negative and positive affect scales were used to assess convergent and discriminant validity, respectively. Internal consistency for the subscale items were α = .90 (Positive affect) and α = .91 (Negative affect).
Predictive Validity
The Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991) is a six-item scale that assesses gradations in tobacco dependence. The FTND items have adequate psychometric properties (Heatherton et al., 1991). A smoking heaviness index was derived from two items – “How many minutes after you wake do you smoke your first cigarette” and “How many cigarettes a day do you smoke” (Etter, Vu Duc, & Perneger, 1999); this was assessed at Time 1 and Time 2 for test of predictive validity.
Data Analytic Plan
The factor structure at Time 1 was examined using structural equation modeling (Confirmatory Factor Analysis; CFA). A single-factor and three-factor model were analyzed. Analyses were conducted using Mplus version 7.1 (Muthén & Muthén, 1998–2012). A second CFA was conducted using data collected at Time 2 to confirm the factor structure. Factor stability was assessed by first assessing measurement invariance according to Meredith (1993), by examining whether factor loadings (i.e., weak invariance), and then factor intercepts (i.e., strong invariance) held. Following this, within-factor paths were examined across Time 1 and Time 2 using the best-fitting model. Cronbach’s alpha was used to document internal consistency of factor items. Inter-correlations were computed to assess test-retest reliability of factor scores. Zero-order correlations were computed between the ASI-3 factor scores at Time 1 in relation to the relevant measures at Time 1. Path modeling in Mplus was used to assess the predictive validity of the ASI-3 factor scores at Time 1 and Time 2 in terms of smoking characteristics.
Robust Maximum Likelihood (MLR) was employed as the estimation method; indicators loaded on their underlying factors and inter-factor correlations were allowed. Their corresponding measurement errors were estimated as well. Based on the original measure validation (Taylor et al., 2007), each item was constrained to load onto one factor. With respect to model fit, several tests were used to evaluate the models. First, the overall model Yuan-Bentler adjusted χ2 (e.g., Bollen, 1989) was used. Generally, a non-significant chi-square test, leading to non-rejection of the model, would suggest a relatively good approximation of the data. Second, the model fit was evaluated using the Root Mean Square Error of Approximation with values of .00 to .05 indicating excellent fit, values of .06–.08 indicating reasonable fit, and values about .10 suggesting poor fit (RMSEA; Browne & Cudeck, 1993). The Comparative Fit Index (CFI; Bentler, 1990) and the Tucker-Lewis Index were also used, with values greater than .90 as indicative of good fit (TLI; Hu & Bentler, 1999). Finally, because the CFA models and the models of measurement invariance were nested models, we evaluated comparative model fit using the χ2 difference test and the Akaike information criterion (AIC) with a non-significant χ2 indicating better fit for the more parsimonious model and smaller AIC values indicating better fit (Kline, 2011).
Results
Confirmatory Factor Analysis
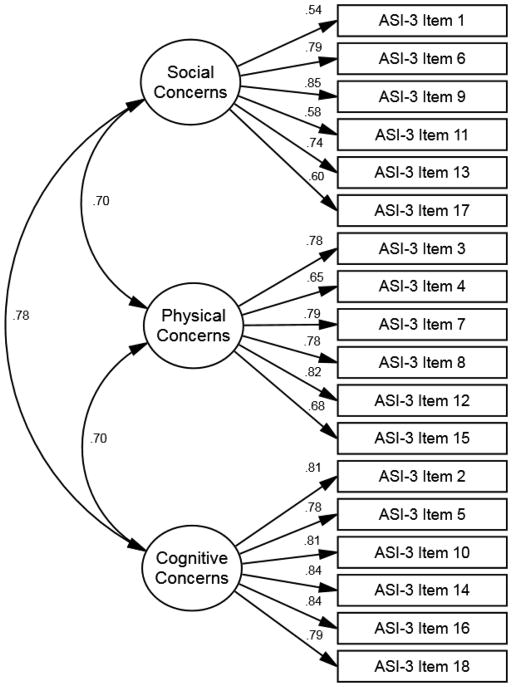
First, a single-factor model was fit to the data. The model was statistically significant χ2(135, n = 464) = 799.40, p < .01. Overall, the results indicated poor model fit (RMSEA =.10, CI90% = .10–.11; CFI = .80; TLI = .78). Based on the poor fit the single-factor was rejected. Next, the three-factor model was fit to the data (Taylor et al., 2007). The model and results are shown in Figure 1. The model was statistically significant χ2(132, n = 464) = 335.29, p < .01. Furthermore, this model evidenced adequate fit (RMSEA =.06, CI90% = .05–.07; CFI = .94; TLI = .93). Using the nested chi-square difference test, results indicated that the three-factor model improved the model significantly relative to the single-factor model, χ2 (3) = 219.56, p < .001. Additionally, the three-factor model produced a lower Akaike’s Information Criterion (AIC) value than the single-factor solution (AICs = 18928, 19624 respectively). Next, ASI-3 data from Time 2 was used to examine the three-factor model. Consistent with Time 1, the model was significant, χ2(132, n = 137) = 171.04, p < .05. The model evidenced good fit (RMSEA =.05, CI90% = .02–.07; CFI = .96; TLI = .95). See Figure 1 in supplement.
Figure 1.
Three-factor model for Time 1
Note. Path estimates are standardized regression weights. All path estimates are significant at p < .001
Test of Factor Structure Stability
Weak measurement invariance (i.e., equal factor loadings) was achieved (χ2 (15) = 9.71, p = .84), as was strong invariance (i.e., equal intercepts; χ2 (15) = 37.48, p = .16); see supplement Figure 2. Within-factor paths across Time 1 and Time 2 CFA models were tested (as in Berninger et al., 2010). Each of the ASI-3 factor items exhibited high levels of stability as estimated by the values of the within-factor paths across Time 1 and Time 2 for the CFA. The path effects for each factor were as follows: ASI-3 Physical concerns factor (β = .73), ASI-3 Social concerns factor (β = .82), and ASI-3 Cognitive concerns factor (β = .65); all p’s < .001.
Reliability: Internal Consistency and Test-retest
Reliability tests are presented in Table 1. Results revealed high internal consistency at Time 1 and Time 2 for the all ASI-3 factor items. For test-retest reliability, inter-correlations from Time 1 to Time 2 for all of the ASI-3 factor scores were statistically significant.2
Table 1.
Psychometric Statistics for the ASI-3
| Variable | Mean (SD) | ASI-3 Physical | ASI-3 Cognitive | ASI-3 Social |
|---|---|---|---|---|
| Reliability | ||||
| Internal Consistency (α) | -- | .881 | .920 | .842 |
| Test-Retesta (r) | -- | .702* | .600* | .815* |
|
| ||||
| Convergent Validity (r) | ||||
|
| ||||
| Anxiety Sensitivity Indexb | 18.0 (11.26) | .80* | .74* | .72* |
| Anxious Arousalc | 11.1 (4.24) | .54* | .50* | .49* |
| Body Vigilanced | 12.1 (7.70) | .44* | .29* | .31* |
| Negative Affecte | 19.1 (7.31) | .50* | .62* | .60* |
|
| ||||
| Discriminant Validity (r) | ||||
|
| ||||
| Positive Affectf | 32.2 (7.36) | −.20* | −.31* | −.28* |
| Well-Beingg | 22.6 (6.70) | −.21* | −.29* | −.29* |
|
| ||||
| Predictive Validity | Outcome β (SE) | |||
|
| ||||
| Predictor | ASI-3 Physical | ASI-3 Cognitive | ASI-3 Social | |
|
|
||||
| Genderh | −.01 (.39) | −.02 (.32) | −.07 (.40) | |
|
|
||||
| Axis I Psychopathologyi | .12 (.42)* | .15 (.35)* | .15 (.43)* | |
| Medical Problemsj | .10 (.41)* | −.05 (.35) | −.05 (.43) | |
| Negative Affect | .45 (.03)* | .58 (.02)* | .55 (.03)* | |
|
|
||||
| Predictor | Time 1 Smoking Heaviness Index k | |||
|
|
||||
| Gender | −.07 (.05) | |||
| Medical Problems | −.01 (.05) | |||
| Axis I Psychopathology | .05 (.05) | |||
| Negative Affect | −.10 (.06) | |||
| ASI-3 Physical | .17 (.07)* | |||
| ASI-3 Cognitive | .02 (.08) | |||
| ASI-3 Social | −.05 (.07) | |||
|
|
||||
| Predictor | Time 2 Smoking Heaviness Index | |||
|
|
||||
| Smoking Heaviness Time 1 | .66 (.06)* | |||
| Treatment Conditionl | .04 (.11) | |||
| ASI-3 Physical | .25 (.09)* | |||
| ASI-3 Cognitive | .03 (.11) | |||
| ASI-3 Social | −.10 (.12) | |||
p < .05;
Test-retest of Time 1- Time 2;
Anxiety Sensitivity Index (ASI);
Inventory of Depression and Anxiety Scale (IDAS-Panic subscale);
Body Vigilance Scale (BVS);
Positive and Negative Affect Scale (PANAS-Negative Affect subscale);
Positive and Negative Affect Scale (PANAS-Positive Affect subscale);
Inventory of Depression and Anxiety Scale (IDAS-Well-Being subscale);
Gender (coded 0 = male; 1 = female);
Axis I psychopathology (past year, per SCID-I/NP; coded 0 = no disorder, 1 = disorder);
Tobacco-related medical problems (coded 0 = no, 1 = yes);
FTND Heaviness Index (FTND items 1 and 2);
Treatment condition (coded 0 = standard, 1 = anxiety-focused). Test of predictive validity was tested simultaneously in one predictive model.
Validity: Convergent, Discriminant, and Predictive
Tests of convergent, discriminant and predictive validity are presented in Table 1. All ASI-3 factor scores were positively associated with Time 1 scores on measures of anxiety sensitivity (per ASI), anxious arousal, body vigilance, and negative affect. All ASI-3 factor scores were significantly and negatively correlated with positive affect, indexed by two different measure scores. Regarding tests of predictive validity, a path model was constructed to examine the ASI-3 factor scores (allowed to correlate) in terms of predicting smoking heaviness at Time 1 and Time 2. Gender, presence of tobacco-related medical problems, presence of past-year psychopathology3, and trait negative affect were entered as covarying predictors of the ASI-3 factors and Time 1 smoking heaviness index. Time 1 smoking heaviness and treatment condition were entered as predictors of Time 2 smoking heaviness index. Model fit was good [χ2(14) = 28.46, p = .012; RMSEA =.05,;CI90% = .02–.07; CFI = .98; TLI = .96). Results indicated that only ASI-3 Physical concerns scores were predictive of smoking heaviness at Time 1 (β = .17, p = .014) and at Time 2 (β = .25, p = .005).
Discussion
The test of the factor structure revealed a three-factor solution was the strongest fit to the data, relative to a one-factor model. This was true of data collected at two time points, approximately four months apart. Thus, at least among treatment-seeking smokers, it appears that the lower-order constituent factors scores of the ASI-3 remain consistent across time. Moreover, follow-up reliability testing of the identified ASI-3 factors scores revealed high internal consistency for all factor scores across both time points. These results are consistent with findings in non-smoking samples (Ebesutani et al., 2014; Taylor et al., 2007). Additionally, the ASI-3 factor scores demonstrated adequate test-retest reliability. Importantly, findings indicate that reductions in anxiety sensitivity were observed across all ASI-3 factor scores from Time 1 to Time 2. As such, these data document the stability of factor structure and measure reliability at both time points, regardless of intervention or acute smoking abstinence status.
Findings also support the convergent validity of the ASI-3 factor scores in terms of other anxiety sensitivity indices, anxious arousal, body vigilance and negative affectivity, and divergent validity evidenced by negative associations of ASI-3 factor scores and positive affectivity scores. Physical concerns about anxiety-relevant sensations emerged as a unique predictor of smoking heaviness at both time points, after adjusting for relevant covariates. In particular, mis(interpreting) the meaning of bodily sensations may specifically pose as a barrier for actual cessation, given high anxiety sensitive smokers tend to expect interoceptive/somatic threat during acute smoking abstinence (Farris, Langdon, DiBello, & Zvolensky, in press).
A few limitations should be considered. First, study attrition should be considered when interpreting test-retest indices. Additionally, given the participants in the sample were undergoing a cessation attempt, and changes in anxiety sensitivity were observed (footnote 2), this test of reliability may not be the strongest test of measure stability, thus warranting replication to determine the generalizability of these findings. Second, the psychometric properties (e.g., factor structure) could not be tested at Time 2 by smoking abstinence status given small sample size at that time point. Last, reductions in ASI-3 scores were reported for primarily descriptive purposes (footnote 2), however, the reason for these reductions were not explicitly tested here (beyond the scope of this investigation).
There is overwhelming evidence that documents the role of anxiety sensitivity in terms of various aspects of cigarette smoking (Leventhal & Zvolensky, in press). Findings here support the validity and reliability of scores on the ASI-3 as a measure of anxiety sensitivity among treatment-seeking cigarette smokers, and suggest that the multidimensional nature of anxiety sensitivity is particularly important to consider among smokers (i.e., constructs had differential predictive effects).
Supplementary Material
Acknowledgments
This work was funded by a National Institute of Mental Health grant awarded to Drs. Michael J. Zvolensky and Norman B. Schmidt (R01-MH076629-01A1). Ms. Farris is supported by a pre-doctoral National Research Service Award from the National Institute of Drug Abuse (F31-DA035564). Please note that the content presented does not necessarily represent the official views of the National Institutes of Health, and that the funding sources had no other role other than financial support.
Footnotes
Given the difference in sample size between Time 1 and Time 2 points (in part due to non-eligible participants being excluded and part due to study attrition), group differences were examined in terms of baseline factors. First, a series of t-tests indicated that those who were randomized and provided Time 2 data (n = 137) versus those who did not (n = 261), did not significantly differ in terms of prior number of lifetime quit attempts, or baseline levels of nicotine dependence, expired carbon monoxide, negative or positive affectivity, panic or depressive symptoms (all p’s > .05). Additionally, those who provided Time 2 data versus those who did not were not significantly different in terms of Time 1 ASI-3 factor scores (all p’s > .05). A chi-square test also indicated that there were no sex differences in those who provided Time 2 data [x2(1) = 1.240, p = .265], and the presence of anxiety or/depressive psychopathology at Time 1 did not statistically differ between those participants who provided Time 2 data (n = 41, 29.9% with psychopathology) versus those who did not (n = 91, 34.9%); [x2(1) = 989, p = .320].
A paired-sample t-test revealed a significant reduction in ASI-3 factors scores from Time 1 to Time 2: Physical concerns [M = 4.2 (SD = 4.54) vs. M = 2.8 (SD = 3.57), t = 4.89, p < .0001], Social concerns [M = 7.0 (SD = 4.90) vs. M = 5.5 (SD = 5.00), t = 4.94, p < .0001], and Cognitive concerns [M = 3.1 (SD = 4.19) vs. M = 2.2 (SD = 3.59), t = 2.89, p = .005].
Table 1 in supplement includes means, standard deviations, and test of groups differences by ASI-3 subscales for gender (male versus female), presence of past-year psychopathology (versus no disorder; anxiety psychopathology versus no anxiety psychopathology), and presence of tobacco-related disease (versus no self-reported tobacco-related disease).
No authors have any conflicts of interests or financial disclosures to report.
Contributor Information
Samantha G. Farris, University of Houston
Angelo M. DiBello, University of Houston
Nicholas P. Allan, Florida State University
Julianna Hogan, University of Houston.
Norman B. Schmidt, Florida State University
Michael J. Zvolensky, University of Houston and University of Texas MD Anderson Cancer Center
References
- Assayag Y, Bernstein A, Zvolensky MJ, Steeves D, Stewart SS. Nature and role of change in anxiety sensitivity during NRT-aided cognitive-behavioral smoking cessation treatment. Cognitive Behaviour Therapy. 2012;41(1):51–62. doi: 10.1080/16506073.2011.632437. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berninger A, Webber MP, Cohen HW, Gustave J, Lee R, Niles JK, Kelly K. Trends of Elevated PTSD Risk in Firefighters Exposed to the World Trade Center Disaster: 2001–2005. Public Health Rep. 2010;125(4) doi: 10.1177/003335491012500411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein A, Stickle TR, Zvolensky MJ, Taylor S, Abramowitz J, Stewart S. Dimensional, categorical, or dimensional-categories: Testing the latent structure of anxiety sensitivity among adults using factor-mixture modeling. Behavior Therapy. 2010;41(4):515–529. doi: 10.1016/j.beth.2010.02.003. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York, NY: Wiley; 1989. [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addict Behav. 2001;26(6):887–899. doi: 10.1016/S0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Beverly Hills, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Ebesutani C, McLeish AC, Luberto CM, Young J, Maack DJ. A bifactor model of anxiety sensitivity: Analysis of the Anxiety Sensitivity Index-3. Journal of Psychopathology and Behavioral Assessment. 2014;36(3):452–464. [Google Scholar]
- Escocard MRPG, Fioravanti-Bastos ACM, Landeira-Fernandez J. Anxiety sensitivity factor structure among Brazilian patients with anxiety disorders. Journal of Psychopathology and Behavioral Assessment. 2009;31(3):246–255. [Google Scholar]
- Etter JF, Vu Duc T, Perneger TV. Validity of the Fagerström test for nicotine dependence and of the Heaviness of Smoking Index among relatively light smokers. Addiction. 1999;94(2):269–281. doi: 10.1046/j.1360-0443.1999.94226910.x. [DOI] [PubMed] [Google Scholar]
- Farris SG, Langdon KJ, DiBello AM, Zvolensky MJ. Why do anxiety sensitive smokers perceive quitting as difficult?: The role of expecting “interoceptive threat” during acute abstinence. Cognitive Therapy and Research (in press) [Google Scholar]
- Farris SG, Leventhal AM, Schmidt NB, Zvolensky MJ. Anxiety sensitivity and pre-cessation smoking processes: Testing the independent and combined mediating effects of negative affect reduction beliefs and smoking motives. J Stud Alcohol Drugs. doi: 10.15288/jsad.2015.76.317. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris SG, Zvolensky MJ, DiBello AM, Schmidt NB. Validation of the Avoidance and Inflexibility Scale (AIS) among treatment-seeking smokers. Psychological Assessment. doi: 10.1037/pas0000059. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition (SCIDI/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2007. [Google Scholar]
- Goodwin RD, Lavoie KL, Lemeshow AR, Jenkins E, Brown ES, Fedoronko DA. Depression, anxiety, and COPD: the unexamined role of nicotine dependence. Nicotine Tob Res. 2012;14(2):176–183. doi: 10.1093/ntr/ntr165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Johnson KA, Stewart S, Rosenfield D, Steeves D, Zvolensky MJ. Prospective evaluation of the effects of anxiety sensitivity and state anxiety in predicting acute nicotine withdrawal symptoms during smoking cessation. Nicotine & Tobacco Research. 2012;26(2):289–297. doi: 10.1037/a0024133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemper CJ, Lutz J, Bähr T, Rüddel H, Hock M. Construct validity of the anxiety sensitivity index–3 in clinical samples. Assessment. 2012;19(1):89–100. doi: 10.1177/1073191111429389. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3. New York, NY: The Guilford Press; 2011. [Google Scholar]
- Leventhal AM, Zvolensky MJ. Anxiety, depression, and cigarette smoking: A transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychological Bulletin. doi: 10.1037/bul0000003. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: A meta-analytic review and synthesis. Psychological Bulletin. 2009;135(6):974–999. doi: 10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Osman A, Gutierrez PM, Smith K, Fang Q, Lozano G, Devine A. The Anxiety Sensitivity Index-3: Analyses of dimensions, reliability estimates, and correlates in nonclinical samples. Journal of Personality Assessment. 2010;92(1):45–52. doi: 10.1080/00223890903379332. [DOI] [PubMed] [Google Scholar]
- Perkins KA, Karelitz JL, Giedgowd GE, Conklin CA, Sayette MA. Differences in negative mood-induced smoking reinforcement due to distress tolerance, anxiety sensitivity, and depression history. Psychopharmacology. 2010;210(1):25–34. doi: 10.1007/s00213-010-1811-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. 1985. pp. 107–121. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behavior Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Trakowski JH. Body vigilance in panic disorder: Evaluating attention to bodily perturbations. Journal of Consulting and Clinical Psychology. 1997;65(2):214–220. doi: 10.1037//0022-006x.65.2.214. [DOI] [PubMed] [Google Scholar]
- Stellman JM, Smith RP, Katz CL, Sharma V, Charney DS, Herbert R, Udasin I. Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. National Emergency Training Center; 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Cox BJ. An expanded Anxiety Sensitivity Index: Evidence for a hierarchic structure in a clinical sample. Journal of Anxiety Disorders. 1998;12:463–483. doi: 10.1016/S0887-6185(98)00028-0. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, Stuart S. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychological Assessment. 2007;19(3):253–268. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Wheaton MG, Deacon BJ, McGrath PB, Berman NC, Abramowitz JS. Dimensions of anxiety sensitivity in the anxiety disorders: Evaluation of the ASI-3. Journal of Anxiety Disorders. 2012;26(3):401–408. doi: 10.1016/j.janxdis.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Wong M, Krajisnik A, Truong L, Lisha NE, Trujillo M, Greenberg JB, Leventhal AM. Anxiety sensitivity as a predictor of acute subjective effects of smoking. Nicotine & Tobacco Research. 2013;15(6):1084–1090. doi: 10.1093/ntr/nts208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Farris SG, Schmidt NB, Smits JAJ. The Role of Smoking Inflexibility/Avoidance in the Relation Between Anxiety Sensitivity and Tobacco Use and Beliefs Among Treatment-Seeking Smokers. Experimental and Clinical Psychopharmacology. 2014 doi: 10.1037/a0035306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.