Abstract
Background:
Global burden of hospital-associated infection (HAI) is on the rise and contributes significantly to morbidity and mortality of the patients. Mobile phones are indispensible part of communication among doctors and other health care workers (HCWs) in hospitals. Hands of HCWs play an important role in transmission of HAI and mobile phones which are seldom cleaned and often touched during or after the examination of patients without hand washing can act as a reservoir for transmission of potent pathogens. This study aimed to investigate the rate of bacterial contamination of mobile phones among HCWs in our tertiary care hospital and to compare it with personal mobile phones of non-HCWs (control group).
Materials and Methods:
The mobile phones and dominant hands of 386 participants were sampled from four different groups, hospital doctors and staff (132), college faculty and staff (54), medical students (100) and control group (100). Informed consent and questionnaire was duly signed by all the participants. Samples were processed according to standard guidelines.
Results:
316 mobile phones (81.8%) and 309 hand swab samples (80%) showed growth of bacterial pathogens. The most predominant isolates were Coagulase-negative Staphylococcus, Staphylococcus aureus, Acinetobacter species, Escherichia coli, Klebsiella pneumoniae, Pseudomonas species and Enterococcus species.
Conclusion:
Hundred percent contamination was found in mobile phones and hands of HCWs indicating mobile phones can be the potential source of nosocomial pathogens. Our study results suggest that use of mobile phones in health care setup should be restricted only for emergency calls. Strict adherence to infection control policies such as proper hand hygiene practices should be followed.
Keywords: Acinetobacter, cell phones, health care workers, methicillin-resistant Staphylococcus aureus, nosocomial pathogens
INTRODUCTION
The global system for mobile telecommunication (GSM) was established in 1982 in Europe to provide improved communication network and today mobile phones have become one of the most indispensable accessories of professional and social life.[1] The telecom regulatory authority of India (TRAI) in its annual report (2009-2010) gave an increase of mobile phone users in India by 49.5% in just one year.[2] Mobile phones are also increasingly becoming an important means of communication among doctors and other health care workers (HCWs) in hospitals where hospital-associated infections (HAI) are prevalent.[3] Global burden of HAI is on the rise and contributes significantly to morbidity and mortality of the patients. It has been estimated that one third of all nosocomial infections may be preventable and are frequently caused by organisms acquired within the hospital environment.[4] Hands of HCWs play an important role in transmission of HAI and mobile phones which are seldom cleaned and often touched during or after the examination of patients without hand washing can act as a reservoir as well as vehicle for transmission of nosocomial infections.[3,5] Moreover, sharing of mobile phones between HCWs and non-HCWs directly facilitates the spread of potentially pathogenic bacteria to the community.[6] The potential of mobile phones as vectors to nosocomial infection has been studied before.[6,7,8,9] However, no study has been conducted in this part of country. In this study we investigated the rate of bacterial contamination of mobile phones among HCWs employed in our tertiary health care teaching hospital and compared it with personal mobile phones of non-HCWs (control group).
MATERIALS AND METHODS
Study duration and population
This study was conducted for a period of 6 months (October 2011 to March 2012) at a tertiary health care teaching hospital of Uttarakhand state, India.
The mobile phones and dominant hands of 386 participants were sampled without any prior intimation and were categorized in four different groups as hospital doctors and staff (132), college faculty and staff (54), first year medical students (100) and public colony/control group (100). The control group consisted of residents of the public colony not working in any health care institution and using the mobile phones for at least 1 month. A questionnaire was designed to know the extent of usage of mobile phones, the location of use, the awareness of disinfection practices of mobile phones and the frequency of hand washing after using their phones.
The study protocol was approved by Institutional Ethical committee (IEC) and concept of the study was explained to all the participants and their consent and duly filled questionnaire was sought.
Sample collection and processing
Separate teams were formed for the sample collection and processing to avoid any bias. Sterile latex gloves were worn before sampling mobile phones. Sterile cotton swab moistened with normal saline was swabbed over the keys, mouth piece, ear phone, hot keys, sides and back of the mobile phones which were being used for at least 1 month. Dominant hand of the user was swabbed along the fingers, webs, nail endings and palm. Samples were labeled using codes and submitted to processing team in microbiology laboratory within 30 minutes of sample collection. Samples were inoculated onto sheep Blood agar (BA) and MacConkey's agar (MA) plates and incubated at 37°C aerobically for 24 hours. Plates were examined for the growth and the identification was made on the basis of colony morphology, gram reaction, and the battery of biochemical tests. Methicillin sensitivity for all staphylococcal isolates was done by Kirby Bauer disc diffusion method using cefoxitin disc (30 μg) as a surrogate marker for methicillin and the results were interpreted as per CLSI guidelines.[10,11]
All dehydrated media, reagents and antibiotic discs were procured from Hi-media Laboratories Pvt. Ltd, Mumbai, India.
RESULTS
A total of 386 mobile phones and hand swab samples were analyzed for the presence of bacterial pathogens. Out of these, 316 mobile phones (81.8%) and 309 hand swab samples (80%) showed growth of bacterial pathogens.
Out of the total 316 contaminated mobile phones, highest contamination was in hospital doctors and staff (100%) followed by the medical students (92%), college faculty and staff (87%) and least in the residents of the public colony (45%).
Among total of 309 contaminated hand samples, highest contamination was again seen in hospital doctors and staff (100%) followed by the medical students (94%), the college faculty and staff (83%) and the least in the residents of the public colony (38%) [Figure 1].
Figure 1.
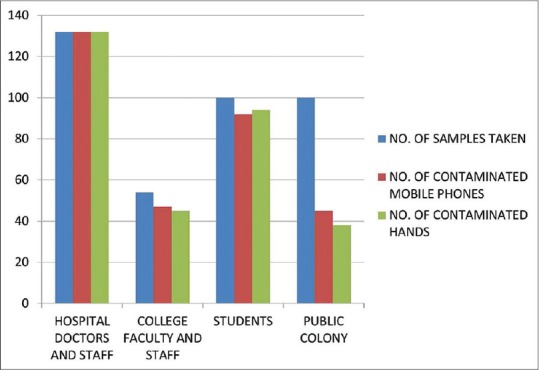
Contaminated samples in various groups
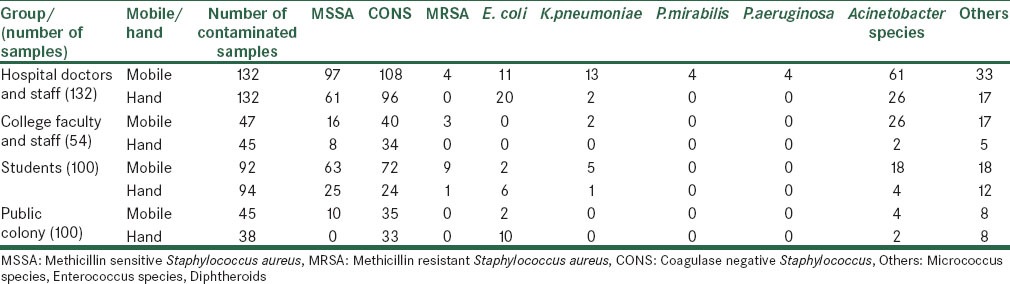
Among the total 664 bacterial isolates contaminating the mobile phones, the gram-positive bacteria were coagulase-negative Staphylococcus (CONS) (255), followed by methicillin-sensitive Staphylococcus aureus (MSSA) (186), methicillin-resistant Staphylococcus aureus (MRSA) (16), Micrococcus sp. (27), Diptheroids (22), Enterococcus sp.(10).
Among gram-negative isolates Acinetobacter species (86), Escherichia coli (15), Klebsiella pneumoniae (20), Enterobacter species (9), Citrobacter species (8), Pseudomonas aeruginosa (6) and Proteus mirabilis (4) were common. [Figure 2].
Figure 2.
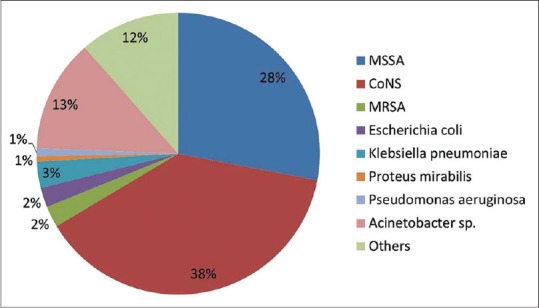
Distribution of various bacterial isolates in the mobile phones
Among the total 397 bacterial isolates contaminating the hands, the highest count was that of CONS (187), followed by MSSA (94), E. coli (36), Acinetobacter sp. (34), Micrococcus sp. (16), Diptheroids (8), Enterococcus sp. (8), Citrobacter sp. (6), Enterobacter sp. (4) and K. pneumoniae (3). Only one MRSA was isolated [Figure 3].
Figure 3.
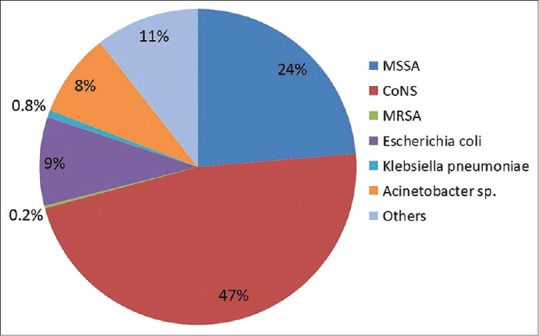
Distribution of various bacterial isolates from the hand swabs
A total of 16 MRSA were isolated from the mobile phones which were distributed as surgery (3), orthopedics (1), physiology (3) and medical students (9). Out of total 186 MSSA isolated from the mobile phone samples 97 were from the hospital doctors and staff, 16 from the college faculty and staff, 63 from the students and 10 from the public colony.
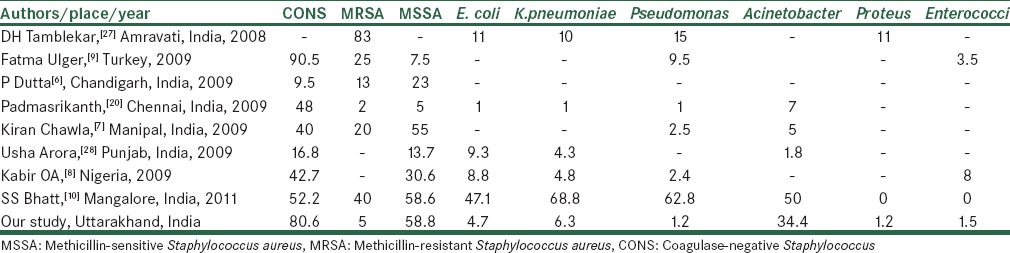
Among the 94 MSSA isolated from the hand swab samples, 61 belonged to the hospital doctors and staff, 8 to the college faculty and staff, 25 to the students and none in the public colony [Table 1]. A single MRSA isolated from the hand swab sample belonged to the medical students group.
Table 1.
Distribution of various bacterial isolates among different groups
DISCUSSION
Nosocomial infections continue to pose significant risk of increased mortality and morbidity among the patients and the various etiological agents responsible for such infections vary from hospital to hospital and also in different geographical regions.[3] However, incidence of such infections can be reduced by maintaining proper hygiene among the HCW as well as in the hospital environment. Mobile phones have become an inseparable part in a health care set up and it has been proved as important potential fomites for the transmission of nosocomial infections.[6,7,8,9] One third of the mobile phones belonging to HCWs are contaminated by potential pathogens.[12]
In our study the mobile phones and hands of HCWs showed a high contamination rate (81.8% and 80%, respectively) with bacteria and also with nosocomial pathogens, this corroborates with the results of other studies, Ulger et al.[8] from Turkey (94.5%), Goel et al.[13] from Himachal Pradesh, India (94.5%), Jayalakshmi et al.[14] from Coimbatore, India (91.60%), Chawla et al.[6] from Karnataka, India (92.5%), Dutta et al.[5] from Chandigarh, India (72%), Famurewa et al.[15] from Nigeria (82.6%).
Among the various reports regarding the role of mobile phones in the spread of nosocomial infection had shown that the combination of constant handling and heat generated by the mobile phones creates a prime breeding ground for microorganisms that are normally found on our skin. This may be because these types of bacteria increase in optimum temperature and mobile phones are perfect for breeding these microorganisms as they are kept warm and easy to handle in pockets, handbags and briefcases.[3]
Out of four groups studied, HCW group has highest rate of contamination (100%), followed by student group (92%), college faculty and staff (87%) and public colony (45%). The reason for high contamination rate among HCW could be improper usage of disinfection and poor hand hygiene practices probably due to patient overload. High contamination rate among medical student group could be lack of awareness of nosocomial infection and its mode of transmission. Public group was the least contaminated, as they are not so frequently exposed to healthcare set up. Our results were in contrast to the study from Manglore by Khivsera et al.[16] who has reported lesser contamination rate of the hands of HCWs (30%). Another study from Nigeria by Akinyemi et al.[7] reported HCWs to be the least contaminated (15.3%) and marketers and food vendors to be the most contaminated group (37%).
Coagulase-negative Staphylococci were the most prevalent bacteria (80.6%) isolated from mobile phones and this finding correlates well with the results of other researchers Ulger et al. (90.5%), Jayalakshmi et al. (82%), Srikanth et al. (48%), Akinyemi et al. (42.7%), Chawla et al. (40%).[6,7,8,14,17]
S. aureus is one of the frequently isolated bacteria in hospital infection and in the present study was isolated from 202 (63.9%) contaminated mobile phones out of which 16 (7.9%) were MRSA. Among the contaminated hand samples 95 (30.7%) isolates were S. aureus out of which 1 (1.1%) isolate was MRSA. Isolation of MRSA was a cause of concern as these are epidemiologically important drug-resistant pathogens. Our finding is in agreement with the work of Khivsera et al.[16] who reported 40% of the mobile phones at Mangalore hospital to be contaminated by S. aureus. Whereas J. Omololu-Aso et al. from Nigeria[18] reported that 17.14% to 25.71% of mobile phones in different wards were contaminated by S. aureus. The MRSA carriage status however is much higher in Indian hospitals than those reported from western countries which range from 0 to 1.9%.[3,19] Comparatively poor hygiene and hand washing practices followed by HCWs in India might be the contributory factor.
High isolation rate of Acinetobacter species was of major concern because of its well-known identity as a multi-drug resistant (MDR) nosocomial pathogen. Our findings were in support of the study conducted in Israel.[20] In another study from Israel it was found that a significant percentage of mobile phones were contaminated with MDR Acinetobacter species and that cross contamination between hands, mobile phones and patients occurred.[21] A similar study at Soroka university medical center Israel identified MDR Acinetobacter baumannii in the hands, mobile phones of the HCWs and patients admitted to the ICU.[22] Ability of the Acinetobacter to contaminate mobile phones is not unlikely as studies have revealed that Acinetobacter along with S. aureus are commonly acquired through cross transmission because of their propensity of drying and to contaminate fomites.[23] Other organisms isolated in the present study included K. pneumoniae (6.3%), E. coli (4.7%), Pseudomonas (1.2%), Proteus mirabilis (1.2%), Enterococcus (1.5%).
It's a well-established fact that all these organisms are agents of nosocomial infection.[24] Pseudomonas aeruginosa has been reported in the United States by the Centre of disease control and prevention to be the most isolated nosocomial pathogen accounting for 10.1% of all HAI.[25] The horizontal spread of resistance factors into environmental gram negative bacilli (GNB) has seen the emergence of MDR Acinetobacter, Pseudomonas, and coliforms, wherever looked for, even in skin carriage strains.[26] Isolation of E. coli and K. pneumoniae indicate the improper or casual hand hygiene practices. Isolation of nosocomial pathogens on mobile phones concurs there potential as fomites for HAIs. Moreover, recovery of similar bacteria from the hands of mobile phone users suggests that hands may be the source of contamination for mobile phones. Hence, the results of our study conclude that mobile phones get contaminated through hands and vice versa and then from hands to other exposed areas of the body which indicates the presence of skin flora on mobile phones. Different studies reported a varied range of isolates shown in Table 2.
Table 2.
Distribution of isolates among various studies conducted
Questionnaire results shown in Table 3 were also alarming to know the response from the HCWs and students. Almost all the HCW used the mobile phones and majority of them use it for other than regular calls and text messages. Most of the clinicians admitted that they use mobile phones for taking photograph of the patients in the ward and even in operation theatre (OT). With the advent of internet facilities in the mobile phones, its use has increased many folds for browsing and acquiring information regarding the cases. Usage of mobile phone while attending patients has the major health implications. The new guidelines published by infection control nurses association (ICNA) in 2002 emphasized the primary role of hand decontamination in the prevention and transmission of infection.[29] Also, pathogens from patients can be transmitted to the mobile phones of HCWs and increase the risk of infection among them and their family members too. 97% of the subjects accepted of not disinfecting their mobile phones regularly. This finding substantiates the high rate of contamination and its transmission between hands and mobile phones in our study.
Table 3.
Questionnaire results
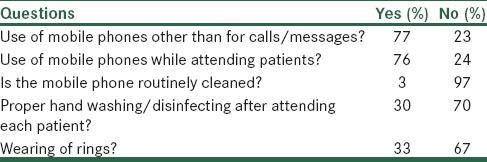
From our study results it is evident that significant numbers of pathogenic organisms were isolated from the mobile phones as well as hands of the HCWs than that of the control group. There are no guidelines for the care, cleaning and restriction of the mobile phones in our health care setting. Microbial contamination of the mobile phones and their increased use among the HCWs pose a significant epidemiological risk to the public. Simple measures such as proper hand hygiene practices and regular decontamination of the mobile phones with alcohol wipes may reduce the risk of HAI's caused by these devices.[30]
Hence, we conclude that there is an urgent need to stress awareness among the HCWs about the potential role of mobile phones in transmission of infectious agents in and outside the hospital. Although regular cleaning of the mobile phones and adhering to the infection control practices would significantly decrease the transmission rate still there use inside the hospital premises should be restricted for emergency calls only. Infection control committee of every hospital can step forward to make clear cut guidelines regarding the use of mobile phones in health care set up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sowah LN. The future of the mobile phone Internet: How do we tap into its fullest benefits? Technology Blogs. 2008:1–2. [Google Scholar]
- 2.Telecom regulatory authority India. Annual report 2009-2010. [Last accessed on 2012 June 27]. Available from: http://www.trai.gov.in/annualreport/AnnualReport_09_10 English.pdf .
- 3.Brady RR, Wasson A, Stirling I, McAllister C, Damani NN. Is your phone bugged? The incidence of bacteria known to cause nosocomial infection in healthcare workers’ mobile phones. J Hosp Infect. 2006;62:123–5. doi: 10.1016/j.jhin.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Hughes JM. Study on the efficacy of nosocomial infection control (SENIC Project): Results and implications for the future. Chemotherapy. 1988;34:553–61. doi: 10.1159/000238624. [DOI] [PubMed] [Google Scholar]
- 5.Datta P, Rani H, Chander J, Gupta V. Bacterial contamination of mobile phones of health care workers. Indian J Med Microbiol. 2009;27:279–81. doi: 10.4103/0255-0857.53222. [DOI] [PubMed] [Google Scholar]
- 6.Chawla K, Mukhopadhayay C, Gurung B, Bhate P, Bairy I. Bacterial ‘cell’ Phones: Do cell phones carry potential pathogens? Online J Health Allied Scs. 2009;8:8. [Google Scholar]
- 7.Akinyemi KO, Atapu AD, Adetona OO, Coker AO. The potential role of mobile phones in the spread of bacterial infections. J Infect Dev Ctries. 2009;3:628–32. doi: 10.3855/jidc.556. [DOI] [PubMed] [Google Scholar]
- 8.Ulger F, Esen S, Dilek A, Yanik K, Gunaydin M, Leblebicioglu H. Are we aware how contaminated our mobile phones with nosocomial pathogens? Ann Clin Microbiol Antimicrob. 2009;8:7. doi: 10.1186/1476-0711-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhat SS, Hegde SK, Salian S. Potential of mobile phones to serve as a reservoir in spread of nosocomial pathogens. Online J Health Allied Scs. 2011;10:14. [Google Scholar]
- 10.Clinical and Laboratory Standard Institute. Vol. 1. Pennsylvania, USA: Clinical and Laboratory Standard Institute; 2007. Performance Standards for Antimicrobial Susceptibility Testing; pp. M2–A9. [Google Scholar]
- 11.Koneman EW, Allen SD, Janda WM, Winn WC, Procop GW, Schreckenberger PC, et al. Color Atlas and Textbook of Diagnostic Microbiology. 6th ed. Philadelphia: JB Lippincott Co; 2006. Characteristics for presumptive identification of bacteria; pp. 212–301. [Google Scholar]
- 12.Fleming K, Randle J. Toys-friend or foe? A study of infection risk in a paediatric intensive care unit. Paediatr Nurs. 2006;18:14–8. [PubMed] [Google Scholar]
- 13.Goel M, Goel A. Beware! Your phone is ‘bugged’ mobile phones of dental professionals a potential source of bacterial contamination-A bacteriological study. Indian J Dent Sci. 2009;1:42–7. [Google Scholar]
- 14.Jayalakshmi J, Appalaraju B, Usha S. Cellphones as reservoirs of nosocomial pathogens. J Assoc Physicians India. 2008;56:388–9. [PubMed] [Google Scholar]
- 15.Famurewa O, David OM. Cell phones: A medium of transmission of bacterial pathogens. World Rural Observations. 2009;1:69–72. [Google Scholar]
- 16.Khivsara A, Sushma TV, Dhanashree B. Typing of staphylococcus aureus from mobile phones and clinical samples. Curr Sci. 2006;90:910–12. [Google Scholar]
- 17.Srikanth P, Rajaram E, Sudharsanam S, Lakshmanan A, Umamaheswari SS, Kalyani J. The mobile phone in a tropical setting-emerging threat for infection control. Sri Ramachandra Journal of Medicine. 2009;2:18–20. [Google Scholar]
- 18.Omololu-Aso J, Kolawole DO, Omololu-Aso OO, Ajisebutu SO. Antibiotics sensitivity pattern of staphylococcus aureus from fomites in the Obafemi Awolowo University Teaching Hospital Complex Nigeria. Int J Med Med Sci. 2011;3:32–6. [Google Scholar]
- 19.Braddy CM, Blair JE. Colonization of personal digital assistants used in a health care setting. Am J Infect Control. 2005;33:230–2. doi: 10.1016/j.ajic.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Borer A, Gilad J, Smolyakov R, Eskira S, Peled N, Porat N, et al. Cell phones and acinetobacter transmission. Emerg Infect Dis. 2005;11:1160–1. doi: 10.3201/eid1107.050221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borer A, Gilad J. Cellphone and acinetobacter transmission. Emerging Infect Dis. 2005;7:1–3. doi: 10.3201/eid1107.050221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Isaacs D, Daley A, Dalton D, Hardiman R, Nallusamy R. Swabbing computers in search of nosocomial bacteria. Pediatr Infect Dis J. 1998;17:533. doi: 10.1097/00006454-199806000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Wendt C, Dietze B, Dietz E, Rüden H. Survival of Acinetobacter baumannii on dry surfaces. J Clin Microbiol. 1997;35:1394–7. doi: 10.1128/jcm.35.6.1394-1397.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rusin P, Maxwell S, Gerba C. Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria, and phage. J Appl Microbiol. 2002;93:585–92. doi: 10.1046/j.1365-2672.2002.01734.x. [DOI] [PubMed] [Google Scholar]
- 25.Todar M. Pseudomonas aeruginosa in Web Review of Todar's Online Textbook of Bacteriology “The Good, the Bad, and the Deadly”. Science Magazine. 2004;304:1–12. [Google Scholar]
- 26.Yavankar SP, Pardesi KR, Chopade BA. Species distribution and physiological characterization of acinetobacter genospecies from healthy human skin of tribal population in India. Indian J Med Microbiol. 2007;25:336–45. doi: 10.4103/0255-0857.37335. [DOI] [PubMed] [Google Scholar]
- 27.Tamblekar DH, Gulhane PB, Dahikar SG, Dudhane MN. Nosocomial hazards of doctor's mobile phones in hospitals. J Med Sci. 2008;8:73–6. [Google Scholar]
- 28.Arora U, Devi P, Chadha A, Malhotra S. Cellphones a modern stayhouse for bacterial pathogens. JK Science. 2009;11:127–9. [Google Scholar]
- 29.Infection Control Nurses Association. Hands decontamination guidelines. ICNA. (2nd ed) 2002 [Google Scholar]
- 30.Jeske HC, Tiefenthaler W, Hohlrieder M, Hinterberger G, Benzer A. Bacterial contamination of anaesthetists’ hands by personal mobile phone and fixed phone use in the operating theatre. Anaesthesia. 2007;62:904–6. doi: 10.1111/j.1365-2044.2007.05172.x. [DOI] [PubMed] [Google Scholar]


