Abstract
Background:
Considering an increase in elderly population in recent years, it has become necessary to pay attention to this group so that they can have a higher quality of life (QoL). Oral health is one of the factors affecting the QoL of the elderly.
Aims:
The purpose of this study is to evaluate the effect of oral health on the QoL of the elderly population in Babol, Iran.
Materials and Methods:
In this study, we used the multi-stage cluster sampling technique to select 300 elderly subjects, over 65 years of age, living in Babol. Oral health-related QoL was evaluated by the Persian version of oral health impact profile (OHIP-14) questionnaire. Data were collected on gender, age, occupation, education, the date of the last dental visit, use of prosthetic appliances, and dental treatment needs, including the periodontal, prosthetic, and surgical needs, by interview and examination.
Statistical Analysis Used:
Data were analyzed with SPSS software program using Mann–Whitney and Kruskal–Wallis tests.
Results:
The mean age of the subjects was 71.4 ± 5.6 years, with 183 males (61%) and 117 females (39%). The mean score of OHIP-14 questionnaire was 22.4 ± 8.2, with a range of 5‒50. The highest score was achieved on the psychological discomfort domain. There was no significant difference in OHIP-14 scores according to gender, with significantly lower scores in subjects with academic education. The subjects wearing prosthetic appliances had lower OHIP-14 scores compared to those who did not wear prosthetic appliances. OHIP-14 scores were lower in the dentate individuals compared to the edentulous individuals. There was no correlation between the age and the OHIP-14 score.
Conclusion:
In general, the results of the present study showed a moderate oral health-related QoL in the elderly living in Babol, who have orodental problems.
Keywords: Elderly, oral health impact profile-14 score, oral health, quality of life
Introduction
Improvement of the general health during the second half of the 20th century has increased the mean age of the population. It is also predicted that the number of the elderly population will significantly increase in future, which in turn will increase geriatric diseases.[1] Given the high rate of the aging of the population, it is absolutely necessary to pay attention to this part of the society, so they will have a comfortable, high-quality life.[2] A high prevalence of oral diseases in the elderly can result in low quality of life (QoL). The elderly who have lost the majority of their teeth suffer from serious functional limitations, which lead to nutritional problems.[3] In addition, the number, location, and distribution of the lost teeth influence the severity of such problems.[4] Furthermore, the presence of tooth caries may lead to infections, pain, and discomfort.[3] One aspect of the oral health is its social effect in the elderly population.[5] As the number of the elderly increases, coordination and cost-effectiveness of the health policies become more critical.[6]
The health-related quality of life (HRQoL) is a multi-dimensional concept, incorporating physical, mental, and social health of the patient and has widely been recognized for evaluating healthcare results. A factor that can have a significant effect on the structure of HRQoL is the oral health,[7] which might play a significant role in patients, seeking dental office. Epidemiologic studies have shown factors such as age, gender, loss of teeth, the socio-economic status, cultural background, dental stress, and smoking can affect the oral health-related quality of life (OHRQoL).[8,9]
Evaluation of OHRQoL allows a transition from the conventional medical and dental criteria toward evaluation and care focusing on the individuals’ social and emotional experiences as well as the physical activities to determine proper therapeutic aims.[10]
There are many questionnaires available for the evaluation of OHRQoL. The short form of the oral health impact profile (OHIP) is the most famous one, which contains 14 questions (OHIP-14). The validity and reliability of the Persian version of the questionnaire have already been confirmed.[11] The questionnaire, which consists of seven domains, is applicable to different cultures and has been translated into several languages.[12]
Considering the special physical condition of the elderly and the effects that tooth loss can exert on their function and the way they encounter it, the present study was undertaken to determine the OHRQoL of the elderly in Babol, Iran.
Materials and Methods
In the present cross-sectional study on the elderly residents of Babol, a total of 300 subjects were selected by considering δ1 = 4, δ2 = 6, and d = 1. A multi-stage cluster sampling technique was used for the sampling. Babol was divided into 20 districts based on geographical criteria, of which 10 districts were randomly selected. Thirty subjects were randomly selected from those living in the vicinity of the health centers in each district and were asked to fill out the questionnaire.
The inclusion criteria consisted of an age range of over 65, absence of any cognitive disorders, the ability to cooperate, and the absence of any behaviors that indicates psychological problems.
The Persian version of OHIP-14 questionnaire was used for evaluating OHRQoL. This standard questionnaire consists of 14 questions in 7 domains, including functional limitations, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicaps. Each domain consists of two questions. The choices are never (0), seldom (1), sometimes (2), almost often (3), and often (4). The score range of OHIP-14 questionnaire is 0‒56. A low score indicates the individual's high QoL. The questionnaire for each subject was filled out by the researcher in his/her presence. The data on occupation, education, the time of the last dental visit, the use of prosthetic appliances (complete, partial, and fixed prostheses), and the need for periodontal, endodontic, and prosthetic care were recorded by the researcher through the interview and the examination. Finally, if any oral disease was observed, the patient was referred to the treatment centers. Data were analyzed with Statistical Package for the Social Sciences (SPSS 19, Babol, Iran), using Man–Whitney and Kruskal–Wallis tests.
Results
The mean age of the subjects was 71.4 ± 5.6 years, with 183 (61%) males and 117 (39%) females. Eighty-three subjects (27.7%) were illiterate, 155 (51.7%) had primary education and 62 (20.7%) had academic education. The mean time of the last dental visit was 6.2 ± 6.7 years. Forty-one subjects (19.6%) wore removable partial prostheses, 36 (17.2%) wore fixed partial prostheses, and 139 (68.9%) wore complete prostheses. The treatment needs of the subjects were consisted of the following: Totally, 128 subjects (90.8%) needed periodontal treatment, 55 (39%) needed endodontic, 60 (42.6%) needed surgical, and 107 (75.9%) needed prosthetic treatment. Of all the subjects, 142 (47.3%) were edentulous, of which 3 did not wear any prosthetic appliances.
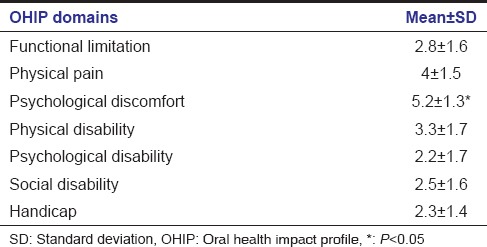
The mean OHIP-14 score of the subjects was 22.4 ± 8.2 of a maximum score of 56 (5‒50). The highest score was recorded in the psychological discomfort domain (P < 0.05) [Table 1].
Table 1.
Means and standard deviations of the OHIP-14 components in the study population
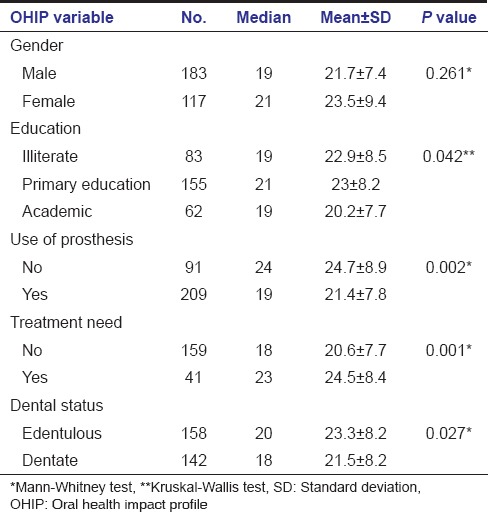
There was no significant difference in OHIP-14 scores between males and females (P = 0.261). The scores of the subjects with academic education were significantly lower than those of the other subjects (P = 0.042). In addition, in subjects wearing prosthetic appliances, the scores were significantly lower than those in the subjects not wearing such appliances (P = 0.002). The scores were significantly lower in those not needing treatment compared to those needing treatment (P = 0.001). In addition, the scores were significantly lower in dentate subjects compared to edentulous subjects (P = 0.027).
There was no correlation between OHIP-14 scores and the age of the subjects (Kendall correlation co-efficient = 0.041, P = 0.312) [Table 2].
Table 2.
Means and standard deviations of OHIP-14 scores in the study population separately in terms of demographic variables
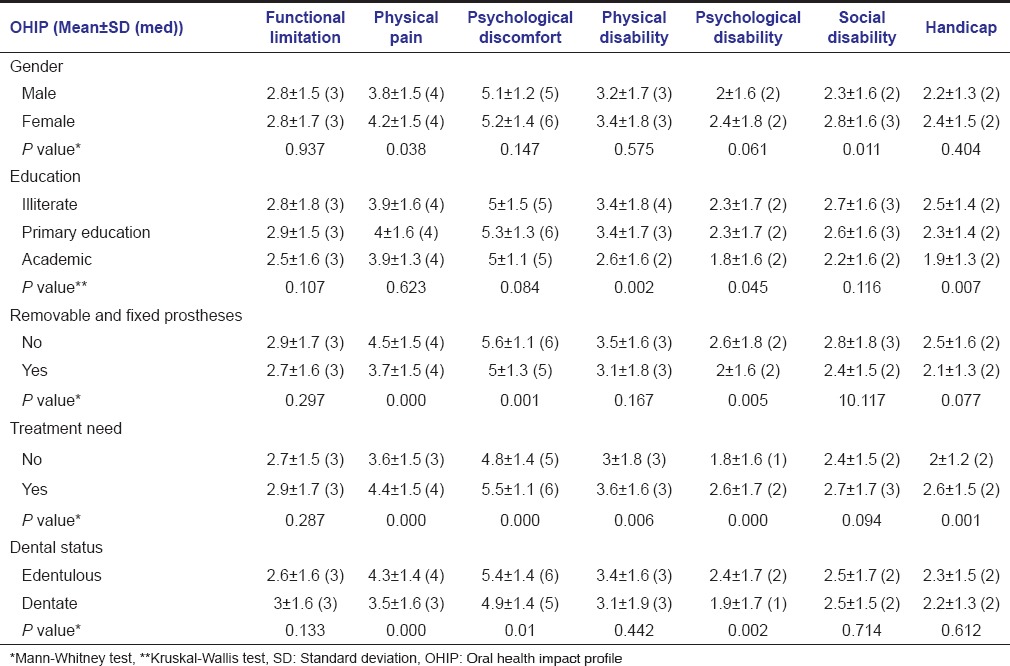
The physical pain and social disability scores were significantly higher in females (P = 0.011 and P = 0.038, respectively). There was no significant difference between males and females in other domains.
The physical disability, psychological disability, and handicap scores were significantly lower in subjects with academic education compared to those without such education (P = 0.007, P = 0.045, and P = 0.002, respectively).
The handicap score in illiterate individuals was significantly higher compared to other subjects (P = 0.007). The physical pain, psychological discomfort, and psychological disability scores in the subjects wearing prosthetic appliances were significantly lower than those in the subjects not wearing such appliances (P = 0.005, P = 0.001, and P < 0.001).
The physical pain, psychological discomfort, physical disability, and handicap scores in the subjects with treatment needs were significantly higher than the subjects without such needs (P = 0.001, P = 0.006, P < 0.001, and P < 0.001, respectively). The physical pain, psychological discomfort, and physical disability scores in the dentate patients were significantly lower compared to the edentulous subjects (P = 0.442, P = 0.01, and P < 0.001, respectively) [Table 3].
Table 3.
Means and standard deviations of OHIP-14 scores separately in terms of gender, education, use of prosthetic appliances, treatment needs and dental status
Discussion
In the present study, the results of the OHIP-14 questionnaire indicated a moderate oral health-related health in the subjects in Babol. Since the highest score was recorded in the domain of psychological discomfort, it is evident that the subjects had emotional and psychological discomfort in relation to the condition of their oral cavity. In a study by Cicciu et al. on subjects with an age range of 65‒87, psychological discomfort had the highest score on the OHIP-14 questionnaire.[1] For those older than 60 years, Ulinski et al.[2] and Kotzer et al.[13] observed that the most commonly affected domains of the OHIP-14 questionnaires were the physical pain and psychological discomfort.
On the other hand, Kushnir et al. showed that the oral health is strongly related to the QoL and oral health problems severely compromise the QoL.[14] In addition, a study in China showed that the general health of the patients older than 46 is compromised with oral diseases.[15]
In the present study, discomfort, disability, and complaints of oral status prevalent in females rather than males, due to the higher sensitivity of females’ emotions and their social problems, especially in the social disability and physical pain domains.
Similarly, Cicciu et al.[1] observed a higher score of OHIP-14 for females compared to the male subjects. This is also in good agreement with the previous results that were obtained by Ulinski et al., in which one of the variables with a negative effect on OHRQoL in the elderly was gender, and it was pointed out that females express more dissatisfaction with their appearance even under the conditions similar to those of males, indicating a higher perception about their oral condition. Females have more complaints regarding pain and the inability to chew.[2]
Tsakos et al. reported that low educational status had an indirect negative effect on the OHRQoL in the elderly that is, with an increase in education the OHIP-14 scores decreased, indicating a better oral health status.[16] In the present study, subjects with academic educations also had a better oral health status due to the higher cultural level and better care of oral health.
In our study, the mean OHIP-14 scores in subjects wearing prosthetic appliances (both fixed and removable) were lower than those not wearing prosthetic that is, those wearing prosthetic had a better oral health status compared to those not wearing prostheses. A similar result was obtained in a study by Dable et al. They showed while the general health did not improve noticeably after the oral rehabilitation, many changes took place in the QoL of the elderly.[17] However, it was reported that the need for prosthesis in the elderly had no negative effect on OHRQoL.[2] In a study on subjects with a mean age of 59, Silva showed while tooth loss and the use of ill-fitting prosthetic appliances did not interfere with daily activities and social relationships, such conditions had a negative effect on some aspects of OHIP-14, including psychological discomfort and physical pain.[18] Similarly, in the present study, the highest scores were recorded in the psychological discomfort domain.
In addition, the OHIP-14 scores were lower in the dentate subjects compared to the edentulous subjects that is, edentulous subjects had more problems in relation to their oral health. This is consistent with the results showed by Cicciu, in which having fewer teeth resulted in higher OHIP-14 scores.[1] Similar result was observed in South Australia, in which the elderly who had lost all of their teeth had higher OHRQoL scores, indicating the lower QoL.[19]
A study by Bethen et al. showed that in edentulous elderly the amount, type, and frequencies of food intake decrease, especially foods containing carotene and Vitamin C,[20] which in turn can be a reason for the decrease in the QoL of the elderly. Zhong et al. showed that OHRQoL is strongly correlated with at least 10 teeth in each jaw.[4] A meta-analysis showed that a minimum number of teeth has the greatest effect on OHRQoL and with a decrease in the number of residual teeth the effect aggravates more clearly; in addition, it was shown that the presence of an anterior tooth loss had more negative effect on OHRQoL compared to the loss of posterior teeth.[21] This is similar to what was observed in our study. Albaker also showed that the patients who used denture in one jaw had better OHRQoL compared to those who wore dentures in both jaws.[22]
In the present study, the subjects who needed treatment had lower OHRQoL due to poorer oral health. Similarly, Jensen et al. showed that poor OHRQoL is significantly correlated with an immediate need for the dental treatment in the elderly.[23] This is also similar to what was showed by Andrade et al. that the elderly needing prostheses had poor OHRQoL.[24]
According to the study of Petersen et al., the number of elderly people is increasing all over the world and non-contagious diseases have rapidly become the main etiologic agents for morbidity and mortality, attracting the attention of policymakers for the community health.[25] In addition, the evaluation of the patients is the pivotal factor for determining the health status. Oral diseases are very common and not only do their impact on the patients physically, but also they exert psychological, social, and economic effects on them. In a large number of patients, the QoL is compromised, affecting several aspects of their lives, including masticatory efficacy and speech.[12] In this case, Luo et al. showed that the OHIP-14 questionnaire scores have a significant correlation with the dental care, odontogenic pain, occupation, and the duration of homelessness (P < 0.05). The results of that study showed that oral health was correlated with the sociodemographic factors and dental problems.[26]
To conclude, the effect of the oral health on the QoL of elderly is an important health-related factor. We have studied the effect of oral health on the QoL of the elderly population in Babol, Iran. The results showed that the elderly population of Babol has undesirable OHRQoL, which might be attributed to their low educational status and treatment needs. Edentulism and not wearing prosthetic appliances have a negative effect on the QoL of the elderly.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Cicciù M, Matacena G, Signorino F, Brugaletta A, Cicciù A, Bramanti E. Relationship between oral health and its impact on the quality life of Alzheimer's disease patients: A supportive care trial. Int J Clin Exp Med. 2013;6:766–72. [PMC free article] [PubMed] [Google Scholar]
- 2.Ulinski KG, do Nascimento MA, Lima AM, Benetti AR, Poli-Frederico RC, Fernandes KB, et al. Factors related to oral health-related quality of life of independent brazilian elderly. Int J Dent 2013. 2013 doi: 10.1155/2013/705047. 705047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El Osta N, Tubert-Jeannin S, Hennequin M, Bou Abboud Naaman N, El Osta L, Geahchan N. Comparison of the OHIP-14 and GOHAI as measures of oral health among elderly in Lebanon. Health Qual Life Outcomes. 2012;10:131–41. doi: 10.1186/1477-7525-10-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Q, Witter DJ, Gerritsen AE, Bronkhorst EM, Creugers NH. Functional dental status and oral health-related quality of life in an over 40 years old Chinese population. Clin Oral Investig. 2013;17:1471–80. doi: 10.1007/s00784-012-0834-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornejo M, Pérez G, de Lima KC, Casals-Peidro E, Borrell C. Oral health-related quality of life in institutionalized elderly in Barcelona (Spain) Med Oral Patol Oral Cir Bucal. 2013;18:e285–92. doi: 10.4317/medoral.18280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Metcalf SS, Northridge ME, Lamster IB. A systems perspective for dental health in older adults. Am J Public Health. 2011;101:1820–3. doi: 10.2105/AJPH.2011.300321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Papagiannopoulou V, Oulis CJ, Papaioannou W, Antonogeorgos G, Yfantopoulos J. Validation of a Greek version of the oral health impact profile (OHIP-14) for use among adults. Health Qual Life Outcomes. 2012;10:7. doi: 10.1186/1477-7525-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 9.Walter MH, Woronuk JI, Tan HK, Lenz U, Koch R, Boening KW, et al. Oral health related quality of life and its association with sociodemographic and clinical findings in 3 northern outreach clinics. J Can Dent Assoc. 2007;73:153. [PubMed] [Google Scholar]
- 10.Sischo L, Broder HL. Oral health-related quality of life: What, why, how, and future implications. J Dent Res. 2011;90:1264–70. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Motallebnejad M, Hadian H, Mehdizadeh S, Hajiahmadi M. Validity and reliability of the Persian version of the oral health impact profile (OHIP)-14. Caspian J Intern Med. 2011;2:314–20. [PMC free article] [PubMed] [Google Scholar]
- 12.Navabi N, Nakhaee N, Mirzadeh A. Validation of a Persian version of the oral health impact profile (OHIP-14) Iran J Public Health. 2010;39:135–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Kotzer RD, Lawrence HP, Clovis JB, Matthews DC. Oral health-related quality of life in an aging Canadian population. Health Qual Life Outcomes. 2012;10:50. doi: 10.1186/1477-7525-10-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kushnir D, Zusman SP, Robinson PG. Validation of a Hebrew version of the oral health impact profile 14. J Public Health Dent. 2004;64:71–5. doi: 10.1111/j.1752-7325.2004.tb02730.x. [DOI] [PubMed] [Google Scholar]
- 15.Liu LJ, Xiao W, He QB, Jiang WW. Generic and oral quality of life is affected by oral mucosal diseases. BMC Oral Health. 2012;12:2. doi: 10.1186/1472-6831-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsakos G, Sheiham A, Iliffe S, Kharicha K, Harari D, Swift CG, et al. The impact of educational level on oral health-related quality of life in older people in London. Eur J Oral Sci. 2009;117:286–92. doi: 10.1111/j.1600-0722.2009.00619.x. [DOI] [PubMed] [Google Scholar]
- 17.Dable RA, Nazirkar GS, Singh SB, Wasnik PB. Assessment of Oral health related quality of life among completely edentulous patients in western India by using GOHAI. J Clin Diagn Res. 2013;7:2063–67. doi: 10.7860/JCDR/2013/6377.3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva ME, Villac EL, Magalh˜aes CS, Ferreira EF. Impact of tooth loss in quality of life. Cien Saude Colet. 2010;15:841–50. doi: 10.1590/s1413-81232010000300027. [DOI] [PubMed] [Google Scholar]
- 19.Slade GD, Spencer AJ, Locker D, Hunt RJ, Strauss RP, Beck JD. Variations in the social impact of oral conditions among older adults in South Australia, Ontario, and North Carolina. J Dent Res. 1996;75:1439–50. doi: 10.1177/00220345960750070301. [DOI] [PubMed] [Google Scholar]
- 20.Bethene ER, Bruce AD. The effect of functional dentition on healthy eating index scores and nutrient intakes in a nationally representative sample of older adults. J Public Health Dent. 2009;69:207–16. doi: 10.1111/j.1752-7325.2009.00124.x. [DOI] [PubMed] [Google Scholar]
- 21.Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8:1–11. doi: 10.1186/1477-7525-8-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Albaker AM. The oral health-related quality of life in edentulous patients treated with conventional complete dentures. Gerodontology. 2013;30:61–6. doi: 10.1111/j.1741-2358.2012.00645.x. [DOI] [PubMed] [Google Scholar]
- 23.Jensen PM, Saunders RL, Thierer T, Friedman B. Factors associated with oral health-related quality of life in community-dwelling elderly persons with disabilities. J Am Geriatr Soc. 2008;56:711–17. doi: 10.1111/j.1532-5415.2008.01631.x. [DOI] [PubMed] [Google Scholar]
- 24.Andrade FB, Lebrão ML, Santos JL, Teixeira DS, Duarte YA. Relationship between Oral Health–Related Quality of Life, Oral Health, Socioeconomic, and General Health Factors in Elderly Brazilians. J Am Geriatr So. 2012;60:1755–60. doi: 10.1111/j.1532-5415.2012.04104.x. [DOI] [PubMed] [Google Scholar]
- 25.Petersen PE, Yamamoto T. Improving the oral health of older people: The approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33:81–92. doi: 10.1111/j.1600-0528.2004.00219.x. [DOI] [PubMed] [Google Scholar]
- 26.Luo Y, McGrath C. Oral health and its impact on the life quality of homeless people in Hong Kong. Community Dent Health. 2008;25:137–42. [PubMed] [Google Scholar]


