Abstract
Introduction:
Dental treatment is usually a poignant phenomenon for children. Projective scales are preferred over psychometric scales to recognize it, and to obtain the self-report from children.
Aims:
The aims were to evaluate treatment related fear using a newly developed fear scale for children, fear assessment picture scale (FAPS), and anxiety with colored version of modified facial affective scale (MFAS) - three faces along with physiologic responses (pulse rate and oxygen saturation) obtained by pulse oximeter before and during pulpectomy procedure.
Settings and Design:
Total, 60 children of age 6–8 years who were visiting the dental hospital for the first time and needed pulpectomy treatment were selected. Children selected were of sound physical, physiological, and mental condition. Two projective scales were used; one to assess fear - FAPS and to assess anxiety – colored version of MFAS - three faces. These were co-related with the physiological responses (oxygen saturation and pulse rate) of children obtained by pulse oximeter before and during the pulpectomy procedure.
Statistical Analysis Used:
Shapiro–Wilk test, McNemar's test, Wilcoxon signed ranks test, Kruskal–Wallis test, Mann–Whitney test were applied in the study.
Results:
The physiological responses showed association with FAPS and MFAS though not significant. However, oxygen saturation with MFAS showed a significant change between “no anxiety” and “some anxiety” as quantified by Kruskal–Wallis test value 6.287, P = 0.043 (<0.05) before pulpectomy procedure.
Conclusions:
The FAPS can prove to be a pragmatic tool in spotting the fear among young children. This test is easy and fast to apply on children and reduces the chair-side time.
Keywords: Anxiety, fear assessment picture scale, modified facial affective scale, pulse oximeter, pulpectomy
Introduction
Fear is an unpleasant emotional state consisting of psychological and psychophysiological changes in response to real external threat or danger.[1] Anxiety is an emotion similar to fear but arising without any objective source of danger. The fear and anxiety in children during the dental visit could not only affect the quality of the outcome of treatment but also the attitude of a child toward the dental profession.
Assessment of fear and anxiety involves numerous difficulties regarding technique and result interpretation.[2] Fear and anxiety being subjective components, it is advisable to obtain the response through child's own perception, which, however, is not an easy task.[3] The projective scales can aid in recognizing this emotion in children. The information obtained can help the dentist to adopt a proper behavior management technique and to gain consent from parents to apply it, as well.
Fear and anxiety bring about the physiological change in body such as increase in perspiration, breathing rate, blood pressure, heart rate, and pulse rate, which is primarily due to release of stress hormones in the blood such as cortisol, adrenaline, and nor-epinephrine. To record these physiological changes, pulse oximeter, a noninvasive technique is widely used in dentistry. It helps in real-time recording of physiological parameters such as blood pressure, pulse rate, oxygen saturation, and body temperature.[4]
Thus, the aim of the present study was to evaluate the treatment related fear using newly developed fear scale for children fear assessment picture scale (FAPS) and anxiety using colored version of modified facial affective scale (MFAS) - three faces along with physiologic responses (pulse rate and oxygen saturation) obtained by pulse oximeter before and during pulpectomy procedure.
Subjects and Methods
This was an observational cross-sectional study conducted among 60 children of age group between 6 and 8 years who visited Department of Pedodontics and Preventive Dentistry, Peoples College of Dental Sciences and Research Centre, Bhopal. Ethical clearance was obtained from the Institutional Ethical Committee of People's University, Bhopal, Madhya Pradesh.
Inclusion criteria were:
Children aged 6–8 years
It was necessarily the child's first visit to dental hospital
Children with sound physical, psychological, and mental condition.
Exclusion criteria:
Children with previous dental experience
Children with psychological or cognitive disorders
Children with systemic disease that have an effect on normal physiology.
The selected children were rated with Frankl's behavior rating scale[5] to monitor the child's behavior at the time of oral examination.
Thereafter following assessments were done:
To assess fear - FAPS [Figure 1]
To assess anxiety-Colored Version of three faces - MFAS [Figure 2]
To assess physiological response – pulse oximeter was used to record the pulse rate and oxygen saturation.
Figure 1.
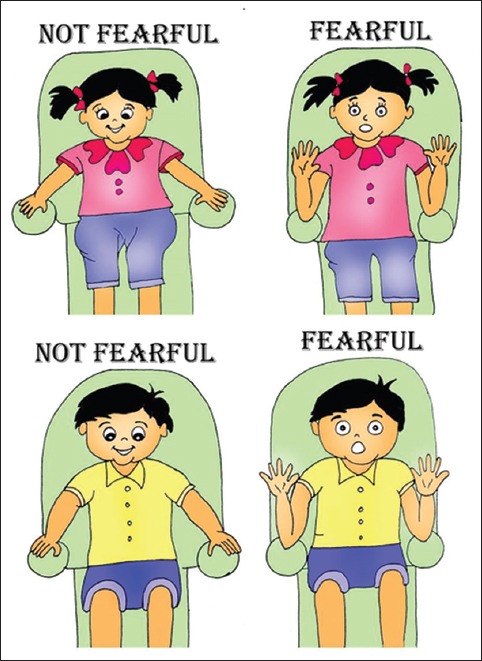
Fear assessment picture scale for girls and boys
Figure 2.

Colored Version of Modified Facial Affective Scale – three faces: 1. No Anxiety; 2. Some Anxiety; 3. Very High Anxiety
The FAPS was designed by taking a part of Klingberg's children dental fear picture test (CDFP) pointing picture,[3] and the images were drawn in frontal aspects so that the expressions can be seen. A girl or a boy cartoon in the dental chair was drawn both these figures were paired with “not fearful” and “fearful” facial expression. In “not fearful” cartoon the expressions were calm, and relaxed while in “fearful” there was change in expressions such as increased eye white area and facial grimace.
FAS visual scale could be used to evaluate the degree of child anxiety quickly and reliably.[3] So, the MFAS- three faces was drawn, colored and was digitalized for this study.
Children were assessed two times in the study
First before, pulpectomy procedure, in which, child who visited the dental hospital for the first time, and underwent oral examination with mouth mirror and probe. Appointment for pulpectomy procedure was given for the next day. Second, on the appointment day for pulpectomy procedure, assessments were done during the biomechanical preparation stage.
When the child was seated on the dental chair, his/her index finger was plugged with pulse oximeter leads. Then the child was asked the question “how do you feel to visit a dentist for oral examination?” The child had to answer the above question by pointing to the Colored Version of MFAS. Then the child was asked “what do you feel when a dentist checks your oral cavity with instruments?” This time the child was made to answer by pointing on FAPS. The physiological statistics were recorded on pulse oximeter alongside the above tests. Later, during pulpectomy phase the same questions were reframed and asked as “how do you feel to visit a dentist again?” and “what feeling did you have when the dentist gave your local anesthesia and used air-rotor on your tooth?”
The response of child on projective scales (FAPS and MFAS) and reading of pulse rate and oxygen saturation were recorded, and statistical analysis was done.
Statistical analysis
Shapiro–Wilk test showed that data were not normally distributed hence nonparametric tests namely McNemar's test, Wilcoxon signed ranks test, Mann–Whitney U-test, and Kruskal–Wallis test were applied for further data analysis. P < 0.05 was considered statistically significant. Data analysis was done using Statistical Package for Social Sciences (SPSS) v. 21.0. (IBM Corporation, 1 New Orchard Road, Armonk, New York 10504-1722, United States) for Windows.
Results
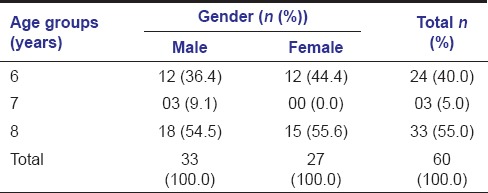
The demographic distribution of study population is presented in Table 1. The mean age of study population was 7.12 ± 0.98 year.
Table 1.
The demographic distribution of study population according to age, mean age of study population was 7.12±0.98 year
Distribution of study population according to Frankl's behavior rating scale versus projective scales (FAPS and MFAS) is presented in Table 2.
Table 2.
Distribution of study population according to Frankl's behavior rating scale versus projective scales (FAPS and MFAS)

Distribution of study population according to projective scales (FAPS and MFAS), before and during pulpectomy procedure is presented in Graph 1. With FAPS, the distribution was uniform for “fearful” and “not fearful” in both phases (McNemar's test P = 1.000 [>0.05], NS). However, with MFAS the percentage of children with “no anxiety” before pulpectomy procedure was 25%, which increased to 55% during pulpectomy phase (Wilcoxon signed ranks test Z = −1.213 P = 0.225 [>0.05], NS).
Graph 1.
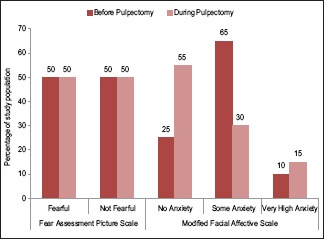
Distribution of study population according to projective scales (fear assessment picture scale and modified facial affective scale), before and during pulpectomy procedure
While comparing the pulse rate and oxygen saturation for different fear scores with FAPS before and during pulpectomy procedure is presented in Graph 2. The result were not statistically significant with Mann–Whitey U-test, for pulse rate before pulpectomy procedure P = 0.48 (>0.05), oxygen saturation P = 0.063 (>0.05), and during pulpectomy for pulse rate P = 0.063 (>0.05), oxygen saturation = 0.218 (>0.05). However, the changes were observed as in a fearful child the pulse rate increased and oxygen saturation decreased from baseline.
Graph 2.
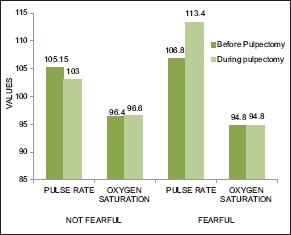
The pulse rate and oxygen saturation for different fear scores with fear assessment picture scale before and during pulpectomy procedure
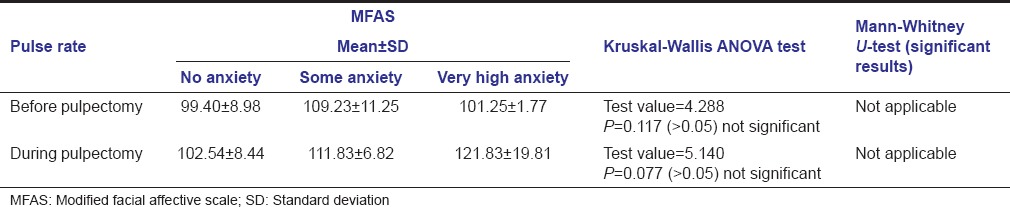
Comparison of pulse rate according to MFAS before and during pulpectomy procedure were also not significant with Kruskal–Wallis ANOVA test, test value = 4.288, P = 0.117 (>0.05) NS) before pulpectomy procedure, and test value = 5.140, P = 0.077 (>0.05) NS during pulpectomy procedure is presented in Table 3.
Table 3.
Comparison of pulse rate according to MFAS before and during pulpectomy procedure
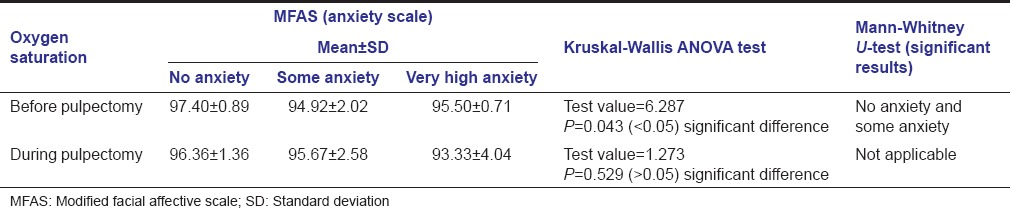
The oxygen saturation with MFAS showed significant change between “no anxiety” and “some anxiety” with Kruskal–Wallis test value = 6.287, P = 0.043 (<0.05) significant difference, before pulpectomy procedure. No difference between different anxiety levels for oxygen saturation during pulpectomy procedure P = 0.529 (>0.05) not significant is presented in Table 4.
Table 4.
Comparison of oxygen saturation with MFAS before and during pulpectomy procedure
Discussion
In literature, for assessment of fear and anxiety various scales have been documented. Questionnaires or psychometric scales such as children's fear survey schedule - dental subscale (Cuthbert and Melamed 1982), dominic questionnaire (Valla et al., 1994), koala fear questionnaire (Muris el al., 2003), etc., are beyond the cognitive skill of small children hence proxy is required. Quiles and Pedroche (2000) stated that the evaluation test must be attractive to child.[3] With the help of projective scale, a child can self-report their anxiety and fear for dental situation nonverbally. Various projective scales have been developed in past to assess fear and anxiety in children like Venham picture test by Venham 1979,[6] for children and Adolescents (PICA) by Ernst et al., 1994, pictorial anxiety test by Dubi and Schneider 2009,[7] facial image scale, Buchanan and Niven 2002,[8] CDFP by Klingberg 1995.[2] These scales may be subjected to misinterpretation unless utilized by dentists who are skilled and knowledgeable in their usage. Furthermore, they are too lengthy to be conducted and may take up to 45–60 min.[2,7,8] Looking into the drawbacks of these scales there is need of a new projective scale that is easy to apply and give results quickly without tiring the child and dentist. FAPS has been developed keeping the children's cognitive skill, their parents’ socioeconomic and educational status in mind.
Original nine face facial affective scale was designed by McGrath et al. (1996) to evaluate pain and discomfort (emotional distress) in children.[3] Quiles et al., (2013) confirm the usefulness of three face scale in detecting anxiety in lower age group children. Therefore to assess anxiety, three faces MFAS has been modified to colored version to make it attractive for children. The FAPS is used parallel with Colored Version of MFAS so that fear and anxiety can be assessed simultaneously.
Totally, 6-8 years of age group (middle childhood), are crucial as child establish a sense of identity, cognitive skills, personality, and motivation.[9] To measure the magnitudes such as the comparison, classification, correspondence, and seriation the child uses his cognitive skill to distinguish between different scores (expression) of projective scale.[3] The child should be psychologically developed to have the ability to identify the emotion and measure it correctly.[10]
This has been observed during this study that children with Frankl's positive rating who were fearful and anxious before pulpectomy procedure turned to “not fearful” and their anxiety decreased during pulpectomy procedure as these children had the willingness to adapt to the dental situation.[5] Moreover, children with Frankl's negative and definitely negative rating shows more fear and anxiety level during pulpectomy procedure, this might be due to their reluctant behavior toward the treatment procedure.[5]
In the present study, the distribution of study population according to FAPS (fear) shows the equal distribution in the “fearful” and “not fearful” categories in both, before and during pulpectomy procedure. This might have occurred due to the presence of different fear stimuli at two different treatment phases. While according to modified FAS (anxiety), before pulpectomy procedure only 25% reported “no anxiety,” that increased to 55% during pulpectomy and 65% “some anxiety” who are borderline case reduced to 30% and 10% “very high anxiety” increased to 15%. Overall the anxiety seems to be decreased in children after visiting dentist due to familiarization to the dental situation.[2] and these results also confirmed by Dedeepya et al., Venham and Gaulin-Kremer, Howitt and Stricker.[4,6,11] Although the results for FAPS were not significantly associated with pulse rate, and oxygen saturation levels but pulse rate was increased in “fearful” children from their baseline and oxygen saturation decreased due to increased stress hormones in the blood.
Before pulpectomy procedure, the oxygen saturation level showed a significant difference between “no anxiety” and “some anxiety.” Oxygen saturation was decreased in “some anxiety” but raised in “very high anxiety” this might have occurred due to hyperventilation in these children as high anxiety may cause an increase in respiration rate.[12] In contrary to this oxygen saturation was low in “very high anxiety” children during pulpectomy procedure as these children were under local anesthetic at this phase and local anesthesia may decrease the oxygen saturation level.[13] In previous studies, Rayen et al. in 2006, Shindova and Belcheva in 2013, Dedeepya et al. in 2013[4,14,15] O2 Saturation remained unaltered, and no significant changes were seen. This is due the different study design.
Conclusion
FAPS can prove to be a pragmatic tool in spotting the fear among young children. This test is easy to apply on children and does not take much time of child and dentist both. The dentist then can appoint propitious behavior management technique. The regular use of this aid needs to be enhanced and refined. The future study might investigate the extension of FAPS on larger population including lower age group and children with special health care need and its application on other treatment modalities.
Acknowledgment
The authors are grateful to Dr. Palak Shrivatava (BDS, Peoples College of Dental Science and Research Centre) and Dr. Suyog Jain (Post Graduate Student, Pedodontics and Preventive Dentistry, Rungta College of Dental Science and Research, Bhilai) for drawing and digitalizing the images for FAPS.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health. 7th ed. 2003. [Retrieved 20 May 2014]. elsevierhealth.com. Available from: http://www.medical-dictionary.thefreedictionary.com/fear .
- 2.Klingberg G, Löfqvist LV, Hwang CP. Validity of the Children's Dental Fear Picture test (CDFP) Eur J Oral Sci. 1995;103:55–60. doi: 10.1111/j.1600-0722.1995.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 3.Ortigosa Quiles JM, García-Banda García G, Chellew K, Ponsell Vicens E, Riquelme Marín A, Nicolás Carrasco MP. Identification of degrees of anxiety in children with three- and five-face facial scales. Psicothema. 2013;25:446–51. doi: 10.7334/psicothema2012.287. [DOI] [PubMed] [Google Scholar]
- 4.Dedeepya P, Nuvvula S, Kamatham R, Nirmala SV. Behavioural and physiological outcomes of biofeedback therapy on dental anxiety of children undergoing restorations: A randomised controlled trial. Eur Arch Paediatr Dent. 2014;15:97–103. doi: 10.1007/s40368-013-0070-3. [DOI] [PubMed] [Google Scholar]
- 5.Frankl SN, Shiere FR, Fogels HR. Should the parent remain in the operatory? J Dent Child. 1962;29:150–62. [Google Scholar]
- 6.Venham LL, Gaulin-Kremer E. A self-report measure of situational anxiety for young children. Pediatr Dent. 1979;1:91–6. [PubMed] [Google Scholar]
- 7.Dubi K, Schneider S. The Picture Anxiety Test (PAT): A new pictorial assessment of anxiety symptoms in young children. J Anxiety Disord. 2009;23:1148–57. doi: 10.1016/j.janxdis.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Buchanan H, Niven N. Validation of a facial image scale to assess child dental anxiety. Int J Paediatr Dent. 2002;12:47–52. [PubMed] [Google Scholar]
- 9.Bee H, Boyd D. The Developing Child. 12th ed. Boston: Pearson Education; 2009. [Google Scholar]
- 10.Besenski LJ, Forsyth SJ, von Baeyer CL. Screening young children for their ability to use self-report pain scales. Pediatr Pain Lett. 2007;9:1–7. [Google Scholar]
- 11.Howitt JW, Stricker G. Sequential changes in response to dental procedures. J Dent Res. 1970;49:1074–7. doi: 10.1177/00220345700490051201. [DOI] [PubMed] [Google Scholar]
- 12.Padma R, Goel S, Shriniwas M, Shreedhara A, Malagi S, Radhika B, et al. Comparative evaluation of oxygen saturation levels using pulse oxymeter during nonsurgical and surgical periodontal therapy in chronic periodontitis patients. Contemp Dent Pract. 2012;13:661–4. doi: 10.5005/jp-journals-10024-1205. [DOI] [PubMed] [Google Scholar]
- 13.Dutra RM, Neves IL, Neves RS, Atik E, Santos Ude P. Peripheral oxygen saturation, heart rate, and blood pressure during dental treatment of children with cyanotic congenital heart disease. Clinics (Sao Paulo) 2014;69:314–8. doi: 10.6061/clinics/2014(05)03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rayen R, Muthu MS, Chandrasekhar Rao R, Sivakumar N. Evaluation of physiological and behavioral measures in relation to dental anxiety during sequential dental visits in children. Indian J Dent Res. 2006;17:27–34. doi: 10.4103/0970-9290.29895. [DOI] [PubMed] [Google Scholar]
- 15.Shindova M, Belcheva A. The effect of parental presence on the dental anxiety during clinical examination in children aged 6-12 years. J of IMAB. 2013;19:435–8. [Google Scholar]


