Abstract
Aims:
The aim of this study was to assess oral health-related quality of life (OHRQoL) using short form (SF) of child oral health impact profile (COHIP) in children aged 11–15 years who sought orthodontic treatment. A comparison was done between these children and age-matched peers who never had or sought orthodontic treatment.
Methodology:
This cross-sectional study included 227 children aged 11–15 years. A total of 110 participants had sought orthodontic treatment at KSR Institute of Dental Science and Research (orthodontic group) and 117 participants from a nearby school who had never undergone or sought orthodontic treatment (comparison group). OHRQoL was assessed with the SF of the COHIP, and malocclusion severity was assessed with the index of orthodontic treatment needs. Data presentation and statistical analysis were performed with the Statistical Package for the Social Sciences Software (Version 19, SPSS, Chicago, IL, USA). The Chi-square test and Fischer exact tests were used to analyze the qualitative data.
Results:
Children with little to borderline treatment needs have a better quality of life when compared to children with definitive treatment needs (P = 0.049). No statistically significant difference in COHIP-SF scores was found between boys and girls (P > 1.000). In the orthodontic group, children with little to borderline treatment needs were 4.8 times (P = 0.037) more likely to report better OHRQoL when compared to children with definitive treatment needs.
Conclusion:
Children who sought orthodontic treatment had lower quality of life scores than those who never had or never sought treatment.
Keywords: Child oral health impact profile-short form scale, oral health-related quality of life, index of orthodontic treatment need index
Introduction
The constitution of the World Health Organization defines quality of life (QoL) as individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.[1] Dealing only with the disease and not the other domains such as environmental, psychosocial, and cultural influences is one of the principal limitations of biomedical paradigm.[2] In recent years, there has been a broad paradigm shift from medical model of health care to socioenvironmental model, which involves a change in aspects that constitute the health and the strategies necessary to construct it.[3] Earlier, there was a tendency to treat oral cavity as an autonomous anatomical entity. This approach was challenged by socioenvironmental model of health care necessitating the understanding of physical and social environments as one of the major determinants of health status.[4] As a result, an atomistic or reductionist way of thinking was replaced by a more holistic perspective, thereby enhancing the health outcomes and QoL of an individual.[5]
Oral health related QoL (OHRQoL) is a rapidly emerging phenomenon, which has surfaced over the past two decades. Locker and Allen defined OHRQoL as “the impact of oral diseases and disorders on aspects of everyday life that a patient or person values, which are of sufficient magnitude, in terms of frequency, severity or duration to affect their experience, and perception of their life overall.”[6] In other words, OHRQoL is “a multidimensional construct that reflects (among other things) people's comfort when eating, sleeping, and engaging in social interaction; their self-esteem; their satisfaction with respect to their oral health.”[7] Various studies have demonstrated that oral diseases can have significant influences on the QoL of individuals.[8,9,10] Although common oral diseases are not life-threatening, their outcomes may influence the overall well-being of the individuals. This has resulted in greater clinical focus on improving QoL as a major objective of dental care for conditions like orthodontic problems.[11]
The impact of dental esthetics on social acceptance and self-concept dictates the need for evaluating OHRQoL among orthodontic patients. Zhang et al. have shown that patients with malocclusion can develop feelings of self-consciousness and shame about their dental condition or feel shy in social contexts.[12] Nevertheless, a malocclusion can be perceived differently by the affected person, and a person's self-awareness of the malocclusion might not be related to its severity. A variety of index systems have been developed to measure OHRQoL. Among these, child oral health impact profile (COHIP) and its short form (SF) is the first children's questionnaire to incorporate positive and negative health impacts.[13] With its five domains (oral health, functional well-being, social-emotional well-being, school environment, and self-image), the SF of COHIP is an established instrument for measuring OHRQoL in children and adolescents.[14] The aim of this study was to assess OHRQoL using SF of COHIP in children aged 11–15 years who sought orthodontic treatment. A comparison was also done between these children and age-matched peers who were not seeking orthodontic treatment.
Methodology
This cross-sectional study was conducted in the Department of Pedodontics and Preventive Dentistry, KSR Institute of Dental Science and Research (KSRIDSR), Tiruchengode, Tamil Nadu, India from June 2014 to October 2014. The study protocol was approved by the Institutional Review Board and the ethical committee of KSRIDSR. Children with chronic medical conditions, craniofacial abnormalities, untreated severe dental caries, and poor periodontal health status were excluded from the study to prevent possible confounding bias as these conditions could influence their QoL.
Children in the age range of 11–15 years participated in the study. Totally, 115 children who sought orthodontic treatment at KSRIDSR constituted the orthodontic group. Informed consent was obtained from the parents who accompanied their children to the hospital. Only those children who had the consent to participate were included into this study. Five parents did not allow their children to participate in the study (4.3% loss), and hence the orthodontic group had a final sample size of 110 children. All the children in the orthodontic group belonged to private schools in and around Tiruchengode. After the inclusion of children into the orthodontic group, the participants in the comparison group were recruited. This group comprised of 125 age-matched children from a private school in Tiruchengode. The type of school can be used as an alternative indicator for socioeconomic status.[15] Hence, matching based on age, place, and socioeconomic status was possible in this study. The purpose of the study was explained to the school authorities, and their approval was obtained. A consent form was sent to each parent along with a question, asking whether their children had already sought or undergone any kind of orthodontic treatment. Eight children were excluded as they already had undergone orthodontic treatment. Therefore, the comparison group consisted of 117 children (6.4% loss). Hence, the final study sample consisted of 227 children belonging to two groups: The orthodontic group (110) and the comparison group (117). This cross-sectional study carried out over a period of 4 months used a convenience sampling method. Care was taken to include a sample size similar to the study done by Feu et al.,[9] as this sample size was sufficient to estimate the difference between the comparison group and the orthodontic group, with a power of 80% at a significance level of 0.05.
The OHRQoL of all these children (OHRQoL) was assessed by SF of COHIP-SF. It consists of 19 items (17 negative, 2 positive) forming five conceptually distinct domains. The questionnaire was designed to be completed in 10–15 min. Any difficulties faced by the child in understanding the questions were clarified by the primary investigator (PI). For the 2 positive items, ordinal responses were recorded as “never = 0,” “almost never = 1,” “sometimes = 2,” “fairly often = 3”, and “almost all of the time = 4.” Scoring for the 17 negatively worded items was reversed. Higher COHIP scores reflected more positive OHRQoL while lower scores reflected lower OHRQoL.
After completion of the questionnaires, children were clinically examined to assess malocclusion severity and orthodontic treatment needs using dental health component (DHC) of the index of orthodontic treatment need (IOTN). The malocclusion severity was based on the evaluation of five occlusal traits: Missing teeth, overjet, crossbite, displacements of contact points, and overbite. The most severe occlusal trait was identified for each person, and children were categorized according to it. The DHC of IOTN consists of five grades that have been grouped following validation into Grades 1 and 2 representing “slight or no need for treatment,” Grade 3 representing “borderline” cases, and Grades 4 and 5 representing those in “definitive need of orthodontic treatment.”
Students in the comparison group were examined in their school premises under natural light with adequate illumination (American Dental Association Type III examination). Clinical examination for all the children was done by the PI. To test intra-examiner agreement, 25 children were re-examined approximately 6 weeks later after their initial examination (10 from the comparison group and 15 from the orthodontic group).
Data presentation and statistical analysis were performed with the Statistical Package for the Social Sciences statistical package (Version 19, SPSS, Chicago, IL, USA). The Chi-square test and Fischer exact test were used to analyze the qualitative data. Significance level was set at 0.05. Kappa statistics was used to evaluate the consistency of intra-examiner reliability.
For COHIP-SF analysis, all the 19 ordinal responses were summed to produce an overall score that could range from 0 to 76, with higher score indicating better OHRQoL. In the statistical analysis, COHIP-SF scores were transformed into a dichotomous variable using a cut-off value, the median for the whole sample (n = 227). Scores higher than median value indicate better QoL, while lower scores indicate lower QoL. A score of sometimes, fairly often, and almost all of the time was used to indicate participants who had experienced at least some oral health impact. For the DHC scores (range, 1–5), subjects with scores >3 were considered to have an objective orthodontic treatment need. These determinations of orthodontic treatment needs were based on the cut-off points for index dichotomization of Mandall et al.[16]
Results
Intra-examiner reliability was very good (Kappa, 0.91), indicating substantial consistency in DHC assessment. The median value for the whole sample (n = 227) was 59. Thus, COHIP-SF scores higher than 59 were considered to reflect positive OHQoL and those lower than or equal to 59 indicated lower OHQoL. The mean age of the orthodontic group and comparison group were 12.99 ± 1.36 years and 13.01 ± 1.41, respectively (P = 0.91).
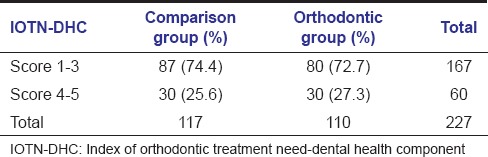
Table 1 shows the distribution of study sample, according to gender and treatment needs. Table 2 shows the distribution of DHC component of IOTN in both the groups based on index dichotomization.
Table 1.
Distribution of study sample according to gender and treatment needs
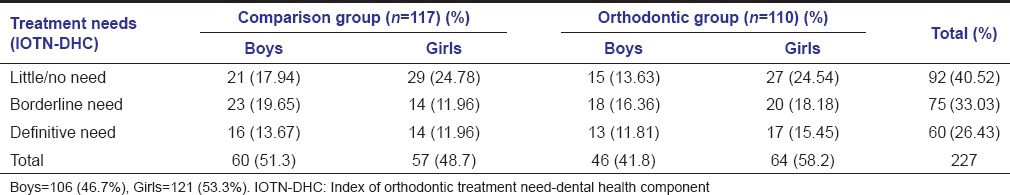
Table 2.
Distribution of DHC component of IOTN in comparison and orthodontic group
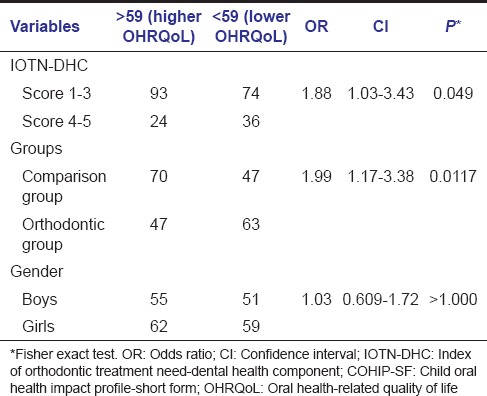
Overall, children with little to borderline treatment needs have better QoL when compared to children with definitive treatment needs (odds ratio [OR] = 1.88, confidence interval [CI] = 1.03–3.43, P = 0.049). COHIP-SF scores were significantly higher in comparison group when compared to children who seek orthodontic treatment (OR = 1.99, CI = 1.17–3.38, P = 0.0117). However, no statistically significant difference in CHOIP-SF scores was found between boys and girls (OR = 1.03, CI = 0.609–1.72, P > 1.000) as shown in Table 3.
Table 3.
Association between IOTN-DHC, groups, gender, and COHIP-SF scores
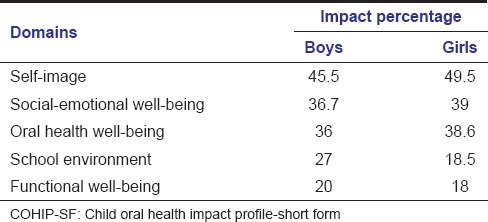
In the orthodontic treatment group, children with IOTN-DHC scores of 1–3 were 4.8 times (OR = 4.87, CI = 2.039–11.69, P = 0.037) more likely to report better OHRQoL when compared to children with definitive treatment needs (Scores 4–5). Even though girls reported better COHIP-SF scores than the boys, the difference was not statistically significant (OR = 1.03, CI = 0.478–2.22, P > 1.000) [Table 4]. Self-image, social-emotional well-being, and oral health well-being were the most negatively affected domains in both boys and girls. However, girls were comparatively more negatively affected than the boys [Table 5].
Table 4.
Association between IOTN-DHC, gender and COHIP-SF scores within the orthodontic group
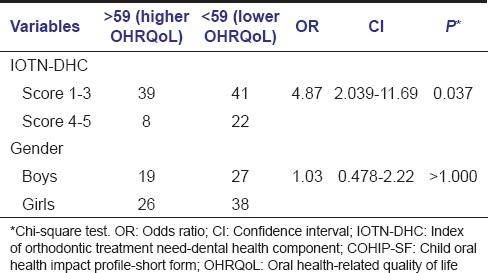
Table 5.
Impact percentage of boys and girls in the orthodontic group on the specific domains of COHIP-SF
Discussion
OHRQoL is a multidimensional phenomenon that records an individual's well-being and perceptions. It can play an important role in understanding subjective evaluations. The subjective evaluation of an individual in healthcare decision-making process leads to a change in dynamics of clinical practice and health outcomes.[17] OHRQoL instruments may be used in clinical practice as they reflect “a better understanding of treatment needs and outcomes from the patient's perspective.”[18]
This cross-sectional study was done to assess the relationship between OHRQoL and orthodontic treatment needs in adolescents with reliable and valid instruments: The COHIP-SF and the DHC of IOTN. Various other instruments are available to measure the QoL in children. Michigan OHRQoL[19] and the early childhood oral health impact score[20] are targeted for preschool children. The child perceptions questionnaire (CPQ) was the first instrument created for school-aged children. It has been validated for children 8–10 years (CPQ8-10)[21] and 11–14 years (CPQ11-14).[22] In 2011, the pediatric OHRQoL was created and had been validated for use in preschool, school-aged, and preteen children.[23] None of these instruments includes positive and negative items to assess the QoL. As both are needed to encompass all aspects of well-being, the COHIP scale was introduced.
The original COHIP, developed by Broder et al. in 2007, consists of 34 items (28 negative, 6 positive).[24] Later in 2012, a SF of COHIP was developed, which contains 19 items (17 negative, 2 positive). Reliability and validity testing verified that the COHIP-SF had good psychometric properties and can be used as a stable instrument to measure OHRQoL across school-aged pediatric populations.[14] Even though COHIP-SF is suitable for ages between 8 and 15 years, children in the age range of 11–15 years were selected for this study, as they are capable of abstract thinking, reckoning about timing of past events, and correlating them with their experiences.[25]
The IOTN was described by Brook and Shaw and modified by Richmond (1990).[26] It consists of two components, DHC and esthetic component and is known to provide reliable and practical results. In various populations, malocclusion was examined using the IOTN, and the reproducibility of IOTN has been proven.[27,28] However, the major disadvantage of this index is risk of insensitivity and its inability to map the minor irregularities about which a patient is deeply concerned.[29] Only DHC of IOTN was used in this study to ascertain the need for orthodontic treatment.
Similar to the previous literature, more girls sought dental treatment than boys during the recruitment period of this study.[30,31] It was not surprising to find that those children who sought orthodontic treatment had more negative OHRQoL impacts since these conditions may cause discomfiture at school and other social situations.[32] In this study, orthodontic treatment needs had almost similar impact on the OHRQoL of both males and females. This is in concordance with the study done by Feu et al.[9] and in contrast to the studies done by Tung and Kiyak[33] and Oliveira and Sheiham[11] who demonstrated that children with definitive treatment need had no overall health impact. A study done by Calis et al. demonstrated that boys scored significantly lower (higher impact) on the subscales “oral symptoms” and “emotional well-being” than girls.[34] However, in this study, impact was higher in girls than boys. The domains that were more negatively affected were in the order of self-image, social-emotional well-being, and oral well-being. Their greatest impact was at the psychosocial level. Feu et al. have shown that the individual personality behavior probably has an impact on OHQOL and making negative impacts might not be dependent on malocclusion severity.[9]
Esthetics and appearance assume paramount importance during adolescence. Children who seek orthodontic treatment are concerned of improving their appearance and social acceptance. Apart from improving oral function, health, and esthetics, it is important to enhance self-esteem and QoL of an individual through orthodontic treatment.[33] The OHRQoL questionnaire, as a part of treatment planning, could help to identify the individuals’ perceptions and thereby enhance their satisfaction to the treatment outcome.
Conclusion
Within the limitations of this cross-sectional study, it could be demonstrated that children who sought orthodontic treatment had lower QoL than those who had never sought treatment. There was no significant difference in the impact on OHRQoL between boys and girls.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Orley J, Kuyken W, editors. Quality of Life Assessment: International Perspectives. Heidelberg: Springer Verlag; 1994. The WHOQOL Group. The development of the World Health Organization quality of life assessment instrument (the WHOQOL) pp. 41–60. [Google Scholar]
- 2.Allen PF. Assessment of oral health related quality of life. Health Qual Life Outcomes. 2003;1:40. doi: 10.1186/1477-7525-1-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nettleton S. Cambridge: Polity Press; 1995. The Sociology of Health and Illness. [Google Scholar]
- 4.Locker D, Allen F. What do measures of ‘oral health-related quality of life’ measure? Community Dent Oral Epidemiol. 2007;35:401–11. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 5.Coulter ID, Marcus M, Atchison KA. Measuring oral health status: Theoretical and methodological challenges. Soc Sci Med. 1994;38:1531–41. doi: 10.1016/0277-9536(94)90115-5. [DOI] [PubMed] [Google Scholar]
- 6.Locker D. Oral health and quality of life. Oral Health Prev Dent. 2004;2(Suppl 1):247–53. [PubMed] [Google Scholar]
- 7.Rockville, Maryland: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institute of Health (NIH Publication 00-4713); 2000. Oral Health in America: A Report of the Surgeon General; p. 7. [Google Scholar]
- 8.Klages U, Bruckner A, Zentner A. Dental aesthetics, self awareness, and oral health-related quality of life. Eur J Orthod. 2002;24:53–9. doi: 10.1093/ejo/26.5.507. [DOI] [PubMed] [Google Scholar]
- 9.Feu D, de Oliveira BH, de Oliveira Almeida MA, Kiyak HA, Miguel JA. Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop. 2010;138:152–9. doi: 10.1016/j.ajodo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 10.Manjith CM, Karnam SK, Manglam S, Praveen MN, Mathur A. Oral health-related quality of life (OHQoL) among adolescents seeking orthodontic treatment. J Contemp Dent Pract. 2012;13:294–8. doi: 10.5005/jp-journals-10024-1140. [DOI] [PubMed] [Google Scholar]
- 11.de Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31:20–7. doi: 10.1179/146531204225011364. [DOI] [PubMed] [Google Scholar]
- 12.Zhang M, McGrath C, Hägg U. The impact of malocclusion and its treatment on quality of life: A literature review. Int J Paediatr Dent. 2006;16:381–7. doi: 10.1111/j.1365-263X.2006.00768.x. [DOI] [PubMed] [Google Scholar]
- 13.Sischo L, Broder HL. Oral health-related quality of life: What, why, how, and future implications. J Dent Res. 2011;90:1264–70. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broder HL, Wilson-Genderson M, Sischo L. Reliability and validity testing for the child oral health impact profile-reduced (COHIP-SF 19) J Public Health Dent. 2012;72:302–12. doi: 10.1111/j.1752-7325.2012.00338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Piovesan C, Pádua MC, Ardenghi TM, Mendes FM, Bonini GC. Can type of school be used as an alternative indicator of socioeconomic status in dental caries studies? A cross-sectional study. BMC Med Res Methodol. 2011;11:37. doi: 10.1186/1471-2288-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mandall NA, Wright J, Conboy F, Kay E, Harvey L, O’Brien KD. Index of orthodontic treatment need as a predictor of orthodontic treatment uptake. Am J Orthod Dentofacial Orthop. 2005;128:703–7. doi: 10.1016/j.ajodo.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 17.Inglehart MR, Bagramian RA, editors. Chicago: Quintessence Publishing Co., Inc; 2002. Oral Health-Related Quality of Life. [Google Scholar]
- 18.Awad M, Al-Shamrany M, Locker D, Allen F, Feine J. Effect of reducing the number of items of the Oral Health Impact Profile on responsiveness, validity and reliability in edentulous populations. Community Dent Oral Epidemiol. 2008;36:12–20. doi: 10.1111/j.1600-0528.2006.00364.x. [DOI] [PubMed] [Google Scholar]
- 19.Filstrup SL, Briskie D, da Fonseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: Child and parent perspectives. Pediatr Dent. 2003;25:431–40. [PubMed] [Google Scholar]
- 20.Pahel BT, Rozier RG, Slade GD. Parental perceptions of children's oral health: The early childhood oral health impact scale (ECOHIS) Health Qual Life Outcomes. 2007;5:6. doi: 10.1186/1477-7525-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26:512–8. [PubMed] [Google Scholar]
- 22.Locker D, Jokovic A, Tompson B. Health-related quality of life of children aged 11 to 14 years with orofacial conditions. Cleft Palate Craniofac J. 2005;42:260–6. doi: 10.1597/03-077.1. [DOI] [PubMed] [Google Scholar]
- 23.Huntington NL, Spetter D, Jones JA, Rich SE, Garcia RI, Spiro A., 3rd Development and validation of a measure of pediatric oral health-related quality of life: The POQL. J Public Health Dent. 2011;71:185–93. [PMC free article] [PubMed] [Google Scholar]
- 24.Broder HL, McGrath C, Cisneros GJ. Questionnaire development: Face validity and item impact testing of the child oral health impact profile. Community Dent Oral Epidemiol. 2007;35(Suppl 1):8–19. doi: 10.1111/j.1600-0528.2007.00401.x. [DOI] [PubMed] [Google Scholar]
- 25.Hetherington EM, Parke RD, Locke VO. Child Psychology: A Contemporary Viewpoint. 5th ed. New York: McGraw-Hill; 1999. [Google Scholar]
- 26.Brook PH, Shaw WC. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11:309–20. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 27.So LL, Tang EL. A comparative study using the occlusal index and the index of orthodontic treatment need. Angle Orthod. 1993;63:57–64. doi: 10.1043/0003-3219(1993)063<0057:ACSUTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Burden DJ, Holmes A. The need for orthodontic treatment in the child population of the United Kingdom. Eur J Orthod. 1994;16:395–9. doi: 10.1093/ejo/16.5.395. [DOI] [PubMed] [Google Scholar]
- 29.Shaw WC, Richmond S, O’Brien KD. The use of occlusal indices: A European perspective. Am J Orthod Dentofacial Orthop. 1995;107:1–10. doi: 10.1016/s0889-5406(95)70151-6. [DOI] [PubMed] [Google Scholar]
- 30.Al Yami EA, Kuijpers-Jagman AM, Van’t Hof MA. Orthodontic treatment need prior to orthodontic treatment and 5 years post retention. Community Dent Oral Epidemiol. 1998;26:421–7. doi: 10.1111/j.1600-0528.1998.tb01982.x. [DOI] [PubMed] [Google Scholar]
- 31.Locker D, Jokovic A, Clarke M. Assessing the responsiveness of measures of oral health-related quality of life. Community Dent Oral Epidemiol. 2004;32:10–8. doi: 10.1111/j.1600-0528.2004.00114.x. [DOI] [PubMed] [Google Scholar]
- 32.Klages U, Zentner A. Dentofacial aesthetics and quality of life. Semin Orthod. 2007;13:104–15. [Google Scholar]
- 33.Tung AW, Kiyak HA. Psychological influences on the timing of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1998;113:29–39. doi: 10.1016/S0889-5406(98)70274-4. [DOI] [PubMed] [Google Scholar]
- 34.Calis EM, Geels LM, Prahl-Andersen B, Zentner A. Oral health-related quality of life and dental esthetics in Amsterdam schoolchildren. J Dent Child (Chic) 2009;76:130–5. [PubMed] [Google Scholar]


