BACKGROUND
As part of the Clinical Learning Environment Review (CLER) program, the Accreditation Council for Graduate Medical Education (ACGME) core competency in Practice-Based Learning and Improvement (PBLI) will encompass attributes of the institutional environment for quality improvement (QI). Currently, the depth and breadth of QI education curricula varies widely across surgical residency programs. There is a clear need to better understand structural and programmatic factors that facilitate learning about and implementation of improvement programs for and by residents.1
Because of the increasing emphasis on delivering high quality care, there is a pressing need to train the next generation of physician leaders with the necessary skills to deliver competent patient care and promote system-wide improvements. As the CLER program has recognized, QI training will be dependent on faculty development to support these areas and a clinical learning environment infrastructure that engages residents in improvement efforts.
OBJECTIVE
In this context, we developed and piloted a novel QI program entitled Team Action Projects in Surgery (TAPS) at the University of Michigan. This multi-level team-based approach integrates didactic coursework in QI methodology with practical experience via meaningful QI projects based on observed clinical problems or gaps in quality. Other tangible benefits include didactic and practical training for faculty mentors (“training the trainer”), development of leadership skills for residents, and an opportunity for students to gain clinical and research experience in surgery (“feeding the academic pipeline”).
METHODS
We structured TAPS using a framework of QI training across all levels of learners. The program embodied problem-based learning: the didactic component was based on “managing to learn” Lean principles while the practical component included resident-initiated and led improvement projects. Structurally, each TAPS team consists of one or two faculty mentors, one or two residents, and a variable number of medical students and/or undergraduate/graduate students (e.g., Nursing, Engineering). The pilot project took place during residents’ dedicated academic development time (ADT), which is between the third and fourth clinical years. Residents self-identified a quality improvement target based on their clinical interests. With selected faculty mentors, each project was tailored and appropriately scoped to meet the educational needs of the individual resident while fulfilling a stated QI goal.
TAPS allowed us to “train the trainers,” since one of the challenges of implementing quality programs includes ensuring a cadre of experienced faculty mentors for QI projects. All team members participated in a formalized education program in Lean principles as a conceptual scaffold for the TAPS project2. The identified problem (“burning platform”) is extensively investigated with the creation of an A3 to guide understanding of the current state.3 An A3 is a concise problem-solution tool, which happens to be written on an 11”×17” piece of paper, (A3 in international paper sizing guidelines) serving as a guide to the quality improvement process. Through the process of A3 development, teams went to the “gemba” to collect data and to develop a deep understanding of the issues underlying the problem they sought to address. This allowed them to then define potential solutions.
A unique aspect of TAPS includes opportunities for longitudinal development of the “academic pipeline.” By leveraging manpower from an active surgery student research program, intelligent but clinically uninitiated learners gained a valuable clinical experience in surgery while affording our residents the opportunity to develop leadership skills.
RESULTS
In the first year of the program, five pilot TAPS projects were initiated, spanning a broad range of clinical and educational arenas. A brief description of each project is listed below.
Living Related Kidney Donor Program
Enhanced-recovery protocols are gaining momentum for many general surgery procedures. To date, no such protocols have been implemented in transplantation surgery. To address post-operative pain issues and improve length of stay following living kidney donation, an enhanced-recovery protocol was developed to address this need. Working with a medical student and a nursing student, the resident lead on this project developed and implemented such a protocol. Early results show decreased narcotic use, decreased post-operative pain scores and a significant reduction in post-operative length of stay.
Improving Acute Care Surgical Consults
A resident team identified the lack of efficient management of emergent, non-trauma surgical consults as a quality improvement area with substantial room for improvement. To begin this project, the resident-led team developed a Value Stream Map framework for analyzing consults to the acute care surgery service4. Working with institutional Lean process facilitators, the residents conducted qualitative research with medical students and senior industrial engineering students to identify the components of the surgical consult process that most contribute to physician dissatisfaction and increased delays for urgent or emergent consults. Three key areas for initial QI efforts were identified: reducing redundancy in the paging system, creating and codifying consult guidelines, and developing a department-wide policy for managing readmissions. Early feedback following changes to these processes has been positive.
Optimizing venous thromboembolism (VTE) prophylaxis
Although sequential-compression device (SCD) use in conjunction with chemical thromboprophylaxis has been shown to reduce VTE in post-surgical patients,5 SCD compliance in general care post-operative patients at our institution was noted to be poor. Based on early observations, this was hypothesized to be due to the size, weight and need for external power of currently used devices. To determine if compliance could be improved through the use of battery-powered mobile units, a randomized controlled trial was undertaken in post-surgical patients on two general care floors. Initial results show a significant improvement in compliance with use of battery-powered devices.
Standardizing C-Diff Treatment
Clinical observations of faculty and residents revealed large variations in the management of hospital-acquired Clostridium Difficile infection among different clinical services throughout our institution, despite clearly published, institution-specific, clinical practice guidelines. In this project, a resident-led team conducted chart reviews to assess appropriateness of therapy and discovered that a significant portion did not receive appropriate treatment. Furthermore, inappropriate therapy was associated with increased mortality. Currently, the team is developing a pager-notification system to alert clinicians when patients are receiving inappropriate therapy, and to offer treatment alternatives.
Understanding Variation in Laparoscopic Cholecystectomy Operative Duration
Data from the statewide regional quality collaborative revealed our institution was a high outlier in operative times of laparoscopic cholecystectomy, and showed significant inter-surgeon variability. Given the implications of prolonged operative times on clinical outcomes and institutional costs, a prospective observational study was initiated to better understand factors that contribute to increased times, and identify potential targets for quality improvement. A member of the team observed every elective and non-elective procedure performed at the institution to collect primary data, which is currently pending analysis.
DISCUSSION
TAPS is a multilevel educational initiative that meets the important goals of training residents in the principles of QI and providing practical experiences in developing and implementing improvement projects. Five projects spanning a range of clinical issues have been piloted and demonstrate not only the feasibility of this program but also the positive effects that this team-based approach can have on training for all learners and on overall improvements in quality of care based on implementation of the program. Post hoc evaluation of the pilot program residents demonstrated a high level of satisfaction among participating residents, with an average score of 4.1 on a 5-point Likert scale assessing the value of the multi-level TAPS approach and resident-initiated QI projects.
From our pilot work, we learned that identification of an appropriately scoped clinical project can be challenging, but we expect that this process will improve with experience at the faculty level. Thus far, implementation of QI solutions has gone well, but sustainability has yet to be tested. A future challenge will be maintaining the academic pipeline required for the actual work of the improvement projects, but with extremely positive feedback from our students, we do not anticipate a shortage of participants.
Early experience with TAPS has fostered faculty development in QI training, as well as provided a unique clinical research experience for all learners. A multi-level team approach to teaching and implementing QI principles appears to be a novel and effective way to enhance educational curriculum in PBLI.
Figure 1.
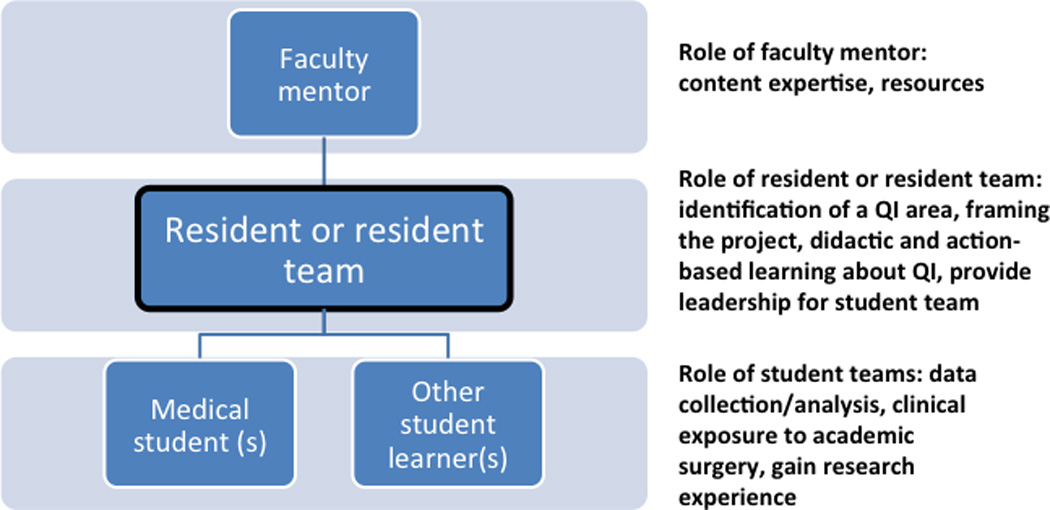
Team Action Projects in Surgery (TAPS) schema illustrating a multi-level approach to quality improvement (QI) projects.
Acknowledgments
Source of Funding: This work is supported by a grant from The Third Century Initiative (TCI) from the University of Michigan Office of the Provost.
Footnotes
Conflict of Interest: None of the authors have any conflicts of interest to disclose
REFERENCES
- 1.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system--rationale and benefits. The New England journal of medicine. 2012 Mar 15;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 2.Shook J. Managing to Learn: Using the A3 management process to solve problems, gain agreement, mentor, and lead. Cambridge, MA: Lean Enterprise Institute; 2010. [Google Scholar]
- 3.Collar RM, Shuman AG, Feiner S, et al. Lean management in academic surgery. J Am Coll Surg. 2012 Jun;214(6):928–936. doi: 10.1016/j.jamcollsurg.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Rother M, Shook J Lean Enterprise Institute. Learning to see : value stream mapping to create value and eliminate muda. 1.3 ed. Brookline, MA: Lean Enterprise Institute; 2003. [Google Scholar]
- 5.Henke PK, Arya S, Pannucci C, et al. Procedure-specific venous thromboembolism prophylaxis: a paradigm from colectomy surgery. Surgery. 2012 Oct;152(4):528–534. doi: 10.1016/j.surg.2012.07.012. discussion 534-526. [DOI] [PMC free article] [PubMed] [Google Scholar]


