To the Editor—Sood et al modeled the effects of a “test-and-treat” program for the men who have sex with men population in Los Angeles [1]. Relative to the status quo, this deterministic epidemiologic model predicted that “test-and-treat” could lead to a 34% reduction in new human immunodeficiency virus (HIV) infections, a 19% reduction in deaths, and a 39% reduction in new AIDS cases. However, it also predicted that the benefits from this expansion of HIV therapy would be counterbalanced by an 89% increase (from 4.79% to 9.06%) in the prevalence of multidrug resistance (MDR) over 10 years. They conclude that the risks of developing widespread MDR may exceed the benefits derived from “test and treat,” but that much of the benefit could derive from larger-scale testing alone.
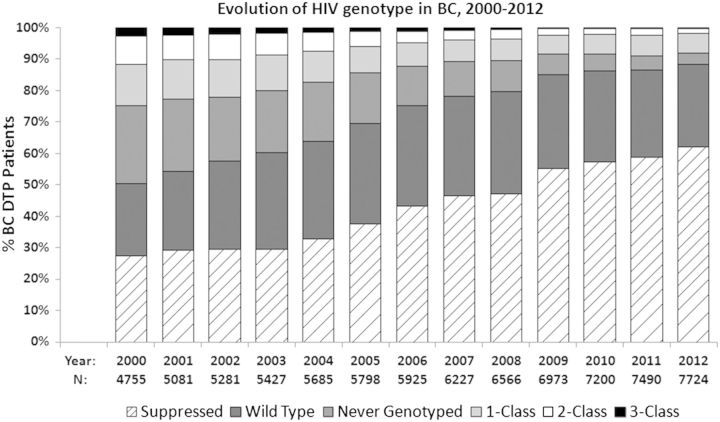
However, actual data collected during 12 years of province-wide follow-up in British Columbia, Canada, during a period of treatment expansion [2] do not support the model's conclusions regarding drug resistance (Figure 1). On the contrary, we now observe a much lower proportion of MDR in 2012 in comparison to 2000, despite the number of patients on therapy expanding from 4755 to >7700 during the same period.
Figure 1.
In 2012, 88% of British Columbia Drug Treatment Program (BC DTP) patients had either undetectable viremia (<50 copies/mL) or wild-type human immunodeficiency virus (HIV). Individuals with resistance to 2 or more antiretroviral (ARV) drug categories made up <2% of the HIV-positive population engaged in care in BC, down from 12% in 2000. Patients were grouped by the total number of drug resistance categories (nucleoside reverse transcriptase inhibitor, nonnucleoside reverse transcriptase inhibitor, protease inhibitor) observed in genotypes performed in each calendar year. In years where drug resistance was not assessed, patients were assigned the previous year's result. “Suppressed” are patients with undetectable plasma viral load (pVL; <50 copies/mL) throughout the entire year. “Never Genotyped” are ARV-naive persons or ARV-experienced patients with no previous genotypes. Annual Ns are all patients engaged in care in the BC DTP who had 1 or more pVL measurements that year. Estimates of HIV-positive persons not known to the BC DTP, including HIV-positive persons unaware of their serostatus, are not included. Abbreviations: BC, British Columbia; DTP, Drug Treatment Program; HIV, human immunodeficiency virus.
Part of the discordance between our data and Sood et al's model may be due to the parameters used for resistance development and the definition of “MDR” used [1, 3], both of which may be outdated. The rates of development and the clinical significance of HIV resistance have both declined as more and better HIV medications have led to improved rates of HIV suppression [4]. Furthermore, the definition of “MDR” used and its estimated rate of development appear to consist of resistance to >1 drug or drug class—for example, resistance to merely lamivudine/emtricitabine and/or nonnucleoside reverse transcriptase inhibitors [1, 3], rather than pandrug resistance. Obviously any resistance is of concern, but some levels of resistance are less clinically threatening.
More than 25 approved antiretrovirals in 6 classes exist, and regimens with fully active drugs can be constructed even for patients harboring MDR strains resistant to 2 or more drug classes. Currently, few patients in British Columbia harbor strains with 3-drug-class resistance, let alone to all drugs from all 6 classes.
In addition, even if the estimates of Sood et al for MDR in their model were correct and the proportion of cases of MDR would increase, the total number of cases of MDR would increase only slightly. The relatively small increase in the number of cases of MDR would be a very small price to pay for preventing approximately 18 000 new infections and 15 000 deaths.
“Test-and-treat” remains a very promising strategy for the control of HIV and AIDS. The whole point of developing the array of effective antiretrovirals now available was to have a variety of options to treat the vast majority of HIV-infected patients who require these therapies for their own individual health benefit (and reap the secondary societal benefits described by Sood et al), rather than reserve these therapies due to a theoretical, possibly overemphasized, concern about the future effectiveness of the medications.
Notes
Acknowledgments. We acknowledge the Government of Canada for the Vanier Canada Graduate Scholarship granted to C. J. B. and to the Canadian Institutes of Health Research (CIHR) for the GlaxoSmithKline–CIHR Research Chair awarded to P. R. H. We also thank the patients of the Drug Treatment Program and the staff at the BC Centre for Excellence for HIV/AIDS for maintaining and updating our database.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Sood N, Wagner Z, Jaycocks A, Drabo E, Vardavas R. Test-and-treat in Los Angeles: a mathematical model of the effects of test-and-treat for the men who have sex with men population in Los Angeles County. Clin Infect Dis. 2013;56:1789–96. doi: 10.1093/cid/cit158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montaner JS, Lima VD, Barrios R, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–9. doi: 10.1016/S0140-6736(10)60936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith RJ, Okano JT, Kahn JS, Bodine EN, Blower S. Evolutionary dynamics of complex networks of HIV drug-resistant strains: the case of San Francisco. Science. 2010;327:697–701. doi: 10.1126/science.1180556. [DOI] [PubMed] [Google Scholar]
- 4.Gill VS, Lima VD, Zhang W, et al. Improved virological outcomes in British Columbia concomitant with decreasing incidence of HIV type 1 drug resistance detection. Clin Infect Dis. 2010;50:98–105. doi: 10.1086/648729. [DOI] [PMC free article] [PubMed] [Google Scholar]