Abstract
Cardiac resynchronization therapy with an implantable cardioverter-defibrillator (CRT-D) is the preferred treatment for patients with severe heart failure, dyssynchrony, and an increased risk of sudden cardiac death or for primary ventricular arrhythmia survivors. Rarely, left ventricular epicardial pacing can induce ventricular tachyarrhythmia rather than a beneficial effect. We describe an ischemic cardiomyopathy patient who underwent CRT-D therapy and developed sustained torsades de pointes (TdP) immediately after switching to biventricular pacing (BVP) mode. Here, TdP possibly developed owing to the change in the dispersion of repolarization of the left ventricle myocardium. The diagnosis and management of BVP-induced ventricular arrhythmia is discussed.
Keywords: CRT-induced VF, BVP-induced TdP, Torsades de pointes, Ventricular fibrillation
1. Introduction
Several randomized trials have shown that cardiac resynchronization therapy (CRT) improves exercise capacity, quality of life, and functional class in patients with severe drug-refractory congestive heart failure (CHF) caused by left ventricular (LV) dysfunction and electrical dyssynchrony [1]. The combination of CRT and an implantable cardioverter-defibrillator (ICD) is the preferred treatment for patients with severe heart failure, dyssynchrony, and an increased risk of sudden cardiac death or for survivors of a primary ventricular arrhythmia episode. Though it produces satisfactory improvements in hemodynamic parameters, functional class, and exercise capacity, the anti-arrhythmic effect of CRT therapy is not well established. Some studies have shown that biventricular pacing (BVP) is associated with a decrease in the incidence or excitability of monomorphic ventricular tachycardia (MMVT) [2–4], while others demonstrated a pro-arrhythmic potential [5–7].
Here, we present a patient with ischemic cardiomyopathy who underwent CRT-D implantation and developed sustained torsades de pointes (TdP) immediately after switching to BVP mode. In this case, the development of TdP was possibly due to the change in the dispersion of repolarization of the left ventricle myocardium.
2. Case report
A 59-year-old woman with a previous high lateral myocardial infarction and ischemic cardiomyopathy was admitted to our institution several times owing to heart failure decompensation. Coronary angiography performed after she suffered a transmural myocardial infarction in 2008 revealed 30–40% diffuse atherosclerotic plaque after the first septal branch of the left anterior descending (LAD) artery and subtotal stenosis of the first diagonal with a small calibration. The right coronary and circumflex arteries were found to be normal. At this time, her ejection fraction was 40% with LV anterior wall hypokinesis and moderate mitral regurgitation on transthoracic echocardiography. In 2011, gated myocardial perfusion scintigraphy (TC-99m MIBI) revealed a small ischemic area near the apex and a fixed perfusion defect consistent with a transmural myocardial infarction at the anterior wall segment from the mid-ventricle to the base and at the anterior-lateral wall segment of the LV mid-ventricle with an ejection fraction of 35%. The patient׳s condition worsened over time, with her New York Heart Association (NYHA) functional class increasing from I to III. In 2013, cardiac resynchronization therapy was considered after three admissions for acute heart failure decompensation. At this time, her electrocardiogram (ECG) showed a QRS duration of 160 ms with an LBBB morphology and sinus rhythm (Fig. 1). The LV ejection fraction decreased to 20% with global akinesis, and severe mitral and tricuspid regurgitation was present at the time of intervention. ICD combined with CRT was the preferred method for primary prevention as there were no prior episodes of syncope and tachycardia.
Fig. 1.

A baseline ECG shows normal sinus rhythm and an LBBB morphology with a QRS duration of 160 ms.
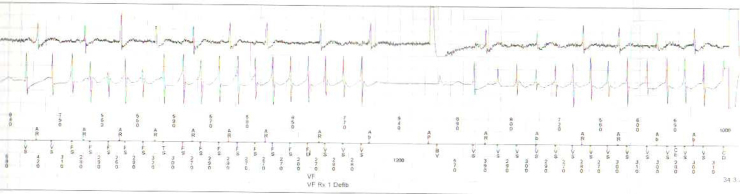
Implantation of the LV lead of the CRT-D into the posterior-lateral branch of the coronary sinus was performed successfully. After the activation of the BVP mode in the operating room, an incessant electrical storm of TdP commenced. After three antitachycardia pacing (ATP) attempts, defibrillation occurred and the tachycardia started repeatedly. Each TdP episode was stopped by device defibrillation (Fig. 2). As there was no history of ventricular tachycardia (VT) since the start of heart failure, it appeared that the tachycardia was associated with the ventricular pacing mode, and the BVP mode was stopped. Owing to the patient׳s instability, we could not perform echocardiography under the BVP mode and LV pacing mode. Every pacing attempt with these modes resulted in TdP, and accordingly the device was switched off. All electrolyte levels were in the normal range before and after the operation. After two days without any tachycardia episode, the BVP mode was reactivated in the coronary care unit and tachycardia started again. Atrial and ventricular pacing was re-attempted, and VT started after LV pacing. No tachycardia was detected with right ventricular pacing and atrial pacing. The patient was observed in the hospital for another seven days with the device switched off and no tachycardia occurred. The patient was discharged under oral treatment with amiodarone 200 mg twice daily.
Fig. 2.
Intracardiac electrograms show multiple ventricular fibrillations and defibrillations.
A repositioning of another lead to a different branch of the coronary sinus vein was planned, but the patient refused.
3. Discussion
CRT has become an established adjunctive treatment to optimal pharmacological therapy in patients with advanced CHF, diminished LV function, and intra-ventricular conduction delay [8]. Despite the benefits of CRT including improvements in exercise capacity, functional class, and ventricular hemodynamics, a pro-arrhythmic effect is less clear. The incidence of pro-arrhythmia reported in a limited single series was low, ranging from 3.4% to 4% during the first few days, with a predominance for ischemic cardiomyopathy patients [7–9]. Tachyarrhythmia was observed as MMVT, mostly in ischemic cardiomyopathy patients, or as polymorphic ventricular tachycardia (PMVT) or TdP, as seen in our case.
Most MMVTs seen in ischemic cardiomyopathy patients are caused by reentry and involve complex circuits in the LV [10]. The induction of a reentrant VT may be site specific, and can be facilitated by pacing at or near these circuits [11]. Reentry is the mechanism responsible for MMVT in CRT-implanted patients.
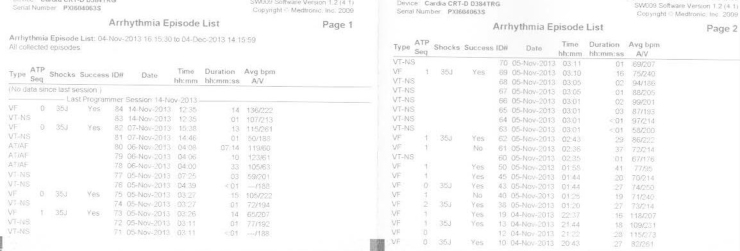
Normally, ventricular activation starts at the endocardium via the subendocardial Purkinje network and spreads across the ventricular wall. Although the epicardium is activated last, it repolarizes first because of its shorter action potential duration. This produces a repolarization sequence opposite to activation [12]. On ECG, this activation and repolarization sequence produces an upright T wave with the same polarity as the QRS [12]. LV epicardial pacing via the coronary sinus route abolishes normal repolarization of the LV by prolonging the QT interval, JT interval, and transmural dispersion of repolarization. First defined in 2003 by Medina-Ravell et al. [5], pacing site-dependent changes in ventricular repolarization potentially constitute the mechanism of TdP. Prolongation of ventricular repolarization time, the same circumstance as in long QT syndromes, makes the ventricle vulnerable to ventricular extrasystoles that result in R on T phenomenon and TdP. With BVP mode, the patient׳s QTc interval was prolonged from 521 ms to 536 ms, the JTc interval was prolonged from 305 ms to 360 ms, and the T peak–T end interval was prolonged from 120 ms to 190 ms. All markers of myocardial dispersion of repolarization were prolonged with LV epicardial pacing, and BVP was followed by ventricular extrasystole over the T wave resulting in TdP. Despite amiodarone infusion, 12 appropriate CRT-D defibrillations occurred (Fig. 3). As noted above, switching off the BVP mode stopped the electrical storm of TdP.
Fig. 3.
The ICD event recorder has recorded multiple ventricular fibrillations and defibrillations.
4. Conclusion
CRT can complicate incessant ventricular arrhythmia that may be resistant to medical therapy and therefore endanger the patient׳s life. In such situations, the BVP mode should be switched off and the LV pacing mode will usually terminate tachyarrhythmia. Reentry is thought to be the main mechanism of MMVT while LV repolarization dispersion is thought to be the mechanism of PMVT and TdP. Patients with a long QT, long JT, and T wave dispersion on initial ECG who have undergone CRT without an ICD are at an increased risk of sudden cardiac death. Luckily, CRT-D was present in our patient and the ICD saved her life. This clearly shows that CRT can induce ventricular arrhythmias and implies the need for CRT to systematically be associated with a defibrillation system.
Conflict of interest
None.
Acknowledgments
AS has followed the patient in coronary care unit, AIT has provided the figures׳ material, CT checked the manuscript and made language corrections, ATA is the chef of the service and helped in proof-reading.
References
- 1.Abraham W.T., Hayes D.L. Cardiac resynchronization therapy for heart failure. Circulation. 2003;108:2596–2603. doi: 10.1161/01.CIR.0000096580.26969.9A. [DOI] [PubMed] [Google Scholar]
- 2.Higgins S.L., Yong P., Sheck D. Biventricular pacing diminishes the need for implantable cardioverter defibrillator therapy: Ventak CHF Investigators. J Am Coll Cardiol. 2000;36:824–827. doi: 10.1016/s0735-1097(00)00795-6. [DOI] [PubMed] [Google Scholar]
- 3.Garrigue S., Barold S.S., Hocini M. Treatment of drug refractory ventricular tachycardia by biventricular pacing. Pacing Clin Electrophysiol. 2000;23:1700–1702. doi: 10.1046/j.1460-9592.2000.01700.x. [DOI] [PubMed] [Google Scholar]
- 4.Zagrodzky J.D., Ramaswamy K., Page R.L. Biventricular pacing decreases the inducibility of ventricular tachycardia in patients with ischemic cardiomyopathy. Am J Cardiol. 2001;87:1208–1210. doi: 10.1016/s0002-9149(01)01498-9. [DOI] [PubMed] [Google Scholar]
- 5.Medina-Ravell V.A., Lankipalli R.S., Yan G.X. Effect of epicardial or biventricular pacing to prolong QT interval and increase transmural dispersion of repolarization: does resynchronization therapy pose a risk for patients predisposed to long QT or torsade de pointes? Circulation. 2003;107:740–746. doi: 10.1161/01.cir.0000048126.07819.37. [DOI] [PubMed] [Google Scholar]
- 6.Rivero-Ayerza M., Vanderheyden M., Verstreken S. Images in cardiovascular medicine. Polymorphic ventricular tachycardia induced by left ventricular pacing. Circulation. 2004;109:2924–2925. doi: 10.1161/01.CIR.0000130731.98722.F8. [DOI] [PubMed] [Google Scholar]
- 7.Shukla G., Chaudhry G.M., Orlov M. Potential proarrhythmic effect of biventricular pacing: fact or myth? Heart Rhythm. 2005;2:9551–9568. doi: 10.1016/j.hrthm.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 8.Ray Basu, Fendelander L., Singh J.P. Cardiac resynchronization therapy and its potential proarrhythmic effect. Clin Cardiol. 2007:498–502. doi: 10.1002/clc.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bleeker G.B., Yu C.M., Nihoyannopoulos P. Optimal use of echocardiography in cardiac resynchronization therapy. Heart. 2007;93:1339–1350. doi: 10.1136/hrt.2005.076422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stevenson W.G., Delacretaz E. Radiofrequency catheter ablation of ventricular tachycardia. Heart. 2000;84:553–559. doi: 10.1136/heart.84.5.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Josephson M.E. Electrophysiology of ventricular tachycardia. Pacing Clin Electrophysiol. 2003;26:2052–2067. doi: 10.1046/j.1460-9592.2003.00320.x. [DOI] [PubMed] [Google Scholar]
- 12.Yan G.X., Antzelevitch C. Cellular basis for the normal T wave and the electrocardiographic manifestations of the long-QT syndrome. Circulation. 1998;98:1928–1936. doi: 10.1161/01.cir.98.18.1928. [DOI] [PubMed] [Google Scholar]