Abstract
A 65-year-old woman with a history of syncope was diagnosed with hypertrophic cardiomyopathy. She had previously undergone mastectomy of the left breast owing to breast cancer. Holter electrocardiogram (ECG) and monitor ECG revealed sick sinus syndrome (Type II) and non-sustained ventricular tachycardia. Sustained ventricular tachycardia and ventricular fibrillation were induced in an electrophysiological study. Although the patient was eligible for treatment with a dual chamber implantable cardioverter defibrillator (ICD), venography revealed lack of the right superior vena cava (R-SVC). Lead placement from the left subclavian vein would have increased the risk of lymphedema owing to the patient׳s mastectomy history. Consequently, the defibrillation lead was placed in the right ventricle by direct puncture of the right auricle through the tricuspid valve. The atrial lead was sutured to the atrial wall, and the postoperative course was unremarkable. Defibrillation lead placement using a transthoracic transatrial approach can be an alternative method in cases where a transvenous approach for lead placement is not feasible.
Keywords: Implantable cardioverter defibrillator, Left superior vena cava, Transthoracic transatrial
1. Introduction
Patients with fatal arrhythmias are routinely treated with an implantable cardioverter defibrillator (ICD), whereby lead placement is performed transvenously. However, a transvenous approach is limited in cases of venous occlusion or malformation. This report describes a case in which the defibrillation lead was placed using a transthoracic transatrial approach owing to inadequate transvenous access due to lack of the right superior vena cava (R-SVC).
2. Case report
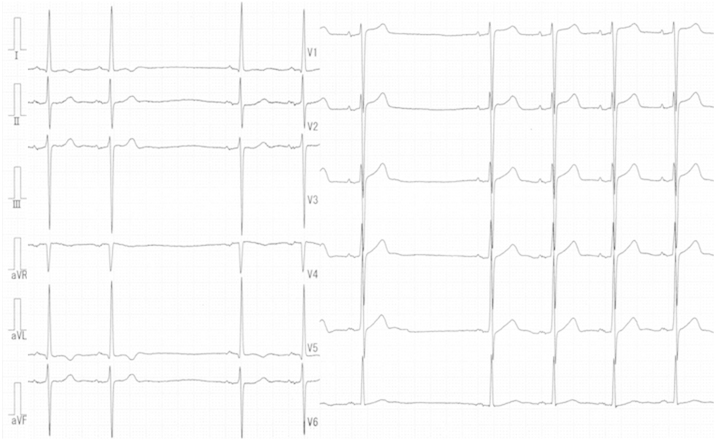
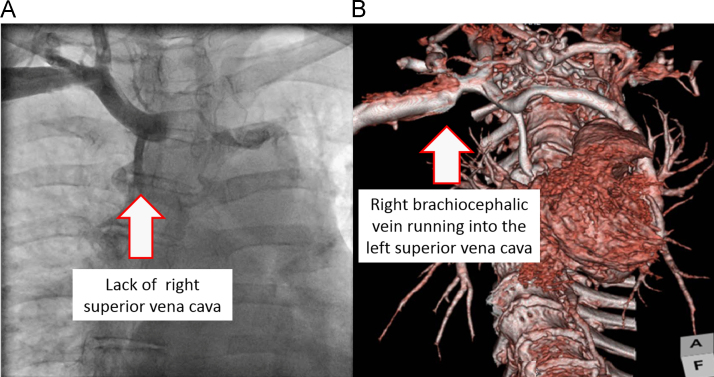
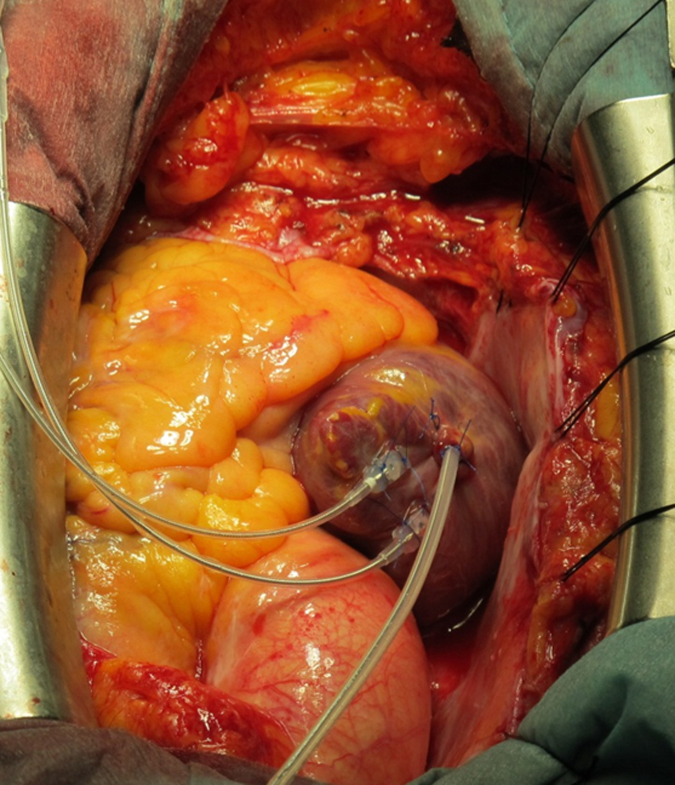
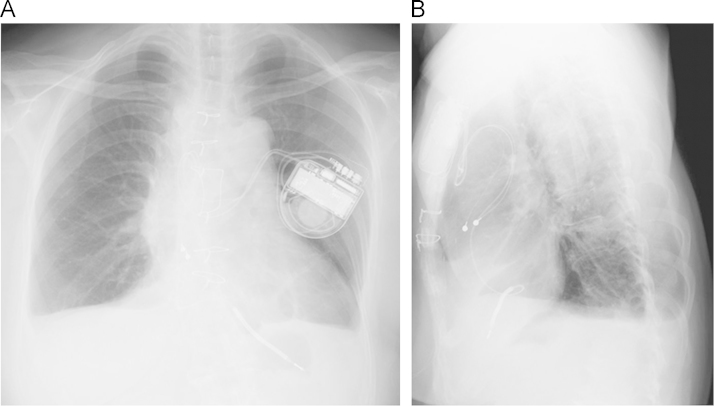
A 65-year-old woman with a history of syncope and diastolic dysfunction was diagnosed with hypertrophic cardiomyopathy, as evaluated by echocardiography and myocardial biopsy. Although she had no family history of sudden death or cardiomyopathy, she had experienced syncope at the age of 42 years, which had not been fully examined. She had previously undergone a mastectomy of the left breast due to breast cancer. An electrocardiogram (ECG) indicated unstable sinus node function and Holter ECG recording revealed sinus arrest lasting up to 2.6 s (Fig. 1). Furthermore, non-sustained ventricular tachycardia with a cycle length of 400 ms lasting for a maximum of 3 s was observed several times. Transthoracic echocardiography showed asymmetric mural thickening from the base of the mid-interventricular septum. The left ventricular ejection fraction was recorded as 65%, and the left ventricular end-diastolic and end-systolic diameters measured 48 mm and 23 mm, respectively. There were no findings indicative of left ventricular dyssynchrony, while a thoracic MRI revealed delayed enhancement within the hypertrophied interventricular septum. The left ventricular outflow tract was observed to be free of obstruction. During the electrophysiological study, ventricular tachycardia induced by bursting stimuli from the right ventricular apex degraded to ventricular fibrillation and was terminated by an external defibrillator. Although the indication of ICD therapy seemed to be controversial, the patient consented to receive ICD for fear of sudden death. She was eligible for dual chamber ICD treatment to prevent sudden cardiac death and to create atrial pacing for brachycardia. Lack of the R-SVC was indicated by venography, and a CT scan revealed a right brachiocephalic vein running into the left superior vena cava (L-SVC) (Fig. 2). Lead insertion from the left subclavian vein was possible but there was a risk of lymphedema owing to the patient׳s mastectomy history. Although the greater pectoral muscle and subcutaneous fat were preserved during mastectomy, the left breast was surgically removed and the axillary lymph nodes were dissected. Therefore, we elected to use a transthoracic transatrial approach for surgical lead placement for ICD treatment. Thoracotomy was performed during median sternotomy and leads were placed on the beating heart. A scalpel was used to cut the center of a small purse-string suture on the right auricle, and a defibrillation lead was positioned in the right ventricle via the tricuspid valve. Bleeding around the lead was well controlled and diminished by the purse-string suture. An epicardial atrial lead was sutured to the atrial wall (Fig. 3) to overcome sinus bradycardia. Oversensing was avoided owing to the small size of the far-field R wave. A subcutaneous pocket was created in the left precordial area, and the leads were passed from the pericardial cavity through the intercostal space to the pocket and connected to a dual chamber ICD device designed to deliver a maximum of 35 J (Fig. 4). We performed single defibrillation threshold testing (DFT) during the operation, and a 25-J shock successfully terminated ventricular fibrillation (VF). We did not perform DFT repeatedly in order to minimize the damage to the heart under thoracotomy. The postoperative course and 12-month follow-up assessment were unremarkable.
Fig. 1.
Electrocardiogram on admission, indicating unstable sinus node function.
Fig. 2.
A: Venography of the right subclavian vein illustrating lack of the right superior vena cava. The vein branching from the right subclavian vein is the azygos vein.
B: Three-dimensional computed tomography scan image of the right brachiocephalic vein running into the left superior vena cava. The right brachiocephalic vein is compressed as it enters the left superior vena cava.
Fig. 3.
Intraoperative image (bottom is cranial) illustrating puncturing of the right auricle as a result of defibrillation lead insertion. The epicardial atrial lead was sutured to the atrial wall.
Fig. 4.
Postoperative chest radiograph. The leads were passed from the pericardial cavity through the intercostal space and connected to a dual chamber implantable cardioverter defibrillator device in the left precordial area.
3. Discussion
Transvenous ventricular lead placement is routinely used for ICD treatment in patients with fatal arrhythmia. However, this approach is limited and an alternative procedure is required in complicated cases such as those with venous occlusion or malformation, those undergoing dialysis, or those with previous breast surgery.
Implantation of a defibrillation patch under thoracotomy has been used for implantation in the beginning and is still in use in cases where venous access is inadequate, and studies have reported postoperative heart failure in 3 of 35 ICD patients treated with a defibrillation patch [1]. In such cases, heart failure was considered to be related with the epicardial patch, resulting in removal of the patch. It is important to be attentive towards diastolic dysfunction before surgery [2]. In our case, heart failure due to diastolic dysfunction was observed before surgery and an epicardial patch was considered to be harmful for this patient. Subcutaneous ICD, which is widely used in western countries, may be an alternative in cases where sinus bradycardia is absent, but in our patient atrial pacing would have been required with such an approach.
In this case, lead insertion from the left subclavian vein via the L-SVC was feasible. Persistent left superior vena cava (PLSVC) is a congenital venous malformation occurring in 0.3–0.5% of the general population [3], but its presence in the absence of the R-SVC is a very rare congenital anomaly [4]. ICD placement is a complicated procedure in PLSVC cases, but is nevertheless still feasible [5]. A report indicated that lymphedema occurs in approximately 50% of cases with a history of mastectomy [6], which in turn leads to a decrease in the patients׳ quality of life. Lead implantation from the left subclavian vein via the L-SVC would have been precarious owing to the increased risk of lymphedema; therefore, lead implantation from the right subclavian vein via the L-SVC was the alternative option. However, the right brachiocephalic vein was compressed on entry into the L-SVC leading to an increased risk of lead dislodgement and was therefore considered to be unfeasible. A transthoracic transatrial approach was quite a distinct choice for lead placement, and earlier reports of 35 patients who were treated in this way as the transvenous approach was difficult showed that 8 patients were without any particular complications for up to 14 years [7,8]. We chose this approach in our case, and the postoperative course was uneventful.
Although our approach was successful, there is limited literature on the durability of the implanted lead using this method. As a result, we continue to monitor the patient remotely to ensure we are able to respond to any concerns with the lead in a timely manner.
4. Conclusion
Defibrillation lead placement using a transthoracic transatrial approach can be a useful alternative in cases where lead placement cannot be performed using a transvenous approach.
Conflict of interest
None declared.
References
- 1.Chevalier P., Moncada E., Canu G. Symptomatic pericardial disease associated with patch electrodes of the automatic implantable cardioverter defibrillator: an underestimated complication? Pacing Clin Electrophysiol. 1996;19:2150–2152. doi: 10.1111/j.1540-8159.1996.tb03292.x. [DOI] [PubMed] [Google Scholar]
- 2.Thomas O., Leenhardt A., Masquet C. Pericardial constriction caused by epicardial patches of automatic implantable defibrillators. Apropos of 3 cases. Arch Mal Coeur Vaiss. 1994;87:931–935. [PubMed] [Google Scholar]
- 3.Parreira L.F., Lucas C.C., Gil C.C. Catheterization of a persistent left superior vena cava. J Vasc Access. 2009;10:214–215. doi: 10.1177/112972980901000315. [DOI] [PubMed] [Google Scholar]
- 4.Srivastava V., Mishra P., Kumar S. Persistent left SVC with absent right SVC: a rare anomaly. J Card Surg. 2007;22:535–536. doi: 10.1111/j.1540-8191.2007.00474.x. [DOI] [PubMed] [Google Scholar]
- 5.Guenther M., Kolschmann S., Rauwolf T.P. Implantable cardioverter defibrillator lead implantation in patients with a persistent left superior vena cava – feasibility, chances, and limitations: representative cases in adults. Europace. 2013;15:273–277. doi: 10.1093/europace/eus287. [DOI] [PubMed] [Google Scholar]
- 6.Morrell R.M., Halyard M.Y., Schild S.E. Breast cancer-related lymphedema. Mayo Clin Proc. 2005;80:1480–1484. doi: 10.4065/80.11.1480. [DOI] [PubMed] [Google Scholar]
- 7.Molina JE. Surgical options for endocardial lead placement when upper veins are obstructed or nonusable. J Interv Card Electrophysiol. 2004;11:149–154. doi: 10.1023/B:JICE.0000042354.87946.39. [DOI] [PubMed] [Google Scholar]
- 8.Cannon B.C., Friedman R.A., Fenrich A.L. Innovative techniques for placement of implantable cardioverter–defibrillator leads in patients with limited venous access to the heart. Pacing Clin Electrophysiol. 2006;29:181–187. doi: 10.1111/j.1540-8159.2006.00314.x. [DOI] [PubMed] [Google Scholar]