Abstract
Introduction
This paper describes methamphetamine (MA) use patterns, specifically duration of continuing abstinence (“time to relapse”) for periods averaging 5 years post-discharge from treatment for MA use, and the relationship with selected user and treatment characteristics.
Methods
A sample of 350 treatment admissions from a large county substance use disorder (SUD) treatment system was randomly selected (within gender, race/ethnicity, treatment modality strata). Retrospective self-report data are from natural history interviews (NHI) conducted approximately 3 years after treatment and a follow-up 2-3 years later. Relapse is defined as any use of MA with time as the number of months of continuous MA abstinence after treatment discharge until relapse. This outcome was constructed from a monthly MA use timeline using NHI data. A Cox model was used to examine time to relapse and predictors.
Results
Sixty-one percent of the sample relapsed to MA use within 1 year after treatment discharge and 25% during years 2-5. Significant protective factors predicting longer time to relapse included having experienced serious MA-related psychiatric/behavioral problems (hazard ratio [HR]=0.75, p=0.027), longer duration of the index treatment episode (HR=0.93, p=0.001), and participating in self-help or other treatment during the post-treatment abstinence period(HR=0.29, p<0.001); risk factors for shorter time to relapse included having a parent with alcohol and/or drug use problems (HR =1.35, p=0.020) and involvement in MA sales (HR=1.48, p=0.002).
Conclusions
Results contribute a long-term perspective on patterns of MA use following treatment and support a need for early post-treatment and long-term continuing care and relapse- prevention services.
Keywords: methamphetamine, relapse, continuing abstinence, long-term follow-up, Cox regression, Natural History Interview
1. Introduction
Methamphetamine [MA] is the primary drug of the class of amphetamine-type substances ranking second in world-wide illicit drug use after cannabis; notably, MA is the primary illicit drug threat in Asia (UNODC, 2011, 2012). MA use increased dramatically in the U. S. from 1990 to about 2005-7, by which time MA accounted for substantial proportions of substance use disorder (SUD) treatment admissions in several states (e.g., 35% of California SUD admissions in 2007; Maxwell and Brecht, 2011; Rawson et al., 2008; SAMHSA, 1996, 2009, 2013). Chronic MA use is linked to significant public health, legal, and environmental problems, as well as medical, psychiatric and cognitive deficits (Dean et al., 2013; Gonzales et al., 2010; Meredith et al., 2005).
Accumulating evidence supports short-term effectiveness of treatment for MA use, e.g., during treatment and up to 1-2 years post-treatment (Anglin et al., 2007; Brecht et al., 2006; Brecht and Urada, 2011; Glasner-Edwards et al., 2008; Hillhouse et al., 2007; Hser et al., 2005; Roll et al., 2006; Shoptaw et al., 2008). A few reports have examined MA abstinence patterns for longer post-treatment periods (Rawson et al., 2002 [2-5 years post-treatment]; Marinelli-Casey et al. reported in Calabria et al., 2010 [3 years]; McKetin et al., 2012 [3 years]). These studies suggest that treatment effects decline over time, as measured by MA use status. However, there is not yet a comprehensive literature on patterns of continuing abstinence and relapse for even longer post-treatment follow-up durations. The current study contributes to filling this gap by examining continuing MA-abstinence and time to relapse for a period averaging five years following treatment for MA use.
While few data exist on MA use patterns for long post-treatment periods, long-term treatment outcome studies for users of other substances provide a context for the current study (cf., Calabria et al., 2010 for a review of 15 prospective studies with 3-33-year follow-up). Continuing abstinence declines over time (Gossop et al., 2000, 2003; Ribeiro et al., 2007; Simpson et al., 1999, 2002), with early periods of abstinence predicting later and continuing abstinence (Weisner et al., 2003; Mertens et al., 2012; Dennis et al., 2007).
Most studies of post-treatment substance use patterns are based on snapshots of use status (e.g., during past month, past year, etc.) at specific time points (e.g., one year post-treatment, 3 years), allowing an overview of patterns but often not providing detail on duration of continuing abstinence or specific timing of relapse to support development of appropriately timed continuing care. For example, Hser et al. (2003) provided informative results showing 10-15% of MA users reporting MA use in each of 12 months following treatment admission, but these results did not track individuals' continuous periods of abstinence. Use of natural history data has supported more detailed temporal perspectives on substance use patterns for heroin and cocaine (Hser, 2007; Grella and Lovinger, 2011). The current study uses natural history data (see Methods section) to examine duration of continuing abstinence (or time to relapse) following treatment.
To contribute to a broader picture of MA-use patterns following treatment for MA use, the current study describes MA abstinence and time to relapse for a period averaging 60.5 months following discharge from “treatment as usual” in a large county SUD treatment system, and examines predictors. A Cox regression approach is used to model time to relapse with selected predictors from domains including demographics and background, MA use history and behaviors, and SUD treatment characteristics. The current study provides results which may be important in identifying both the timing of and risk factors for relapse to MA use, which, in turn, can contribute to the content and timing of continuing care.
2. Methods
2.1 Participants
A study of the natural history of MA use provided data for a sample of MA-using clients admitted to the publicly funded Los Angeles County SUD treatment system. A random sample (within gender, ethnicity, modality [outpatient, residential] strata) of admission records was selected from the California Alcohol and Drug Data System, primarily from 1996. Seventy-five percent of these admissions were located and 76% of those located were interviewed, yielding a sample size of 350 for the current analysis (Brecht et al., 2004; von Mayrhauser et al., 2002). In the current paper, MA abstinence/relapse patterns are examined following discharge from this index [sampled] episode.
The initial interview (n=350) occurred approximately three years after the index episode. A follow-up interview was conducted with 277 of the analysis sample (79% follow-up rate) 2-4 years later. Data from the index episode admission records allowed limited comparison of the analysis sample vs. those originally sampled but not in the analysis sample (e.g., not located or interviewed/died/incomplete data). This comparison showed no significant differences in education, age of first MA use, age at index episode admission, number of prior treatment episodes, employment status, whether homeless, pregnant, or under legal supervision. Examination of the n=350 analysis sample by follow-up status (277 with a follow-up interview vs. 73 without) also found no significant differences in the predictors considered in the current study.
2.2 Instrument
Subjects were interviewed using the Natural History Interview (NHI) protocol. This face-to-face interview included questions on sociodemographic and background factors, substance use, criminal behaviors, and physical and mental health. It also collected detailed life-course data on use of selected substances and treatment utilization beginning at age 14. The NHI has been used for over 30 years in substance abuse research (Hser, 2007; McGlothlin et al., 1977; Nurco et al., 1975). The interviewer works closely with the respondent, using corroborative information and memory aids (e.g., major life and historical events) to optimize recall. Reliability has been supported in previous studies (Anglin et al., 1993; Murphy et al., 2010). Reliability was also supported in the current study: 1) acceptable levels of agreement for self-reported current/recent MA use and urinalysis (88% in the first interview); and 2) differences < .08 in measures of association between MA use in the past year as recalled from two perspectives (from proximal recall in the year preceding the initial interview and distal recall for the same year recalled from the second interview) with the potential predictors for the current study. Self-reports of substance use have also been found to be acceptably reliable in other studies (Brigham et al., 2008; Denis et al., 2012; Fals-Stewart et al., 2000).
2.3 Variables
The primary outcome variable for this analysis is number of months of continuous MA abstinence following discharge from the index treatment episode (also termed “time to relapse). Abstinence was defined as no use of MA in each month. The outcome variable was calculated from a monthly timeline of self-reported MA use constructed from participants' reports (NHI) of MA use frequency and changes in frequency. MA use status during specific months is also described (during month 12, 24, 36, 48, and 60 following treatment discharge), since this status description has been a more typical outcome measure in long-term follow-up studies that may not collect more detailed substance use histories.
Selected predictors represent broad domains potentially impacting post-treatment substance use. Since less research is available on predictors of post-treatment MA use patterns, some cited references come from studies of other drugs. Note also that research support has often been inconsistent for many potential predictors. Data for predictors for the current analysis are self-report, most from the initial interview (NHI); data for post-treatment continuing care participation were from both interviews.
Socio-demographics included gender (Grella et al., 2008; Hser et al., 2003; Walitzer and Dearing, 2006); ethnicity (Grella and Joshi, 2003; Hser et al., 2006); education (dichotomized to 0=less than high school education, 1=high school/GED or higher; Brecht et al., 2006; Jaffe et al., 2012); and percentage of months employed during the two years preceding treatment admission (Adamson et al., 2009; Hser et al., 2007). An indicator of childhood family context included parental drug/alcohol problems (yes=1, no=0; Chassin et al., 2004). Other potential vulnerabilities included psychological comorbidity defined as ever diagnosed (self-reported) with major mental illness (1=yes, 0=no; Hillhouse et al., 2007; Hser et al., 2007; McKay et al., 2002) and early (before age 15) sexual abuse (1=yes, 0=no; Boles et al., 2005; Grella and Joshi, 2003).
Drug use and MA-related characteristics included young age of onset of MA use (1=younger than 16 years, 0=16 or older; Brecht et al., 2000; Sharma et al., 2012); any intravenous drug use in lifetime (1=yes, 0=no; Rawson et al., 2007); ever having sold MA (1=yes, 0=no; Brecht et al., 2000); the average number of days per month using MA during the two years preceding treatment (Adamson et al., 2009; Hillhouse et al., 2007); and having experienced three specific serious problems (paranoia, hallucinations, violent behavior) perceived as resulting from the participant's MA use (Brecht et al., 2006).
Treatment (index episode) characteristics included age at admission (Anderson et al., 2007; Brecht et al., 2006), type of treatment (1=residential vs. 0=out-patient; Prendergast et al., 2002), legal or criminal justice system pressure for admission (1=yes, 0=no; Perron and Bright, 2008), and number of months in the index episode (Brecht et al., 2000; Hser et al., 2007). A post-treatment measure indicated subject participation in self-help or other SUD treatment following discharge from the index episode and prior to relapse (1=yes, 0=no; Gossop et al., 2007; Grella et al., 2010; Kissin et al., 2003; Witbrodt et al., 2012).
Note that two predictors were dichotomized for analysis. Education in our study was originally an 8-category ordinal variable, not normally distributed. Since an earlier study of 2-year treatment outcomes had found that a collapsed coding (<high school vs. high school completion) captured a relationship with outcomes (Brecht et al., 2005), current analysis used this simplified coding. While early/adolescent substance use onset has been related to development of SUD (Chen et al., 2009), use of a standard age cutoff for early onset has not been consistent in the literature, but often ranges from 15 to 17 years (Hser, 2007; Chen et al., 2009). We selected the middle of this range for dichotomizing age of onset of MA use. Using different age cutpoints (14-18) did not appreciably change results.
2.4 Data Analyses
The outcome measure used self-report data from initial and follow-up NHI to maximize the duration of reported MA history following discharge from the index treatment episode. Seventy-three subjects did not have a second interview, thus having shorter histories (average 39 months vs. 66 for those with both interviews). However, all 350 subjects were included in the current analysis. The average post-treatment follow-up period was 60.5 months (sd=14.8); 93% had follow-up periods of 36 months or more, 80% had 48 months or more, 59% had 60 months or more. The variation in length of MA-use history was handled as right-censoring; each subject was considered in the time-to-relapse analysis up to the end of his/her observation period or to relapse, whichever occurred first. Note that a majority of subjects, even those with shorter observation periods, relapsed within their observed follow-up, thus contributing full information to the relapse analysis. As noted in the Participants section, those with and without a second interview did not differ significantly on any of the selected predictors. The primary analysis is based on probabilities of relapse conditional on being observed. In descriptive results, we report two sets of percentages for abstinence durations: 1) unconditional, as percentages of the total sample (n=350); and 2) conditional on having at least the specified duration of follow-up (e.g. 5-year abstinence as a percentage of the n=206 who had at least five years of follow-up duration).
To avoid dropping two predictors because of one missing value for each, imputed values were computed as the average for the subject across 10 multiply-imputed data sets using the EM algorithm in SAS PROC MI and substituted for the two missing values (Janssen et al., 2010). Analyses did not include adjustment for subjects nested within treatment program because preliminary analyses calculated a very small intraclass correlation of <.001.
A Cox proportional hazards model examined time to relapse to MA use and predictors. Because the study was not a randomized clinical trial with pre-specified hypotheses, we adopted a model-building analysis approach (Hosmer and Lemeshow, 2000). A preliminary step estimated univariate models identifying variables with little relationship, to optimize parsimony and reduce shrinkage in a multivariable model (Parmar and Machin, 1996; Steyerberg et al., 2000). Four predictors with p>.65 were dropped from further consideration: race/ethnicity, early sexual abuse, serious mental illness, treatment modality. A multivariable Cox model was then estimated with the remaining 13 predictors (called the “full model”; detailed results not presented in this paper). A parsimonious (“reduced”) model was estimated with only the subset of variables with p<.20. The assumption of proportional hazards was supported for the reduced model (p=.995). Additional survival curves for specific subgroups of subjects are also presented. Sensitivity analyses examined the robustness of results across several scenarios as described briefly in supplementary material1; results indicated substantial robustness of results.
3. Results
3.1. Sample Description
The sample was demographically diverse: 56% male, 44% female; 17% African-American, 30% Hispanic, 47% non-Hispanic White, 7% other and/or mixed race/ethnicity (see Table 1). The sample displayed potential vulnerabilities from childhood/adolescence/early adulthood: 56% reported parents with drug and/or alcohol problems; 32% had less than a high school education. Employment (part- or full-time) was low during the two years before the index treatment episode (averaging 29% of the 24 month-period). Past or present diagnosis of severe mental illness was self-reported by 19%; 33% had experienced sexual abuse before age 15.
Table 1. Sample Description (n=350).
| Sample characteristics (self-reported) | % or mean (st.dev.) |
|---|---|
| Background | |
| Male | 56.3 |
| Race/ethnicity | |
| African-American | 16.6 |
| Hispanic | 29.7 |
| Non-Hispanic White | 47.1 |
| Other/multi-ethnic | 6.6 |
| Less than high school education | 32.0 |
| Parental alcohol and/or drug use | 56.0 |
| Sexual abuse before age 15 | 33.1 |
| Ever diagnosed with major mental illness | 19.1 |
| Employment--% of months during 2 years prior to index treatment | 29.9 (37.8) |
| Drug use history | |
| 1st MA use younger than 16 | 30.0 |
| Ever sold MA | 55.4 |
| MA-related problems (% with all 3: paranoia, hallucinations, violent behavior) | 38.0 |
| MA use severity (avg. number of days per mo. with MA use in 2 years prior to index tx) | 15.7 (10.3) |
| Ever injected drugs | 46.6 |
| Index treatment (tx) characteristics | |
| Legal pressure to enter tx | 51.4 |
| Age at admission | 29.4 (6.9) |
| Residential tx (vs. outpatient) | 62.0 |
| No. months in tx | 3.7 (3.2) |
| Post-treatment characteristics | |
| Any self-help and/or other treatment participation | 38.3 |
MA use was initiated by 30% of the sample before age 16; 47% had injected drugs; and 56% had sold MA. Experiencing at least one serious MA-related problem was reported by 80%: 66% reported paranoia, 61% hallucinations, and 56% violent behavior; 38% experienced all three MA-related problems (data not shown in Table 1).
The average age at admission to the index treatment episode was 29 years. Fifty-one percent reported admission under some legal pressure. Treatment modality was residential for 62% and outpatient for 38%. Time in the index treatment episode averaged 3.7 (range 1-18 months). Thirty-eight percent reported self-help and/or other treatment participation during their follow-up period prior to relapse; 21% reported only self-help, 6% only other treatment, 11% both.
3.2. Abstinence and Time to Relapse
Twenty-three percent maintained MA-abstinence during their entire observed follow-up period, with abstinence durations of 22-90 months. Thus, 77% of the sample had relapsed to MA use within their observed follow-up period, ending periods of abstinence of 0-79 months. Thirteen percent (n=47) of the sample achieved at least five years of continuing abstinence. These n=47 constituted 23% of the subset of participants (n=206) whose observed follow-up periods were at least five years long.
The greatest decrease in the probability of continuing abstinence occurred early in the post-treatment period: 61% relapsed within the first year following discharge from the index treatment episode (see Figure 1). Considering first-year relapse in more detail showed that: 1) 36% percent had no months of abstinence directly following treatment discharge, i.e. resuming MA use during the first month after discharge or using MA when they left treatment); 2) 14% relapsed in months 2-6; and 3) 11% relapsed within months 7-12.
Figure 1. Survival Curve—Probability of Continuing Abstinence (n=350).
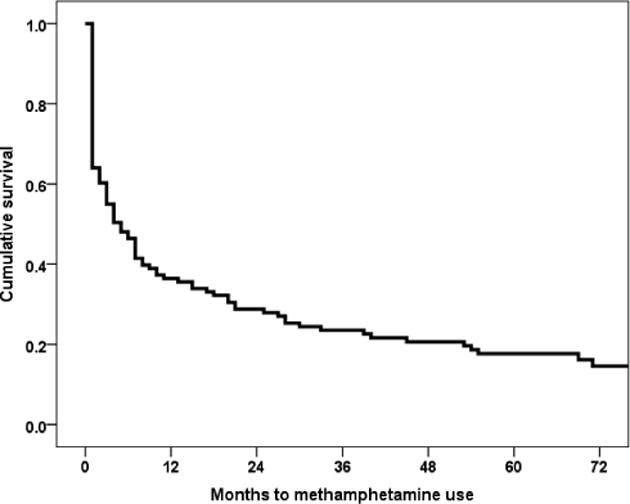
Three percent relapsed during months 13-18 and 4% during months 19-24, totaling 7% in the second post-treatment year. Three percent relapsed in each of the third and fourth years, 2% in year 5, and 1% in years 6-7. In terms of continuing abstinence, 32%, 26%, 21%, and 13% of the total sample had at least 2, 3, 4, and 5 years of continuing abstinence, respectively. (Note that percentages for 2-5 year continuing abstinence recalculated from subsets with observed follow-ups durations of at least the corresponding length gives 32% [of n=350 at 2 years], 32% [of n=325 with at least 3-year follow-up], 26% [4-year, n=277], and 23% [5-year, n=206].)
While duration of continuing abstinence post-treatment was the primary focus of this report, data on MA abstinence status at specific time points showed 66% of the sample as MA-abstinent specifically during the 12th post-treatment month (regardless of previous history of MA abstinence or use during the follow-up period); 75% were abstinent during month 24. Seventy-seven percent of the observable sample was abstinent during month 36, 80% during month 48, and 79% during month 60.
Focusing on the subset (n=206) with follow-up periods of 60 or more months, participants averaged 44 months of abstinence (not necessarily continuous) in the 60- month period. The 159 (of 206) who relapsed before 60 months (with average time to relapse of 7 months) had additional abstinent time following their relapse: 94% had at least 6 months of abstinence following their initial relapse (within the 60-month observation period). The relapsed subgroup averaged 39 months of MA abstinence during the 60-month period including their initial abstinence period.
3.3 Predictors of Time to Relapse
The full multivariable Cox model identified five predictors (p<.20) for inclusion in a reduced (parsimonious) Cox model. This reduced model was significant at p<.001 (likelihood ratio chi square=106.46, df=5), showing little loss of predictive capability from the full 13-predictor model (likelihood ratio chi square=110.71, df=13). Significant risk factors for shorter time to relapse included parental drug use (hazard ratio [HR] =1.35, p=0.020) and ever having sold MA (HR=1.48, p=0.002). (See Table 2.) Protective factors predicting longer time to relapse included having experienced three serious problems perceived as related to MA use (paranoia, hallucinations, violent behavior) (HR=0.75, p=0.027), more months in the index treatment episode (HR=0.93, p=0.001), and participation in self-help and/or additional SUD treatment during the abstinence period (HR=0.29, p<0.001). The strongest effect size (as indicated by the hazard ratio) was for self-help/other treatment participation.
Table 2. Predictors of Time to Relapse from Cox Proportional Hazards (Reduced) Model (n=350)1.
| Coefficient (st. error) | Probability | Hazard ratio (95% CI) | |
|---|---|---|---|
| Parental alcohol and/or drug use | 0.30 (0.13) | 0.020 | 1.35 (1.05-1.73) |
| Ever sold MA | 0.39 (0.13) | 0.002 | 1.48 (1.15-1.90) |
| MA-related psychiatric/behavioral problems | -0.29 (0.13) | 0.027 | 0.75 (0.58-0.97) |
| No. months in index treatment episode | -0.07 (0.02) | 0.001 | 0.93 (0.89-0.97) |
| Any post-discharge self-help or other substance abuse treatment participation | -1.22 (0.14) | <0.001 | 0.29 (0.22-0.39) |
Model fit: χ2=106.46, df=5, p<.0001
estimates from the reduced Cox model with the 5 listed predictors; these predictors were selected from the full (13 predictors) multivariable model by retaining variables with p<.20.
Illustration of selected partial effects appears in Figure 2, showing the substantially greater survival rate (that is, the higher curve in each graph) for the subgroup who participated in self-help/other treatment during their post-index treatment abstinence as compared to non-participants. This effect was observable for those with varying levels of relapse risk based on parental drug use and MA sales: Fig. 2A includes those without these two risks; 2B, with either risk factor; 2C, with both risk factors. While the survival curves are somewhat lower as the risk factors increase, there remains a significant difference depending on self-help/other treatment participation (p<.01 for each risk subgroup). Further exploration included interaction effects between the primary facilitator (additional self-help/treatment) and each risk factor (parental drug use and MA sales involvement). Interactions were not significant.
Figure 2.
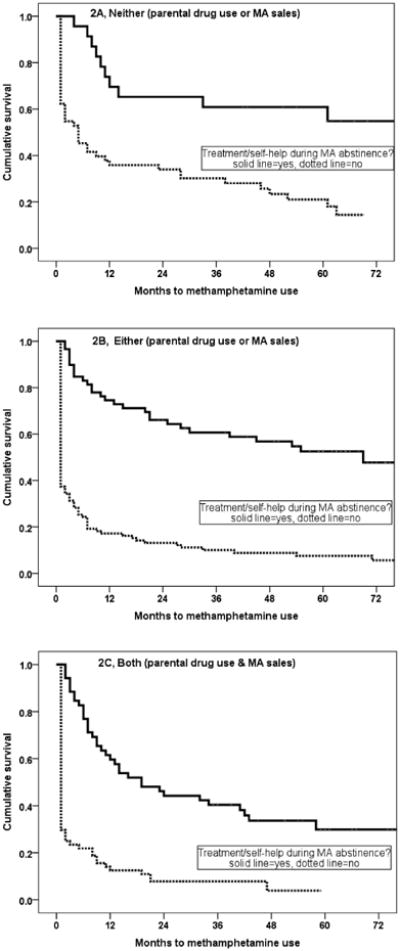
Conditional Survival Curves by Abstinence Facilitator (Self-Help/Other Treatment during post-treatment abstinence [dotted line=no, solid line=yes]) and Relapse Vulnerabilities (Parental Drug Use and/or Have Sold Methamphetamine [neither, yes on one, yes on both])
2A. Neither Parental Drug Use nor Have Sold Methamphetamine
2B. Either Parental Drug Use or Have Sold Methamphetamine
2C. Both Parental Drug Use and Have Sold Methamphetamine
4. Discussion
The study provides a first look at duration of continuous post-treatment MA abstinence (and time to relapse) from a long-term perspective. Thirteen percent of the sample of 350 MA users achieved at least five years of continuous MA abstinence. Sixty-one percent relapsed to MA use within the first year following treatment, with considerably declining relapse rates in subsequent years. Of the subset (n=206) with at least five years of available post-treatment history, 23% had at least5-years continuous-abstinence.
Results showed first year continuous MA-abstinence (39%) slightly higher than McKetin et al. (2012) (31% following residential treatment) and 3-year continuous MA-abstinence (26%) close to that in Mooney et al. (2009) (22%). Note that in the current sample, 1-yr continuous abstinence rates were lower than in a preliminary analysis (57%) based on short-term follow-up data for a subset of 98 subjects from the current study; this preliminary subset comprised the first 98 providing initial interviews and thus short follow-up periods (Brecht et al., 2000). This difference between results from shorter-term follow-up (with a subsample) and a longer-term perspective shows the importance of studying relapse across several temporal perspectives and in completed samples.
The rate of early relapse is of particular concern because results of studies of cocaine, heroin, and/or alcohol samples indicate that treatment clients who experience early relapse are likely to continue to have more difficulty maintaining abstinence on the short-term (Charney et al., 2010), while earlier periods of abstinence are predictive of longer-term abstinence (Dennis et al., 2007; Hser, et al., 2006; Siegal et al., 2002; Weisner et al., 2003). Similar to findings reported by Dennis et al. (2007), our results indicated relapse rates declined substantially for those achieving two or more years of abstinence post-treatment, although some risk of relapse continued to persist.
In spite of high early relapse rates, many in our MA user sample had subsequent periods of MA abstinence. These results support a cyclic nature of substance abuse (Scott et al., 2005; Hser et al., 2008). While our study considered MA abstinence directly following treatment discharge, it may also be important to consider long-duration abstinence wherever it occurs in the substance use history as an additional indicator of remission (Dennis et al., 2007; Hser, 2007). A third interview with the current sample (nearly completed) will allow the examination of abstinence duration and patterns within an even longer time-frame than reported in the current paper.
MA abstinence status at specific time points places our sample within the wide range of drug use remission at specific follow-up points after SUD treatment, varying across studies depending on type of drug, duration of follow-up, geography, and definition of remission (Calabria, 2010). Our results suggest that post-treatment remission patterns over 3-5 years may not be substantially worse for MA users even though MA users are often seen as more difficult to treat (CA Dept. of Alcohol and Drug Programs, 2007) partly because of the cognitive deficits and psychiatric problems such as paranoia related to MA use (Dean et al., 2013; Salo et al., 2011).
Only a small subset of client and treatment characteristics was significantly associated with time to relapse. Results showed a positive effect of longer index treatment duration, consistent with other shorter-term studies of treatment-as-usual of MA users in California (Hser et al., 2003; Rawson et al., 2008). Another predictor of longer time to relapse was experiencing three major problems (hallucinations, paranoia, and violent behavior) perceived by the participant as MA-related. Such perception may indicate participants' recognition of drug-related health and mental health problems and need for treatment, potentially increasing motivation to remain abstinent in an effort to reduce these problems (Falck et al., 2007; Laudet et al., 2009).
Also consistent with studies of drugs other than MA (Kissin et al., 2003; Moos and Moos, 2004; Siegal et al., 2002), our findings showed that self-help or additional treatment after the target treatment episode was associated with longer continuous post-treatment abstinence. Note, however, that while Gossop et al (2007) found a short-term effect on stimulant use for self-help attendees, no significant effect was found 4-5 years after treatment. Further study should examine whether specific patterns (timing and frequency) of self-help participation or other continuing care/after-care/relapse-prevention can improve the maintenance of abstinence for MA users.
Two risk factors were identified. Parental drug use was associated with earlier relapse. This factor has been identified as a risk for drug use initiation and adolescent drug problems (Hoffmann and Cerbone, 2002; Yule et al., 2013) and may indicate lasting vulnerabilities (Chassin et al., 2004). However, our data do not allow an examination of the mechanism of this risk. While our predictors were not significantly multicollinear, parental drug use may, nevertheless, act as a partial proxy for a broad set of early family environment risk factors. A second significant risk factor was involvement in MA sales, consistent with research showing that social context can influence patterns of substance use and treatment outcomes (Matto et al., 2007).
Across a wide range of possible predictors of continuing abstinence, we found few predictive user characteristics (e.g., from demographic, background, and substance use history domains), similar to findings from Hser et al. (2006) for predicting long-duration cocaine abstinence. Several alternative explanations should be considered in further analysis. Some background factors may diminish in influence as the substance use life course progresses, and predictors of abstinence and relapse may differ at varying points in the post-treatment period. For example, our early analyses with a small subset of the current sample showed age of first MA use as a predictor of time to relapse to MA use during the first two years after treatment (Brecht et al., 2000), but this variable was not significant in the current longer-term followup with the complete sample. Further research should include more detailed temporal patterns of personal and contextual characteristics concurrent with or proximal to substance use measures over time.
4.1 Methodological Considerations
Generalization to other geographic areas should be approached cautiously; however, the included county, its SUD treatment population, and the study sample were diverse in ethnicity and urban/rural representation. Substance use histories were self-reported and could be biased; however, we had good proximal reliability between self-reported current use and urine tests (88%) and nearly identical relationships between past year MA use and potential predictors from the current analysis for both proximal and distal recall of MA use for the 12 months prior to the initial interview.
Time to relapse is only one of many possible indicators of remission, recovery, and treatment outcomes (McLellan, 2010; White, 2012). Complementary indicators should also be considered for future studies to contribute to a comprehensive picture. Longer-term followup should also be studied, along with examination of frequency, timing, and predictors of transitions between use and abstinence, durations of successive episodes, and changes in these patterns over the life course. Note also that the modeling approach included several analyses, thus potentially reducing power and increasing the likelihood of a Type I error.
While a diverse set of potential predictors was included, there may be other salient personal and contextual factors not available in the current study (self-efficacy, quality of life, clinical psychiatric diagnosis and history, social networks), which should be considered in future research. Note also that our data did not include clinical psychiatric assessment and diagnoses, but used self-reported diagnoses of major mental illness as a proxy. This may account for inconsistency of our non-significant results for this predictor compared to other studies that have found psychiatric severity related to post-treatment drug use outcomes (Darke et al., 2007; Hser et al., 2007).
Even though data are not current (collected in 1999-2003 with reference to an index treatment episode in 1996), we feel that study results provide a contribution since there are few long-term studies of post-treatment MA use/abstinence. While SUD treatment approaches for MA use continue to improve and expand and a growing proportion of SUD treatment providers have MA-related experience and/or training, treatment for MA use has remained generally psycho-social in nature and MA-specific evidence-based approaches may still not be in widespread use. Further study could target more recent “treatment-as-usual” across a broad range of treatment programs to examine whether abstinence and relapse patterns remain consistent with our study results.
4.2 Conclusions
In conclusion, our study has provided a long-term perspective on the duration and predictors of time to relapse to MA use following treatment-as-usual for a large and diverse sample of MA users. Highest rates of relapse occurred early in the post-treatment period, with half the sample relapsing within six months. This predominant early relapse emphasizes the need for further development of continuing care and strategies for connecting/engaging MA users to abstinence-promoting resources immediately following SUD treatment (Dennis and Scott, 2012; McKay et al., 2009; Laudet and Humphreys, 2013). And while the risk of relapse decreased with increasing duration of continuing abstinence, some risk of relapse remained years after treatment discharge, thus pointing to a need for continuing availability of resources to the long-time abstinent MA user. In spite of high relapse rates, 13% of the full sample (23% of those with a full 5-year or longer followup period) sustained at least five years of continuing MA abstinence, and many more had additional periods of abstinence following their initial abstinence. Study results showed potential vulnerabilities that could be easily identified at treatment admission, such that specifically targeted interventions could be strengthened. Results also show that even with such vulnerabilities, longer duration of treatment and continuing treatment and/or self-help are associated with longer duration of continued abstinence for MA users.
Supplementary Material
Acknowledgments
The authors thank Dr. Priscilla Kehoe for suggestions on the revised manuscript, Katherine Lovinger for contributions to statistical analyses, and the entire project team for data collection and participants for sharing their experiences.
Role of fund source: Dr. Mary-Lynn Brecht received support from National Institute on Drug Abuse grants R01DA11020, R01DA025113, P30 DA016383-06; Diane Herbeck was supported by R01DA025113.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Contributors: MLB designed the study, conducted statistical analysis, and wrote first and final drafts of the paper. DH collaborated in writing the paper. Both authors contributed to and have approved the final manuscript.
Conflict of interest: Neither of the authors has a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adamson S, Sellman J, Frampton C. Patient predictors of alcohol treatment outcome: a systematic review. J Subst Abuse Treat. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Anderson K, Ramo D, Schulte M, Cummins BS. Substance use treatment outcomes for youth: integrating personal and environmental predictors. Drug Alcohol Depend. 2007;3:367–381. doi: 10.1016/j.drugalcdep.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglin MD, Hser YI, Chou CP. Reliability and validity of retrospective behavioral self-report by narcotics addicts. Eval Rev. 1993;17:90–107. [Google Scholar]
- Anglin MD, Urada D, Brecht ML, Hawken A, Rawson R, Longshore D. Criminal justice treatment admissions for methamphetamine use in California: a focus on proposition 36. J Psychoactive Drugs Suppl. 2007;4:367–381. doi: 10.1080/02791072.2007.10399898. [DOI] [PubMed] [Google Scholar]
- Boles SM, Joshi V, Grella C, Wellisch J. Childhood sexual abuse patterns, psychosocial correlates, and treatment outcomes among adults in drug abuse treatment. J Child Sex Abuse. 2005;14:39–55. doi: 10.1300/J070v14n01_03. [DOI] [PubMed] [Google Scholar]
- Brecht ML, von Mayrhauser C, Anglin MD. Predictors of relapse after treatment for methamphetamine use. J Psychoactive Drugs. 2000;32:211–220. doi: 10.1080/02791072.2000.10400231. [DOI] [PubMed] [Google Scholar]
- Brecht ML, Greenwell L, Anglin MD. Methamphetamine treatment: trends and predictors of retention and completion in a large stat treatment system (1992-2002) J Subst Abuse Treat. 2005;29:295–306. doi: 10.1016/j.jsat.2005.08.012. [DOI] [PubMed] [Google Scholar]
- Brecht ML, Greenwell L, von Mayrhauser C, Anglin MD. Two-year outcomes of treatment for methamphetamine use. J Psychoactive Drugs SARC Suppl. 2006;3:415–426. doi: 10.1080/02791072.2006.10400605. [DOI] [PubMed] [Google Scholar]
- Brecht ML, O'Brien A, von Mayrhauser C, Anglin MD. Methamphetamine use behaviors and gender differences. Addict Behav. 2004;29:89–106. doi: 10.1016/s0306-4603(03)00082-0. [DOI] [PubMed] [Google Scholar]
- Brecht ML, Urada D. Treatment outcomes for methamphetamine users: California Proposition 36 and comparison clients. J Psychoactive Drugs. 2011;43:68–76. doi: 10.1080/02791072.2011.602279. [DOI] [PubMed] [Google Scholar]
- Brigham J, Lessov-Schlaggar C, Javitz H, McElroy M, Krasnow R, Swan G. Reliability of adult retrospective recall of lifetime tobacco use. Nicotine Tob Res. 2008;10:287–299. doi: 10.1080/14622200701825718. [DOI] [PubMed] [Google Scholar]
- CA Dept. of Alcohol and Drug Programs. [Accessed 11/21/11];Methamphetamine Treatment: A Practitioner's Reference 2007. 2007 from http://www.adp.ca.gov/meth/pdf/MethTreatmentGuide.pdf.
- Calabria B, Degenhardt L, Briegleb C, Vos T, Hall W, Lynskey M, Callaghan B, Rana U, McLaren J. Systematic review of prospective studies investigating “remission” from amphetamine, cannabis, cocaine or opioid dependence. Addict Behav. 2010;35:741–749. doi: 10.1016/j.addbeh.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Charney DA, Zikos E, Gill KJ. Early recovery from alcohol dependence: factors that promote or impede abstinence. J Subst Abuse Treat. 2010;38:42–50. doi: 10.1016/j.jsat.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Chassin L, Fora D, King K. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: the effects of familial alcoholism and personality. J Abnorm Psychol. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Chen CY, Storr CL, Anthony JC. Early-onset drug use and risk for drug dependence problems. Addict Behav. 2009;34:319–322. doi: 10.1016/j.addbeh.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Agostino RB. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Mills KL, Williamson A, Havard A, Teesson M. Patterns of sustained heroin abstinence amongst long-term, dependent heroin users: 36 months findings from the Australian Treatment Outcome Study (ATOS) Addict Behav. 2007;32:897–906. doi: 10.1016/j.addbeh.2007.01.014. [DOI] [PubMed] [Google Scholar]
- Dean AC, Groman SM, Morales AM, London ED. An evaluation of the evidence that methamphetamine abuse causes cognitive decline in humans. Neuropsychopharmacol. 2013;38:259–274. doi: 10.1038/npp.2012.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denis C, Fatséas M, Beltran V, Bonnet C, Picard S, Combourieu I, Daulouède JP, Auriacombe M. Validity of the self-reported drug use section of the Addiction Severity Index and associated factors used under naturalistic conditions. Subst Use Misuse. 2012;47:356–363. doi: 10.3109/10826084.2011.640732. [DOI] [PubMed] [Google Scholar]
- Dennis M, Foss M, Scott C. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Eval Rev. 2007;31:585–612. doi: 10.1177/0193841X07307771. [DOI] [PubMed] [Google Scholar]
- Falck RS, Jichuan Wang J, Carlson RG, Krishnan LL, Leukefeld C, Booth B. Perceived need for substance abuse treatment among illicit stimulant drug users in rural areas of Ohio, Arkansas, and Kentucky. Drug Alcohol Depend. 2007;91:107–114. doi: 10.1016/j.drugalcdep.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell T, Freitas T, McFarlin S, Rutigliano P. The Timeline Followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Glasner-Edwards S, Mooney L, Marinelli-Casey P, Hillhouse M, Ang A, Rawson R the Methamphetamine Treatment Project Corporate Authors. Clinical course and outcomes of methamphetamine-dependent adults with psychosis. J Subst Abuse Treat. 2008;35:445–450. doi: 10.1016/j.jsat.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Gonzales R, Mooney L, Rawson RA. The methamphetamine problem in the United States. Annu Rev Public Health. 2010;31:385–398. doi: 10.1146/annurev.publhealth.012809.103600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Marsden J, Stewart D. Treatment outcomes of stimulant misusers: one year follow-up results from the National Treatment Outcomes Research Study (NTORS) Addict Behav. 2000;25:509–522. [PubMed] [Google Scholar]
- Gossop M, Marsden J, Stewart D, Kidd T. The National Treatment Outcome Research Study (NTORS): 4-5 year follow-up results. Addiction. 2003;98:291–303. doi: 10.1046/j.1360-0443.2003.00296.x. [DOI] [PubMed] [Google Scholar]
- Gossop M, Steward D, Marsden J. Attendance at Narcotics Anonymous and Alcoholics Anonymous meetings, frequency of attendance and substance use outcomes after residential treatment for drug dependence: a 5-year follow-up study. Addiction. 2007;103:119–125. doi: 10.1111/j.1360-0443.2007.02050.x. [DOI] [PubMed] [Google Scholar]
- Grella C, Joshi V. Treatment processes and outcomes among adolescents with a history of abuse who are in drug treatment. Child Maltreat. 2003;8:7–18. doi: 10.1177/1077559502239610. [DOI] [PubMed] [Google Scholar]
- Grella C, Lovinger K. 30-year trajectories of heroin and other drug use among men and women sampled from methadone treatment in California. Drug Alcohol Depend. 2011;118:251–258. doi: 10.1016/j.drugalcdep.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella C, Scott C, Foss M, Dennis M. Gender similarities and differences in the treatment, relapse, and recovery cycle. Eval Rev. 2008;32:113–137. doi: 10.1177/0193841X07307318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella C, Stein J, Weisner C, Chi F, Moos R. Predictors of longitudinal substance use and mental health outcomes for patients in two integrated service delivery systems. Drug Alcohol Depend. 2010;110:92–100. doi: 10.1016/j.drugalcdep.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillhouse M, Marinelli-Casey P, Gonzales R, Ang A, Rawson R the Methamphetamine Treatment Project Corporate Authors. Predicting in-treatment performance and post-treatment outcomes in methamphetamine users. Addiction. 2007;102:84–95. doi: 10.1111/j.1360-0443.2007.01768.x. [DOI] [PubMed] [Google Scholar]
- Hoffmann JP, Cerbone FG. Parental substance use disorder and the risk of adolescent drug abuse: an event history analysis. Drug Alcohol Depend. 2002;66:255–264. doi: 10.1016/s0376-8716(02)00005-4. [DOI] [PubMed] [Google Scholar]
- Hosmer D, Lemeshow S. Applied Logistic Regression. John Wiley; New York: 2000. [Google Scholar]
- Hser YI. Predicting long-term stable recovery from heroin addiction: findings from a 33-year follow-up study. J Addict Dis. 2007;26:51–60. doi: 10.1300/J069v26n01_07. [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E, Huang YC. Treatment outcomes among women and men methamphetamine abusers in California. J Subst Abuse Treat. 2005;28:77–85. doi: 10.1016/j.jsat.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E, Huang D, Brecht ML, Li L. Comparing the dynamic course of heroin, cocaine, and methamphetamine use over 10 years. Addict Behav. 2008;33:1581–1589. doi: 10.1016/j.addbeh.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Evans E, Teruya C, Huang D, Anglin MD. Predictors of short-term treatment outcomes among California's Proposition 36 participants. Eval Program Plann. 2007;30:187–196. doi: 10.1016/j.evalprogplan.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Hser YI, Huang YC, Chou CP, Anglin MD. Longitudinal patterns of treatment utilization and outcomes among methamphetamine abusers: a growth curve modeling approach. J Drug Issues. 2003;33:921–938. [Google Scholar]
- Hser YI, Stark ME, Paredes A, Huang YC, Anglin MD, Rawson R. A 12-year follow-up of a treated cocaine-dependent sample. J Subst Abuse Treat. 2006;30:219–226. doi: 10.1016/j.jsat.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Jaffe A, Du J, Huang D, Hser YI. Drug-abusing offenders with comorbid mental disorders: Problem se verity, treatment participation, and recidivism. J Subst Abuse Treat. 2012;43:244–250. doi: 10.1016/j.jsat.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen KJ, Rogier A, Donders T, Harrell FE, Vergouwe Y, Chen Q, Grobbee DE, Moons KG. Missing covariate data in medical research: to impute is better than to ignore. J Clin Epidemiol. 2010;63:721–727. doi: 10.1016/j.jclinepi.2009.12.008. [DOI] [PubMed] [Google Scholar]
- Kissin W, McLeod C, McKay J. The longitudinal relationship between self-help group attendance and course of recovery. Eval Program Plann. 2003;26:311–323. [Google Scholar]
- Laudet A, Becker J, White W. Don't wanna go through that madness no more: quality of life satisfaction as predictor of sustained remission from illicit drug misuse. Subst Use Misuse. 2009;44:227–252. doi: 10.1080/10826080802714462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A, Humphreys K. Promoting recovery in an evolving policy context: what do we know and what do we need to know about recovery support services? J Subst Abuse Treat. 2013;45:126–133. doi: 10.1016/j.jsat.2013.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matto H, Miller K, Spera C. Examining the relative importance of social context referents in predicting intention to change substance abuse behavior using the EASE. Addict Behav. 2007;32:1826–1834. doi: 10.1016/j.addbeh.2006.12.015. [DOI] [PubMed] [Google Scholar]
- Maxwell JC, Brecht ML. Methamphetamine: here we go again? Addict Behav. 2011;36:1168–1173. doi: 10.1016/j.addbeh.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan T. What is recovery? Revisiting the Betty Ford Institute Consensus Panel Definition. J Subst Abuse Treat. 2010;38:200–201. doi: 10.1016/j.jsat.2009.11.002. [DOI] [PubMed] [Google Scholar]
- McGlothlin WH, Anglin MD, Wilson BD. An Evaluation of the California Civil Addicts Program. National Institute on Drug Abuse; Rockville, MD: 1977. NIDA Services Research Monograph ADM 78-558. [Google Scholar]
- McKay JR, Carise D, Dennis ML, Dupont R, Humphreys K, Kemp J, Reynolds D, White W, Armstrong R, Chalk M, Haberle B, McLellan T, O'Connor G, Pakull B, Schwartzlose J. Extending the benefits of addiction treatment: practical strategies for continuing care and recovery. J Subst Abuse Treat. 2009;36:127–130. doi: 10.1016/j.jsat.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Pettinati HM, Morrison R, Feeley M, Mulvaney FD, Gallop R. Relation of depression diagnoses to 2-year outcomes in cocaine-dependent patients in a randomized continuing care study. Psychol Addict Behav. 2002;16:225–235. [PubMed] [Google Scholar]
- McKetin R, Najman JM, Baker AL, Lubman DI, Dawe S, Ali R, Lee NK, Mattick RP, Mamun A. Evaluating the impact of community-based treatment options on methamphetamine use: findings from the Methamphetamine Treatment Evaluation Study (MATES) Addiction. 2012;107:1998–2008. doi: 10.1111/j.1360-0443.2012.03933.x. [DOI] [PubMed] [Google Scholar]
- Meredith C, Jaffe C, Ang-Lee K, Saxon A. Implications of chronic methamphetamine use: a literature review. Harv Rev Psychiatry. 2005;13:141–154. doi: 10.1080/10673220591003605. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Kline-Simon AH, Delucchi KL, Moore C, Weisner CM. Ten-year stability of remission in private alcohol and drug outpatient treatment: non-problem users versus abstainers. Drug Alcohol Depend. 2012;125:67–74. doi: 10.1016/j.drugalcdep.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney L, Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Hunter J, Haning W, Colescott P, Ling W, Rawson R. Health conditions in methamphetamine-dependent adults 3 years after treatment. J Addict Med. 2009;3:155–163. doi: 10.1097/ADM.0b013e3181a17c79. [DOI] [PubMed] [Google Scholar]
- Moos R, Moos B. Long-term influence of duration and frequency of participation in Alcoholics Anonymous on individuals with alcohol use disorders. J Consult Clin Psychol. 2004;72:81–90. doi: 10.1037/0022-006X.72.1.81. [DOI] [PubMed] [Google Scholar]
- Murphy D, Hser YI, Huang D, Brecht ML, Herbeck D. Self-report of longitudinal substance use: comparison of the UCLA Natural History Interview and the Addiction Severity Index. J Drug Issues. 2010;40:495–516. doi: 10.1177/002204261004000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurco D, Bonito A, Lerner M, Balter M. Studying addicts over time: methodology and preliminary findings. Am J Drug Alcohol Abuse. 1975;2:183–196. doi: 10.3109/00952997509002733. [DOI] [PubMed] [Google Scholar]
- Parmar MK, Machin D. Survival Analysis. John Wiley & Sons; New York: 1995. [Google Scholar]
- Perron B, Bright C. The influence of legal coercion on dropout from substance abuse treatment: results from a national survey. Drug Alcohol Depend. 2008;92:123–131. doi: 10.1016/j.drugalcdep.2007.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Chang E, Urada D. The effectiveness of drug abuse treatment: a meta-analysis of comparison group studies. Drug Alcohol Depend. 2002;67:53–72. doi: 10.1016/s0376-8716(02)00014-5. [DOI] [PubMed] [Google Scholar]
- Rawson RA, Gonzales R, Brecht ML, Crèvecoeur-MacPhail D, Hemberg J. Integrated Substance Abuse Programs. Evaluation of the California Outcomes Measurement System (CalOMS) Final Report. University of California; Los Angeles: 2008. [Accessed 11/16/09]. from http://www.adp.state.ca.us/oara/pdf/CalOMS_Final_Report_2008.pdf. [Google Scholar]
- Rawson RA, Gonzales R, Marinelli-Casey P, Ang A. Methamphetamine dependence: a closer look at treatment responses and clinical characteristics associated with route of administration in outpatient treatment. Am J Addict. 2007;16:291–299. doi: 10.1080/10550490701389864. [DOI] [PubMed] [Google Scholar]
- Rawson RA, Huber A, Brethen P, Obert J, Gulati V, Shoptaw S, Ling W. Status of methamphetamine users 2-5 years after outpatient treatment. J Addict Dis. 2002;21:107–119. doi: 10.1300/j069v21n01_09. [DOI] [PubMed] [Google Scholar]
- Ribeiro M, Dunn J, Sesso R, Lima M, Laranjeira R. Crack cocaine: a five-year follow-up study of treated patients. Eur Addict Res. 2007;13:11–19. doi: 10.1159/000095810. [DOI] [PubMed] [Google Scholar]
- Roll J, Petry N, Stitzer M, Brecht ML, Peirce J, McCann M, Blaine J. Contingency management for the treatment of methamphetamine use disorders. Am J Psychiatry. 2006;163:1993–1999. doi: 10.1176/ajp.2006.163.11.1993. [DOI] [PubMed] [Google Scholar]
- Salo R, Gabay S, Fassbender C, Henik A. Distributed attentional deficits in chronic methamphetamine abusers: evidence from the Attentional Network Task (ANT) Brain Cogn. 2011;77:446–452. doi: 10.1016/j.bandc.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. Office of Applied Studies. [Accessed 7/20/13];Treatment episode data set—Data for states. 2013 available online at: http://wwwdasis.samhsa.gov/webt/newmapv1.htm.
- SAMHSA. Office of Applied Studies. Drug and Alcohol Services Information System (DASIS) Treatment Episodes Dataset (TEDS) National Admissions to SubstanceAbuse Treatment Services; 1996. [Accessed 12/21/11]. from http://wwwdasis.samhsa.gov/teds96/teds96.htm. [Google Scholar]
- SAMHSA. Trends in Methamphetamine Admissions to Treatment: 1997-2007. [Accessed 11/21/11];The TEDS Report. 2009 from http://www.oas.samhsa.gov/2k9/209/209MethTrends2k9.htm.
- Scott CK, Foss MA, Dennis ML. Pathways in the relapse—treatment—recovery cycle over 3 years. J Subst Abuse Treat. 2005;28:S63–S72. doi: 10.1016/j.jsat.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Sharma A, Upadhyaya S, Bansal P, Nijhawan M, Sharma D. A study of factors affecting relapse in substance abuse. Indian J L Sci. 2012;2:31–35. [Google Scholar]
- Siegal HA, Li L, Rapp RC. Abstinence trajectories among treated crack cocaine users. Addict Behav. 2002;27:437–449. doi: 10.1016/s0306-4603(01)00184-8. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Reback C, Larkins S, Wang P, Rotheram-Fuller E, Dang J, Yang X. Outcomes using two tailored behavioral treatments for substance abuse in urban gay and bisexual men. J Subst Abuse Treat. 2008;35:285–293. doi: 10.1016/j.jsat.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Simpson D, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Arch Gen Psychiatry. 2002;59:538–544. doi: 10.1001/archpsyc.59.6.538. [DOI] [PubMed] [Google Scholar]
- Simpson D, Joe G, Fletcher B, Hubbard R, Anglin MD. A national evaluation of treatment outcomes for cocaine dependence. Arch Gen Psychiatry. 1999;56:507–514. doi: 10.1001/archpsyc.56.6.507. [DOI] [PubMed] [Google Scholar]
- Steyerberg E, Eijkemans M, Harrell F, Jr, Habbema J. Prognostic modeling with logistic regression analysis: a comparison of selection and estimation methods in small data sets. Stat Med. 2000;19:1059–1079. doi: 10.1002/(sici)1097-0258(20000430)19:8<1059::aid-sim412>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- UNODC. [accessed 10/2/12];World Drug Report, Global Illicit Drug Trends. 2011 Available at http://www.unodc.org/unodc/en/data-and-analysis/WDR.html.
- UNODC. [accessed 10/4/12];World Drug Report, 2012. 2012 Available at http://www.unodc.org/unodc/en/data-and-analysis/WDR-2012.html.
- von Mayrhauser C, Brecht ML, Anglin MD. Use ecology and drug use motivations of methamphetamine users admitted to substance abuse treatment facilities in Los Angeles: an emerging profile. J Addict Dis. 2002;21:45–60. doi: 10.1300/j069v21n01_05. [DOI] [PubMed] [Google Scholar]
- Walitzer K, Dearing R. Gender differences in alcohol and substance use relapse. Clin Psychol Rev. 2006;26:128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Weisner C, Ray GT, Mertens JR, Satre DD, Moore C. Short-term alcohol and drug treatment outcomes predict long-term outcome. Drug Alcohol Depend. 2003;71:281–294. doi: 10.1016/s0376-8716(03)00167-4. [DOI] [PubMed] [Google Scholar]
- Yule AM, Wilens TE, Martelon MK, Simon A, Biederman J. Does exposure to parental substance use disorders increase substance use disorder risk in offspring? A 5-year follow-up study Am J Addict. 2013;22:460–465. doi: 10.1111/j.1521-0391.2013.12048.x. [DOI] [PubMed] [Google Scholar]
- White W. Recovery/remission From Substance Use Disorders. Great Lakes Addiction Technology Transfer Center (and Philadelphia Dept. of Behavioral Health and Intellectual Disability Services); Chicago: 2012. [Google Scholar]
- Witbrodt J, Mertens J, Kaskutas LA, Bond J, Chi F, Weisner C. Do 12-step meeting attendance trajectories over 9 years predict abstinence? J Subst Abuse Treat. 2012;43:30–43. doi: 10.1016/j.jsat.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


