Abstract
Most studies of immigrant health are cross-sectional and fail to collect information prior to migration, leading to potential bias and confounding. The present pilot study examines the feasibility of studying migrants prospectively, with baseline data collected before migration. The study followed two cohorts of Filipinos for one year, a migrant cohort (n=27) that emigrated to the U.S. and a second non-migrant cohort (n=26) in the Philippines. The one-year retention rate was 96% The migrant cohort arrived in the U.S. within 2 months of their baseline assessment. Migrants and non-migrants did not differ with regard to body mass index, waist circumference or waist to hip ratio at baseline or at follow-up. It is feasible to conduct a transnational, longitudinal study of two cohorts of Filipinos. This design provides important pre-migration information, is analogous to a natural experiment, can be upscaled, and allows for a rigorous examination of immigrant health.
Keywords: immigrant, prospective, Asian American, obesity, study design, transnational, comparative
Introduction
Obesity is a significant public health issue that shows little sign of abating.1 Within the United States, rates of obesity more than doubled over three decades, increasing from 15 percent in 1976-1980 to 36 percent in 2009-2010.1-3 These trends are also observed globally, with rates of obesity rising in countries worldwide.4-7
In general, immigrants to the U.S. appear to have lower rates of obesity than the general population. For example, data from the 2003-2008 National Health Interview Survey (NHIS) showed rates of obesity of 8.1% for newly arrived immigrants (less than 1 year) compared with 26.5% for U.S.-born adults.8 This observation of immigrants having better health indicators is sometimes called the “healthy migrant effect” or the “immigrant health advantage.”9
Yet, studies indicate that this advantage often disappears with time in the U.S. Data from the same NHIS study show that obesity prevalence increases with duration. For example, the rates were 8.1%, 10.8%, 14.6%, and 16.4% for immigrants with less than 1 year, 1-5 years, 5-9 years, and 10-15 years in the U.S., respectively.8
A widely adopted interpretation of these patterns is that obesity increases with “acculturation.”10-12 The basic premise is that immigrants adopt “American” diets and physical activity patterns over time, and that these behaviors contribute to obesity. Some evidence for dietary changes among Asian immigrants has been reported.10,13 Yet, there are other plausible explanations for these changes beyond acculturation that have been inadequately studied.
One alternative explanation is secular trends. Perhaps these increasing rates of obesity among immigrants simply reflect historical increases in obesity worldwide. Stated another way, the counterfactual is whether rates of obesity would rise even if these immigrants had never left their home countries. Indeed, many countries have seen increases in rates of obesity.14,15 Some of these increases are likely related to broader societal changes, including the presence of multinational corporations, social media, and globalization of the food supply.16-18
Studies of immigrants often fail to consider more global, transnational effects because they simply are not designed to do so. To study this process, one needs to have not only a cohort of immigrants, but a comparison cohort of non-migrants who remain in the sending country. This provides a necessary (but not sufficient) element in the design to allow for the assessment of secular trends.
An ideal dual-cohort design would include two additional features. First, the study must be longitudinal. Cross-sectional studies cannot adequately track how obesity changes with duration. Cross-sectional studies also raise the extremely problematic concern that duration (i.e. time in the U.S.) is confounded with other temporal factors, such as age, age of entry, and historical period.19-21
The few longitudinal studies that exist do not provide a consistent picture of the relation between duration and obesity. For example, one study followed youth, ages 11-19, and found that the body mass index (BMI) rises with age, but it is not clear if this was an age or duration effect.22 Another longitudinal study of Hispanic and Chinese immigrants, ages 45-88, noted subgroup variations.23 Duration was associated with BMI and waist circumference among Mexicans, but not among other Hispanics or Chinese. Thus, there is need for further longitudinal research.
Nevertheless, longitudinal data are not enough. Studies of immigrant health should ideally begin prior to migration, in the country of origin. A handful of studies consider these issues, including studies of Mexican migrants to the U.S. and Russian migrants to Israel,24-26 although these studies are extremely rare. Pre-migration information is critical if the claim is related to acculturation. After all, if the central claim is cultural change, then one must have initial information as to one's “baseline culture” and behaviors. For example, if an “American diet” is partially indexed by the eating of fast food27, then one would want to know how much fast food is being consumed in the country of origin.
Baseline data collected in the country of origin is critical given globalization. For example, the McDonald's restaurant chain serves 68 million people in over 119 countries daily.28 This is not a recent phenomenon. For instance, the first McDonald's opened in 1981 in the Philippines, and now has more than 400 restaurants there. Furthermore, McDonald's is but one of several fast food chains. A more popular chain in the Philippines is Jollibee, which serves hamburgers, fried chicken, and spaghetti. In 1984, Jollibee introduced the “Jollibee Champ” sandwich to compete directly with the McDonald's “Big Mac.”29 The point here is that American companies are selling American products in other countries, and local businesses in those countries are developing products that mimic American products.17,18 These observations raise serious questions about whether acculturation represents the adoption of new “American” practices because some behaviors may have begun pre-migration. There is no way to assess whether immigrant's behaviors actually change as a result of migration without pre-migration data.
One of the most important and comprehensive studies on these issues comes from the Mexican Family Life Survey (MxFLS), which was a nationally representative sample of Mexican adults. Their longitudinal follow-up included respondents who stayed in Mexico, as well as those who emigrated to the United States.26 But, the findings from Mexican migrants cannot be extrapolated to other immigrants, especially to immigrants coming from countries that do not share a border with the U.S. As noted by the authors, this geographic proximity seems to lessen the healthy immigrant effect among Mexican migrants compared with migrants from other countries.26 That is, there may be less of a health difference between migrants and non-migrants coming from Mexico compared with other countries.
Herein, we build on this body of research by studying migrants from the Philippines. This country provides an informative setting for such research. Many emigrants leave the Philippines to settle overseas each year. In 2010, there were an estimated 9.5 million Filipinos living in other countries, with about 3.2 million in the United States alone.30 About 100 Filipinos per day permanently settle in the U.S.31 Among Asian Americans as a whole, Filipino Americans are the second largest ethnic group, just behind Chinese Americans.32 Further, the Philippines has had strong ties with the United States since the late 1800s. An example of these ties is the recognition of American English as one of the country's two official languages.
This paper reports on the execution of a pilot study designed to address these limitations. The main goal was to assess the feasibility of implementing a dual-cohort, transnational longitudinal study. This approach to studying immigrant health is novel given the considerable logistical challenges of studying migration from one country to another.
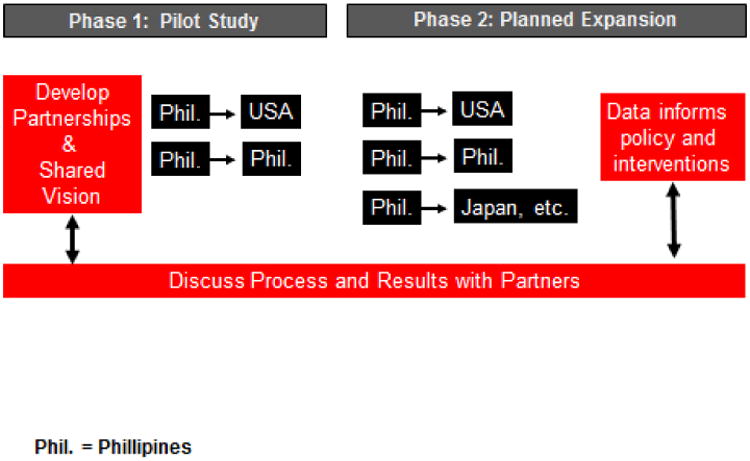
The study was conducted as a partnership with the Commission for Filipinos Overseas (CFO) and the Occupational Health Nurses Association of the Philippines (OHNAP) with university-based researchers. The project is conceptualized in two broad phases (Figure 1), with the initial phase designed to gather input from stakeholders, develop a shared agenda, and evaluate research strategies. This pilot study is part of the first phase. In the future, we hope to obtain support to enact the second phase of this project, whereby we upscale the pilot study and produce research findings that ultimately contribute to policy and interventions that may benefit members of the Filipino diaspora.
Figure 1. Process and vision.
Methods
Study Design Overview
Our pilot study followed two cohorts (migrant and non-migrant) over one year. Both cohorts had a baseline assessment in Manila, Philippines. The non-migrant cohort remained in the Philippines throughout the duration of the study and was assessed at three time points: baseline, 3 months, and 12 months. The migrant cohort left for the U.S. within 2 months of the baseline (the majority within 2 weeks), and follow-up data were collected from them in the U.S. Migrants were assessed at six time points: baseline, 3 months, 5 months, 7 months, 9 months, and 12 months. The 3 month follow-up corresponded to approximately a month or two after the migrant arrived in the U.S. Because migrants are highly mobile, we assessed them frequently within the U.S. in order to facilitate retention within the study and to ascertain the degree of internal migration within the U.S. To avoid respondent fatigue, not all data were collected at every wave.
This study received human subjects research approval from UCLA and the University of Washington.
Recruitment
Migrants (n=27) were recruited from the offices of the Commission on Filipinos Overseas (CFO), the Philippines national agency that regulates all legal, permanent exits from the country. Migrants regulated by the CFO plan to settle permanently in another country and exclude temporary workers and students. The CFO requires that all emigrants attend a 2-hour information session (pre-departure orientation seminar) which can only be taken after the migrant has secured their visas and all other formal approvals for exit. Usually, individuals attend this information session a few weeks prior to their departure, when they already have plane tickets or other travel documents in-hand.
With the approval of the CFO, our study recruited participants from this information session. Inclusion criteria for study participation were: plans to emigrate to the U.S. within the next 4 months, residency in the Philippines for the past 5 years, ability to speak English or Tagalog, and age of 21 years or older. Individuals were informed of the study procedures and invited to participate at the CFO office in Manila. Informed consent and study procedures were conducted in a private research office located about 20 minutes from the CFO office.
Non-migrants (n=26) were recruited in several ways to assess the feasibility of different recruitment strategies. The first was to find a control participant matched on age (within 5 years), gender, and educational level. Migrants were asked to pass information regarding the study to persons who fit the matching criteria for potential inclusion into the study. The second method was to recruit visitors to the CFO office who had no immediate plans to emigrate but were seeking information related to migration. The third method was via convenience sampling of persons working or living in Manila. The inclusion criteria were similar to those for migrants, except that non-migrants must have no plans to emigrate within the next 2 years. Participants provided informed consent and data at a private research office as noted above.
Information on non-responders was kept in a separate file which unfortunately was lost. Accordingly, we are unable to calculate response rates.
Process challenges and strategies
Our study included challenges typical of all studies (e.g. retention) as well as some unique ones. Table 1 summaries some of the key challenges and strategies employed to overcome them. We highlight several of these issues below.
Table 1. Challenges and Strategies for Implementing This Pilot Study.
| Key Challenges | Strategies |
|---|---|
|
| |
| Overseas Partnerships | |
|
|
|
| |
| Instrumentation | |
|
|
|
| |
| Cultural Sensitivity | |
|
|
|
| |
| Recruitment | |
|
|
|
| |
| Retention | |
|
|
Partnerships
Our study involved both governmental (CFO) and community partners (OHNAP) in another country. These partnerships made our study possible, but did raise several challenges. Some were relatively minor (e.g. coordinating across time zones), while others were more involved. An important one is the fact that governmental and community agencies are there to serve their constituents and not often vested in doing basic research. Therefore, it was quite important that the researchers meet periodically with CFO and OHNAP staff and leaders to collaborate on the research aims, ensure common goals, and update on progress. Further, governmental agencies do experience changes in leadership related to election cycles, and we cannot overstate the necessity of meeting face-to-face with new leaders to build trust and find common ground. We were very fortunate to have worked with such thoughtful partners who appreciated the scientific process and were generous with their time and insights.
Retention
To minimize loss of follow-up, we asked for the participants' contact information in both the Philippines and the U.S., as well as contact information for family and close friends. Participants were also provided with cell phones (migrants) or pre-paid cell phone minutes (non-migrants) to facilitate contact. We further maintained contact via a newsletter, birthday cards, and webpage. Participants received a modest monetary incentive based on the “wage payment” method33, adjusted for their location (i.e., Philippines or the U.S.). Additionally, migrants were contacted every other month to obtain updated contact information.
All staff with participant contact was born in the Philippines (regardless of whether the staff were in the U.S. or the Philippines). This was critical in order to maximize the principles of respect and cultural familiarity with participants. This was especially important for our U.S.- based staff. Although one can be of Filipino heritage or fluent in Tagalog, these surface characteristics do not ensure that someone understands the experiences of a Filipino emigrant. Indeed, there is evidence of cultural clashes between U.S.-born Filipinos and their Philippines-born counterparts.34 Moreover, there can be subtle differences in cultural values and expression that may be more easily communicated or recognized by someone born in the Philippines. Accordingly, all of our staff who had direct contact with participants were either Filipino (i.e., remained in the Philippines) or born in the Philippines. Among the latter, all had been to the Philippines within the past 5 years.
Translation and Language
All questionnaire materials were initially developed in English, then translated into Tagalog. Our goal was not simply to produce instruments that were semantically equivalent to their English versions but also psychometrically sound. In addition, we wanted an instrument that reflected the context of an interpersonal interaction between Filipinos. That is, we wanted an instrument that was more conversational than formal because of concerns that an overly formal instrument could encourage response bias (e.g. excessive formality might cause some participants to avoid speaking about sensitive topics). Accordingly, we used a collaborative iterative method for translation rather than the conventional translation-back translation method.35
Three bilingual persons in the United States independently translated our instruments. One translator taught Tagalog language classes at a university, another was a nurse and professional researcher, and the third was a local Filipino community leader who taught Tagalog in community-based settings. A fourth person -- bilingual and with a degree in linguistics -- compiled all three translations and selected the version of the translation (on an item-by-item basis) that appeared to be: (1) the most conceptually consistent with the construct being measured; and (2) the most appropriate for an in-person interview (for example, some translations were written in too formal a manner). This compilation was then reviewed by all of the translators and the research investigators for further commentary and revision. The instrument was pilot tested in the Philippines and amended before the instruments were finalized.
Data Collected
The study collected a wide variety of information, beginning with a 5-hour in-person baseline assessment. This included: (1) a 24-hour dietary recall and a food frequency questionnaire; (2) waist and hip circumference, height, and weight; (3) blood pressure (Omron brand electronic blood pressure machine); and (4) a questionnaire assessing demographics, psychosocial stress, discrimination, mental and physical health, acculturation, homesickness, and social desirability reporting bias. Additionally, physical activity was assessed with an accelerometer (New-Lifestyles, Lees Summit, Missouri) over one week. These measures were all assessed in-person for non-migrants for the duration of the study. For migrants, all baseline assessments were administered in-person and follow-up assessments were administered either in-person on over the telephone. Dietary information was obtained by a dietician, while blood pressure and anthropometrics were taken by a nurse. All staff collecting data received intensive training by the investigators (blinded) to ensure that standardized protocols were followed. Presently, we report on basic demographic characteristics and indicators of adiposity.
Analyses
We used chi-square and two-sample t-tests to compare the migrants and non-migrants on baseline characteristics. We used analysis of covariance to evaluate whether migrants and non-migrants differed in BMI, waist circumference or waist-to-hip ratio at baseline, adjusting for age and gender, or differed in change over time in these measures, adjusting for age, gender and baseline measurement
Results
The study achieved a retention rate of 96% (51/53) over the duration of one year. One participant was lost in each cohort. One participant suddenly lost contact with the study and all of his network members after 3 months for unknown reasons. Another person declined to continue participation after 6 months due to a busy work schedule. Both dropouts were young males.
Table 1 shows descriptive statistics of the sample at baseline (prior to migrants leaving the Philippines). Migrants and non-migrants did not differ with regard to mean age, educational level, or times lived abroad. However, migrants were more likely than non-migrants to be male, speak English at home, and report speaking English well or very well.
Migrants were less likely to be currently employed. About a third of the migrants were unemployed because they were about to leave the country. About 11% of migrants reported that they already had a job waiting for them in the U.S. (not shown).
About 44% of the migrants left for the U.S. within 2 weeks of the baseline assessment, with the remainder leaving within 2 months. The vast majority (88%) of non-migrants had no plans for leaving the Philippines.
The migrants had wanted to move to the U.S. for 10 years on average. About 26% reported that they were “very well prepared” and another 77% reported that they were “somewhat prepared” for their moves. About 74% of the migrants said that they would definitely return to the Philippines within the next 2 years. About 11% actually did return to the Philippines within one year.
Table 2 summarizes BMI, waist circumference, and the waist-to-hip ratio at baseline and one-year follow-up for the two cohorts. Migrants and non-migrants did not differ on BMI, waist circumference, or waist-to-hip ratio at baseline, adjusting for age and sex. Non-migrants showed a significant increase in BMI over one year (+0.4 k/m2; SD=0.6; p<.05), and migrants showed a non-significant trend towards increase (+0.2 k/m2; SD=1.6; p>.05). Neither cohort had significant changes in waist circumference or waist-to-hip ratio over one year. Migrants and non-migrants did not differ with regard to change over time in BMI, waist circumference, or waist-to-hip ratio, adjusting for age, sex and baseline measurement.
Table 2. Selected Characteristics of the Study Sample at Baseline, By Cohort.
| Non-migrants (n=26) | Migrants (n=27) | Sig. | |
|---|---|---|---|
| Age, mean (SD) | 34 (2) | 37 (2) | |
| Male, % | 46 | 74 | * |
| Education, % | |||
| High school or less | 11 | 0 | |
| Some college | 27 | 26 | |
| Finished college | 58 | 63 | |
| Some post-graduate | 4 | 11 | |
| Employment, % | |||
| Currently employed | 73 | 41 | * |
| Unemployed because moving to new country | 0 | 37 | |
| Unemployed for some other reason | 27 | 19 | |
| Speaks English at home, % | 27 | 52 | + |
| Speaks English well/very well, % | 31 | 89 | *** |
| When do you plan to move to USA, % | |||
| Within next 2 weeks | 0 | 44 | |
| Within next 2-4 weeks | 0 | 33 | |
| Within the next 1-2 months | 0 | 22 | |
| Within the next 3-24 months | 0 | 0 | |
| Two or more years from now | 12 | 0 | |
| No plan | 88 | 0 | |
| Times lived outside of the Philippines for longer than 1 year, % | |||
| Zero | 85 | 89 | |
| 1 time | 11 | 7 | |
| 2 times | 4 | 4 | |
| 3 or more | 0 | 0 | |
| How long have you wanted to move to U.S.? (years), mean (SD) | n/a | 10 (8) | |
| How prepared do you feel about moving to America?, % | |||
| Very well prepared | n/a | 26 | |
| Somewhat prepared | 70 | ||
| Unprepared | 4 | ||
| Very unprepared | 0 | ||
| Plan to temporarily visit the Philippines within next 2 years, % | |||
| Definitely yes | n/a | 74 | |
| Maybe | 22 | ||
| Definitely not | 4 |
Sig. = significance; SD = standard deviation; n/a = not applicable
Percentages may not add to 100 due to rounding
p<.10;
p<= 0.05;
p <= 0.01;
p <= 0.001
Discussion
The goal of this pilot study was to evaluate the feasibility of conducting a dual-cohort, transnational, longitudinal study. We recruited both a migrant and non-migrant cohort and retained 96% of participants over one year. Although our sample size is small, our preliminary observations provide interesting ideas for future work given the rarity of pre-migration information.
One observation concerns the use of English language. Language is often used as a measure of acculturation, with the presumption that use of English represents acculturation.36 This is a more complicated proposition in the case of the Philippines, where English is regularly used in business and educational contexts. It is striking that half of the migrants and a quarter of the non-migrants use English at home within the Philippines. One might presuppose a preferred usage of English in business settings to communicate with colleagues. Yet, the use of English in the home setting seems to be more related to the (historical and present-day) penetration of English into everyday life (i.e., television, radio, cinema, literature, advertising). This observation opposes conventional assumptions within the immigrant health literature that English language is a marker of acculturation to a new country36 and suggests new avenues of research focused on bilingualism.37
Additionally, a large majority of the migrants reported being able to speak English well or very well. This high level of English proficiency may be partially related to migrants' preparation for their journeys. Migrants noted that they had wanted to move to the U.S. for many years, a decade on average. Because migrant participants had visas to permanently settle in the U.S., it seems reasonable to presume that participants actively learn about and prepare for life in their new country as much as possible prior to migrating, rather than simply being “empty vessels” that passively acculturate only after migration.
About a quarter of migrants felt very well-prepared, while most felt somewhat prepared, and a small minority felt unprepared. We do not have detailed information about the nature of this preparation; future studies should consider incorporating more comprehensive measures of migration preparedness. Indeed, there are many businesses within the Philippines that develop classes that specifically prepare people for travel, work, and settlement in the United States. Some of these classes are specific to occupations (e.g. nursing), while others are more for everyday life. Preparation for emigration can be considered the acquisition of cultural capital. In general, higher levels of capital (social capital, human capital, etc.) are related to improved health.38,39 This suggests the hypothesis that greater pre-migration preparation may be related to better health outcomes.25
These findings highlight the value of collecting pre-migration data. As noted above, many migrants reported fluency with English while in the Philippines. Had we only observed data post-migration, as is commonplace among studies of Asian American immigrants, we might assume that those migrants acquired proficiency in the U.S. Yet, data showing that many immigrants report proficiency with English in their home countries requires a re-examination of our assumptions.
Another interesting observation concerns return migration. The literature on Asian American immigrant health has remained relatively silent on this topic, although it is gaining traction in studies of Mexican migrants.40-42 At baseline, 3 out of 4 migrants said that they would “definitely” plan to visit the Philippines within the next 2 years, while another 22% said “maybe.” Over the course of 1 year, we found that 11% actually did return. We had expected no returns in this short period because travel to the Philippines can be very expensive and very challenging for people who are starting new jobs.
Most studies of acculturation assume that once in the U.S., the immigrants lives are shaped by exposure to American norms. But the process of return migration suggests that for some immigrants, their lives are shaped by the dual exposure to both American society and that of their parent countries. Analytically, it suggests that there may be an interaction between acculturation measures and return migration, such that the effects of acculturation measures (such as duration in the U.S.) may be attenuated among those who frequently return to their home countries compared to those who do not return.
In debriefing, one migrant mentioned returning to get married while other participants cited business travel. These anecdotal observations suggest additional questions for future inquiry. Business travel, for example, raises questions about the validity of other measures, such as income, which may be more complicated for individuals earning money overseas. Similarly, in the case of marriage, it was not clear that the participant's spouse would be able to emigrate to the U.S. in the near future. Therefore, standard questions about things like marital status may not capture the complexity of social relationships that may be dispersed over multiple countries. More generally, future work should consider the effects of social networks and settlement in ethnic enclaves as potential moderators.43-45
In future studies, there is one additional issue related to temporal change that could be considered. We have discussed how duration in the U.S. could represent not only acculturation, but secular trends. There is at least one other interpretation of duration effects related to the intersection between nativity and racial stratification.46 Immigrants are not merely sojourners who are warmly received in a new country. Instead, immigrants enter a socially stratified society.47 In the U.S., immigration policy has historically been tied to race and ethnicity.48 In the case of Filipinos, they are suddenly given a new identity as “Asians,” and can potentially become subject to racial bias.49 Accordingly, the longer they stay here, the greater the potential exposure to discrimination.49,50 Hence, duration may not simply be a proxy for age, acculturation to an American life or secular trends, but can also represent greater accumulation of social stressors and allostatic load (the “wear and tear” on body systems related to chronic stress).51 There is a long history of stress research among immigrants52-54, but this literature is less developed with regard to the study of obesity.55 One possible extension is whether the stress of minority status over time might explain the increase of obesity with duration.55 Indeed, a recent cross-sectional study showed that obesity rose with duration only among Asian Americans who reported racial discrimination; among Asian Americans who reported no discrimination, there was no relationship between obesity and duration.56
Overall, we found no statistically significant differences between migrants and non-migrants with regard to changes in BMI, waist circumference or waist-to-hip ratio over one year. This null finding is possibly due to small samples, but not surprising for a one-year study. Within non-migrants, there was a small and statistically significant increase in BMI, whereas among migrants there was a small nonsignificant increase in BMI over time. These analyses are too preliminary to draw any conclusions, but the trends towards increasing BMI across both cohorts are consistent with the hypothesis of secular changes in obesity.1,16
The study has other valuable features. It is focused on a single ethnic group. This is useful because prior research has criticized studies that aggregate all Asian ethnic groups without attention to within-group heterogeneity. Additionally, the study was culturally tailored to this group. We did not attempt to back-translate our instrument from Tagalog to English. Instead, our translated instrument was vetted through a collaborative effort that involved about 12 people in 2 nations throughout its development over 6 months. As noted above, this cultural tailoring was not merely in the translation and adaptation of instruments, but incorporated into the hiring of research staff who had first-hand knowledge of the Filipino immigrant experience.
The cultural tailoring was one of several strategies used to maximize retention in the study. We believe that each of our strategies was useful in retention, although probably the most important strategy was contacting migrants every other month. One migrant moved four times over 12 months, and would probably have been lost to follow-up without this regular contact. Frequent contact also helped build rapport.
A limitation of our pilot study was related to the non-representative sampling of migrants. For future work, we plan to recruit participants through stratified random sampling of households, which would improve generalizability and reduce sampling bias. An additional limitation is that we cannot randomize individuals to migration or non-migration, limiting our ability to make inferences about the counterfactual (i.e. would migrants remain the same if they did not emigrate?). The lack of randomization raises questions about selection bias. However, we can employ propensity score matching to mitigate some concerns about selection effects. 57,58
We believe that the dual-cohort design provides a useful framework for future studies of Asian American immigrants and facilitates the study of new research questions. These questions include basic information as to what is known pre-migration and the effects of return migration. This framework can be applied to examining the diaspora of immigrants (e.g. Filipino migrants to Canada and Japan). Contrasting migrants to non-migrants allows for assessment of acculturation versus secular trends. With the globalization of products, media, tastes, and behaviors,16 it is more important than ever to consider the effects of secular trends when studying the health of migrants.
Table 3. Change in Adiposity Measures over One Year, by Cohort.
| Baseline mean (SD) | Follow-up mean (SD) | Change (SD) | P-value, adjusted difference at baseline | P-value, change within group | P-value, adjusted difference in change over time | |
|---|---|---|---|---|---|---|
| BMI | ||||||
| Non-migrants | 22.7 (4.1) | 23.1 (4.0) | +0.4 (0.6) | .48 | .005 | .87 |
| Migrants | 25.0 (4.4) | 25.2 (4.4) | +0.2 (1.6) | .63 | ||
| Waist circumference | ||||||
| Non-migrants | 79.6 (11.2) | 79.6 (10.7) | 0.007 (3.0) | .37 | .99 | .86 |
| Migrants | 86.2 (12.3) | 85.1 (12.0) | -1.04 (6.9) | .47 | ||
| Waist to hip ratio | ||||||
| Non-migrants | 0.88 (0.06) | 0.87 (0.06) | -0.01 (0.04) | .95 | .23 | .21 |
| Migrants | 0.91 (0.06) | 0.91 (0.06) | -0.0006 (0.07) | .97 |
Change within groups was assessed using paired t tests. Adjusted difference at baseline was adjusted for age and sex. Adjusted difference in change over time was adjusted for baseline measure, age and sex
Acknowledgments
The research reported in this publication was supported by the National Cancer Institute of the National institutes of Health (NIH) under award number 1R21CA137297, NIH – National Center for Research Resources award number 5KL2RR025015, and through additional support from the NIH/National Center for Advancing Translational Science UCLA CTSI Grant Number UL1TR000124, and the California Center for Population Research at UCLA) under grant number R24-HD041022 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. We thank Scarlett Lin-Gomez and several anonymous reviewers for feedback on earlier drafts of this document. The authors also wish to acknowledge the Commission on Filipinos Overseas; Occupational Health Nurses Association of the Philippines, Inc.; Mr. Eularito Tagalog; Ms. Anna Espano; Ms. Mercedes Castillo; Ms. Victoria Alcantara; Mr. John Santos; Ms. Kathlene Manimtim; and Ms. Margot Perrin for their assistance with this research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Institute for Occupational Safety and Health.
Contributor Information
Gilbert C. Gee, Fielding School of Public Health at the University of California, Los Angeles.
A.B. de Castro, School of Nursing and Health Studies at the University of Washington— Bothell.
May C. Wang, Fielding School of Public Health at the University of California, Los Angeles.
Catherine M. Crespi, Fielding School of Public Health at the University of California, Los Angeles.
Brittany N. Morey, Fielding School of Public Health at the University of California, Los Angeles.
Kaori Fujishiro, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Bibliography
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Obesity in the United States, 2009-2010. 2012 [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among us adults, 1999-2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among us adults, 1999-2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 4.Prentice AM. The emerging epidemic of obesity in developing countries. International journal of epidemiology. 2006;35(1):93–99. doi: 10.1093/ije/dyi272. [DOI] [PubMed] [Google Scholar]
- 5.Dahly DL, Gordon-Larsen P, Emch M, Borja J, Adair LS. The spatial distribution of overweight and obesity among a birth cohort of young adult Filipinos (Cebu Philippines, 2005): an application of the Kulldorff spatial scan statistic. Nutrition & diabetes. 2013;3:e80. doi: 10.1038/nutd.2013.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: a review. Bulletin of the World Health Organization. 2004;82(12):940–946. [PMC free article] [PubMed] [Google Scholar]
- 7.Schmeer KK. Union Transitions and Changes in BMI among Adults in Mexico. Journal of health and social behavior. 2012;53(2):263–275. doi: 10.1177/0022146512445898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh G, Siahpush M, Hiatt R, Timsina L. Dramatic Increases in Obesity and Overweight Prevalence and Body Mass Index Among Ethnic-Immigrant and Social Class Groups in the United States, 1976–2008. J Community Health. 2011;36(1):94–110. doi: 10.1007/s10900-010-9287-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Read JnG, Reynolds MM. Gender Differences in Immigrant Health: The Case of Mexican and Middle Eastern Immigrants. Journal of health and social behavior. 2012;53(1):99–123. doi: 10.1177/0022146511431267. [DOI] [PubMed] [Google Scholar]
- 10.Akresh IR. Dietary Assimilation and Health among Hispanic Immigrants to the United States. Journal of health and social behavior. 2007;48(4):404–417. doi: 10.1177/002214650704800405. [DOI] [PubMed] [Google Scholar]
- 11.Popkin BM, Udry JR. Adolescent Obesity Increases Significantly in Second and Third Generation U.S. Immigrants: The National Longitudinal Study of Adolescent Health. The Journal of Nutrition. 1998;128(4):701–706. doi: 10.1093/jn/128.4.701. [DOI] [PubMed] [Google Scholar]
- 12.Garcia L, Gold EB, Wang L, Yang X, Mao M, Schwartz AV. The relation of acculturation to overweight, obesity, pre-diabetes and diabetes among U.S. Mexican-American women and men. Ethnicity & disease. 2012;22(1):58–64. [PMC free article] [PubMed] [Google Scholar]
- 13.Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and Non-Hispanic Whites. J Nutr. 2011;141(10):1898–1906. doi: 10.3945/jn.111.141473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song Y, Wang HJ, Ma J, Wang Z. Secular trends of obesity prevalence in urban Chinese children from 1985 to 2010: gender disparity. PloS one. 2013;8(1):e53069. doi: 10.1371/journal.pone.0053069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song Y, Park MJ, Paik HY, Joung H. Secular trends in dietary patterns and obesity-related risk factors in Korean adolescents aged 10-19 years. International journal of obesity. 2010;34(1):48–56. doi: 10.1038/ijo.2009.203. [DOI] [PubMed] [Google Scholar]
- 16.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutrition Reviews. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ng SW, Dunford E. Complexities and opportunities in monitoring and evaluating US and global changes by the food industry. Obesity Reviews. 2013;14:29–41. doi: 10.1111/obr.12095. [DOI] [PubMed] [Google Scholar]
- 18.Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obesity Reviews. 2013;14:21–28. doi: 10.1111/obr.12107. [DOI] [PubMed] [Google Scholar]
- 19.Stevens G. The Age-Length-Onset Problem in Research on Second Language Acquisition Among Immigrants. Language Learning. 2006;56(4):671–692. [Google Scholar]
- 20.Antecol H, Bedard K. Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 21.Park J, Myers D, Kao D, Min S. Immigrant obesity and unhealthy assimilation: alternative estimates of convergence or divergence, 1995-2005. Social science & medicine. 2009;69(11):1625–1633. doi: 10.1016/j.socscimed.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris K, Perreira KM, Lee D. Obesity in the transition to adulthood: Predictions across race/ethnicity, immigrant generation, and sex. Archives of Pediatrics & Adolescent Medicine. 2009;163(11):1022–1028. doi: 10.1001/archpediatrics.2009.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Albrecht SS, Roux AVD, Kandula NR, Osypuk TL, Ni H, Shrager S. Immigrant assimilation and BMI and waist size: A longitudinal examination among hispanic and chinese participants in the multi-ethnic study of atherosclerosis. Obesity. 2013;21(8):1695–1703. doi: 10.1002/oby.20104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Breslau J, Borges G, Tancredi DJ, et al. Health selection among migrants from Mexico to the US: childhood predictors of adult physical and mental health. Public health reports. 2011;126(3):361. doi: 10.1177/003335491112600310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chou KL. Pre-migration planning and depression among new migrants to Hong Kong: The moderating role of social support. Journal of Affective Disorders. 2009;114(1–3):85–93. doi: 10.1016/j.jad.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: new findings from the Mexican Family Life Survey. American journal of public health. 2008;98(1):78. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Unger J, Reynolds K, Shakib S, Spruijt-Metz D, Sun P, Johnson CA. Acculturation, Physical Activity, and Fast-Food Consumption Among Asian-American and Hispanic Adolescents. J Community Health. 2004;29(6):467–481. doi: 10.1007/s10900-004-3395-3. [DOI] [PubMed] [Google Scholar]
- 28.About McDonald's: Our Global History. [Accessed 3/10/2014];2014 https://www.mcdonalds.com.ph/content/page/about.
- 29.Jollibee. [Accessed 3/10/2014];2014 http://en.wikipedia.org/wiki/Jollibee. 2014.
- 30.Affairs DoF, editor. Overseas CoF. Stock Estimates of Overseas Filipinos. 2010. [Google Scholar]
- 31.Galias RAG. Personal communication. 2012 [Google Scholar]
- 32.Bureau USC. Asian/Pacific American Heritage Month, May 2010. In: Bureau USC, editor. Profile America: Facts for Features. 2010. [Google Scholar]
- 33.Phillips TB. A Living Wage for Research Subjects. The Journal of Law, Medicine & Ethics. 2011;39(2):243–253. doi: 10.1111/j.1748-720X.2011.00593.x. [DOI] [PubMed] [Google Scholar]
- 34.Tuason MTG, Taylor AR, Rollings L, Harris T, Martin C. On both sides of the hyphen: Exploring the Filipino-American identity. Journal of Counseling Psychology. 2007;54(4):362–372. [Google Scholar]
- 35.Douglas SP, Craig CS. Collaborative and Iterative Translation: An Alternative Approach to Back Translation. Journal of International Marketing. 2007;15(1):30–43. [Google Scholar]
- 36.Gee GC, Walsemann KM, Takeuchi DT. English proficiency and language preference: testing the equivalence of two measures. American journal of public health. 2010;100(3):563–569. doi: 10.2105/AJPH.2008.156976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schachter A, Kimbro RT, Gorman BK. Language Proficiency and Health Status: Are Bilingual Immigrants Healthier? Journal of health and social behavior. 2012;53(1):124–145. doi: 10.1177/0022146511420570. [DOI] [PubMed] [Google Scholar]
- 38.Dufur MJ, Parcel TL, Mckune BA. Capital and Context: Using Social Capital at Home and at School to Predict Child Social Adjustment. Journal of health and social behavior. 2008;49(2):146–161. doi: 10.1177/002214650804900203. [DOI] [PubMed] [Google Scholar]
- 39.Herd P. Education and Health in Late-life among High School Graduates: Cognitive versus Psychological Aspects of Human Capital. Journal of health and social behavior. 2010;51(4):478–496. doi: 10.1177/0022146510386796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Davies AA, Borland RM, Blake C, West HE. The dynamics of health and return migration. PLoS medicine. 2011;8(6) doi: 10.1371/journal.pmed.1001046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ceballos M. Simulating the Effects of Acculturation and Return Migration on the Maternal and Infant Health of Mexican Immigrants in the United States: A Research Note. Demography. 2011;48(2):425–436. doi: 10.1007/s13524-011-0017-4. [DOI] [PubMed] [Google Scholar]
- 42.Ullmann SH, Goldman N, Massey DS. Healthier before they migrate, less healthy when they return? The health of returned migrants in Mexico. Social science & medicine. 2011;73(3):421–428. doi: 10.1016/j.socscimed.2011.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nobari TZ, Wang MC, Chaparro MP, Crespi CM, Koleilat M, Whaley SE. Immigrant enclaves and obesity in preschool-aged children in Los Angeles County. Social science & medicine. 2013;92:1–8. doi: 10.1016/j.socscimed.2013.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Osypuk TL, Diez Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The Multi-ethnic Study of Atherosclerosis. Social science & medicine. 2009;69(1):110–120. doi: 10.1016/j.socscimed.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walton E. Resurgent Ethnicity among Asian Americans: Ethnic Neighborhood Context and Health. Journal of health and social behavior. 2012;53(3):378–394. doi: 10.1177/0022146512455426. [DOI] [PubMed] [Google Scholar]
- 46.Grollman EA. Multiple Disadvantaged Statuses and Health: The Role of Multiple Forms of Discrimination. Journal of health and social behavior. 2014;55(1):3–19. doi: 10.1177/0022146514521215. [DOI] [PubMed] [Google Scholar]
- 47.Kim NY. Imperial Citizens: Koreans and Race from Seoul to LA. Stanford, CA: Stanford University Press; 2008. [Google Scholar]
- 48.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Social science & medicine. 2012;75(12):2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 49.Gee GC, Ro A, Shariff-Marco S, Chae D. Racial discrimination and health among Asian Americans: evidence, assessment, and directions for future research. Epidemiologic reviews. 2009;31:130–151. doi: 10.1093/epirev/mxp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Social science & medicine. 2012;75(12):2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 51.Kaestner R, Pearson JA, Keene D, Geronimus AT. Stress, Allostatic Load and Health of Mexican Immigrants. Social science quarterly. 2009;90(5):1089–1111. doi: 10.1111/j.1540-6237.2009.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Padilla AM, Wagatsuma Y, Lindholm KJ. Acculturation and personality as predictors of stress in Japanese and Japanese-Americans. The Journal of social psychology. 1985;125(3):295–305. doi: 10.1080/00224545.1985.9922890. [DOI] [PubMed] [Google Scholar]
- 53.Lee H, Ahn H, Miller A, Park CG, Kim SJ. Acculturative stress, work-related psychosocial factors and depression in Korean-Chinese migrant workers in Korea. Journal of occupational health. 2012;54(3):206–214. doi: 10.1539/joh.11-0206-oa. [DOI] [PubMed] [Google Scholar]
- 54.Noh S, Avison WR. Asian immigrants and the stress process: a study of Koreans in Canada. Journal of health and social behavior. 1996;37(2):192–206. [PubMed] [Google Scholar]
- 55.Tseng M, Fang CY. Stress is associated with unfavorable patterns of dietary intake among female chinese immigrants. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2011;41(3):324–332. doi: 10.1007/s12160-010-9259-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gee GC, Ro A, Gavin A, Takeuchi DT. Disentangling the Effects of Racial and Weight Discrimination on Body Mass Index and Obesity Among Asian Americans. American journal of public health. 2008;98(3):493–500. doi: 10.2105/AJPH.2007.114025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guo S, Fraser MW. Propensity score analysis. Statistical methods and applications. 2010 [Google Scholar]
- 58.Rubin DB. Estimating causal effects from large data sets using propensity scores. Annals of internal medicine. 1997;127(8_Part_2):757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]


