Abstract
Objective
Since Hispanic ethnicity in the United States is heterogeneous, the purpose of this study was to determine the epidemiology of peripheral arterial disease (PAD) within US Hispanic/Latino groups defined by national background.
Methods
9,648 men and women over the age of 45 years enrolled in the Hispanic Community Health Study – Study of Latinos (HCHS-SOL) included in this analysis. The ankle brachial index (ABI) was computed as the higher of the posterior tibial and dorsalis pedis systolic blood pressures (SBP) for each leg divided by the higher brachial artery SBP. The index ABI was the higher of the two. An ABI ≤ 0.90 was criterion for the presence of PAD.
Results
The mean age was 56 years and 55% were female. Overall, the prevalence of an ABI ≤ 0.90 (PAD), 0.90 to 0.99 (borderline), 1.0 to 1.39 (normal) and ≥ 1.40 (high) was 5.7, 19.3, 72.5 and 2.6%, respectively. After multivariable adjustment for PAD risk factors, and compared to Mexicans, Cubans had nearly a 3-fold higher odds for PAD (OR: 2.9, 95% CI: 1.9 – 4.4). The odds of PAD for the other Hispanic/Latino groups ranged from 1.2 to 1.8. Although males had over a 3-fold higher odds of an ABI ≥ 1.40 (3.6, 2.0 – 6.5), the odds did not differ significantly by Hispanic/Latino background.
Conclusions
Compared to Mexican Americans, all other Hispanic/Latino background groups have a significantly higher odds of having PAD, with the odds being nearly 3-fold higher among Cubans.
INTRODUCTION
In the United States, peripheral arterial disease (PAD) affects over 8 million adults 1 and is associated with significant morbidity and mortality. 2,3 In addition to clinical symptoms, the presence of PAD is typically determined using the ankle-brachial index (ABI). 4 Using ABI data from the Multi-Ethnic Study of Atherosclerosis (MESA), and compared to non-Hispanic Whites, we have previously reported that Hispanic Americans have approximately half the risk of PAD 5, defined as an ABI < 0.90.
Although usually classified as a single ethnic group (as was the case for the aforementioned studies), Hispanic/Latinos are heterogeneous from cultural, socioeconomic, and genetic perspectives and these differences are manifest in measures of cardiovascular disease (CVD). Indeed, recent results from the Hispanic Community Health Study – Study of Latinos (HCHS – SOL) showed that, compared to Mexican Americans, Dominican and Cuban Americans have significantly higher rates of hypertension, while the rates of diabetes mellitus are significantly lower among Cuban Americans and South Americans, and rates of smoking are significantly higher among Cuban and Puerto Rican Americans. 6 Similarly, findings from the Multi-Ethnic Study of Atherosclerosis shows Central and South Americans have significantly lower levels of prevalent coronary artery calcium, Dominican Americans have significantly lower carotid intimal medial thickness and both Puerto Rican and Dominican Americans have significantly higher left ventricular volumes. 7
Given this, we conducted a study to test the hypothesis of differential risks of PAD among the different Hispanic/Latino ethnic groups enrolled in the Hispanic Community Health Study – Study of Latinos.
METHODS
Study Population
The design, implementation and recruitment strategies for the HCHS – SOL have been published in detail previously. 8,9 In brief, between March 2008 and June 2011, the HCHS-SOL recruited and then examined 16,415 self-identified Hispanic/Latino persons between the ages of 18 to 74 years. Households were selected using a stratified 2-stage area probability sample design. Census block groups were randomly selected in the defined community areas of each field center (Bronx, New York; Chicago, Illinois; Miami, Florida; San Diego, California), and households were randomly selected in each sampled block group. Oversampling occurred at each stage, with block groups in areas of Hispanic/Latino concentration, households associated with a Hispanic/ Latino surname, and persons aged 45 to 74 years selected at higher rates than their counterparts. Sampling weights were generated to reflect the probabilities of selection at each stage.{Lavange:2010dj}As a result, the HCHS/SOL included participants from Cuban, Dominican, Mexican, Puerto Rican, Central American, and South American backgrounds. Institutional review boards at each participating institution approved the study and written informed consent was obtained from all participants.
Participants were defined as first generation if they were foreign-born and with parents that were both foreign born. Second generation was defined as US born with at least one foreign-born parent. In addition, foreign-born adults with at least one US born parent were classified as second generation to reflect their mixed cultural backgrounds.2
Six thousand seven hundred and one participants were under the age of 45 years and were not examined using the ankle brachial index. Given this, and excluding other individuals with missing ABI data (n = 66), the sample size for the current analysis was 9,648 men and women.
Data Collection
Information on demographic factors, socioeconomic status, acculturation, cigarette smoking, physical activity and medical history was obtained by survey questionnaires. To complete a current medication inventory, participants were instructed to bring all prescription and nonprescription medications taken in the past month.
Participants were asked to fast and refrain from smoking for 12 hours prior to the examination and to avoid vigorous physical activity the morning of the visit. Height was measured to the nearest centimeter and body weight to the nearest 0.1 kg. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. After a 5-minute rest period, 3 seated blood pressure measurements were obtained with an automatic sphygmomanometer; the second and third readings were averaged and the result used in the analysis. Hypertension was defined as a systolic blood pressure greater than 139 mmHg, a diastolic blood pressure greater than 89 mmHg or taking a blood pressure lowering medication. Blood samples, including plasma glucose (fasting and after a 2-hour oral glucose load) were collected according to standardized protocols. Total serum cholesterol was measured using a cholesterol oxidase enzymatic method and high-density lipoprotein (HDL) cholesterol with a direct magnesium/dextran sulfate method. Low-density lipoprotein (LDL) cholesterol was calculated using the Friedewald equation. 10 Dyslipidemia was defined as a total to HDL cholesterol ratio greater than 5 or use of a cholesterol lowering medication. Plasma glucose was measured using a hexokinase enzymatic method (Roche Diagnostics). Hemoglobin A1c (HbA1c) was measured using a Tosoh G7 Automated HPLC Analyzer (Tosoh Bioscience). Diabetes mellitus was defined as a fasting glucose greater than 125 mg/dL or taking a medication to control blood glucose.
A standardized method was used for determining the ABI. Specifically, with the patient sitting, the circumference of each upper arm was measured and used to determine the appropriate cuff size to be used: Adult (12 cm width) for arm circumference of < 32 cm, Large Adult (16 cm width) for arm circumference of 32-42 cm and Thigh (20 cm width) for arm circumference of ≥ 43 cm. Then, starting in the right arm and moving counter-clockwise, systolic blood pressures were obtained once in the bilateral brachial, anterior tibial and posterior tibial arteries. The limb specific ABI was computed using the higher of the ipsilateral ankle artery pressures and dividing by the higher of the two brachial artery pressures. The index ABI was the lower of the two limb values and the presence of PAD defined as an ABI < 0.90, while an ABI greater than 1.39 is indicative of stiff arteries. 11
Statistical Analysis
All reported values (means, prevalence, and odds ratios [ORs]) were weighted to adjust for sampling probability and nonresponse. More specifically, all reported values were weighted to account for the disproportionate selection of the sample and to at least partially adjust for any bias effects due to differential nonresponse in the selected sample at the household and person levels. The adjusted weights were also trimmed to limit precision losses due to the variability of the adjusted weights, and calibrated to the 2010 Census characteristics by age, sex and Hispanic background in each field site's target population. All analyses also account for cluster sampling and the use of stratification in sample selection.
Adjusted prevalence estimates for the target population of Hispanic/Latinos in the four HCHS/SOL communities were calculated using survey-specific logistic regression procedures adjusting each Hispanic/Latino group to the age, gender, and Hispanic/Latino background distribution of the target population. Survey-specific logistic regression analyses were used to examine associations of risk factors with PAD. Initial models adjusted for age, sex, and Hispanic background. Multivariable models adjusted for all covariates shown. Of note, inclusion of a variable for the field center from which the participant enrolled did not change the results from those in the full model. Also, the field center variable is highly collinear with ethnic background. Therefore, and to ensure model stability, we did not include a “field center” variable in the models. Odds ratios with 95% CIs were computed using survey-specific logistic regression procedures to account for the 2-stage sampling design, stratification, and clustering. All analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC) and SUDAAN Release 10.0.0 (RTI, Research Triangle Park, NC).
RESULTS
Overall, the mean age of the cohort was 56 years and 55% were female (Table 1). Thirty-percent were Mexican American, 27% were Cuban American, 19% were Puerto Rican American, 9% were Dominican American and the remainder (15%) were either Central or South American or of Mixed/Other/Missing Hispanic/Latino ethnicity. Nearly all (91%) were born outside of the United States, 85% endorsed Spanish as their preferred language, 82% have lived in the United States for more than 10 years and 60% had graduated from high school or attained higher levels of education. The mean (SD) BMI and CRP were 29.9 (0.1) and 4.3 (0.1), respectively. Over half (54%) were never smokers, 44% had hypertension and 44% had dyslipidemia, while 61% had either diabetes (27%) or impaired glucose tolerance (34%). Finally, 6% had an ABI < 0.90 (“PAD”), 19% were between 0.90 and 0.99 (“borderline”), 72% were between 1.00 and 1.39 (“normal”) and 3% were 1.40 or higher (“high”). Nearly 9% reported a history of surgical procedure for PAD, while almost 27% reported having intermittent claudication in either leg.
TABLE 1.
COHORT CHARACTERISTICS*
| Continuous Variables | |
|---|---|
| Characteristic | Mean (SD) |
| Age | 56.5 (0.1) |
| Body Mass Index (kg/m2) | 29.9 (0.1) |
| Waist Circumference (cm) | 99.9 (0.2) |
| Pack-Years Smoking | 21.2 (0.7) |
| Triglycerides (mg/dL) | 152.3 (1.9) |
| C-reactive Protein (mg/L) | 4.3 (0.1) |
| Estimated Glomerular Filtration Rate (mL/min/1.73 m2) | 84.2 (0.4) |
| Categorical Variables | |
|---|---|
| Characteristic | Freq (Percent) |
| Female | 5,268 (54.6) |
| Hispanic/Latino Group | |
| Dominican | 892 (9.3) |
| Central American | 632 (6.6) |
| Cuban | 2,615 (27.1) |
| Mexican | 2,923 (30.3) |
| Puerto Rican | 1,804 (18.7) |
| South American | 528 (5.5) |
| Mixed/Other/Missing | 252 (2.6) |
| Cigarette Smoking | |
| Former | 2,489 (25.8) |
| Current | 1,986 (20.6) |
| Hypertension | 4,216 (43.7) |
| Impaired Fasting Glucose | 3,203 (33.2) |
| Diabetes | 2,595 (26.9) |
| Dyslipidemia | 4,274 (44.3) |
| High School Graduate or Higher | 5,808 (60.2) |
| Immigrant Generation | |
| First | 8,239 (85.4) |
| Second | 1,409 (14.6) |
| Language Preference | |
| Spanish | 8,646 (86.5) |
| English | 1,002 (13.5) |
| Years Living in the United States | |
| Less than 10 | 1,714 (17.9) |
| More than 10 | 7873 (82.1) |
| Self Reported Procedure for PAD | 849 (8.8) |
| Self Reported Intermittent Claudication | 2,595 (26.9) |
| ABI Groups | |
| Low/PAD (≤ 0.90) | 548 (5.7) |
| Borderline (0.90 – 0.99) | 1,859 (19.3) |
| Normal (1.00 – 1.39) | 6,991 (72.5) |
| High (≥ 1.40) | 250 (2.6) |
Weighted to the sampling probability
Table 2 shows the characteristics of the cohort by the different Hispanic/Latino groups. Central Americans had the highest triglyceride levels and proportion with dyslipidemia. Cuban Americans were the oldest, had the highest levels of systolic blood pressure and pack-years of cigarette smoking. This group also had the highest proportion of hypertension and current (but not former) smokers. Puerto Rican Americans had the highest levels of C-reactive protein and body mass index, the second high proportion of current smokers and lowest levels of eGFR. South Americans had the highest LDL and total cholesterol levels, as well as former smokers and those diagnosed with diabetes. Those classified as Other/Mixed had the highest waist and hip circumferences. Mexican Americans reported the highest rates of intermittent claudication. There were no significant differences in HDL cholesterol levels, the waist-to-hip ratio and self-reported surgical procedure for PAD across the groups.
TABLE 2.
CHARACTERISTICS BY HISPANIC/LATINO BACKGROUND GROUP*
| Continuous Variables | Dominican (858; 8.9%) | Central Amer (951; 9.9%) | Cuban (1,589; 16.5%) | Mexican (3,578; 37.1%) | Puerto-Rican (1,784; 18.5%) | South Amer (652; 6.8%) | Others (236, 2.4%) | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | ||
| Age (years) | 55.5 | 0.4 | 55.8 | 0.4 | 58.3 | 0.3 | 55.3 | 0.2 | 56.8 | 0.3 | 55.9 | 0.5 | 56 | 0.9 | < 0.01 |
| Body Mass Index (kg/m2) | 29.7 | 0.2 | 29.9 | 0.2 | 29.4 | 0.2 | 29.7 | 0.1 | 31 | 0.3 | 29.3 | 0.3 | 30.3 | 0.5 | < 0.01 |
| Waist Circumference (cm) | 97.9 | 0.5 | 98.4 | 0.6 | 100.1 | 0.4 | 100.1 | 0.3 | 101.3 | 0.5 | 97.1 | 0.6 | 102 | 1.9 | < 0.01 |
| Hip Circumference (cm) | 105.7 | 0.5 | 105.4 | 0.5 | 106.7 | 0.4 | 106.2 | 0.3 | 107.4 | 0.5 | 105 | 0.5 | 108.2 | 1.5 | < 0.01 |
| Waist/Hip Ratio | 0.9 | 0 | 0.9 | 0 | 0.9 | 0 | 0.9 | 0 | 0.9 | 0 | 0.9 | 0 | 0.9 | 0 | < 0.01 |
| SBP (mmHg) | 131.3 | 0.7 | 131 | 0.9 | 132.3 | 0.6 | 125.1 | 0.5 | 129.5 | 0.8 | 126.9 | 1 | 131.9 | 2.4 | < 0.01 |
| DBP (mmHg) | 77.9 | 0.5 | 75.8 | 0.5 | 77.1 | 0.4 | 72.7 | 0.3 | 76.3 | 0.3 | 73.9 | 0.5 | 77.4 | 1.1 | < 0.01 |
| LDL-cholesterol (mg/dL) | 127.3 | 1.9 | 131.6 | 2.1 | 134.1 | 1.2 | 128.6 | 1.2 | 122.4 | 1.3 | 134.9 | 1.8 | 126.6 | 5.1 | < 0.01 |
| HDL-cholesterol (mg/dL) | 50.6 | 0.5 | 49.7 | 0.6 | 49.4 | 0.4 | 49.3 | 0.4 | 49.6 | 0.7 | 50.5 | 0.8 | 50.3 | 1.4 | 0.31 |
| Total Cholesterol (mg/dL) | 203.3 | 2.2 | 212.9 | 2.2 | 213.9 | 1.4 | 209.1 | 1.3 | 200.5 | 1.5 | 215.2 | 2.2 | 205.4 | 5.3 | < 0.01 |
| Triglycerides (mg/dL) | 125.9 | 3.5 | 161.2 | 3.8 | 154.4 | 2.7 | 158.6 | 3.1 | 150.1 | 7.4 | 151.6 | 4.4 | 146.4 | 7.5 | < 0.01 |
| Fasting Glucose (mg/dL) | 107.2 | 1.4 | 112.5 | 1.8 | 108.6 | 1.1 | 111.8 | 1.5 | 111.9 | 1.3 | 104.3 | 1.4 | 120.1 | 4.5 | < 0.01 |
| eGFR (mL/min/1.73 m2) | 81.4 | 0.8 | 85.1 | 1 | 82.7 | 0.9 | 88.1 | 0.5 | 80.5 | 1 | 86.2 | 0.9 | 82 | 3.3 | < 0.01 |
| hsCRP (mg/L) | 4 | 0.4 | 4.7 | 0.8 | 4.7 | 0.2 | 3.8 | 0.2 | 4.9 | 0.2 | 3.8 | 0.3 | 4.4 | 0.5 | < 0.01 |
| Pack-years Smoking** | 19.4 | 1.6 | 16.5 | 1.7 | 29.8 | 1.1 | 12.3 | 0.7 | 22.7 | 0.8 | 17.2 | 2.2 | 17.9 | 2.2 | < 0.01 |
| Years Living in US | 21.55 | 0.54 | 19.98 | 0.52 | 17.05 | 0.80 | 27.06 | 0.60 | 42.67 | 0.64 | 19.01 | 0.77 | 30.05 | 1.99 | < 0.01 |
| Categorical Variables | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | 60.4 | 2 | 60.9 | 2.1 | 48.8 | 1.3 | 56.3 | 1.3 | 53.2 | 1.9 | 60.3 | 2.5 | 56.5 | 5.2 | < 0.01 |
| Former Smoker | 18.9 | 1.7 | 22.5 | 1.9 | 27 | 1.4 | 28 | 1.6 | 24 | 2 | 28.5 | 2.4 | 29.2 | 5 | < 0.01 |
| Current Smoker | 10.5 | 1.5 | 13.3 | 1.4 | 29.1 | 1.7 | 14.5 | 1 | 28.2 | 1.7 | 14 | 1.7 | 16.1 | 3.5 | < 0.01 |
| Hypertension | 45.6 | 2.5 | 41.3 | 2.1 | 52.9 | 1.5 | 34.4 | 1.8 | 47.9 | 2.2 | 33.6 | 2.5 | 47.6 | 5.7 | < 0.01 |
| Impaired Fasting Glucose | 33.4 | 2 | 33.3 | 2 | 36.9 | 1.4 | 33.5 | 1.2 | 32.4 | 2.1 | 37.8 | 2.3 | 30.3 | 4.2 | < 0.01 |
| Diabetes | 25.9 | 1.9 | 29.2 | 2.1 | 25.2 | 1.5 | 27.3 | 1.3 | 29.3 | 1.7 | 17.7 | 1.9 | 41.4 | 6 | < 0.01 |
| Dyslipidemia | 36.8 | 2.2 | 49.9 | 2.5 | 48.2 | 1.3 | 45.3 | 1.6 | 38.6 | 2.2 | 46.3 | 2.6 | 38.7 | 5.3 | < 0.01 |
| Education | 52.2 | 2.1 | 56.2 | 2.4 | 70.8 | 1.5 | 51.6 | 1.9 | 58.1 | 2.1 | 75.1 | 2.5 | 74 | 4.5 | < 0.01 |
| Unemployed (not retired) | 34.5 | 2.1 | 33.1 | 2.1 | 42.2 | 1.6 | 34.3 | 1.6 | 38.1 | 2.3 | 34.6 | 2.4 | 33.9 | 4.8 | < 0.01 |
| First Generation Immigrant | 99.3 | 0.3 | 99.1 | 0.5 | 98.5 | 0.4 | 84.4 | 1.1 | 73.3 | 1.6 | 98.9 | 0.4 | 79 | 4.1 | < 0.01 |
| US Born | 0.7 | 0.3 | 0.4 | 0.2 | 1.3 | 0.4 | 10.9 | 0.9 | 26.3 | 1.6 | 1.2 | 0.4 | 18.4 | 3.6 | < 0.01 |
| PAD Procedure | 6.7 | 2.8 | 1.2 | 1.2 | 7.9 | 3.3 | 11.1 | 4.2 | 12.0 | 3.3 | 2.1 | 2.1 | 6.1 | 4.4 | 0.18 |
| Intermittent Claudication | 38.1 | 2.3 | 23.9 | 1.9 | 19.7 | 1.1 | 25.0 | 1.5 | 36.8 | 2.2 | 22.5 | 2.1 | 28.9 | 7.4 | < 0.01 |
| ABI Groups | |||||||||||||||
| (<= 0.90) | 4.7 | 0.8 | 5.3 | 1 | 9.1 | 0.8 | 3.2 | 0.5 | 5.9 | 0.7 | 4.6 | 1 | 5 | 1.8 | < 0.01 |
| (0.91-0.99) | 21.5 | 1.9 | 19.7 | 1.8 | 25.4 | 1.6 | 14.4 | 1 | 18.1 | 1.8 | 17.2 | 1.9 | 16.6 | 3 | < 0.01 |
| (1.00-1.39) | 72.2 | 1.9 | 73 | 2.1 | 62.7 | 1.7 | 79.9 | 1 | 73 | 1.9 | 75.1 | 2.2 | 77.8 | 3.4 | < 0.01 |
| (>= 1.40) | 1.6 | 0.5 | 2 | 0.6 | 2.9 | 0.5 | 2.6 | 0.5 | 3 | 0.5 | 3.1 | 0.9 | 0.6 | 0.4 | < 0.01 |
Weighted to the Sampling Probability
Of Current/Former Smokers only
SBP = Systolic Blood Pressure, DBP = Diastolic Blood Pressure, eGFR = estimated glomerular filtration rate
The overall prevalence of an ABI less than 0.91 was 5.7%, while the prevalence for an ABI greater than 1.39 was 2.6%. Cuban Americans had the highest prevalence of PAD (9.1%), followed by Puerto Rican (5.9%), Central American (5.3%), Mixed/Other (5.0%), Dominican (4.7%), South American (4.6%) and Mexican Americans (3.2%). The highest prevalence of having an ABI ≥ 1.40 was found among South Americans (3.1%).
Compared with those with a normal ABI value, those with an ABI < 0.90 were older and had higher levels of systolic blood pressure, fasting glucose and pack-years of cigarette smoking, while having a lower eGFR (Table 3). This group was also more likely to be female, Cuban American, current smokers, unemployed, have either diabetes or hypertension, prefer Spanish as their language of choice and report either intermittent claudication or a procedure for PAD. Also compared to those with a normal ABI, those with an ABI ≥ 1.40 were also older and had higher levels of systolic blood pressure, total and LDL cholesterol, triglycerides and fasting glucose, but a somewhat lower eGFR. This group was more likely to be male, unemployed and have either diabetes or hypertension, as well as a procedure for PAD, but less likely to be current smokers.
TABLE 3.
CHARACTERISTICS BY ANKLE BRACHIAL INDEX GROUP*
| Continuous Variables | ABI ≤ 0.90 | 0.90 < ABI < 1.00 | 1.00 < ABI < 1.40 | ABI ≥ 1.4 | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| (486; 5.6%) | (1,723; 19.9%) | (7,224; 83.6%) | (215; 2.5%) | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Age (years) | 60.6 | 0.6 | 58.0 | 0.3 | 55.6 | 0.2 | 61.1 | 0.9 | 0.06 |
| Body Mass Index (kg/m2) | 29.7 | 0.4 | 29.9 | 0.2 | 29.8 | 0.1 | 31.4 | 0.6 | < 0.01 |
| Waist Circumference (cm) | 100.1 | 0.8 | 98.7 | 0.4 | 100.0 | 0.2 | 105.4 | 1.3 | < 0.01 |
| Hip Circumference (cm) | 106.2 | 0.7 | 106.8 | 0.5 | 106.3 | 0.2 | 108.7 | 1.4 | 0.32 |
| Waist/Hip Ratio | 0.9 | 0.0 | 0.9 | 0.0 | 0.9 | 0.0 | 1.0 | 0.0 | < 0.01 |
| Systolic Blood Pressure (mmHg) | 138.7 | 1.5 | 131.5 | 0.6 | 127.5 | 0.3 | 135.7 | 1.8 | < 0.01 |
| Diastolic Blood Pressure (mmHg) | 76.3 | 0.9 | 76.0 | 0.4 | 75.3 | 0.2 | 74.7 | 0.8 | 0.14 |
| LDL Cholesterol (mg/dL) | 133.1 | 2.5 | 133.0 | 1.4 | 128.5 | 0.8 | 117.3 | 3.8 | < 0.01 |
| HDL Cholesterol (mg/dL) | 49.5 | 0.8 | 51.4 | 0.5 | 49.2 | 0.2 | 49.0 | 1.1 | < 0.01 |
| Total Cholesterol (mg/dL) | 213.4 | 2.7 | 213.8 | 1.6 | 207.5 | 0.9 | 198.2 | 4.1 | < 0.01 |
| Triglycerides (mg/dL) | 159.6 | 5.2 | 149.6 | 3.7 | 152.4 | 2.4 | 155.6 | 8.8 | 0.50 |
| Fasting Glucose (mg/dL) | 116.5 | 3.1 | 108.2 | 1.2 | 109.6 | 0.7 | 132.7 | 7.8 | < 0.01 |
| eGFR (mL/min/1.73 m2) | 79.3 | 1.9 | 83.8 | 0.7 | 84.9 | 0.4 | 77.3 | 2.7 | < 0.01 |
| hsCRP (mg/L) | 6.5 | 0.6 | 4.8 | 0.2 | 4.0 | 0.1 | 5.3 | 0.8 | < 0.01 |
| Pack-years Cigarette Smoking** | 30.9 | 2.3 | 25.6 | 1.3 | 18.9 | 0.6 | 24.1 | 3.2 | < 0.01 |
| Years Residing in United States | 25.68 | 1.16 | 24.55 | 1.07 | 26.24 | 0.47 | 27.53 | 1.73 | 0.25 |
| Categorical Variables | % | SE | % | SE | % | SE | % | SE | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Female | 64.9 | 2.8 | 73.2 | 1.7 | 49.7 | 0.8 | 30.2 | 4.7 | < 0.01 |
| Hispanic Background | |||||||||
| - Dominican American | 7.7 | 1.4 | 10.3 | 1.2 | 9.2 | 0.8 | 5.8 | 1.7 | < 0.01 |
| - Central American | 6.1 | 1.2 | 6.7 | 0.8 | 6.6 | 0.4 | 5.1 | 1.5 | < 0.01 |
| - Cuban American | 43.3 | 3.9 | 35.7 | 3.1 | 23.5 | 1.8 | 30.7 | 5.1 | < 0.01 |
| - Mexican American | 16.8 | 2.8 | 22.6 | 1.9 | 33.4 | 1.8 | 29.8 | 4.9 | < 0.01 |
| - Puerto Rican American | 19.4 | 2.6 | 17.5 | 1.9 | 18.8 | 1.1 | 21.5 | 3.3 | < 0.01 |
| - South American | 4.5 | 1.0 | 4.9 | 0.6 | 5.7 | 0.4 | 6.6 | 1.9 | < 0.01 |
| - Mixed/Other/Missing | 2.3 | 0.8 | 2.3 | 0.4 | 2.8 | 0.4 | 0.6 | 0.4 | < 0.01 |
| Smoking Status | |||||||||
| - Former Smoker | 24.7 | 2.6 | 23.5 | 1.4 | 26.4 | 0.9 | 29.0 | 4.7 | < 0.01 |
| - Current Smoker | 36.2 | 3.1 | 24.3 | 1.6 | 18.8 | 0.7 | 7.9 | 1.9 | < 0.01 |
| Hypertension | 65.6 | 2.9 | 48.9 | 2.0 | 40.1 | 1.0 | 58.2 | 4.8 | < 0.01 |
| Impaired Fasting Glucose | 28.5 | 2.6 | 36.6 | 1.9 | 34.2 | 0.8 | 33.0 | 5.3 | < 0.01 |
| Diabetes | 42.8 | 3.0 | 25.7 | 1.5 | 25.4 | 0.8 | 45.5 | 5.1 | < 0.01 |
| Dyslipidemia | 47.0 | 3.0 | 42.4 | 1.8 | 44.7 | 1.0 | 39.6 | 4.6 | 0.42 |
| HS Education or Higher | 52.8 | 2.9 | 59.4 | 2.1 | 61.0 | 1.0 | 59.2 | 5.0 | 0.04 |
| Unemployed (non-retired) | 45.9 | 3.7 | 40.0 | 2.0 | 35.8 | 1.1 | 33.2 | 4.1 | < 0.01 |
| First Generation Immigrant | 91.1 | 1.6 | 91.9 | 1.0 | 88.3 | 0.7 | 89.2 | 2.6 | 0.02 |
| Born Outside the United States | 7.3 | 1.4 | 7.2 | 0.9 | 9.8 | 0.7 | 10.3 | 2.6 | 0.07 |
| Spanish Language Preferred | 90.0 | 1.6 | 86.8 | 1.9 | 84.7 | 0.9 | 83.2 | 3.2 | 0.03 |
| PAD Procedure | 16.9 | 5.6 | 15.9 | 4.5 | 4.9 | 1.5 | 11.8 | 5.4 | 0.02 |
| Intermittent Claudication | 41.6 | 3.3 | 29.3 | 2.0 | 25.1 | 1.1 | 27.1 | 3.1 | < 0.01 |
Weighted to the Sampling Probability
Of Current/Former Smokers only
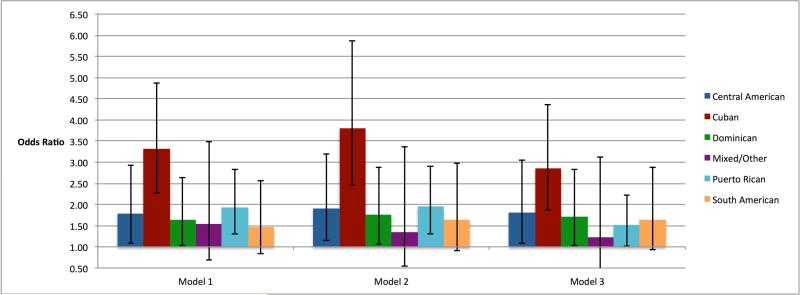
Figure 1 shows the odds for PAD by Hispanic/Latino group. Compared to Mexican Americans, and in a multivariable logistic regression model adjusted for age and gender (model 1), Cuban Americans had over a three-fold higher odds for having PAD (OR = 3.3, 95% CI: 2.3 – 4.9) while all of the other Hispanic/Latino groups had odds that ranged from 1.5 (0.8 – 2.6) to 1.9 (1.3 – 2.8). With additional adjustment for waist, height, immigrant generation, educational attainment, hypertension, diabetes, dyslipidemia and cigarette smoking (model 2), the odds for Cuban Americans decreased to 2.9 (1.9 – 4.4), while the range of odds ratios for the other groups changed from 1.2 (0.5 – 3.1) to 1.8 (1.1 – 3.0). The results were not materially changed when we additionally adjusted for statin medication use and cigar use (model 3) or when we excluded those with a history of a procedure for PAD and adjusted for symptoms of intermittent claudication.
FIGURE 1. ODDS OF PERIPHERAL ARTERIAL DISEASE (ABI ≤ 0.90) BY HISPANIC/LATINO BACKGROUND GROUP*.
*Weighted to the Sampling Probability
Reference Group = Mexican Americans; Vertical Bars = 95% Confidence Intervals
Model 1: Adjusted for age, gender
Model 2: Adjusted for model 1 variables + height + waist circumference + immigrant generation, educational attainment
Model 3: Adjusted for model 2 variables + hypertension + diabetes + dyslipidemia + smoking
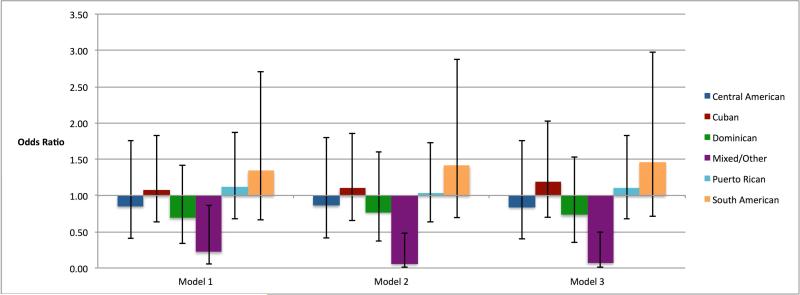
The odds for having an ABI ≥ 1.4 by Hispanic/Latino group are shown in Figure 2. Compared to Mexican Americans, and in a multivariable logistic regression model adjusted for age and gender (model 1), those of Other/Mixed ethnicity had a significantly lower odds for a high ABI (0.22, 0.1 – 0.9), while the odds for all of the other Hispanic/Latino groups were not found to be significantly different. With additional adjustment for waist, height, immigrant generation, educational attainment, hypertension, diabetes, dyslipidemia and cigarette smoking (model 2), the odds for the Other/Mixed group decreased to 0.1 (0.01 – 0.5), while the range of odds ratios for the other groups were not remarkably changed. Of note, in the fully adjusted analyses (model 3), men had over a 3-fold higher odds for a high ABI (3.6, 2.0 – 6.5). The results were not materially different when we excluded those with a history of a procedure for PAD and adjusted for symptoms of intermittent claudication.
FIGURE 2. – ODDS FOR “STIFF ARTERIES” (ABI ≥ 1.40) BY HISPANIC/LATINO BACKGROUND GROUP*.
*Weighted to the Sampling Probability
Reference Group = Mexican Americans; Vertical Bars = 95% Confidence Intervals
Model 1: Adjusted for age, gender
Model 2: Adjusted for model 1 variables + height + waist circumference + immigrant generation, educational attainment
Model 3: Adjusted for model 2 variables + hypertension + diabetes + dyslipidemia + smoking
In sensitivity analyses, and to the final multivariable model, we additionally adjusted for cigar smoking and pack-years of cigarette smoking. We also ran models that added systolic blood pressure, diastolic blood pressure and fasting plasma glucose levels. In all cases, the results were not materially different from those provided above.
DISCUSSION
In this large, population-based cohort study of multiple different Hispanic/Latino groups, we found that, compared to Mexican Americans, Cuban Americans had over a three-fold higher odds for the presence of PAD independent of sociodemographic and traditional cardiovascular disease risk factors. We also found that, after the same adjustment, the other Hispanic/Latino groups enrolled in this study had higher odds of PAD, with those for Central, Dominican and Puerto Rican American being significantly higher and the odds for South Americans being higher, but not significantly, likely due to the smaller number of individuals in this group. Conversely, our analyses did not demonstrate differential odds for the presence of an ABI ≥ 1.40 by Hispanic/Latino group but we did find a strong association between male sex and having a high ABI. In sum, the findings from this study indicate that Hispanic/Latino groups are different with respect to the presence of PAD, but not a high ABI, which may have implications for clinical practice, public health planning and the Hispanic Paradox paradigm. More specifically, clinicians may consider having a higher index of suspicion for PAD among Hispanic/Latino Americans who are not of Mexican background. Additonally, prior studies, based largely on Mexican Americans, have suggested that this group has a lower risk of incident CVD, despite higher levels of CVD risk factors (i.e. Hispanic Paradox). The results of our study suggest that conceptualization of the Hispanic Paradox may need to be modified to account for differences in the prevalence of extant CVD (i.e. PAD) among different Hispanic/Latino ethnic groups.
Using data from the Multi-Ethnic Study of Atherosclerosis, we have previously examined the differences in levels of both traditional and novel CVD risk factors, as well as subclinical measures of atherosclerosis, among different Hispanic/Latino ethnic groups. 7 The results of this study indicated that there were significant differences with respect to the prevalence of current/former smoking, hypertension, dyslipidemia and both the metabolic syndrome and type 2 diabetes mellitus, as well as PAD. Importantly, the number of Cuban Americans in this study was too small for meaningful analyses (n = 56). As such, and based on the number of participants in the other Hispanic/Latino ethnic groups enrolled in the HCHS-SOL, the results of the current study provide much more robust and relevant data on PAD and the presence of an ABI > 1.40 [“stiff arteries”] for the contemporary US population.
An important finding from the current analysis is that the associations between the different Hispanic/Latino ethnicities and PAD were independent of immigrant generation, educational attainment and traditional CVD risks factors. As such, the results suggest there are other factors that may predispose non-Mexican American Hispanic/Latino Americans to more readily develop PAD than Mexican Americans. One such potential explanation for this difference is genetic predisposition. In this regard, we have conducted a study examining the association between genetic admixture and PAD among Hispanic/Latino Americans enrolled in the MESA. The results of this study indicated that higher levels of Native American ancestry were associated with a lower odds for PAD. 12 Paradoxically, Native Americans have a higher prevalence of PAD than Hispanic/Latino Americans. 1 Also, the composition of the Hispanic/Latino population in the MESA is highly skewed toward Mexican Americans. Given this, more research is needed to more fully address the reasons for the differential risk of PAD among non-Mexican American Hispanic/Latino groups residing in the United States.
Previous studies have estimated the overall prevalence of PAD among adults over the age of 40 years to range from 4.5 to 12%, resulting in a burden (based on the 2000 census) of approximately 8 million individuals (using the mean of the range just provided) with 5 million being non-Hispanic White. 1,13,14 Also, we have previously shown that Mexican Americans have half the odds for having PAD, compared to non-Hispanic Whites. 15 This, combined with the results of the current study suggest that, compared to non-Hispanic Whites, Cuban Americans will have a 50% higher odds for PAD, while the odds for the “Other Hispanic/Latino” group will be 25% lower. As such, more current estimates of burden of PAD for these different groups could be computed using data from the 2010 census.
Strengths of the current study are a very large and well-characterized sample that had PAD assessed by a standardized protocol using the ankle brachial index. Also, the HCHS-SOL enrolled individuals from several different Hispanic/Latino ethnic groups using a probability-based sampling strategy aimed at being representative of these groups living in the United States. Conversely, there are limitations to consider. There was no contemporary non-Hispanic White population recruited concomitant to that for the HCHS-SOL. As such, comparisons with this group rely on past samples from other cohort studies. Also, the HCHS-SOL did not assess for several novel markers of atherosclerosis that have been shown to be associated with PAD (e.g. fibrinogen and interleukin-6). 15 Finally, there is the possibility for distortion of the results that may remains after controlling for confounding in the design and/or analysis of a study (residual confounding). However, we noted that the results were largely resistant to change when including different covariates suggesting residual confounding may be minimal.
In conclusion, compared to Mexican Americans, Cuban Americans have a three-fold higher odds for the presence of peripheral arterial disease independent of educational attainment, immigrant generation and traditional CVD risk factors. Similarly, other selected Hispanic/Latino ethnic groups residing in the United States have significantly higher odds for PAD, compared to Mexican Americans. These findings are similar to those published previously that showed non-Mexican American groups (i.e. Cuban and Puerto Rican Americans) having higher rates of prevalent coronary artery disease.6 As these associations were significant after adjustment for risk factors, other potential variables, such as genetic or environmental factors, should be considered to explain the differences.
ACKNOWLEDGEMENTS
The authors thank the staff and participants of HCHS/SOL for their important contributions. Investigators website - http://www.cscc.unc.edu/hchs/. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, NIH Institution-Office of Dietary Supplements.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Allison MA, Ho E, Denenberg JO, Langer RD, Newman AB, Fabsitz RR, et al. Ethnic-specific prevalence of peripheral arterial disease in the United States. American Journal of Preventive Medicine. 2007 Apr;32(4):328–33. doi: 10.1016/j.amepre.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 2.Criqui MH, Denenberg JO. The generalized nature of atherosclerosis: how peripheral arterial disease may predict adverse events from coronary artery disease. Vasc Med. 1998;3(3):241–5. doi: 10.1177/1358836X9800300311. [DOI] [PubMed] [Google Scholar]
- 3.Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992 Feb 6;326(6):381–6. doi: 10.1056/NEJM199202063260605. [DOI] [PubMed] [Google Scholar]
- 4.Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, et al. Measurement and Interpretation of the Ankle-Brachial Index: A Scientific Statement From the American Heart Association. Circulation. 2012 Dec 11;126(24):2890–909. doi: 10.1161/CIR.0b013e318276fbcb. [DOI] [PubMed] [Google Scholar]
- 5.Allison MA, Cushman M, Solomon C, Aboyans V, McDermott MM, Goff DC, et al. Ethnicity and risk factors for change in the ankle-brachial index: the Multi-Ethnic Study of Atherosclerosis. Journal of Vascular Surgery. 2009 Nov;50(5):1049–56. doi: 10.1016/j.jvs.2009.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daviglus M, Talavera GA, Avilés-Santa ML, Allison MA, Cai J, Criqui M, et al. Prevalence of Major Cardiovascular Risk Factors and Cardiovascular Diseases Among Hispanic/Latino Individuals of Diverse Backgrounds in the United States. JAMA: The Journal of the American Medical Association. 2012 Oct 24;308(17):1775–84. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH. Prevalence of and Risk Factors for Subclinical Cardiovascular Disease in Selected US Hispanic Ethnic Groups: The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008 Feb 25;167(8):962–9. doi: 10.1093/aje/kwm402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010 Aug;20(8):629–41. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lavange LM, Kalsbeek WD, Sorlie PD, Avilés-Santa LM, Kaplan RC, Barnhart J, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010 Aug;20(8):642–9. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972 Jun;18(6):499–502. [PubMed] [Google Scholar]
- 11.Ankle Brachial Index Collaboration. Fowkes FGR, Murray GD, Butcher I, Heald CL, Lee RJ, et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA: The Journal of the American Medical Association. 2008 Jul 9;300(2):197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allison MA, Peralta CA, Wassel CL, Aboyans V, Arnett DK, Cushman M, et al. Genetic ancestry and lower extremity peripheral artery disease in the Multi-Ethnic Study of Atherosclerosis. Vasc Med. 2010 Oct;15(5):351–9. doi: 10.1177/1358863X10375586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Criqui MH, Fronek A, Barrett-Connor E, Klauber MR, Gabriel S, Goodman D. The prevalence of peripheral arterial disease in a defined population. Circulation. 1985 Mar;71(3):510–5. doi: 10.1161/01.cir.71.3.510. [DOI] [PubMed] [Google Scholar]
- 14.Selvin E, Erlinger TP. Lippincott Williams & Wilkins, editor. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004 Aug 10;110(6):738–43. doi: 10.1161/01.CIR.0000137913.26087.F0. 2004. [DOI] [PubMed] [Google Scholar]
- 15.Allison MA, Criqui MH, McClelland RL, Scott JM, McDermott MM, Liu K, et al. The effect of novel cardiovascular risk factors on the ethnic-specific odds for peripheral arterial disease in the Multi-Ethnic Study of Atherosclerosis (MESA). J Am Coll Cardiol. 2006 Sep 19;48(6):1190–7. doi: 10.1016/j.jacc.2006.05.049. [DOI] [PubMed] [Google Scholar]