Abstract
Objectives
Mennonites reside in clusters, do not use modern sewage systems and consume water from non-municipal sources. The purpose of this study is to assess risk of Escherichia coli exposure via consumption of non-municipal waters in Mennonite versus non-Mennonite rural households.
Methods
Results were reviewed for non-municipal water samples collected by the local health department from Mennonite and non-Mennonite lifestyle households from 1998 through 2012. Water contamination was examined with the help of two study variables: water quality (potable, polluted) and gastrointestinal (GI) health risk (none, low, high). These variables were analyzed for association with lifestyle (Mennonite, non-Mennonite) and season (fall, winter, spring, summer) of sample collection. Data were split into two periods to adjust for the ceiling effect of laboratory instrument.
Results
From the entire cohort, 82 % samples were polluted and 46 % samples contained E. coli, which is consistent with high GI health risk. In recent years (2009 through 2012), the presence of total coliforms was higher in non-Mennonites (39 %, P = 0.018) and presence of E. coli was higher in Mennonites (P = 0.012). Most polluted samples were collected during summer (45 %, P = 0.019) and had high GI health risk (51 %, P = 0.008) as compared to other seasons.
Conclusions
Majority of non-municipal waters in this region are polluted, consuming those poses a high GI health risk and contamination is prevalent in all households consuming these waters. An association of E. coli exposure with the Mennonite lifestyle was limited to recent years. Seasons with high heat index and increased surface runoffs were the riskiest to consume non-municipal waters.
Keywords: Water quality, Mennonites, Non-municipal waters, Gastrointestinal health risk
Introduction
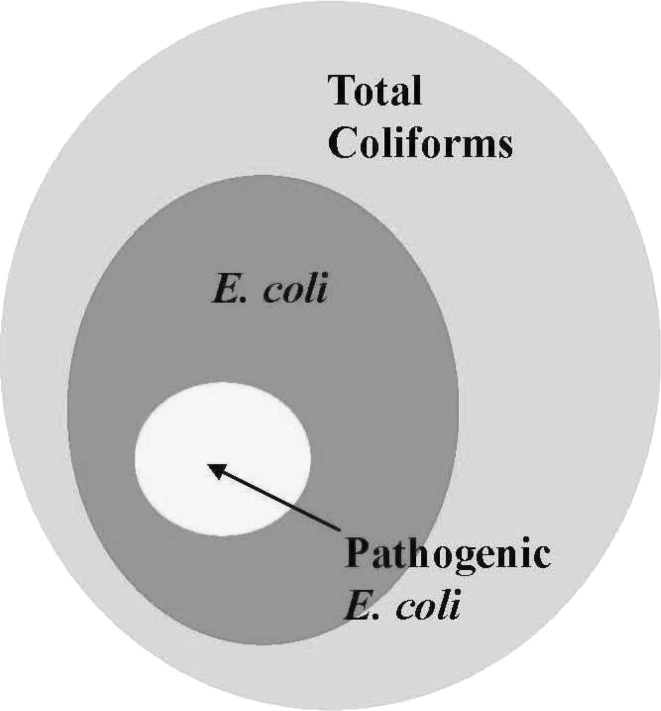
As developed nations shift the focus of their healthcare efforts towards prioritizing non-communicable over communicable diseases, there are significant sections of their society which stand exposed to high risk of communicable diseases. Many acute and chronic gastrointestinal (GI) diseases, due to consumption of contaminated water, can be attributed to living conditions [1]. There are multiple microorganisms found in drinking water that can cause GI infections [2]. The World Health Organization (WHO) and the United States Centers for Disease Control and Prevention (CDC) evaluate the quality of drinking water by testing for the presence of total coliforms, which can contain fecal bacteria such as Escherichia coli (Fig. 1) [3–5]. Escherichia coli, located in the normal intestinal flora of warm blooded animals, is the most frequent culprit of gastro-enteric bloody diarrhea and resultant fatal complications [6–8]. Certain E. coli strains have been the cause of large-scale acute GI infection outbreaks in developed countries, where approximately 20 % cases developed fatal complications; increasing risk of morbidity and mortality in susceptible populations [8–10]. Presence of E. coli in water or food is the best indicator of high risk of severe GI illness and warrants immediate public health intervention [5, 11].
Fig. 1.
The spectrum of coliforms [4]
The vast majority of Americans consume municipally provided waters which, as per the United States Safe Drinking Water Act (1974), are strictly regulated by the United States Environmental Protection Agency (US EPA) guidelines and must maintain Maximum Contaminant Level Goal (MCLG) of zero coliform bacteria per 100 ml [12, 13]. Non-municipal water sources are not subject to such regulation, especially sources located on private properties where the federal, state or local laws have no jurisdiction [14, 15]. Therefore, the non-municipal water may contain microorganisms known to cause GI illness.
The Old Order Mennonite (Mennonite) families do not utilize electricity or modern plumbing facilities in their houses and also preclude the use of municipally provided waters or the independent operation of systems to purify water, which are often utilized in the non-Mennonite population [16, 17]. Further accentuating the risk of consumption of non-municipal water which can cause GI diseases in the Mennonite population, as opposed to non-Mennonite populations consuming non-municipal water, is the fact that Mennonite traditional practices include living in clusters, with their non-municipal water sources surrounded by animals and farms. In absence of modern sewage or any certifiable sanitary facilities, the ill-disposed feces, garbage and animal dander from these households have a high probability of seepage into nearby water sources [18].
On the other hand, the non-Mennonite rural population living in remote rural locations of the United States, that uses non-municipal waters, also acquires water from nearby natural sources. These households have been often reported to use rural sewage disposal systems and independent water purification systems, reducing the chances of domestic contamination of their non-municipal water sources.
Specific aims of this study
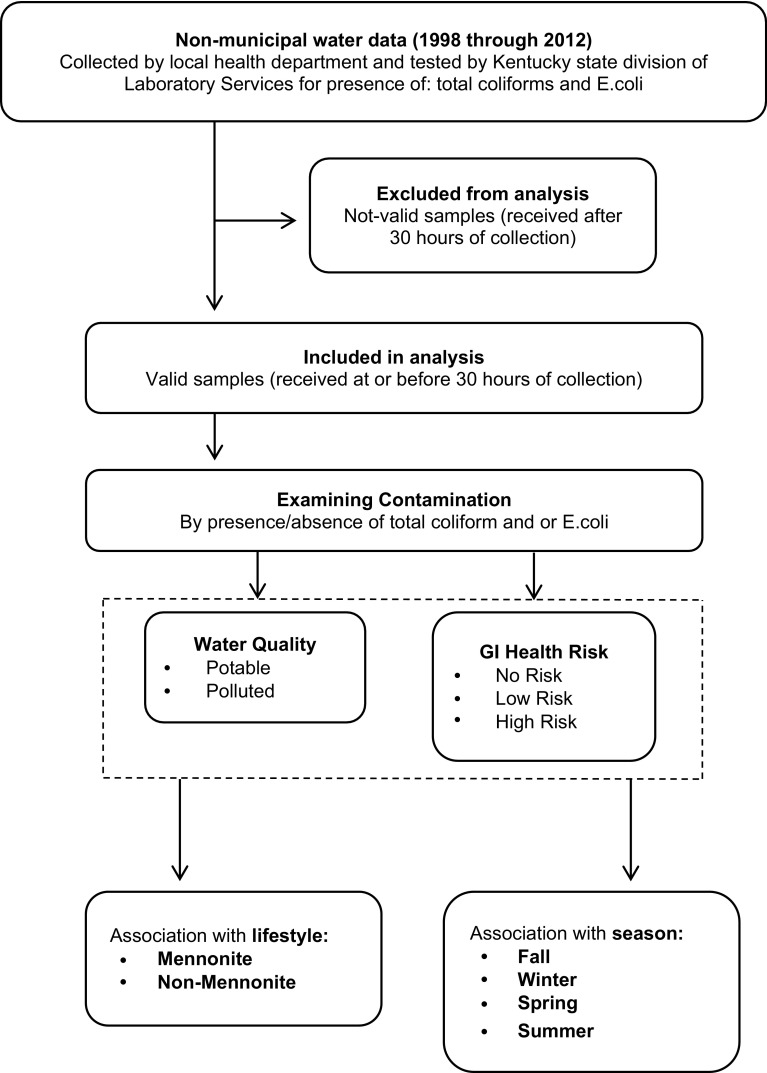
In light of these differences in lifestyle and health habits between Mennonite and non-Mennonite households, it is our hypothesis that the Mennonite community is exposed to higher levels of contaminated water as compared to non-Mennonite households consuming non-municipal water. The first aim of this study is to examine the association of lifestyle variation among Mennonites as compared to non-Mennonites on contamination of non-municipal water acquired by them from nearby sources. The second aim is to examine the association of seasonal variation on non-municipal water contamination and resulting risk of gastrointestinal diseases via the presence of E. coli in these waters. The scheme of this study is presented in Fig. 2.
Fig. 2.
Scheme of research
Any epidemiological evidence about the Mennonite community uncovered in this study will play an important role in shaping public health for a sizeable population worldwide, who utilize non-municipal waters for daily activities in absence of universally accepted safety protocols [19, 20]. To the best of our knowledge, this is the first study to probe drinking water contamination in the Mennonite community.
Methods
This is a cross-sectional study of quality of non-municipal water samples collected by the local health department from August 1998 through October 2012. This study was approved by the Institutional Review Board and written consents were not required.
Water sample source
All samples were collected from non-municipal water sources, defined as: springs, wells, ponds and other sources not governed by the US EPA drinking water quality requirements.
Study population
All samples were acquired from households in Allen County, Kentucky, USA, which is home to a sizeable population of the Mennonite community and other non-Mennonite rural households [17, 19].
Data collection and validity
All samples were collected as per an US EPA directed protocol from non-municipal water sources by the Allen County Health Department, Scottsville, Kentucky and analyzed by the Division of Laboratory Services, Department of Public Health, Frankfort, Kentucky [16, 21]. Samples were collected in a standard 100 ml cup. Water collected from a running water line was initially allowed to run for approximately 2 min before sample collection. In the case of a natural spring, collection cups were held face down and water from the deepest possible layer was collected.
Difference between collection time and laboratory receiving time was calculated as holding time. As per the US EPA guidelines for drinking water compliance, samples received by the laboratory within or at 30 h of collection were deemed valid and those received later were excluded from our study [22].
Independent variables
Lifestyle To address the effect of lifestyle differences, all samples were identified as collected from either a Mennonite or a non-Mennonite household.
Seasons To address the effect of seasonal variation, date of sample collection was used to identify the season: fall was September through November; winter was December through February; spring was March and April and summer was May through August. Approximately 2–4 samples were collected each month.
Laboratory analysis
Samples were analyzed for the presence of total coliforms and E. coli as colony-forming units (CFUs) per 100 ml. Colilert reagent was used to detect the presence of total coliform and E. coli (“Appendix” Fig. 3) [23]. Quanti-Tray and Quanti-Tray/2000 filled with a mixture of Colilert reagent and water sample were used to calculate the presence of Most Probable Number (MPN) of coliforms (“Appendix” Fig. 4) [24].
Fig. 3.
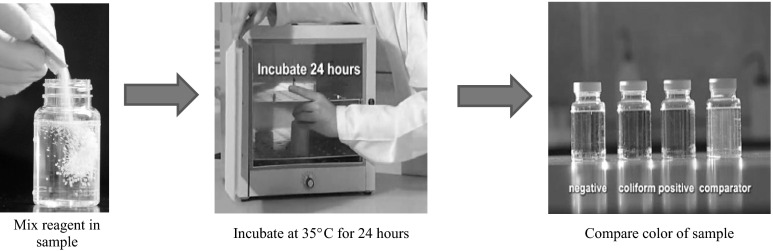
Colilert reagent for detection of total coliforms and E. coli [21, 23]. The mixture of Colilert reagent and water sample turns yellow if any coliform bacteria are present and yellow plus fluorescent if specifically E. coli is present (color figure online)
Fig. 4.
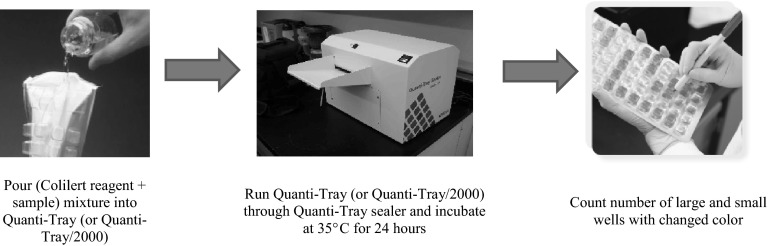
Quanti-Trays for calculating most probable numbers of total coliforms and E. coli [21, 24]. A table or software is used to calculate the Most Probable Number of total coliforms and E. coli in Quanti-Trays (or Quanti-Tray/2000) with changed colors (color figure online)
Water contamination scoring
Microbial aspects quantified by the WHO guidelines for drinking water (2011) and the US EPA revised Total Coliform Rule (2013) were used to define two categorical outcomes for measurement of water contamination in our study (Table 1) [5, 13]: “water quality” and “gastrointestinal (GI) health risk”.
Table 1.
Outcomes to measure water contamination
| Outcome measures | Score | Total coliforms (CFUs/100 ml) | E. coli (CFUs/100 ml) |
|---|---|---|---|
| Water quality [5, 13] | Potable | Zero | Zero |
| Polluted | ≥1 | Zero or ≥1 | |
| GI health risk [5, 13] | No risk | Zero | Zero |
| Low risk | ≥1 | Zero | |
| High rsk | ≥1 | ≥1 |
CFUs colony forming units, GI gastrointestinal
Water quality Sample quality was potable when both, total coliform and E. coli, were absent. Sample quality was polluted when at least one total coliform was detected.
GI health risk Sample posed no risk when total coliform and E. coli were both absent. Sample posed low risk when total coliforms were present, but E. coli was absent. Sample posed high risk when at least one E. coli was present.
Limitation of instrument precision
The Quanti-Tray instrument, which can calculate maximum 200.5 CFUs/100 ml, was used from August 1998 through December 2008 [21, 24]. The Quanti-Tray/2000 instrument, which can calculate maximum 2419.6 CFUs/100 ml, was used from January 2009 through October 2012 [21, 24]. This was a form of truncation arising due to limitation of instrument precision. To account for these changes in upper limit of instrument precision, data were split into two time periods [25]. This limitation did not affect the specific aims of our study.
Period one Period one was from August 1998 to January 2009, when Quanti-Tray was used. Measurements exceeding 200.5 CFU/100 ml in this period were reported at their truncated value of 200.5 CFU/100 ml. 180 out of 240 valid samples were included in this period.
Period two Period two was from January 2009 through October 2012, when Quanti-Tray/2000 was used. Measurements exceeding 2419.6 CFU/100 ml in this period were reported at their truncated value of 2419.6 CFU/100 ml. 60 out of 240 valid samples were included in this period.
Statistical analysis
Data were entered using Microsoft Access and analyzed with SAS [26, 27]. Analyses for total coliform and E. coli counts along with proportion of truncated and non-truncated values were conducted separately for each period. In addition, associations of water quality and GI health risk with lifestyle variation were conducted for each period.
For categorical characteristics, frequency of the characteristics between groups was conducted and tested using Pearson’s Chi-squared test [28]. Fisher’s exact test was used when any cell counts were less than 5 [28]. For continuous characteristics, the Wilcoxon rank sum test was used [29]. Splitting into separate periods resulted in insufficient amount of data; hence, regression models were not used to estimate relationships [30]. Statistical significance was defined as P < 0.05.
Results
A total of 303 samples were collected from Mennonite (24 %) and non-Mennonite (76 %) households, out of which 63 were excluded due to holding time of greater than 30 h and 240 were retained as valid samples. General associations of lifestyle with seasons and contamination, without splitting data into separate time periods, are presented in “Appendix” Table 4. There were no significant associations between lifestyle and water contamination scores (water quality, GI health risk) when data were not split into separate time periods.
Table 4.
General association of lifestyle with season and contamination without splitting into separate time periods
| Characteristics | Total | Lifestyle | ||
|---|---|---|---|---|
| Mennonite | Non-Mennonite | P Value | ||
| Total water samples (%) | 303 | 74 (24.4) | 229 (75.6) | 0.3 |
| Not-valid (%) | 63 (20.8) | 12 (16.2) | 51 (22.3) | |
| Valid (%) | 240 (79.2) | 62 (25.8) | 178 (74.2) | |
| Mean holding time in hours (95 % CI) | 30 (23.1–36.9) | 32.6 (13.9–51.3) | 29.2 (22.2–36.2) | 0.7 |
| Seasons | 0.007 | |||
| Fall (%) | 82 (27.1) | 13 (17.6) | 69 (30.1) | 0.034 |
| Winter (%) | 52 (17.2) | 18 (24.3) | 34 (14.8) | 0.060 |
| Spring (%) | 47 (15.5) | 18 (24.3) | 29 (12.7) | 0.016 |
| Summer (%) | 122 (40.3) | 25 (33.8) | 97 (42.4) | 0.2 |
| Contamination scores in valid samples (N = 240) | ||||
| Water Quality | 0.4 | |||
| Potable (%) | 40 (16.7) | 8 (12.9) | 32 (18) | |
| Polluted (%) | 200 (83.3) | 54 (87.1) | 146 (82) | |
| GI health risk | 0.7 | |||
| No risk (%) | 40 (16.7) | 8 (12.9) | 32 (18) | |
| Low risk (%) | 87 (36.3) | 23 (37.1) | 64 (36) | |
| High risk (%) | 113 (47.1) | 31 (50) | 82 (46.1) | |
| Contaminant levels | ||||
| Mean total coliform CFUs/100 ml (95 % CI) | 353.3 (267.2–439.4) | 285.5 (200.7–370.4) | 547.8 (325.8–769.9) | 0.3 |
| Mean E. coli CFUs/100 ml (95 % CI) | 69.3 (35.1–103.4) | 91.8 (9.3–174.3) | 61.4 (25.4–97.5) | 0.8 |
CI confidence interval, GI gastrointestinal, Fall september–november, Winter december–february, Spring march–april, Summer may–august
Associations of coliform contamination during two separate time periods are presented in Table 2. During period one (1998 through 2008), the mean E. coli count was borderline higher in non-Mennonites (35 CFUs) as compared to Mennonites (15 CFUs, P = 0.052). During period two (2009 through 2012), majority of low-risk samples were collected from non-Mennonites (39 %) as compared to Mennonites (10 %, P = 0.018). However, during period two, Mennonite samples (86 %) had high GI health risk (one or more E. coli CFUs) as compared to non-Mennonites (46 %, P = 0.012). This period also showed high mean count of total coliforms from Mennonite samples (1426 CFUs) as compared to non-Mennonite samples (853 CFUs, P = 0.02). Similarly, high count of E. coli was found in Mennonite samples (241 CFUs) as compared to non-Mennonites (154 CFUs, P = 0.014).
Table 2.
Association of coliform contamination with lifestyle in two time periods
| Characteristics | Total valid samples (N=240) | Lifestyle | ||
|---|---|---|---|---|
| Mennonite (N = 62) | Non-Mennonite (N = 178) | P value | ||
| Period #1 (N) | 180 | 41 | 139 | |
| Water quality | 0.8 | |||
| Potable (%) | 33 (18.3) | 7 (17.1) | 26 (18.7) | |
| Polluted (%) | 147 (81.7) | 34 (82.9) | 113 (81.3) | |
| GI health risk | 0.2 | |||
| No risk (%) | 33 (18.3) | 7 (17.1) | 26 (18.7) | |
| Low risk (%) | 70 (38.9) | 21 (51.2) | 49 (35.3) | |
| High risk (%) | 77 (42.8) | 13 (31.7) | 64 (46.0) | |
| Mean total coliform CFUs/100 ml (95 % CI) | 119.9 (108.1-131.6) | 98 (75.2–120.9) | 126.3 (110.9–141.7) | 0.1 |
| Mean E. coli CFUs/100 ml (95 % CI) | 30.8 (22.7–38.9) | 15.2 (3.4–27.0) | 35.4 (25.4–45.3) | 0.052 |
| Period #2 (N) | 60 | 21 | 39 | |
| Water quality | 0.2 | |||
| Potable (%) | 7 (11.7) | 1 (4.8) | 6 (15.4) | |
| Polluted (%) | 53 (88.3) | 20 (95.2) | 33 (84.6) | |
| GI health risk | 0.012 | |||
| No risk (%) | 7 (11.7) | 1 (4.8) | 6 (15.4) | 0.2 |
| Low risk (%) | 17 (28.3) | 2 (9.5) | 15 (38.5) | 0.018 |
| High risk (%) | 36 (60.0) | 18 (85.7) | 18 (46.2) | 0.012 |
| Mean total coliform CFUs/100 ml (95 % CI) | 1053.6 (915.8–1191.4) | 1426 (1154.9–1697.0) | 853.1 (698.9–1007.2) | 0.020 |
| Mean E. coli CFUs/100 ml (95 % CI) | 184.8 (119.7–249.9) | 241.4(106.1–376.6) | 154.3 (80.5–228.2) | 0.014 |
Period #1—1998 through 2008
Period #2—2009 through 2012
CI confidence interval, GI gastrointestinal
Associations of seasons with water quality and GI health risk, without splitting data into separate periods, are presented in Table 3. Analyzing the water quality during different seasons, we found that fall season had the highest number of potable samples (n = 16), and the proportion of potable samples collected in the fall season (40 %) was also significantly higher than the proportion of polluted samples collected in that season (22 %, P = 0.016). Summer season had the highest number of polluted samples (n = 90), and the proportion of polluted samples collected in that season (45 %) was also significantly higher than the proportion of potable samples collected in that season (25 %, P = 0.019). Analyzing the GI health risk during different seasons, we found that safest samples (no risk, zero total coliform CFUs) were mostly collected in fall season (40 %), as compared to winter (18 %), spring (18 %) or summer (25 %, P = 0.0016). In contrast, worst samples (high GI risk—one or more E. coli CFUs) were mostly collected in summer (51 %), as compared to fall (18 %), winter (16 %) and spring (15 %, P = 0.008).
Table 3.
Association of seasons with water quality and GI health risk
| Seasons | Total valid samples (N = 240) | Water quality | GI health risk | |||||
|---|---|---|---|---|---|---|---|---|
| Potable (N = 40) | Polluted (N = 200) | P value | No risk (N = 40) | Low risk (N = 87) | High risk (N = 113) | P Value | ||
| Seasons | 0.055* | 0.053* | ||||||
| Fall (%) | 60 (25) | 16 (40) | 44 (22) | 0.016** | 16 (40) | 24 (27.6) | 20 (17.7) | 0.016*** |
| Winter (%) | 42 (17.5) | 7 (17.5) | 35 (17.5) | 1.0** | 7 (17.5) | 17 (19.5) | 18 (15.9) | 0.8*** |
| Spring (%) | 38 (15.8) | 7 (17.5) | 31 (15.5) | 0.8** | 7 (17.5) | 14 (16.1) | 17 (15) | 0.9*** |
| Summer (%) | 100 (41.7) | 10 (25) | 90 (45) | 0.019** | 10 (25) | 32 (36.8) | 58 (51.3) | 0.008*** |
Fall september–november, Winter december–february, Spring march–april, Summer may–august, GI gastrointestinal
*P value for overall effect of season in model
**P value comparing percentages of potable vs. polluted samples collected in a specific season against all other seasons
***P value comparing percentages of no risk, low risk and high risk samples collected in a specific season against all other seasons
Discussion
Upon examining the water quality and GI health risk from consumption of non-municipal waters among Mennonite and non-Mennonite households of Allen County, Kentucky, we found that a majority of water from these sources was polluted (total coliform contamination) and almost half of the samples of non-municipal waters were exposed to high GI health risk (E. coli contamination). An association of E. coli exposure with the Mennonite lifestyle was limited to recent years. However, a concrete association between non-municipal water contamination and Mennonite or non-Mennonite lifestyle was not found in our dataset.
Addressing the first aim of this study, we found that during period one (1998 through 2008), water pollution and GI health risk levels were substantially high and there was no difference in these outcomes between the Mennonite or non-Mennonite lifestyles. However, during period two (2009 through 2012), samples from Mennonite households had significantly higher E. coli contamination, which exposed them to a high GI health risk. There was a similar relationship for high volume of total coliforms and E. coli microorganisms in samples collected from Mennonite households during period two. This increase in health risk among Mennonites could be due to the relatively steady rise in septic tank installations and adaptation of other safe waste disposal techniques by the non-Mennonite households during recent years [16]. However, results from period two should be interpreted with caution due to the small sample size. It is important to note that the water samples from non-Mennonite households had considerable contaminations of total coliforms and E. coli, which indicate that the non-municipal waters consumed by non-Mennonites are also substantially polluted and carry a considerable GI health risk.
The second aim of this study found that summer was the riskiest season to consume non-municipal waters. As is evident in the existing literature, higher E. coli contamination in non-municipal water sources was found to be associated with summer months [31–33]. Surface runoffs during rainfall and high heat indices during summer are well-known facilitating factors for distribution of fecal coliforms, i.e., E. coli [33–35]. Runoffs, which contain animal fecal material, in this hilly rural farming region, increased the chances of E. coli contamination in water sources and thus increased the burden of GI health risk in the surrounding population [31, 32].
Presence of naturally occurring total coliforms is not classified as a direct health risk, but rather, indicates presence of multiple unwanted microorganisms and increases the potential risk of exposure to E. coli (Fig. 2) [2, 4, 5]. On the other hand, E. coli contamination of one or more CFUs per 100 ml is directly associated with serious GI illness and has been established as a triggering point for public health safety measures [5, 12, 13, 36].
During period two, majority samples collected from non-Mennonite households, as compared to Mennonites, had significant presence of low GI health risk (zero E. coli, but one or more total coliform CFUs), but the average count of total coliform CFUs was higher among Mennonites. Irrespective of the mixed indications of health risk between the two lifestyles, there was substantial low GI health risk during period two in the entire region, along with a high mean of total coliform CFUs. Evident from these associations, both, Mennonites and non-Mennonites consuming non-municipal waters have a significantly increased potential of exposure to high GI health risk factors (fecal bacteria like E. coli). Incidences of Hepatitis A infections have been widely observed after consumption of water with high total coliform count, which can be reiterated by the fact that heavy presence of total coliforms increases chances of presence of viruses and other pathogenic contaminants [13, 37]. Bacterial load of as low as 23 total coliforms per 100 ml is capable of causing an acute outbreak of Hepatitis A in healthy children and other susceptible populations [38]. Similarly, a low infectious dose of 10–100 organisms per liter can cause Shigellosis, which is responsible for over one million deaths worldwide [39]. Hence, even in absence of detectable E. coli and in presence of high counts of total coliform, non-municipal waters could still carry a substantial potential of high GI health risk.
This study was successful in engaging the conservative Mennonite community; an important breakthrough for future public health policies. A top health priority in this region should be safeguarding drinking water sources and an immediate intervention strategy for all users of non-municipal waters.
Limitations
The main limitation of our study was low power of analysis, which further decreased due to exclusion of samples violating the holding time criteria. The maximum detectable limit of Quanti-Trays may have masked the true value of contamination in many samples; however, this did not affect the specific aims of our study. Data were not split into separate time periods while analyzing associations with seasonal variation as that would have critically reduced the sample size.
Although there is a statistical difference in sample collection from Mennonite versus non-Mennonite households during different seasons (“Appendix” Table 4), this may be due to logistic reasons. The distribution of main outcome variables, i.e., lifestyle, water quality and GI health risk, was not known prior to data collection and the selection of samples did not depend on these outcome factors. Thus, associating any predictor variable with these outcome variables is valid with limitation to only sample size. To validate these results further, a larger study is recommended in which similar number of samples should be collected during each season from same point sources.
Acknowledgments
We would like to acknowledge the contributions of Margaret Ann Vick, RS, Senior Environmental Health Specialist, Allen County Health Department, Scottsville, Kentucky in data gathering and the support of the Old Order Mennonite community of Allen County, Kentucky. Dr. Shesh Rai is the Wendell Cherry Chair in Clinical Trial Research at the University of Louisville and is supported by Dr. DM Miller, Director, James Graham Brown Cancer Center.
Conflict of interest
No conflict of interest to disclose.
Abbreviations
- ACHD
Allen County Health Department, Local Health Department
- CFU
Colony-forming units
- E. coli
Escherichia coli
- GI
Gastrointestinal
- GI health risk
Risk of GI illness from E. coli/other coliform drinking water contamination
- Lifestyle
Difference in lifestyle between Mennonite and non-Mennonite households
- Mennonites
Households following Old Order Anabaptist Mennonite lifestyle
- Municipal waters
Treated and regulated water under public health safety requirements
- Non-Mennonites
Households not following Old Order Anabaptist Mennonite lifestyle
- Non-municipal waters
Untreated and unregulated water from natural sources
- Total coliforms
Pathologically significant/non-significant microbial contaminants
- Period one
1998 through 2008
- Period two
2009 through 2012
- US EPA
United States Environmental Protection Agency
- Water quality
Potable/polluted for human consumption
Appendix
References
- 1.Kirk MD, et al. Assessing the incidence of gastroenteritis among elderly people living in long term care facilities. J Hosp Infect. 2010;76(1):12–17. doi: 10.1016/j.jhin.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 2.United States Environmental Protection Agency. Water: Basic Information about Regulated Drinking Water Contaminants. 2014. http://water.epa.gov/drink/contaminants/basicinformation/pathogens.cfm. Cited 25 April 2015.
- 3.Centers for Disease Control and Prevention. Private Water Systems—well testing. 2010. http://www.cdc.gov/healthywater/drinking/private/wells/testing.html. Cited 25 April 2015.
- 4.United States Environmental Protection Agency. Revised Total Coliform Rule—Webinar. 2013. http://water.epa.gov/lawsregs/rulesregs/sdwa/tcr/upload/rtcrwebinar41013-1-2.pdf. Cited 25 April 2015.
- 5.World Health Organization. Guidelines for Drinking-Water Quality, 4th ed. 2011. http://whqlibdoc.who.int/publications/2011/9789241548151_eng.pdf. Cited 25 April 2015.
- 6.Nataro JP, Kaper JB. Diarrheagenic Escherichia coli. Clin Microbiol Rev. 1998;11(1):142–201. doi: 10.1128/cmr.11.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levine MM. Escherichia coli that cause diarrhea: enterotoxigenic, enteropathogenic, enteroinvasive, enterohemorrhagic, and enteroadherent. J Infect Dis. 1987;155(3):377–389. doi: 10.1093/infdis/155.3.377. [DOI] [PubMed] [Google Scholar]
- 8.Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005;365(9464):1073–1086. doi: 10.1016/S0140-6736(05)71144-2. [DOI] [PubMed] [Google Scholar]
- 9.Bell BP, et al. A multistate outbreak of Escherichia coli O157:H7-associated bloody diarrhea and hemolytic uremic syndrome from hamburgers. The Washington experience. JAMA. 1994;272(17):1349–1353. doi: 10.1001/jama.1994.03520170059036. [DOI] [PubMed] [Google Scholar]
- 10.Frank C, et al. Epidemic profile of Shiga-toxin-producing Escherichia coli O104:H4 outbreak in Germany. N Engl J Med. 2011;365(19):1771–1780. doi: 10.1056/NEJMoa1106483. [DOI] [PubMed] [Google Scholar]
- 11.Edberg SC, et al. Escherichia coli: the best biological drinking water indicator for public health protection. Symp Ser Soc Appl Microbiol. 2000;29:106S–116S. doi: 10.1111/j.1365-2672.2000.tb05338.x. [DOI] [PubMed] [Google Scholar]
- 12.93rd United States Congress, Safe Drinking Water Act (SDWA). Washington, DC; 1974.
- 13.United States Environmental Protection Agency National primary drinking water regulations: revisions to the total coliform rule. Final Rule. Fed Register. 2013;70(30):10270–10365. [Google Scholar]
- 14.Centers for Disease Control and Prevention. Private Water Systems. 2014. http://www.cdc.gov/healthywater/drinking/private/index.html. Cited 25 April 2015.
- 15.United States Environmental Protection Agency. Private Drinking Water Wells. 2013. http://water.epa.gov/drink/info/well/index.cfm. Cited 25 April 2015.
- 16.Allen County Health Department. Scottsville, Kentucky.
- 17.Wilson, L. The quiet life. 2013. http://www.bgdailynews.com/news/the-quiet-life/article_8a74798d-bba1-579e-8ba3-4d8511c3a0c0.html. Cited 25 April 2015.
- 18.Valcour JE, et al. Associations between indicators of livestock farming intensity and incidence of human Shiga toxin-producing Escherichia coli infection. Emerg Infect Dis. 2002;8(3):252–257. doi: 10.3201/eid0803.010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones DE. Religious congregations & membership in the United States, 2000: An enumeration by region, state, and county based on data reported for 149 religious bodies, G.R. Center, Editor. Glenmary Research Center: Nashville, Tennessee; 2002.
- 20.Scharg P. Two-thirds world—what we learn from MWC’s membership census, in Mennonite World Review. 2013.
- 21.Department for Public Health, Division of Laboratory Services. Frankfort, Kentucky.
- 22.United States Environmental Protection Agency. Analytical methods approved for drinking water compliance monitoring under the Total Coliform Rule. 2009. http://www.epa.gov/ogwdw/methods/pdfs/methods/methods_tcr.pdf. Cited 25 April 2015.
- 23.IDEXX Laboratories Inc. Colilert. 2014. https://www.idexx.com/water/products/colilert.html. Cited 25 April 2015.
- 24.IDEXX Laboratories Inc. Quanti-Tray and Quanti-Tray/2000. 2014. https://www.idexx.com/water/products/quanti-tray.html. Cited 25 April 2015.
- 25.Rai SN, Sun J. Truncation in time to event data in encyclopedia of quantitative risk analysis and assessment. In Melnick EL, Everitt BS, editors. Wiley; 2008.
- 26.Microsoft Inc. 2014. http://www.microsoft.com. Cited 25 April 2015.
- 27.SAS Inc. 2014. http://www.sas.com. Cited 25 April 2015.
- 28.Agresti A. Categorical Data Analysis. Wiley; 2002.
- 29.Wilcoxon F. Individual comparisons by ranking methods. Biom Bull. 1945;1(6):80–83. doi: 10.2307/3001968. [DOI] [Google Scholar]
- 30.Hosmer, D. and S. Lemeshow, Applied Logistic Regression. 2000: Wiley.
- 31.Mukherjee A, et al. Preharvest evaluation of coliforms, Escherichia coli, Salmonella, and Escherichia coli O157:H7 in organic and conventional produce grown by Minnesota farmers. J Food Prot. 2004;67(5):894–900. doi: 10.4315/0362-028x-67.5.894. [DOI] [PubMed] [Google Scholar]
- 32.Salgado M, et al. Effect of soil slope on the appearance of Mycobacterium avium subsp. paratuberculosis in water running off grassland soil after application of contaminated slurry. Appl Environ Microbiol. 2013;79(12):3544–3552. doi: 10.1128/AEM.00610-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.St Laurent J, Mazumder A. Influence of seasonal and inter-annual hydro-meteorological variability on surface water fecal coliform concentration under varying land-use composition. Water Res. 2014;48:170–178. doi: 10.1016/j.watres.2013.09.031. [DOI] [PubMed] [Google Scholar]
- 34.Hong H, Qui J, Liang Y. Environmental factors influencing the distribution of total and fecal coliform bacteria in six water storage reservoirs in the Pearl River Delta Region, China. J Environ Sci (China) 2010;22(5):663–668. doi: 10.1016/S1001-0742(09)60160-1. [DOI] [PubMed] [Google Scholar]
- 35.National Climatic Data Center. 2014. http://www.ncdc.noaa.gov/IPS/. Cited 25 April 2015.
- 36.Soller J, et al. Risk-based evaluation of Escherichia coli monitoring data from undisinfected drinking water. J Environ Manage. 2010;91(11):2329–2335. doi: 10.1016/j.jenvman.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 37.Sowmyanarayanan TV, et al. Investigation of hepatitis A outbreak in children in an urban slum in Vellore, Tamil Nadu, using geographic information systems. Indian J Med Res. 2008;128(1):32–37. [PMC free article] [PubMed] [Google Scholar]
- 38.Chen J, et al. A hepatitis A outbreak caused by contaminated well water in a primary school of Jiangxi province, China, 2009. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(10):1014–1017. [PubMed] [Google Scholar]
- 39.Kotloff KL, et al. Global burden of Shigella infections: implications for vaccine development and implementation of control strategies. Bull World Health Organ. 1999;77(8):651–666. [PMC free article] [PubMed] [Google Scholar]