Abstract
Tolosa-Hunt syndrome, an idiopathic granulomatous inflammation of the cavernous sinus, is primarily a diagnosis of exclusion. The majority of patients present with unilateral orbital pain and features suggestive of paralysis of one or more of the cranial nerves passing through the cavernous sinus and/or superior orbital fissure. MRI of the head may show unilateral enhancement of the cavernous sinus and orbital apex. Treatment is with high-dose intravenous steroids followed by tapering oral steroids. Rapid amelioration of pain within 24–48 h supports this rare diagnosis. Resolution of neuropathies may take longer. We describe a case of a young man who presented with left periorbital pain, complete ophthalmoplaegia and ptosis of the left eye. MRI showed enhancement of the left cavernous sinus and orbital apex. High dose steroids led to complete resolution of pain, while ptosis and ophthalmoplaegia improved gradually.
Background
Tolosa-Hunt syndrome is a very rare diagnosis.1 The treating physician should rule out the more common causes of cavernous sinus syndrome, including cavernous sinus thrombosis, intraorbital or intraparenchymal tumours, and systemic granulomatous diseases such as sarcoidosis and tuberculosis. Once this diagnosis is considered, steroid therapy should be instituted and it should be kept in mind that the neuropathies may take a much longer time to resolve, which can be worrisome for the patient as well as for the doctor.
Case presentation
A 29-year-old previously healthy man presented with a 7-day history of severe pain around his left eye, extending back to the left temporal region. Pain was moderate to severe in intensity, sharp and continuous. This was associated with subsequent development of blurry vision and drooping of the left eyelid, without vomiting, dizziness, loss of consciousness or limb weakness. There was no history of fever, facial pain or hearing loss on the affected side.
At presentation, the patient's pulse rate was 83 bpm, blood pressure was 130/87 mm Hg and respiratory rate was 18 breaths/min. He was afebrile. He was alert, conscious and oriented to time, place and person. Examination of the left eye revealed partial ptosis, complete ophthalmoplaegia (frozen eye), decreased visual acuity, normal but blurred visual field and relative afferent pupillary defect (figure 1). There was no chemosis or proptosis. The right eye had normal ocular movements, visual acuity and visual field. Fundoscopy was normal in both eyes. Complete ophthalmological evaluation was performed to rule out glaucoma and other local eye pathologies. The rest of the neurological and systemic examination was unremarkable.
Figure 1.

Partial ptosis of the left eye. Examination also showed complete ophthalmoplaegia.
Family history was negative for any neurological disease. The patient was a non-smoker and did not use alcoholic. He was sexually active with one female partner without any risk factors for sexually transmitted diseases. He was not using any medications at the time of presentation.
Investigations
Complete blood count showed mild leucocytosis (white cell count of 12 000/µL) and haemoglobin of 17.1 g/dL (haematocrit 48.5%). Erythrocyte sedimentation rate was 20 mm/h. Serum chemistry, including liver function tests, was normal. Chest X-ray was negative for lesions. CT of the head was unremarkable except for mild asymmetric thickening of the left optic nerve sheath complex. Cerebrospinal fluid parameters were within normal limits including mycobacterial DNA. MR venography of the head and orbits showed thickening and significant enhancement of the lateral rectus muscle on the left side, along with ill-defined enhancement along the orbital apex extending into the left optic nerve canal. The left cavernous sinus appeared to be more homogenously enhanced compared to the right (figures 2–4). There was no evidence of an intraorbital mass or optic nerve enhancement. There were no areas of abnormal intensities in brain parenchyma, including the brainstem.
Figure 2.
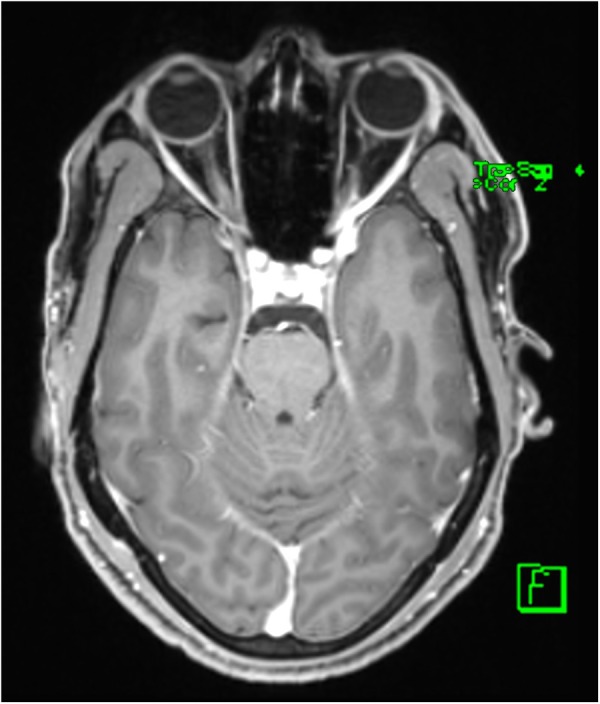
MRI of the brain (transverse section) showing enhancement of the cavernous sinus on the left side, extending into the orbital apex, along with involvement of the left lateral rectus muscle.
Figure 3.
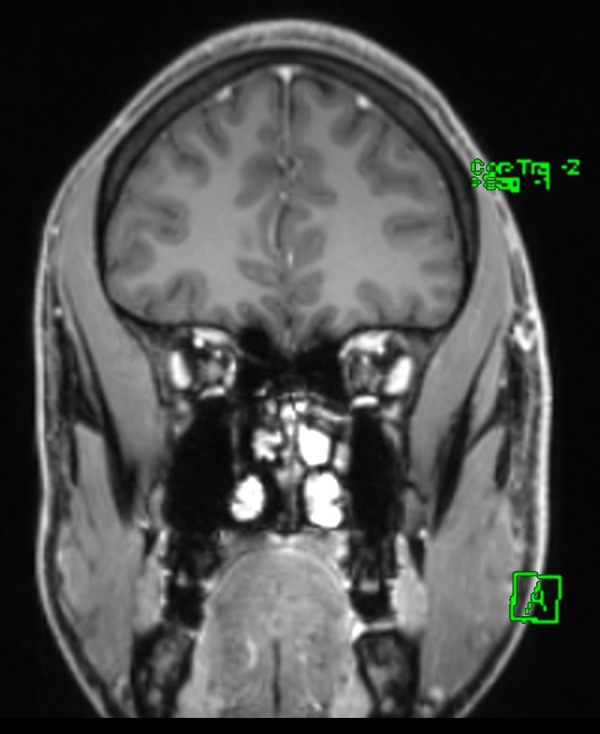
MRI of the brain (coronal section) showing homogenous enhancement of the left lateral rectus muscle and the orbital space.
Figure 4.
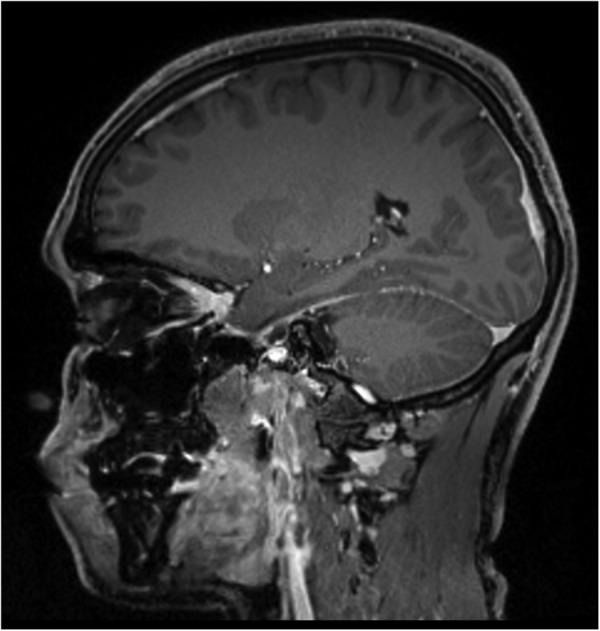
MRI of the brain (sagittal section) showing enhancement of the left cavernous sinus with extension into the orbital cavity.
Differential diagnosis
In palsy of a combination of the third, fourth and fifth cranial nerves, the pathology is most likely to be seated in the areas where all three of these nerves are in close proximity to each other. Two such areas are the cavernous sinus and orbital apex (including superior orbital fissure and part of the orbital cavity). Cavernous sinus thrombosis is the most ominous differential diagnosis. The cavernous sinus can also be compressed from outside by an intraparenchymal space occupying lesion, especially a tumour. Orbital tumours or pseudotumours can have such a presentation, but such cases frequently have proptosis and chemosis. MRI of the brain and orbits with angiography is invaluable in such a scenario, as it has high sensitivity in detecting most of these. As Tolosa-Hunt syndrome is an idiopathic granulomatous inflammation, systemic granulomatous diseases such as sarcoidosis and tuberculosis should be ruled out before considering it.2
Treatment
The patient was treated with high-dose intravenous methylprednisolone (1 g/day) for 5 days. By day 2, the pain was completely resolved. The ophthalmoplaegia, ptosis and blurry vision were still present. By day 5, his ophthalmoplaegia had slightly improved. On the sixth day, the patient was discharged on oral steroids and with regular appointments for follow-up.
Exclusion of the other causes of such a presentation, MRI findings and his response to steroids supported the diagnosis of Tolosa-Hunt syndrome.
Outcome and follow-up
The patient was discharged on oral steroids with tapering doses for 6 weeks. On follow-up visits, he showed gradual improvement in his motor deficits. His 6-week follow-up office visit showed complete resolution of ophthalmoplaegia as well as the ptosis (figure 5). Follow-up MRI showed resolution of findings seen on the previous imaging (figure 6–8).
Figure 5.

Resolved ptosis of the left eye after a 6-week course of steroids. Examination also showed resolution of ophthalmoplaegia.
Figure 6.

Follow-up MRI of the brain (transverse section) after completing a 6-week course of steroids. Significant resolution of enhancement seen on previous imaging (compare with figure 2).
Figure 7.
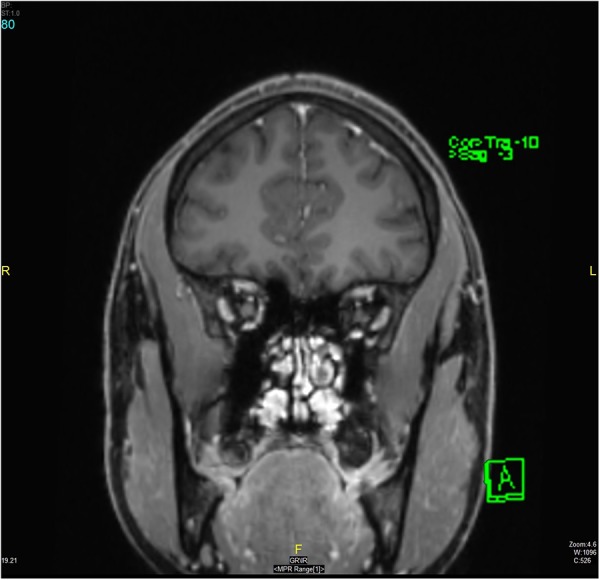
Follow-up MRI of the brain (after steroids). Significant reduction in enhancement of left lateral rectus muscle and orbital space seen on previous imaging (compare with figure 3).
Figure 8.
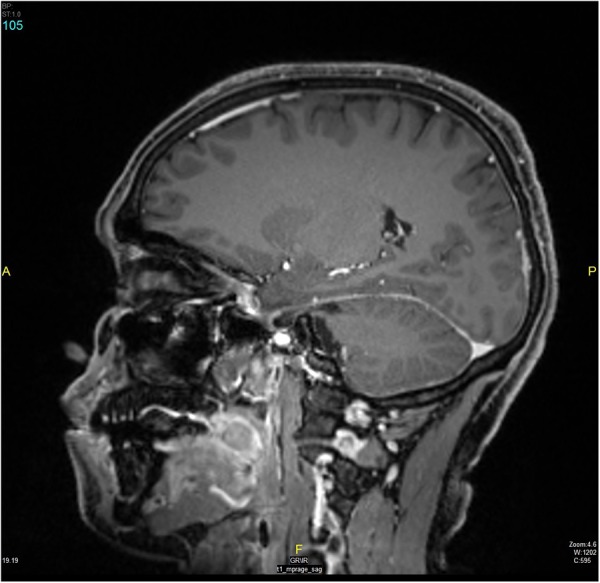
Follow-up MRI of the brain (after steroids). Significant improvement in left cavernous sinus enhancement (compare with figure 4).
Discussion
First described in 1954, Tolosa-Hunt syndrome is a granulomatous inflammation of the cavernous sinus and/or superior orbital fissure leading to the compression of any or all of the following: the third, fourth or sixth cranial nerves, V1 and/or V2 divisions of the fifth cranial nerve or the intracavernous part of the internal carotid artery.3 This produces either partial or complete ophthalmoplegia, ptosis and orbital/periorbital/hemicranial pain.4 Inflammation usually originates in the cavernous sinus, and extends forward to involve the superior orbital fissure and orbital cavity. Some reported cases have also mentioned the involvement of the second, fifth and acoustic nerves. It tends to be an episodic illness, with the episodes spaced apart over many months and lasting for a few weeks to months. It is a very rare disorder with a reported incidence of one in a million individuals per year.
The aetiology of Tolosa-Hunt syndrome is largely unknown.4 As described above, the hallmark of this disease is the non-specific granulomatous inflammation characterised by infiltration of lymphocytes and plasma cells primarily in and around the cavernous sinus, with variable extension into and beyond the superior orbital fissure/orbital apex. What incites this inflammatory reaction is still unclear. It is considered a very benign illness, but exclusion of more malignant diseases bears utmost importance whenever any patient presents with such clinical features.5 6 Knowing the differential diagnoses is more important to rule out other causes than to rule in the syndrome itself.
Tolosa-Hunt does not have any age or sex predilection7 and can affect anyone in the first to eighth decade of life. It is almost always unilateral (except in 4–5% of cases) and if bilateral, it shifts the balance in support of other differential diagnoses. The main utility of MRI with MR venography of the brain is to exclude cavernous sinus thrombosis and intraorbital or intraparenchymal tumour. Typical MRI findings include enhancement of the affected cavernous sinus.8 These findings are not unique to Tolosa-Hunt syndrome and may also be found in other diseases, such as lymphoma. Biopsy of the lesion is the most definitive diagnostic test, but it is seldom necessary unless the patient is not responding to standard therapy and is worsening clinically.4
The International Headache Society diagnostic criteria for Tolosa-Hunt syndrome are as follows.9
One or more episodes of unilateral orbital pain persisting for weeks if untreated.
Paresis of one or more of the third, fourth and/or sixth cranial nerves and/or demonstration of cavernous sinus granuloma by MRI or biopsy.
Paresis coincides with the onset of pain or follows it within 2 weeks.
Pain and paresis resolve within 72 h when treated adequately with corticosteroids.
Other causes have been excluded by appropriate investigations.
It usually resolves spontaneously, only to recur and remit in some cases.10 11 High-dose glucocorticoids are the first line treatment for Tolosa-Hunt syndrome considering its inflammatory pathology.3 There is not sufficient evidence for the appropriate dose, route of administration and duration of therapy.12 A remarkable feature of glucocorticoid therapy is the rapid resolution of the orbital pain within 1–3 days, which also serves as diagnostic confirmation.10 13 Our patient responded in a similar manner. In one study, 40% of patients achieved pain relief within 72 h and 78% within a week. In contrast, resolution of neuropathies lags behind for months,10 which necessitates a longer course of steroids. Sometimes, in unfortunate cases, the neurological deficits may persist for life. Radiological improvement takes an even longer time to resolve; therefore, persistence of MRI findings, unless non-regressing, should not alter the recommended duration of therapy. After an initial high-dose steroid regimen, an oral taper over the course of several weeks is recommended, along with regular follow-up with subsequent MRI studies to document the resolution of the disease. Immunosuppressive drugs are the other therapeutic modality for Tolosa-Hunt syndrome. Recurrence of the disease occurs in about 50% of the patients, which is quite alarming.
Learning points.
Tolosa-Hunt syndrome is a diagnosis of exclusion. More ominous causes should be ruled out when a patient presents with such features.
Steroids have both diagnostic as well as therapeutic significance in Tolosa-Hunt syndrome.
Dramatic reduction of pain is typical with steroids while the motor signs due to cranial neuropathies may take a few weeks to resolve.
Patients should be followed up regularly to ensure resolution of symptoms and signs, and also for early detection of relapse, which happens in nearly 50% of the patients.
MRI of the brain and orbits with MR venography is of utmost importance in Tolosa-Hunt syndrome, especially to rule out other pathologies involving the cavernous sinus and orbital apex.
Footnotes
Contributors: AA and SN actively participated in writing this case report as well as in appropriate literature review. AA was also involved in taking direct care of the patient under the supervision of AR. MSP helped the authors in the literature review as well as in manuscript writing and in organising the images in an appropriate manner. The case report was finalised by all four authors before submission.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lachanas VA, Karatzias GT, Tsitiridis I et al. Tolosa-Hunt syndrome misdiagnosed as sinusitis complication. J Laryngol Otol 2008;122:97–9. 10.1017/S0022215106005317 [DOI] [PubMed] [Google Scholar]
- 2.Gladstone JP. An approach to the patient with painful ophthalmoplegia, with a focus on Tolosa-Hunt syndrome. Curr Pain Headache Rep 2007;11:317–25. 10.1007/s11916-007-0211-7 [DOI] [PubMed] [Google Scholar]
- 3.Kline LB, Hoyt WF. The Tolosa-Hunt syndrome. J Neurol Neurosurg Psychiatry 2001;71:577–82. 10.1136/jnnp.71.5.577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paovic J, Paovic P, Bojkovic I et al. Tolosa-Hunt syndrome—diagnostic problem of painful ophthalmoplegia. Vojnosanit Pregl 2012;69:627–30. 10.2298/VSP1207627P [DOI] [PubMed] [Google Scholar]
- 5.Singh MK, Marshall B, Hawley J. Painful ophthalmoplegia: a case of Tolosa-Hunt syndrome. Mil Med 2014;179:e1409–10. 10.7205/MILMED-D-14-00265 [DOI] [PubMed] [Google Scholar]
- 6.Abdelghany M, Orozco D, Fink W et al. Probable Tolosa-Hunt syndrome with a normal MRI. Cephalalgia 2015;35:449–52. 10.1177/0333102414539053 [DOI] [PubMed] [Google Scholar]
- 7.Peterfi A, Zadori P, Suto G et al. [Tolosa-Hunt syndrome]. Ideggyogy Sz 2011;64:24–8. [PubMed] [Google Scholar]
- 8.Jain R, Sawhney S, Koul RL et al. Tolosa-Hunt syndrome: MRI appearances. J Med Imaging Radiat Oncol 2008;52:447–51. 10.1111/j.1440-1673.2008.01988.x [DOI] [PubMed] [Google Scholar]
- 9.Colnaghi S, Versino M, Marchioni E et al. ICHD-II diagnostic criteria for Tolosa-Hunt syndrome in idiopathic inflammatory syndromes of the orbit and/or the cavernous sinus. Cephalalgia 2008;28:577–84. 10.1111/j.1468-2982.2008.01569.x [DOI] [PubMed] [Google Scholar]
- 10.Zhang X, Zhang W, Liu R et al. Factors that influence Tolosa-Hunt syndrome and the short-term response to steroid pulse treatment. J Neurol Sci 2014;341:13–16. 10.1016/j.jns.2014.03.031 [DOI] [PubMed] [Google Scholar]
- 11.Kovacic M, Kovacic I, Krvavica A et al. [Tolosa-Hunt syndrome: a case report]. Lijec Vjesn 2010;132:147–50. [PubMed] [Google Scholar]
- 12.Kirbas D, Topcular B, Ozcan ME et al. Idiopathic Tolosa-Hunt syndrome: four additional cases. Ideggyogy Sz 2008;61:250–4. [PubMed] [Google Scholar]
- 13.Hung CH, Chang KH, Wu YM et al. A comparison of benign and inflammatory manifestations of Tolosa-Hunt syndrome. Cephalalgia 2013;33:842–52. 10.1177/0333102412475238 [DOI] [PubMed] [Google Scholar]


