Abstract
Context:
Cost-effectiveness analysis should continually assess competing health care options especially in high volume environments like cataract surgery.
Aims:
To compare the cost effectiveness of phacoemulsification (PE) versus manual small-incision cataract surgery (MSICS).
Settings and Design:
Prospective randomized controlled trial. Tertiary care hospital setting.
Subjects and Methods:
A total of 52 consenting patients with age-related cataracts, were prospectively recruited, and block randomized to PE or MSICS group. Preoperative and postoperative LogMAR visual acuity (VA), visual function-14 (VF-14) score and their quality-adjusted life years (QALYs) were obtained, and the change in their values calculated. These were divided by the total cost incurred in the surgery to calculate and compare the cost effectiveness and cost utility. Surgery duration was also compared.
Statistical Analysis Used:
Two group comparison with Student's t-test. Significance set at P < 0.05; 95% confidence interval (CI) quoted where appropriate.
Results:
Both the MSICS and PE groups achieved comparative outcomes in terms of change (difference in mean [95% CI]) in LogMAR VA (0.03 [−0.05−0.11]), VF-14 score (7.92 [−1.03−16.86]) and QALYs (1.14 [−0.89−3.16]). However, with significantly lower costs (INR 3228 [2700–3756]), MSICS was more cost effective, with superior cost utility value. MSICS was also significantly quicker (10.58 min [6.85–14.30]) than PE.
Conclusions:
MSICS provides comparable visual and QALY improvement, yet takes less time, and is significantly more cost-effective, compared with PE. Greater push and penetration of MSICS, by the government, is justifiably warranted in our country.
Keywords: Cost-effectiveness, manual small incision cataract surgery, phacoemulsification, quality adjusted life year, visual function-14
Undoubtedly, better health services improve health. It is often the available resources that become the limiting factor when one has to choose between competing options. To maximize health outcomes, vis-à-vis the costs, decision makers use health economics to compare and rate different programs.[1]
Various methods to compare the relative costs as well as health gains of different health interventions such as cost-benefit analysis (CBA), cost-effectiveness analysis (CEA), cost utility analysis (CUA), cost efficiency analysis and cost minimization analysis exist.[2] CBA compares both the costs and benefits that accrue in monetary terms. CUA assesses both technical and allocative efficiency within the health care sector: The basic outcome is “healthy years.” The years of life in states less than full health can be converted to healthy years by the use of various techniques like quality-adjusted life years (QALYs) and disability-adjusted life years DALYs.[1] The idea behind QALY is that it assumes that a year of life lived in perfect health is worth 1 QALY (1-year of life × 1 utility value = 1 QALY) and that a year of life lived in a state of less than this perfect health is worth <1.
The weight values are usually determined in three common ways: In time-trade-off,[3] the individual is asked to choose between remaining in a state of ill-health for a period of time, or being restored to perfect health but with a shorter life expectancy; standard gamble requires a respondent to trade off the certainty of being in an intermediate health state for his remaining life expectancy with a “treatment” which offers a chance of regaining full health for his remaining life expectancy but that also entails a risk of immediate death;[4] finally, an individual is asked to rate a state of ill health on a visual analog scale (VAS) from 0% to 100%, with 0 representing death and 100 representing perfect health. The last has the advantage of being easiest to ask but is the most subjective.[5]
Quality adjusted life years can be incorporated with medical costs to reach a final common denominator of cost/QALY which can be used to develop a CEA of any intervention. CEA concentrates on one major desired outcome or benefit in terms of effectiveness rather than valuing it in terms of money. It is particularly useful to evaluate different interventions for the same disease to identify which one is better both in terms of cost and health gain, and is an important aid to public health decision making.
The WHO also recommends the CEA approach to evaluate a range of health interventions,[6] especially when confronted with competing alternatives in the face of scarce resources. CEA has been extensively used in all fields of health care, including ophthalmology. Cataract surgery is a routine intervention, the demand for which is expected to increase strongly as the population is ageing.[7,8] Phacoemulsification (PE) is considered the standard of care for cataract surgery in the developed world.[9] Costs, in terms of equipment, consumables, and training, has limited its use in the developing world, in contrast to manual small incision cataract surgery (MSICS).
We evaluated the cost-effectiveness of PE (with foldable intraocular lenses [IOLs]) versus MSICS (with rigid IOLs), from the point of view of the limited finances available in the university's health scheme; and also because we found such studies to be few and far from our country.
Subjects and Methods
After obtaining clearance from the institutional review board, 52 consenting patients with age-related cataracts, were prospectively recruited and block randomized to PE group or MSICS group. We included patients of ≥40 years, with an operable cataract; and excluded those with ocular co-morbidity likely to impact vision, such as corneal opacity, maculopathy or macular edema; also excluded were patients who failed to comprehend our questionnaire or those refusing participation. Detailed biomicroscopy and ophthalmoscopy were undertaken, including dry and wet retinoscopy and LogMAR visual acuity (VA). Preoperatively, the patients were scored on the visual function-14 (VF-14) questionnaire (served in colloquial Hindi),[10] and their QALYs were calculated as the product of the VAS and life expectancy.[11] A similar exercise was carried out at 4–6 weeks postoperatively, to obtain a change in score on the VF-14 and in QALYs.
The costs of surgery were calculated using 2012–2013 as the base year: And included the combined costs incurred by the hospital (capital costs) and the patient. Capital costs included the cost of building, equipment (surgical microscopes, PE machine, and surgical instruments) and running-overtime (OT) costs (i.e., the cost of the personnel and electricity). Costs of building, personnel and electricity were aggregated and divided by the total available OT table time (in hours) to calculate the cost of OT table time/h (overhead rate). Total time of surgery was calculated from the time at an entry to exit from the OT: To which we added 1-h, assuming this would cover pre- and post-operative time in the OT environs. This was multiplied by the overhead rate to get the overhead costs. Cost of the equipment per patient was calculated by dividing the depreciated cost of the equipment by the average number of patients being operated in a year.
Salient details about the cost-calculations
Annual cost of OT building was INR 108,464.76 (using the PWD manual, and based on covered area). This cost for the whole year was divided by the product of 260 days (the average number of working days in a year) and 8 h (the average working hours in a day) to arrive at cost/h: 108,464.76/(260 × 8) = INR 52.14/h.
Similarly, the hourly cost of electricity (INR 98.93/h) and manpower or personnel (INR 1320.98/h) was calculated.
Combined hourly cost of the building electricity and manpower was thus the sum of: 52.14 + 98.93 + 1320.98 = INR 1472.05/h, now referred to as hourly overhead cost.
The cost of the equipment was calculated as the purchase price depreciated linearly over the life span of the equipment as suggested by Asimakis et al.[12] The cost of the equipment per patient was calculated by dividing the cost for 1-year by the number of patients operated in 1-year. In the case of the PE machine, the annual cost was divided by the number of patients undergoing PE only: We obtained values of INR 435.3 in MSICS and INR 1602.98 in PE group.
Patient costs included hospital fees, laboratory charges, consumables and transportation costs and included cost due to loss of wages of the patient and accompanying attendant; with the last being nil in the case of unemployed. Patient costs were split into direct costs (IOL cost + cost of other consumables + investigation and admission charges) and indirect costs (travel costs + loss of wages); since we were interested in the former, because that is, the amount reimbursed by our university.
Our main outcome measures thus were costs per unit change in QALYs, VF-14 scores and LogMAR VA, which were compared between PE and MSICS groups using t-tests, with significance set at P < 0.05.
Results
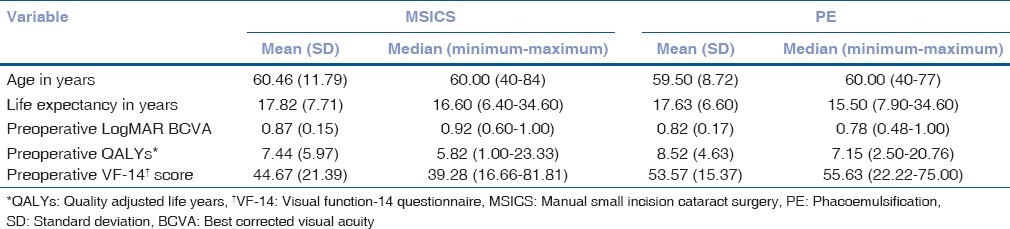
Age distribution, LogMAR best corrected VA (BCVA), VF-14 scores, life expectancy and QALYs were similar in the two groups at baseline [Table 1]. Gender-wise distribution was similar: Females were 57.69% (15 of 26) in MSICS and 50% (13 of 26) in PE group (χ2 P = 0.78).
Table 1.
Baseline characteristics of patients in MSICS (n=26) and PE (n=26) groups
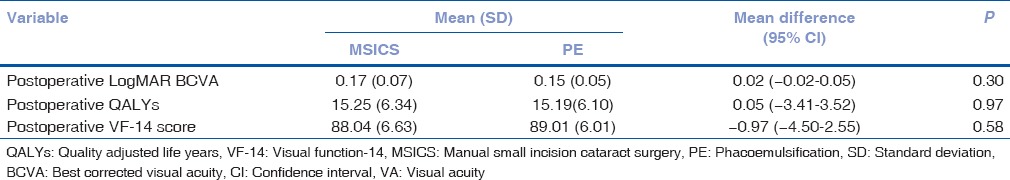
Postoperative LogMAR BCVA, QALYs, and VF-14 scores are depicted and compared between groups in Table 2.
Table 2.
Comparison of postoperative LogMAR BCVA (VA), QALYs and VF-14 core between MSICS and PE groups
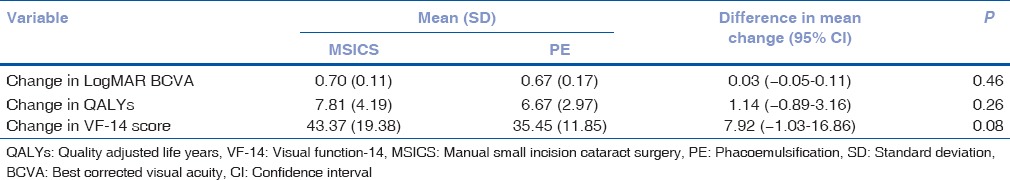
Between groups, comparison of change of LogMAR BCVA, QALYs, and VF-14 scores, from preoperative to postoperative values, are shown in Table 3.
Table 3.
Comparison of gains in LogMAR BCVA, QALYs and VF-14 scores following surgery in MSICS (n=26) and PE (n=26) groups
In our study, PE (duration in minutes: Mean [standard deviation (SD)]: 45.35 [6.39]) took significantly longer, compared to MSICS (34.77 [6.98] min): Mean difference (10.58 min, 95% confidence interval [CI] for difference: 6.85–14.30 min; P < 0.001).
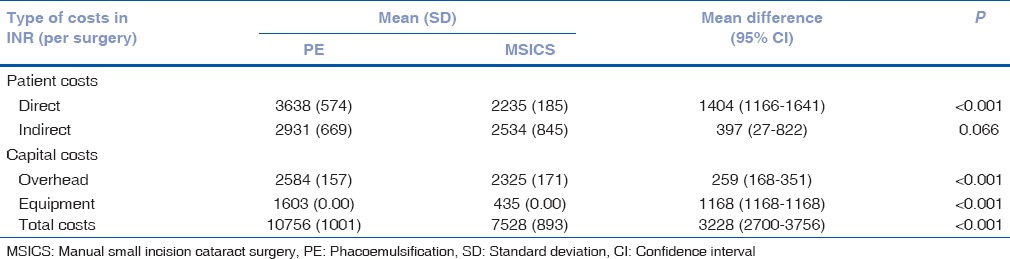
The group-wise comparative cost of surgery, rounded off to the nearest rupee, is presented in Table 4.
Table 4.
Comparison of the costs (in INR) incurred in MSICS and PE groups
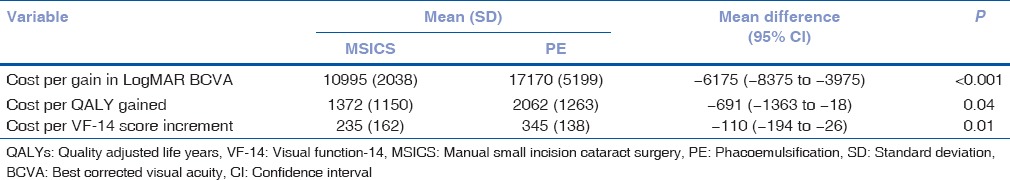
Cost for one unit gain in LogMAR BCVA, VF-14 scores and QALYs in both the groups is shown in Table 5.
Table 5.
Comparison of cost per unit gain in LogMAR BCVA, VF-14 score and QALYs in MSICS (n=26) and PE (n=26) groups
Discussion
In our study, both the MSICS and PE groups achieved comparable outcomes [Table 2]. The mean change in LogMAR BCVA at 6 weeks was 0.7 (SD = 0.11) in MSICS and 0.67 (SD = 0.17) in PE group (P = 0.46) [Table 3]. The mean postoperative LogMAR BCVA was 0.17 (SD = 0.07) in MSICS group and 0.15 (SD = 0.05) in PE group (P = 0.30) [Table 2]. Gogate in a randomised controlled trial (RCT) in Nepal found no significant differences in proportion with BCVA >6/18 at 6 weeks postoperatively: 184 of 187 (98.4%) in MSICS and 182 of 185 (98.4%) in PE group (P = 0.549).[13] Khanna reported equivalent proportion of patients with BCVA >6/12 Snellen in the two groups: 84.3% (440 of 522) in MSICS and 88% (446 of 507) in PE group (P = 0.09).[14]
Likewise, Ruit et al. in his RCT found no difference in the proportion of patients with BCVA ≥20/60 in the two groups: 98% in each.[15] Similarly Jongsareejit et al., Ang et al. and Venkatesh et al. in their respective studies found MSICS to be safe and effective.[16,17,18]
By 4–6 weeks, there was a similar gain in QALYs in both our groups: A mean change of 7.81 (SD = 4.19) in MSICS group and 6.67 (SD = 2.97) in PE group (P = 0.26) [Table 3]. There was also increment in VF-14 score with a nonsignificant difference in mean change of 43.37 (SD = 19.38) in MSICS group and 35.45 (SD = 11.18) in PE group (P = 0.08) [Table 3]. Manaf et al. in an RCT in Malaysia reported a significant, but comparable increase in VF-14 scores 6 weeks postcataract surgery, in both extracapsular cataract extraction (ECCE) and PE: A mean increase in VF-14 scores of 32.71 in ECCE and 27.03 in the PE (P = 0.225).[19] Unlike us, their study had ECCE as the comparator, while we had MSICS.
In our study, time-wise, PE duration was significantly longer compared to MSICS by on average 10.58 min (95% CI: 6.85–14.30). Ruit et al. and Venkatesh et al. in their respective studies also found that MSICS was quicker than PE.[15,20]
The direct costs to the patients were significantly more for PE compared to MSICS, by on average INR 1404 (P < 0.001) [Table 4]. This is largely on account of differences in cost of IOLs. Ruit et al. in their study also found similar results.[15] Given an average of 775 cataract cases (on the basis of average of the last 3 years (2011–2013) data at our institution) being operated in a year, if all the cases were to undergo PE, the total direct costs would be INR 2,819,450 (775 × 3638 i.e., average number of cases operated annually X direct costs in PE). Similarly, the total direct costs would be INR 1,732,125 if all the cases would undergo MSICS. In such a hypothetical situation, if everyone opted for MSICS instead of PE, in terms of direct costs (which are the costs funded by sponsoring agencies) there would be a net saving of INR 1,087,325 annually. These direct costs are usually reimbursed by the health scheme resources. We believe these resources could be directed toward more cost effective alternatives not only in the field of ophthalmology but other medical treatments too. Likewise, the overhead cost was significantly higher in the PE group by INR 259 (P < 0.001). Furthermore, the cost of the equipment was significantly greater by INR 1168 (P < 0.001) in the PE group, essentially due to the inclusion of the cost of the PE machine. Ruit et al., Gogate et al. and Muralikrishnan et al. in their studies also found the cost of equipment to be higher in PE group.[15,21,22] In our study, the total cost per surgery was found to be significantly higher in the PE group by INR 3228 (P < 0.001).
Comparison of cost per unit increment in VF-14 score gained in the two groups showed it to be higher in the PE group by INR 110.0 (P = 0.01), implying that MSICS is a more cost effective option. Manaf et al. in his RCT also calculated cost per VF-score gained, and found it to be US $14 for ECCE as compared to US $20 for PE, and like us, concluded that ECCE was more cost effective than PE.[19] Our study also showed the cost per gain in LogMAR BCVA to be significantly higher in PE group by INR 6175 (P < 0.001) [Table 5]. It makes for more intuitive understanding if we compare costs per line LogMAR gained (each line being equivalent to 0.1 LogMAR): Thus PE was costlier by an average of INR 618 for each line VA gained on the LogMAR chart compared to MSICS.
The cost-utility was significantly (P = 0.04) superior in MSICS (INR 1372 per QALY gained) compared to PE (INR 2062 per QALY gained).
In health programs, where there is chronic scarcity of funds, as evidenced by a 20% reduction in health from the annual national budget (India Today December, 2014), interventions which are cheaper and yet provide equally good outcomes should be adopted and actively propagated. Our study shows that MSICS is comparably as effective as PE in terms of visual rehabilitation and increasing the quality of life in cataract patients. However, MSICS is significantly less expensive and does not require the capital expenditure and maintenance of PE machine which requires a dependable source of energy, which is usually a limiting factor in developing countries. Training in PE also has a steeper learning curve.[13] The foldable IOLs used in PE are also far more expensive than the rigid polymethyl methacrylate IOLs used in MSICS. Treating cataract in the developing world is a formidable challenge with significant barriers like cost, lack of awareness and shortage of trained personnel. MSICS with its shorter surgical time and its requirement for less expensive and less technology dependent equipment can help in overcoming this challenge. Health care expenditures are continuously rising throughout the world. Regular cost-effectiveness studies should be carried out in various fields to look for the best intervention amongst the alternatives. This will ensure proper channelization of resources for a sustainable growth in the medical field.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Satpathy SK, Bansal RD. Health economics – Concepts and conceptual problems. Health Popul Perspect Issues. 1982;5:23–33. [PubMed] [Google Scholar]
- 2.Phillips C, Thompson G. Health Economics. What is Series. [Last accessed on 2012 Dec 07]. Available from: http://www.whatisseries.co.uk/what-is-cost-effectiveness/
- 3.Burström K, Johannesson M, Diderichsen F. A comparison of individual and social time trade-off values for health states in the general population. Health Policy. 2006;76:359–70. doi: 10.1016/j.healthpol.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 4.Torrance GW. Measurement of health state utilities for economic appraisal. J Health Econ. 1986;5:1–30. doi: 10.1016/0167-6296(86)90020-2. [DOI] [PubMed] [Google Scholar]
- 5.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–36. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 6.Edejer TT, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, et al. Geneva: World Health Organization; 2003. WHO Guide to Cost-Effectiveness Analysis. [Google Scholar]
- 7.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 8.Dandona L, Dandona R, John RK. Estimation of blindness in India from 2000 through 2020: Implications for the blindness control policy. Natl Med J India. 2001;14:327–34. [PubMed] [Google Scholar]
- 9.Minassian DC, Rosen P, Dart JK, Reidy A, Desai P, Sidhu M, et al. Extracapsular cataract extraction compared with small incision surgery by phacoemulsification: A randomised trial. Br J Ophthalmol. 2001;85:822–9. doi: 10.1136/bjo.85.7.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112:630–8. doi: 10.1001/archopht.1994.01090170074026. [DOI] [PubMed] [Google Scholar]
- 11.SRS Based Abridged Life Tables. [Last accessed on 2014 Jul 15]. Available from: http://www.censusindia.gov.in/vital_statistics/SRS_Based/India_2006.10.pdf .
- 12.Asimakis P, Coster DJ, Lewis DJ. Cost effectiveness of cataract surgery. A comparison of conventional extracapsular surgery and phacoemulsification at Flinders Medical Centre. Aust N Z J Ophthalmol. 1996;24:319–25. doi: 10.1111/j.1442-9071.1996.tb01602.x. [DOI] [PubMed] [Google Scholar]
- 13.Gogate PM, Kulkarni SR, Krishnaiah S, Deshpande RD, Joshi SA, Palimkar A, et al. Safety and efficacy of phacoemulsification compared with manual small-incision cataract surgery by a randomized controlled clinical trial: Six-week results. Ophthalmology. 2005;112:869–74. doi: 10.1016/j.ophtha.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 14.Khanna RC, Kaza S, Palamaner Subash Shantha G, Sangwan VS. Comparative outcomes of manual small incision cataract surgery and phacoemulsification performed by ophthalmology trainees in a tertiary eye care hospital in India: A retrospective cohort design. BMJ Open. 2012;2:pii–e001035. doi: 10.1136/bmjopen-2012-001035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruit S, Tabin G, Chang D, Bajracharya L, Kline DC, Richheimer W, et al. A prospective randomized clinical trial of phacoemulsification vs manual sutureless small-incision extracapsular cataract surgery in Nepal. Am J Ophthalmol. 2007;143:32–38. doi: 10.1016/j.ajo.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 16.Jongsareejit A, Wiriyaluppa C, Kongsap P, Phumipan S. Cost-effectiveness analysis of manual small incision cataract surgery (MSICS) and phacoemulsification (PE) J Med Assoc Thai. 2012;95:212–20. [PubMed] [Google Scholar]
- 17.Ang GS, Wheelan S, Green FD. Manual small incision cataract surgery in a United Kingdom university teaching hospital setting. Int Ophthalmol. 2010;30:23–9. doi: 10.1007/s10792-008-9286-3. [DOI] [PubMed] [Google Scholar]
- 18.Venkatesh R, Das M, Prashanth S, Muralikrishnan R. Manual small incision cataract surgery in eyes with white cataracts. Indian J Ophthalmol. 2005;53:173–6. doi: 10.4103/0301-4738.16675. [DOI] [PubMed] [Google Scholar]
- 19.Manaf MR, Aljunid SM, Annuar FH, Leong CK, Mansor N. Cost-effectiveness analysis of cataract surgery with intraocular lens implantation: Extracapsular cataract extraction versus phacoemulsification. Med J Indones. 2007;16:25–31. [Google Scholar]
- 20.Venkatesh R, Tan CS, Sengupta S, Ravindran RD, Krishnan KT, Chang DF. Phacoemulsification versus manual small-incision cataract surgery for white cataract. J Cataract Refract Surg. 2010;36:1849–54. doi: 10.1016/j.jcrs.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 21.Gogate P, Deshpande M, Nirmalan PK. Why do phacoemulsification?. Manual small-incision cataract surgery is almost as effective, but less expensive. Ophthalmology. 2007;114:965–8. doi: 10.1016/j.ophtha.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 22.Muralikrishnan R, Venkatesh R, Prajna NV, Frick KD. Economic cost of cataract surgery procedures in an established eye care centre in Southern India. Ophthalmic Epidemiol. 2004;11:369–80. doi: 10.1080/09286580490888762. [DOI] [PubMed] [Google Scholar]


