INTRODUCTION
Anxiety is common in pre-operative patients and may be associated with hypertension, arrhythmias, increased pain perception and increased requirement of anaesthetic drugs.[1] Pre-operative education decreases anxiety and improves the patient knowledge about the general process of anaesthesia, the risks associated with it and dispels the misconception.[2] Many studies suggest that pre-anaesthesia interviews are not enough for adequate transfer of knowledge, and hence, alternative methods are required.[3] Hence, we decided to study the effect of anaesthesia information booklet on patient anxiety and knowledge.
METHODS
After Institutional Ethics Committee approval, 100 consenting patients of American Society of Anaesthesiologists physical status I and II with knowledge of English, of 18–60 years age group, undergoing elective surgeries were included. Patients who had received anaesthesia in previous 3 years, health care professionals, visually impaired or mentally unstable were excluded. Considering a 25% difference in anxiety and knowledge to be clinically relevant, with a power of 80% and α = 0.05, the sample size required was calculated as 46 patients in each group. All patients underwent a pre-anaesthesia check on an outpatient basis. Patients were admitted the evening before surgery and were visited by an anaesthesia registrar who explained the visual analogue scale (VAS) score for the patients for assessing their anxiety levels (0–100 mm where, 0 = no anxiety, 100 = maximum anxiety). Patients then answered a questionnaire and recorded their VAS score. The 10-point questionnaire was designed to assess knowledge, retention of facts pertaining to the risks of anaesthesia procedure, perioperative instructions, the role of the anaesthesiologist and misconceptions. The questions included three process questions, three risk questions and four questions on misconception of anaesthesia. Responses were recorded as true or false. One point was assigned for each correct answer with no points for unanswered questions or a wrong answer and the total score was recorded.
The patients were then randomly allocated to either Group A or Group B, based on a computer generated number kept in sealed envelopes. Patients in Group A were given an information booklet on anaesthesia by a qualified anaesthesiologist not involved in the study or data analysis. The seven-page information booklet (font size 13) introduced the role of the anaesthesiologist, procedural differences, risks of anaesthesia, the rationale for perioperative instructions and answers to frequent concerns about anaesthesia. Group B patients had only a routine pre-operative visit by the same anaesthesiologist. Although the process, the risks and misconceptions of anaesthesia procedure were explained, and queries from the patient were answered during the visit, it was not standardised in order to make our study applicable to real practice.
Both groups of patients were once again given the 10 item questionnaire, approximately after 2 h by the same anaesthesia registrar blinded to the groups, to reassess their knowledge and anxiety levels. Comparisons were made between groups using Student's t-test and Chi-square test. The level of significance was set at P < 0.05. Statistical analysis was performed using SPSS software version 20.
RESULTS
The study population included 100 patients; 50 in Group A and 50 in Group B. The demographic data were comparable in both groups. Baseline patient anxiety VAS score levels in both groups were comparable. After the intervention, both groups had a decreased anxiety level from the baseline with a significant decrease in Group A (P < 0.01) [Figure 1]. In Group A, 82% understood the process of anaesthesia as against only 44% in Group B (P < 0.001). Similarly, risks associated with anaesthesia were understood by 78% in Group A versus 24% in Group B (P < 0.001). Misconceptions related to anaesthesia were cleared in 54% patients in Group A as against 16% in Group B (P < 0.001) [Table 1].
Figure 1.
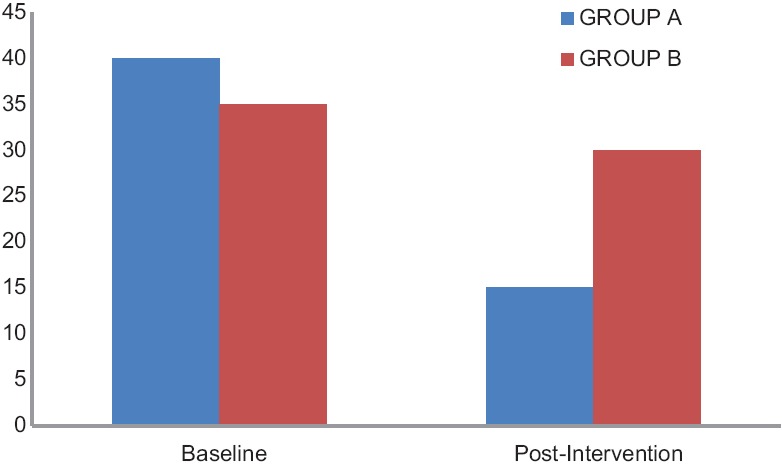
Visual analogue scale score
Table 1.
Information gained after intervention
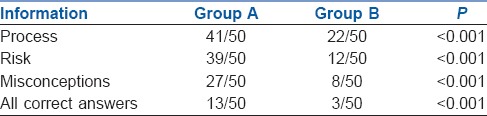
Overall, Group A had more transfer of information than Group B with 26% patients in Group A getting all correct answers as compared to only 6% patients in Group B (P < 0.001) [Table 1].
DISCUSSION
Pre-operative education results in beneficial outcomes for the patient by reducing anxiety. In this study, we found that giving information through a booklet during the pre-operative period helped in the reduction of the anxiety levels of patients undergoing elective surgery [Figure 1]. A systematic review of randomised control trial of media-based interventions also found that anxiety levels were reduced in subjects receiving printed information compared to those receiving no intervention.[2] The ‘state-trait anxiety inventory’ (STAI) is the ‘gold standard’ for measuring pre-operative anxiety.[4] However, the test procedure is rather complex and difficult to use in clinical practice. The VAS score for anxiety is simple, sensitive and correlates well with STAI (correlation coefficient r of 0.62-0.84) in the perioperative setting.[5,6] Hence, we used the VAS score for anxiety measurement.
We decided to give the information booklet to patients the evening before surgery, to ensure sufficient time to read and reflect on the information gained. Inglis et al. found that providing information on the night before surgery did not increase patient's level of anxiety, whereas Arellano et al. found a small reduction in state of anxiety when patients received information immediately before surgery compared with those who received information 1-week prior to surgery.[7]
We observed that giving written information increased knowledge about risk and process while dispelling misconceptions of anaesthesia. Many studies agree that interview alone is an insufficient technique for imparting knowledge and alternative methods to help information gain are required.[2,3] With the help of our questionnaire, we found that the recall of risk, process and misconceptions of anaesthesia was better in the booklet group. Around 26% patients in Group A got all correct answers as compared to only 6% in Group B. This was similar to findings from other studies that used an information brochure pre-operatively.[2,8]
Although this study confirms the benefit of an information booklet, knowledge of English restricted the study population. Translation of booklet into various languages will allow unbiased comparison of the two interventions.
CONCLUSION
There is no uniform standardisation of pre-operative consultation in practice; patient information material may improve patient understanding about anaesthesia and reduce pre-operative anxiety. For a valid informed consent, the pre-operative visit continues to be irreplaceable to provide patient specific information.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jlala HA, French JL, Foxall GL, Hardman JG, Bedforth NM. Effect of preoperative multimedia information on perioperative anxiety in patients undergoing procedures under regional anaesthesia. Br J Anaesth. 2010;104:369–74. doi: 10.1093/bja/aeq002. [DOI] [PubMed] [Google Scholar]
- 2.Lee A, Chui PT, Gin T. Educating patients about anesthesia: A systematic review of randomized controlled trials of media-based interventions. Anesth Analg. 2003;96:1424–31. doi: 10.1213/01.ANE.0000055806.93400.93. [DOI] [PubMed] [Google Scholar]
- 3.Swinhoe CF, Groves ER. Patients’ knowledge of anaesthetic practice and the rôle of anaesthetists. Anaesthesia. 1994;49:165–6. doi: 10.1111/j.1365-2044.1994.tb03380.x. [DOI] [PubMed] [Google Scholar]
- 4.Fisher PL, Durham RC. Recovery rates in generalized anxiety disorder following psychological therapy: An analysis of clinically significant change in the STAI-T across outcome studies since 1990. Psychol Med. 1999;29:1425–34. doi: 10.1017/s0033291799001336. [DOI] [PubMed] [Google Scholar]
- 5.Kindler CH, Harms C, Amsler F, Ihde-Scholl T, Scheidegger D. The visual analog scale allows effective measurement of preoperative anxiety and detection of patients’ anesthetic concerns. Anesth Analg. 2000;90:706–12. doi: 10.1097/00000539-200003000-00036. [DOI] [PubMed] [Google Scholar]
- 6.Boker A, Brownell L, Donen N. The Amsterdam preoperative anxiety and information scale provides a simple and reliable measure of preoperative anxiety. Can J Anaesth. 2002;49:792–8. doi: 10.1007/BF03017410. [DOI] [PubMed] [Google Scholar]
- 7.Arellano R, Cruise C, Chung F. Timing of the anesthetist's preoperative outpatient interview. Anesth Analg. 1989;68:645–8. [PubMed] [Google Scholar]
- 8.Snyder-Ramos SA, Seintsch H, Böttiger BW, Motsch J, Martin E, Bauer M. Patient satisfaction and information gain after the preanesthetic visit: A comparison of face-to-face interview, brochure, and video. Anesth Analg. 2005;100:1753–8. doi: 10.1213/01.ANE.0000153010.49776.E5. [DOI] [PubMed] [Google Scholar]


