There is a need for clear priorities to prevent major work-related health risks and to identify solutions for action. Obviously, cancer at work is the biggest individual threat when looking at the number of deaths in the developed world and this serious and preventable disease is rapidly becoming the biggest killer at places of work in most countries in the world. We can and should have a more ambitious target: to eliminate occupational cancer. This should be achieved via a stepwise and gradual reduction of occupational exposures, in particular, to carcinogens, substances and associated processes, arrangements and jobs that are known to cause or contribute to work-related cancers. This needs wide international collaboration to recognize and market new and evidence-based policies and practices that have been shown to produce results.
What We Know about Occupational Cancer
| ∙ | ILO estimates 666,000 deaths that are caused by occupational cancer globally every year, double of that for occupational accidents; |
| ∙ | In the EU28 102,500 deaths take place, twenty times of that caused by occupational accidents; |
| ∙ | Biggest killer at work in High Income Countries (WHO Classification) including the EU, Japan and others; |
| ∙ | Lung cancer counts for 54–75% of occupational cancer. Occupational exposures cause 5.3–8.4% of all cancers, and among men 17–29% of all lung cancer deaths according to best estimates; |
| ∙ | Asbestos counts for 55–85% of lung cancer, and causes other cancers and asbestos related diseases today, which could have been prevented in the past; |
| ∙ | Cancer and occupational cancer mortality increases due to growing life expectancy and gradual reduction of other causes of death, such as communicable diseases and injuries, work exposures cause cancers that have high case mortality rate, such as lung cancer; |
| ∙ | 10 most important occupational carcinogens count for around 85% of all occupational deaths. |
Estimates of Cancer
Cancer kills globally 8.2 million people and 14 million new cancers are detected every year according to WHO/IARC. The mortality will increase 78% and incidence 70% by the year 2035. In the European Union, EU28, there were a predicted 1,314 million cancer deaths in 2013. While cancer is a multifactorial disease and some causal factors are difficult to modify, it is clear that cancers caused by work can be prevented by reducing or eliminating the exposures leading to the disease. In fact these cancers are the easiest ones to tackle, “such risks can be usually reduced or even eliminated”1), and ethically the right way to go ahead.
So What are the Cancers at Work and What is the Burden of Occupational Cancer?
Doll and Peto estimated in 1981 that 4% of all cancer deaths and 12.5% of lung cancer deaths were caused by work. These were underestimates in the light of present knowledge and gradually increasing number of recognised carcinogens by IARC1, 2). About 17–29% of all lung cancer among men is due to occupational exposure, and lung cancer accounted for 54–75% of occupational cancer2).
The latest global data released by the ILO indicate that some 666,000 fatal work-related cancers occur every year, based on information from 2010 and 20113). Past records from 2008 gave an estimation of 610,000 occupational cancer deaths globally4).
In a UK study recently published in BJC5) Rushton and others estimated 8,010 deaths from occupational cancer annually in Britain alone. The French President François Hollande launched an action plan saying: “There are work-related cancers, which hit at least 14,000 people each year. Two million are regularly exposed to carcinogenic chemicals (in France)”i.
Occupational Cancer in Industrialised Countries
The ILO Global Estimates and corresponding attributable fractions in “High Income Countries” of WHO classification, which includes USA and Canada, USA, most European Union countries, Japan, Australia, New Zealand and Singapore among others, came to 212,000 deaths caused by malignant neoplasms at work (occupational cancers) based on WHO mortality data in 2011. In a recent report made for the Greek Presidency Conference on Occupational Safety and Health in 2014 the EU share of this was 102,500 deaths6). Latest data released in the ILO-ISSA World Congress in August 2014 confirm this estimate in the EU28 based on 2010 and 2011 data from WHO and ILO3).
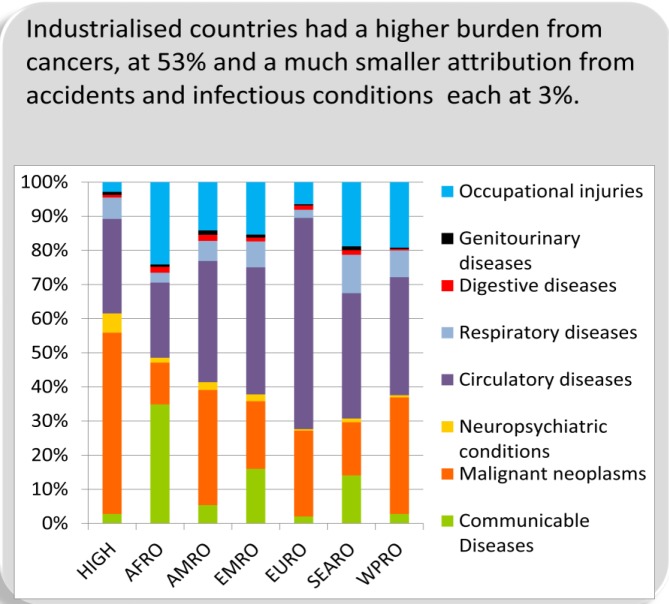
Previous global estimates on occupational cancers by the ILO established that 32% of the deaths in the world related to work are associated with cancers7). However, occupational cancers are quite rapidly globalized and in many industrialising countries, the percentage of occupational cancer deaths among all work-related deaths approaches that of the high-income countries; e.g. in the European Union occupational cancer deaths is already at 53% of all work-related deaths4). The standardised incidence rate (SIR), Relative Risk (RR), and consequently the attributable fraction, morbidity and mortality from various cancer forms varies widely between occupations as shown in the study covering 15 million people and 45 yr follow up period using Nordic cancer registers8).
There is an urgent need to harmonise the estimation methods by various bodies and to resolve these issues. However, experience shows that the more we’ll study occupational carcinogens, mutagens and reprotoxic substances, the higher will be the estimates of negative outcomes. Further research cannot be an excuse for doing nothing, with today’s solutions, most or all of such deaths and lost life years can be eliminated.
Exposures to Occupational Carcinogens, Processes and Jobs
There are 179 agents (chemicals or exposure circumstances) classified by the International Agency for Research on Cancer (IARC in Lyon, France) as known or probable human carcinogens, Groups 1 and 2a, respectively. There are another 285 agents classified as possible human carcinogens, Group 2b9). A large proportion of these agents will be found at work or present in the workplace, such as environmental tobacco smoke. Indications exist that other substances, agents and processes are expected to be carcinogenic as well, as demonstrated by recent important additions to the list, e.g. diesel engine exhaust, and possibility for endocrine disruptors playing a role in hormone related cancers. The gender factors should be further studied as well10). The IARC list of classified carcinogens need to be continually revised and the precautionary principle applied.
A hierarchy of elimination and control protocols exist to protect workers from exposure to these agents and in theory, occupational cancer could be completely preventable. Yet, cases of work-related cancer are still occurring. The proportion of cancer deaths attributable to occupational causes in Finland was 8.3% (13.2% percent among males), and in the UK it was 5.3% (eight percent among males) which equates to 8,010 cancer deaths and nearly 14,000 cancer cases8). Current estimates of occupationally related cancers result from exposures to hazardous agents decades ago, but hazardous substances continue to be found in the workplace and pose a risk for future disease. Some substances such as silica and diesel engine exhaust are process-generated while others such as shift-work are emerging risks which need to become better managed at places of work and regulated under occupational safety and health jurisdiction.
In order to have a comprehensive picture of occupational exposures, cancer exposure registers (CAREX) and job exposure matrices (JEM) have been established in many countries and regions, such as those in Finland, Canada11) and the EU12, 13).
Occupational carcinogens affect 1 in 5 workers in the EU based on EU CAREX (Carcinogen exposure database), or 23% of those employed are exposed to carcinogens14). The corresponding figure according to a recent study in Canada was 43%15) and 37.6% in Australia16). A larger group of workers exposed at lower levels and with a lower risk of disease will also contribute to the overall disease burden17). Exposures must be controlled by measures that are proportional to the risk of disease. It is therefore important to know the proportion of workers exposed to hazardous substances and how exposure levels and patterns differ among those exposed in order to explicitly target the areas that are contributing most to disease and determine where priority action is required. The IRSST Institute in Quebec has launched very practical publications to identify carcinogens at work18).
Fig. 1.
Burden caused by cancer and other work-related diseases by WHO regions, released in 2014. Total number of workplace fatalities was 2.3 million. HIGH: High income countries including, among others, the EU and Japan, AFRO: African Region (low-and middle-income countries), AMRO: Region of the Americas (low-and middle-income countries), EMRO: Eastern Mediterranean Region (low-and middle-income countries), EURO: European Region (low-and middleincome countries), SEARO: South-East Asia Region (low-and middle-income countries), WPRO: Western Pacific Region (low-and middle-income countries)
Asbestos Exposure is the Biggest Killer
Likely underestimation of the magnitude of asbestos-related ill-health
On asbestos-related mortality, some years ago WHO made an estimate of 107,000 cases19) whilst the ILO and the EU estimated this as 100,00020) and 112,000 deaths21) per year, respectively. Using mesothelioma as a proxy for asbestos exposure, McCormack et al. have shown that depending on the type of asbestos used, the number of lung cancers in relation to mesothelioma is between 2–10 times that of mesothelioma cases, the mid-point being 6.1 lung cancers for every mesothelioma death22).
A comprehensive picture of asbestos exposures causing lung cancers, mesothelioma and other cancers, such as larynx, ovary and possibly colorectal cancers should be properly investigated using CAREX exposure estimates and job exposure matrices.
However, this cannot be realistically carried out in every country soon. A reasonable proxy for asbestos exposure will be the asbestos consumption in tons of asbestos used in a country or region. The consumption of asbestos has been surprisingly similar in most countries and some 2/3 of asbestos has been used for asbestos-cement products, such as roofing, wall materials and water pipes. The rest of asbestos has been used for brake pads, heat insulation, gaskets etc. International comparison has shown that, in average, every 170 tons of asbestos used in a country causes one mesothelioma death23).
Using a similar proxy as above on the correlation with asbestos consumption in tons and asbestos-related lung cancer deaths (ARLC) as for mesothelioma, the estimate, based on RR= 2.3 for asbestos-related lung cancer and attributable fraction, AF = 13.8% for males, 2.2% for females, the ratio between mesothelioma and ARLC will be 1:3.524) still well below the average 1:6.1 given by McCormack et al. As a result every 48 tons of asbestos consumption causes one ARLC death.
In the European Union the combined number of deaths will amount to 47,000 lung cancer and mesothelioma deaths caused by asbestos. This still misses other work-related cancers caused by asbestos, such as larynx and ovary, and possibly stomach, colorectal and pharynx cancers.
Japan has an equivalent annual crude mortality rate for mesothelioma as most European Union countries and USA. This is between approximately 10–15 mesothelioma deaths per million population. As a result there may be more than 3,500 mesothelioma deaths and possibly more than 12,000 asbestos-related lung cancer deaths in Japan.
One should keep in mind that it is not just the exposure in the past that creates problems. Asbestos, particular, will be present in our work life for decades in the future requiring proper regulatory measures and management of existing structures, devices and equipment, and removal operations. What is more saddening is the fact that annually some 2 million tons of asbestos are continuously consumed, mostly in Asia.
What Would be the Advice for Policy and Practice
1. We need to influence and advocate for measurable and continuous reduction of exposures caused by work globally and across regions in order to eliminate occupational cancer.
2. An international programme should be launched on the “Elimination of Occupational Cancer” following the WHO model of elimination of smallpox from the world and present programmes to “eliminate asbestos-related diseases”, and to “eliminate silicosis”.
3. Prioritize substitution of carcinogenic, mutagenic and reprotoxic substances in the authorization and restriction processes. Furthermore, revising the worker protection legislation, setting binding occupational exposure limits and ensuring enforcement related to specific exposure of carcinogens, such as crystalline silica, diesel exhaust and wood dust. A comprehensive set of conclusions and recommendations is given in the European Risk Observatory Report on Exposure to carcinogens and work-related cancer25).
Immediate Outputs and Methods
Present unified scientific evidence of the magnitude of the problems, levels of exposures, number of workers exposed, and produce credible data on predicted negative outcomes.
Provide recommendations on evidence-based solutions that are adaptable to different kinds of circumstances, cultures, countries, sectors and sizes of workplaces.
Share findings via well prepared reports and articles published in a high impact journals
Mobilize institutions globally to act on elimination of work-related cancer and expand this action gradually through the International Labour Organization, ILO and its Occupational Safety and Health Flagship programme being established, and through WHO and its ‘collaboration centres’ network, supporting IARC efforts in this field, and mobilising global action through the national stakeholders.
Conclusions for Zero Cancer at Work
The asbestos exposure is a demonstration how poor and slow decisions in the past related to exposures to carcinogens had created serious epidemics. More ambitious targets for the future are needed since a large percentage of workers are still exposed to carcinogens even in countries where asbestos has been banned.
International cooperation can help a lot to avoid losing time26). If we want to promote an ambitious program for “zero work-related cancer”, the cooperation between WHO, ILO and other institutions is crucial. It would be vital to avoid exporting the risks from the developed countries to developing countries.
Footnotes
An update of the estimates of cancers attributable to occupational exposure in France, using tools developed by the French institute for public health surveillance, recently revised upwards the number of cases connected to an exposure to asbestos: mostly due to the inclusion of new cancers, such as laryngeal and ovarian cancers.
References
- 1.Doll R, Peto R. (1981) The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst 66, 1191–308. [PubMed] [Google Scholar]
- 2.Straif K. (2008) The burden of occupational cancer. Occup Environ Med 65, 787–8. [DOI] [PubMed] [Google Scholar]
- 3.Nenonen N, Hämäläinen P, Takala J, Saarela KL, Lim SL, Lim GK, Manickam K.GLOBAL ESTIMATES OF OCCUPATIONAL ACCIDENTS AND FATAL WORK-RELATED DISEASES IN 2014 BASED ON 2010 AND 2011 DATA, Report to the ILO http://goo.gl/UlZorD and http://goo.gl/tN7XDn Tampere, Singapore, ILO Geneva 2014.
- 4.Takala J, Hämäläinen P, Saarela KL, Loke YY, Manickam K, Tan WJ, Heng P, Tjong C, Lim GK, Lim S, Gan S. (2014) Global Estimates of the Burden of Injury and Illness at Work in 2012. J Occup Environ Hyg 11, 326–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rushton L, Sally J Hutchings, Lea Fortunato, Charlotte Young, Gareth S Evans, Terry Brown, Ruth Bevan, Rebecca Slack, Phillip Holmes, Sanjeev Bagga, John W Cherrie and Martie Van Tongeren. Occupational cancer burden in Great Britain Br J Cancer 107: S3-S7; doi: 10.1038/bjc.2012.112 . http://www.nature.com/bjc/journal/v107/n1s/index.html. Accessed May 16, 2013. [DOI] [PMC free article] [PubMed]
- 6.Takala J. Work-related Illnesses, Identification, Causal Factors and Prevention “Safe Work—Healthy Work—or Life”. Greek EU Presidency Conference: www.gr2014.eu/sites/default/files/Work-related%20Illnesses%20Identification,%20Causal%20Factors%20and%20Prevention%20“Safe%20Work%20-%20Healthy%20Work%20–%20For%20Life”.pdf. Accessed December 15, 2014.
- 7.Takala J. Introductory report: Decent work − Safe work: XVIIth World Congress on Safety and Health at Work. Geneva: ILO, 2005, http://www.ilo.org/public/english/region/eurpro/moscow/areas/safety/docs/worldcongressreporteng.pdf. Accessed March 17, 2014.
- 8.Pukkala E, Matinsen JI, Lynge E, Gunnarsdottir HK, Sparén P, Tryggvadottir L, Weiderpass E.Kjaerheim K Occupation and cancer − follow-up of 15 million people in five Nordic countries. Acta Oncologica; 48: 646–790. Available from: http://informahealthcare.com/doi/pdf/10.1080/02841860902913546. Accessed March, 24, 2014. [DOI] [PubMed]
- 9.http://monographs.iarc.fr/ENG/Classification/index.php. Accessed 17 March 17, 2014.
- 10.Anne-Marie M, Tony M, Laurent V.Preventing Work Cancers, A workplace health priority, European Trade Union Institute, Bussels, 2014. http://www.etui.org/Publications2/Guides/Preventing-work-cancers.-A-workplace-health-priority.
- 11.CAREX Canadasee http://www.carexcanada.ca/en/occupational_approach/. Accessed 17 March 17, 2014.
- 12.Timo K. Burden or work-related cancer in Finland and two exposure information systems (CAREX and FINJEM) including estimates of occupational exposure to carcinogens. EU-OSHA Seminar, Berlin 2012, https://osha.europa.eu/en/seminars/workshop-on-carcinogens-and-work-related-cancer/speech-venues/session-a-methods-to-assess-exposure-to-carcinogens-and-the-work-related-cancer-burden/the-burden-of-work-related-cancer-in-finland-and-two-exposure-information-systems-carex-and-finjem-including-estimates-on-occupational-exposure-to-carcinogens and.
- 13.Kauppinen T, Toikkanen J, Pedersen D, Young R, Ahrens W, Boffetta P, Hansen J, Kromhout H, Maqueda Blasco J, Mirabelli D, de la Orden-Rivera V, Pannett B, Plato N, Savela A, Vincent R, Kogevinas M. (2000) Occupational exposure to carcinogens in the European Union. Occup Environ Med 57, 10–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kauppinen T, Toikkanen J, Pedersen D, Young R, Ahrens W, Boffetta P, Hansen J, Kromhout H, Maqueda Blasco J, Mirabelli D, de la Orden-Rivera V, Pannett B, Plato N, Savela A, Vincent R, Kogevinas M. (2000) Occupational exposure to carcinogens in the European Union. Occup Environ Med 57, 10–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peters CE, Ge CB, Hall AL, Davies HW, Demers PA. (2015) CAREX Canada: an enhanced model for assessing occupational carcinogen exposure. Occup Environ Med 72, 64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carey RN, Driscoll TR, Peters S, Glass DC, Reid A, Benke G, Fritschi L. (2014) Estimated prevalence of exposure to occupational carcinogens in Australia (2011-2012). Occup Environ Med 71, 55–62. [DOI] [PubMed] [Google Scholar]
- 17.Straif K. (2012) Estimating the burden of occupational cancer as a strategic step to prevention. Br J Cancer 107 Suppl 1, S1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.IRSSTARE THERE CARCINOGENS IN YOUR WORKPLACE? / Y A-T-IL DES CANCÉROGÈNS DANS VOTRE MILIEU DE TRAVAIL? http://www.irsst.qc.ca/media/documents/PubIRSST/RG-796.pdf and http://www.irsst.qc.ca/media/documents/PubIRSST/RG-790.pdf. Accessed April 16, 2014.
- 19.WHO http://www.who.int/ipcs/assessment/public_health/asbestos/en/.
- 20.ILO: www.ilo.org/global/about-the-ilo/newsroom/features/WCMS_076282/lang--en/index.htm.
- 21.http://www.efbww.org/pdfs/Presentation%20Mr%20Takala.pdf. Accessed March 17, 2014.
- 22. McCormack V, Peto J, Byrnes G, Straif K, Boffetta P.Estimating the asbestos-related lung cancer burden from mesothelioma mortality. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3273352/. Accessed March 17, 2014. [DOI] [PMC free article] [PubMed]
- 23.Tossavainen A. Global use of asbestos and the incidence of mesothelioma. Int J Occup Environ Health. 2004. Jan-Mar;10(1):22–5. [DOI] [PubMed]
- 24.Nurminen M, Karjalainen A. (2001) Epidemiologic estimate of the proportion of fatalities related to occupational factors in Finland. Scand J Work Environ Health 27, 161–213 http://www.sjweh.fi/show_abstract.php?abstract_id=605. [DOI] [PubMed] [Google Scholar]
- 25.European Agency for Safety and Health at Work European Risk Observatory Report, Exposure to carcinogens and work-related cancer, A review of assessment methods. ISSN 1831–9343. EU-OSHA 2014, 160 p, Luxembourg and Bilbao. Available at https://osha.europa.eu/en/publications/reports/report-soar-work-related-cancer. Accessed January 24, 2015.
- 26.Campaign IOSH .“No Time To Lose” launched in November 2014. http://www.notimetolose.org.uk/News-and-events/Occupational-cancer-sufferers-back-new-IOSH-campaign.aspx. Accessed Dec ember 15, 2014.