Abstract
Background
The benefit of preseason concussion education on athletes’ knowledge, attitudes, and behaviors is unclear. The purpose of the study was to determine the influence of preseason concussion education on knowledge and self-reported attitudes and reporting behaviors. We hypothesized that preseason education would lead to better knowledge and self-reported attitudes and better reporting of concussion symptoms during the season.
Methods
Prospective cohort comparing the benefits of a preseason lectured-based concussion education session at one high school with a control school. Participants included males and females age 13–18 years from two community high schools who were participating in higher concussion risk, fall or winter sports (football, soccer, wrestling, and basketball). The education school and control school included 234 and 262 participants, respectively. Outcomes were a pre- and post-season survey assessing knowledge and self-reported attitudes about concussions and an end of season questionnaire assessing concussion reporting behaviors during the season.
Results
Total scores on the combined (p<.0001), knowledge-based (p=.016), and behavioral-based (p<.0001) questions demonstrated statistically significant improvement in the education group. Scores peakedimmediately post education, but dissipated at the end of the season. There was a lower proportion in the education school (72%) compared to the control school (88%) that reported continued play despite having concussion symptoms during the season (p=.025). A similar proportion of athletes diagnosed with concussion during the season in the education (27%) and control schools (23%) reported returning to play before symptoms resolved (p=.81).
Conclusion
These findings suggest that a didactic-based preseason concussion education likely has minimal benefits. Other factors besides knowledge are likely influencing student-athlete concussion reporting behavior. Future research focused on changing the culture of concussion reporting is needed.
Keywords: Concussion, Education, Athlete, Adolescent, Brain Injury
Background
Traumatic brain injuries (TBI) are a leading cause of acquired disability in children. Approximately 1.6–3.8 million TBIs related to sports and recreation occur annually in the US.(1) Most TBIs are classified as mild (mTBI) and are often referred to as concussions.(2, 3) Improper management of concussions may lead to long-term consequences.(4–7) Individuals with a history of concussion are more likely to sustain a second concussion, and there are cumulative effects associated with multiple injuries.(8, 9) Repeated concussions can result in permanent injury or even death.(8, 10–14) If athletes with concussions are diagnosed and managed appropriately, most recover fully.(3, 13, 15, 16)
Concussion consensus statements recommend that any child who suffers a concussion be removed from play immediately and not return that day to prevent repeated concussions and more severe brain injury.(15–18) A first step towards prevention of secondary injuries and complications is to provide concussion education on the signs and symptoms of injury to improve recognition of injury by athletes, parents, and coaches. All states have passed legislation requiring coaches, parents, and, on occasion, athletes, to receive concussion education. Through the “Heads Up” program, developed by the Centers for Disease Control and Prevention (CDC), education provided to parents, coaches, and physicians has improved knowledge of concussion signs and symptoms and improved prevention and management practices;(19–21) however, legislation targeted at coaches is unlikely to lead to changes in athlete attitudes on reporting concussion.(22)
In general, athletes underreport concussions.(23–29) The most common reasons for not reporting are athletes did not realize they suffered a concussion, athletes did not think the injury was serious enough to warrant medical attention and believe the injury posed little danger to them, motivation not to be withheld from competition, and lack of awareness in general about concussions, thus highlighting the importance of providing concussion education to adolescent athletes.(24, 28, 30) Currently, there is a paucity of research related to the impact of education on reporting of concussions and removing oneself from athletic participation. In a cross-sectional survey of high school athletes, better knowledge about concussion was associated with better reporting of concussion symptoms.(31) Another study of high school soccer players provided with education on concussion reported that they were more likely to report their concussion to a coach or athletic trainer; however, limitations to this study were the small sample size (n=60), evaluation of only high school soccer athletes, and it did not examine the actual injury reporting rates.(32) Little prior work has evaluated whether adolescent athletes who receive preseason education about concussions retain this information at the end of the season or whether attitudes about reporting concussions change with education.
Since many states recommend providing pre-season education to student athletes about concussion, the objective of this study was to assess whether a brief, preseason, didactic education program would improve adolescents’ knowledge about concussion signs and symptoms, their attitudes toward reporting concussions, and their reporting of concussion symptoms during the season. We hypothesized that preseason education would lead to better knowledge and self-reported attitudes and better reporting of concussion symptoms during the season compared to a control group.
Methods
Design
This was a community-based cohort study of high school athletes followed over the course of one sports season that received concussion-specific educational compared to a control cohort. Institutional review board (IRB) approval was obtained prior to initiation of the study.
Participants
Participants were recruited from two large, public suburban high schools in Cincinnati, OH that are part of the same school district as previously described (33). This particular school district was approached for participation because the district included two, relatively large, high schools of similar size and demographics for comparison. One school was arbitrarily designated by the research team as the education school and the other as the comparison school. Each participating high school had an enrollment of approximately 2,500 students. The racial and ethnic composition of the participating schools was 74.5% White/non-Hispanic, 10.3% Black, 5.9% Asian or Pacific Islander, 4.8% Hispanic, 4.4% Multiracial, and 0.2% American Indian or Alaskan Native (33, 34). Recruitment was done during fall and winter sports preseason training from August through December of 2012 as previously described (33). Sports included football (boys only), soccer (boys and girls), basketball (boys and girls), and wrestling (boys and girls [1 female participant]). A letter describing the study was provided to each participant and his/her parent or guardian. The participants and their parents were given the option to decline participation by returning an opt-out form. If the opt-out form was not returned, consent was implied and participating athletes were enrolled. The need for signed consent was waived by the IRB. Participants were excluded if the opt-out form was returned or if they were absent the day of the educational session.
Measures
As previously described (33), a questionnaire was developed to assess an athlete’s knowledge of concussion and attitudes / behaviors about their willingness to report or stop activity after sustaining a concussion and other injuries during play. The knowledge-based questions were true/false and queried about the definition of a concussion, symptoms, typical course of recovery, and current recommendations for return to activities. The self-reported behavior and attitudes questions consisted of statements that participants answered using choices of never, sometimes, or always. Correct answers on the behavior question were either “never” or “always” depending on the wording of the question. “Sometimes” was given as a distractor choice to capture participants that may not endorse “always” or “never” in each situation. Questions for this instrument were adapted from the CDC heads up program(20), questions used in a previous study evaluating concussion knowledge and preventative practices in soccer players (32), and a concussion knowledge questionnaire used in the state of Arizona to assess concussion knowledge of all high school athletes.(35) The knowledge-based questions consisted of 13 true/false concussion symptom statements and 12 additional questions (25 total knowledge-based questions), and the behavioral/attitudes section consisted of 11 questions. The survey was written at a 6th grade level. The questionnaire was developed through input by a group of physicians and athletic trainers who care clinically for children after concussions. The questionnaire was also given, in a group setting, to one high school football team that was not involved in the current study after practice to ensure question clarity, ease of completion, and comfort with responding. The athletes did not report problems with understanding or answering the questions; therefore, no changes were made to the questionnaire based on feedback from this group of athletes.
The two outcomes assessed were changes in scores on knowledge and self-reported behaviors and attitudes questions at the end of the season and concussion symptom reporting behaviors during the season. Concussion reporting behaviors were measured by an end of the season questionnaire where participants were asked if they developed symptoms of concussion or were diagnosed with a concussion during the season by their athletic trainer or other healthcare provided and if they continued playing or returned to play before their symptoms resolved. Questions about demographics, previous education about concussions, and prior history of concussion were also included in the data collection.
Study Procedures
The survey was administered by the study research coordinator (C.S.) during the preseason of the respective sport for all participants, immediately after the education intervention in the educational school, and at the end of the season for both schools. All survey questions were completed with paper and pencil, and results were entered into a secure, de-identified, database. Both groups also received baseline computerized neuropsychological testing. The neuropsychological testing was not used as an outcome but was included as an incentive for participation. Through consultation with each school’s athletic trainer, questionnaires were administered at a convenient time during the preseason after cuts had been made. The questionnaire was distributed by the study’s research coordinator during a break in each team’s preseason training. The research coordinator was available to answer participant questions about the survey.
In the education school, the research coordinator provided a 20 minute educational lecture to participants immediately after they completed the preseason survey. The educational intervention was designed to be similar in nature to educational programs commonly being used to comply with the requirement of providing pre-season concussion education to student athletes. The lecture included content on the definition of concussion, signs and symptoms associated with concussions, current concussion guidelines, and return to play recommendations based on prior concussion consensus statements.(17, 36) The lecture also included information on the risk of second impact syndrome and potential chronic problems that could develop after concussion. The educational content in the lecture was tailored to information needed to answer knowledge and attitude survey questions correctly. The educational lecture was delivered as a scripted PowerPoint lecture in a classroom setting and limited to groups of 20–30 participants. Throughout and after the lecture there were opportunities for participants to ask questions about the information presented. After the lecture, the educational school participants completed an immediate post-education survey and returned it to the research coordinator.
Some potential participants may have been absent or unavailable during the testing. In accordance with IRB approval, information on these potential participants is not available because the study team was blinded to identifiable information of participants who did not complete the initial survey. Demographics are only available for individuals that completed the survey at baseline and follow-up. All surveys were anonymous. A master log was created of participants that completed the questionnaire to ensure that individuals that participated in more than one sport (e.g., football and wrestling) did not complete the survey twice (e.g., once during their fall sport and once during their winter sport). Additionally, the master log was used to assist the athletic trainers at each school with identification of participants that needed to complete postseason testing. In consultation with each school’s athletic trainer, postseason testing was completed for all sports involved. We attempted to complete all postseason testing on one day for each team involved in the study; however, additional testing days were scheduled as needed to capture as many participants as possible.
Analysis
Descriptive statistics were used to characterize the baseline demographics of the population, prior concussion education, and results of the questionnaire. T-test and Chi Square analysis was used to compare descriptive variables between the education and control school. Repeated measures analysis using the Statistical Analysis System (SAS) mixed model procedure was used to compare postseason knowledge and behavior and attitudes scores between schools. Both unadjusted and adjusted models were evaluated. Independent variables included in the unadjusted models were school (education or control school), timing of survey (preseason or postseason), and the interaction term of timing of survey and school. The timing of survey and school interaction term was the primary variable of interest to evaluate for differences between schools at the end of the season on the survey questions. In addition to the variables used in the unadjusted models, adjusted models were developed that controlled for age, gender, sport, and history of prior concussion education. Chi-square analysis was used to compare the proportion of participants between the education and control groups who developed symptoms of concussion during the season and continued playing and reported being diagnosed with a concussion during season and returned to play before symptoms resolved. A p-value of <0.05 was used to define statistical significance.
Results
Participant demographics
There were 234 participants who completed the preseason questionnaire in the education school and 262 in the control school. No potential participants returned the opt-out form. Demographic characteristics of the participants are presented in Table 1. More participants in the education school were male (82.91% versus 75.52%). The mean age was similar between the two schools (15.38 versus 15.46 years). The majority of participants played football, with a slightly higher percentage of participants playing football (47.55% versus 38.55%) and lower proportion playing basketball in the education school (13.25% versus 22.14%). More participants in the control school reported being taught about concussions previously (78.24% versus 35.90%).
Table 1.
Baseline characteristics of study participants
| Demographics: n(%) | Education School n=234(47.18%) |
Control School n=262(52.82%) |
|
|---|---|---|---|
| Male* | 194 (82.91) | 190 (75.52) | |
| Age | |||
| 13 Years | 6(2.56) | 4(1.53) | |
| 14 Years | 51(21.79) | 64(24.43) | |
| 15 Years | 73(31.20) | 74(28.24) | |
| 16 Years | 60(25.64) | 54(20.61) | |
| 17 Years | 41(17.52) | 59(22.52) | |
| 18 Years | 3(1.28) | 7(2.67) | |
| Sport** | |||
| Football | 111 (47.55) | 101 (38.55) | |
| Soccer | 57 (24.36) | 66 (25.19) | |
| Wrestling | 35 (14.96) | 37 (14.12) | |
| Basketball | 31 (13.25) | 58 (22.14) | |
| Season of Sport | |||
| Fall | 168 (71.79) | 167 (63.74) | |
| Grade Level | |||
| 9th grade | 71(30.34) | 81 (30.92) | |
| 10th grade | 63 (26.92) | 76(29.01) | |
| 11th grade | 60 (25.64) | 47(17.94) | |
| 12th grade | 40 (17.09) | 58 (22.14) | |
| History of Prior Concussion | 62 (26.50) | 54 (20.61) | |
| If yes, how many concussion have you had? | |||
| 1 | 42 (17.95) | 42 (16.03) | |
| 2 | 12 (5.13) | 9(3.44) | |
| >3 | 6(2.53) | 3 (1.14) | |
| Taught about concussions* | 84 (35.90%) | 205 (78.24) | |
| Source of concussion education*** | |||
| Family | 31(13.25) | 77(29.39) | |
| School | 31(13.25) | 104(39.69) | |
| Coach | 26(11.11) | 84(32.06) | |
| Athletic Trainer | 29(12.39) | 121(46.18) | |
| Doctor | 50(21.37) | 103(39.31) | |
| Other | 7(2.99) | 6(2.29) | |
Significant difference between education and control schools p<0.01
Significant difference between education and control schools p<0.05
Athletes could choose more than one option, so numbers are >100%
In the education school, 232 (99.1%) participants completed the immediate post-education questionnaire, and 167 (71.4%) participants completed the postseason questionnaire. In the control school, 222 (84.7%) participants completed the postseason questionnaire. There was no difference in those that completed the postseason questionnaire compared to the preseason questionnaire in terms of age (15.4[SD 1.2] versus 15.4[SD 1.2] years). A higher percentage of females completed the postseason questionnaire than males (90.2% versus 75.0%).
Questionnaire results
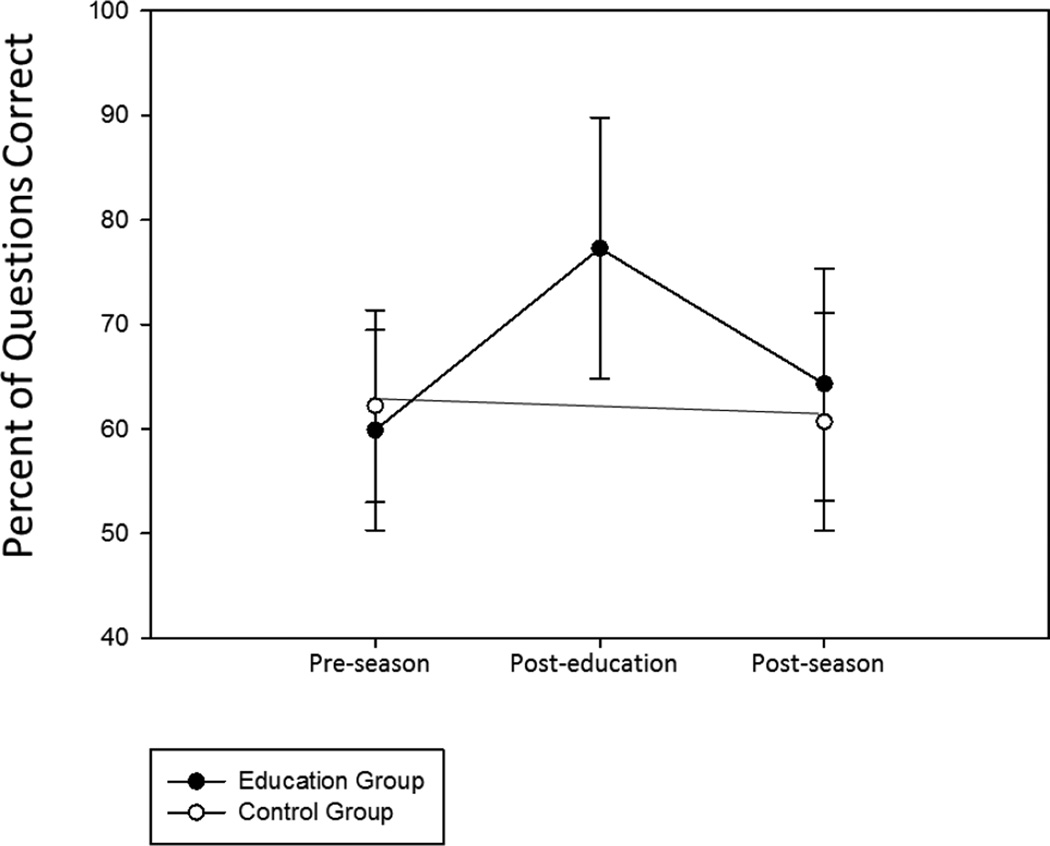
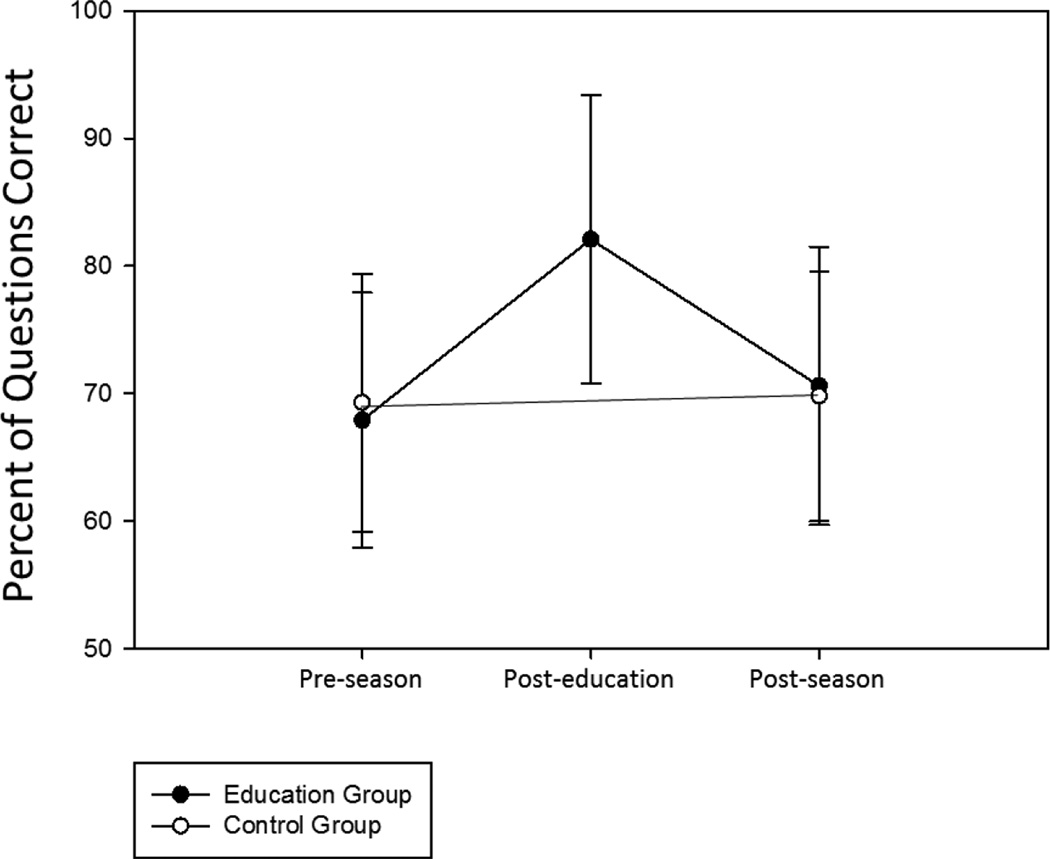
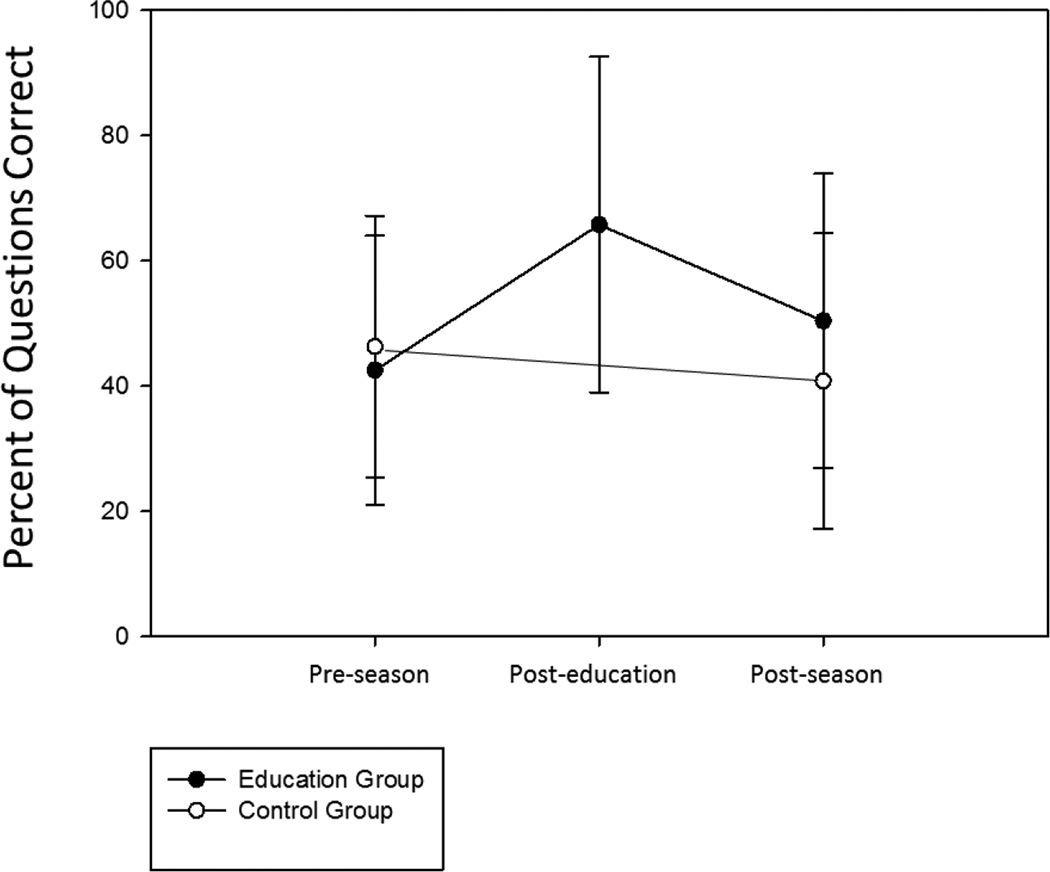
Individual questions on the survey and the percentage of participants answering each question correctly can be found in Table 2. The mean overall (combined knowledge and self-reported attitudes and behavior questions), knowledge-based, and behavior-based percent correct scores on the preseason, immediate post-education, and postseason questionnaires are depicted in Figures 1, 2, and 3. Total score, knowledge-based and behavior-based scores increased immediately post-education and then dissipated over time. Unadjusted and adjusted linear mixed models showed similar results, so only the adjusted models are reported. Total scores on all (p<.0001), knowledge-based (p=.02), and behavioral-based (p<.0001) questions demonstrated statistically significant improvement in the education group postseason compared to preseason (Table 3). However, immediate increases in scores dissipated over time.
Table 2.
Responses for the knowledge and behavior and attitude questions in control and education school
| Education School [n(% correct)] | Control School [n(% correct)] | |||||
|---|---|---|---|---|---|---|
| Questions type (correct response among choices of true/false or always, sometimes, never) |
Preseason (n=234) |
Post- Education (n=232) |
Postseason (n=167) |
Preseason (n=262) |
Postseason (n=222) |
|
| Knowledge questions | ||||||
| Check the following signs and symptoms that you believe a person is likely to experience AFTER a concussion | ||||||
| Emotional Changes (true) | 103(44.02) | 201(86.64) | 88(52.69) | 97(37.02) | 110(49.55) | |
| Neck Pain (false) | 98(41.88) | 124(53.45) | 50(29.94) | 130(49.62) | 73(32.88) | |
| Hallucinations (false) | 116(49.57) | 157(67.67) | 86(51.50) | 162(61.83) | 116(52.25) | |
| Vomiting (true) | 134(57.26) | 197(84.91) | 120(71.86) | 167(63.74) | 152(68.47) | |
| Tingling in Feet (false) | 159(67.95) | 167(71.98) | 97(58.08) | 191(72.90) | 140(63.06) | |
| Sensitivity to Noise (true) | 163(69.66) | 203(87.50) | 139(83.23) | 201(76.72) | 184(82.88) | |
| Nausea (true) | 177(75.64) | 216(94.40) | 144(86.22) | 214(81.68) | 194(87.39) | |
| Difficulty Concentrating (true) | 189(80.77) | 218(93.97) | 149(89.22) | 214(81.68) | 205(92.34) | |
| Sensitivity to Light (true) | 194(82.91) | 227(97.84) | 151(90.42) | 219(83.59) | 200(90.09) | |
| Slower Reaction Time (true) | 206(88.03) | 219(94.40) | 145(86.83) | 227(86.64) | 199(89.64) | |
| Difficulty Remembering (true) | 210(89.74) | 225(96.98) | 146(87.43) | 230(87.79) | 205(92.34) | |
| Confusion (true) | 212(90.60) | 227(97.84) | 147(88.02) | 234(89.31) | 202(90.99) | |
| Headache (true) | 225 (96.15) | 231 (99.57) | 157(94.01) | 252(96.18) | 216(97.30) | |
| A concussion is any injury to the head (false) | 63(26.92) | 115(49.57) | 47(28.14) | 56(21.37) | 51(22.97) | |
| An athlete should not continue to play sports while having a concussion (true) | 215(91.88) | 215(92.67) | 153(91.62) | 241(91.98) | 204(91.89) | |
| There is a higher risk of death if a second concussion occurs before the first one has healed (true) | 205(87.61) | 226(97.41) | 159(95.21) | 226(86.26) | 195(87.84) | |
| A person can only get a concussion if hit in the head (false) | 128(54.70) | 190(81.60) | 128(76.65) | 161(61.45) | 136(61.26) | |
| Imaging of the brain, such as MRI’s and CT scans, show visible physical damage to the brain after a concussion (false) | 46(19.66) | 131(56.47) | 55(32.93) | 46(17.56) | 35(15.77) | |
| If a person gets more than 3 concussions ever, they are not allowed to play sports ever again (false) | 169(72.22) | 190(81.90) | 114(68.26) | 193(73.66) | 154(69.37) | |
| If a person gets one concussion, they are more likely to get another (true) | 160(69.38) | 183(78.88) | 134(80.24) | 172(65.65) | 171(77.03) | |
| Being knocked out causes permanent damage to the brain (false) | 135(57.69) | 134(57.76) | 61(36.53) | 154(58.78) | 92(41.44) | |
| Majority of symptoms last for at least 1 month (false) | 110(47.01) | 141(60.78) | 56(33.53) | 105(40.08) | 81(36.49) | |
| Athletes must complete a gradual return to play before returning to sports (true) | 216(92.31) | 222(95.69) | 164(98.20) | 243(92.75) | 208(93.69) | |
| What is the current treatment for a person with a concussion There isn’t any (false) Play video games, watch movies, and text friends (false) Complete brain rest (true) Carry on with life as if nothing is wrong (false) | 176(75.21) | 202(87.07) | 138(82.63) | 218(83.21) | 185(38.22) | |
| Behavior and attitude questions | ||||||
| I would immediately tell a coach or athletic trainer that I had a headache, fogginess, or dizziness after getting hit in the head during a game or in practice (always) | 89(38.03) | 176(75.86) | 79(47.31) | 12(42.75) | 66(29.73) | |
| I would report having a concussion to a coach or athletic trainer if I knew it meant I would have to sit out a practice or two (always) | 107(45.73) | 179(77.16) | 92(55.09) | 145(55.34) | 90(40.54) | |
| I would report having a concussion to a coach or athletic trainer if I knew it meant I would have to sit out of a game (always) | 78(33.33) | 166(71.55) | 71(42.51) | 97(37.02) | 76(34.23) | |
| If my teammate told me they thought they had a concussion, I would report it to a coach or athletic trainer (always) | 80(34.09) | 176(75.86) | 82(49.10) | 112(42.75) | 71(31.98) | |
| I would continue playing a sport while having a headache that resulted from a minor bump to the head (never) | 21(8.97) | 72(11.37) | 26(15.57) | 17(6.49) | 16(7.21) | |
| I would play through any condition or injury in order for our team to win (never) | 16(6.84) | 75(32.22%) | 26(15.57%) | 24(9.16) | 29(13.06) | |
| I feel that it is important to be thoroughly evaluated by a medical personnel after an injury to make sure I recover completely (always) | 156(66.67) | 178(76.72) | 120(71.86) | 167(63.74) | 134(60.36) | |
| I feel that getting a concussion is not a big deal and actually proves that I’m tough (never) | 196(83.76) | 193(83.19) | 146(87.43) | 227(86.64) | 188(84.68) | |
| I feel that if a star athlete gets a concussion during a state tournament game they should return to the game since it could be their last one of the season (never) | 121(51.71) | 168(72.41) | 109(65.27) | 179(68.32) | 130(58.56) | |
| During a championship game you get injured. It hurts but doesn’t really hinder your ability to play. Knowing that it would result in a more severe injury, I would report the injury to a coach or athletic trainer (always) | 53(22.65) | 95(40.95) | 40(23.95) | 52(19.85) | 39(17.57) | |
| It is ok for an athlete to continue playing in a game in which they have suffered a concussion (never) | 172(73.50) | 195(84.05) | 132(79.04) | 200(76.34) | 156(70.27) | |
Figure 1. Mean percent of All Questions Correct.
The control group did not receive education, so there are no immediate post education results for this group. Error bars represent standard deviations.
Figure 2. Mean Percent of Knowledge-Based Questions Correct.
The control group did not receive education, so there are no immediate post education results for this group. Error bars represent standard deviations.
Figure 3. Mean Percent of Behavior and Attitude Questions Correct.
The control group did not receive education, so there are no immediate post education results for this group. Error bars represent standard deviations.
Table 3.
Adjusted repeated measure models using linear mixed model analysis for all questions, knowledge-based questions, and behavioral-based questions
| All Questions | Knowledge-based Questions |
Behavioral-based Questions |
||||
|---|---|---|---|---|---|---|
| Variable | F-value | p-value | F-value | p-value | F-value | p-value |
| Group | 2.09 | .05 | 1.32 | .25 | 1.13 | .29 |
| Time of survey | 4.05 | <.0001 | 6.31 | .01 | .27 | .61 |
| Age | .14 | .71 | 6.79 | .0094 | 11.35 | .0008 |
| Gender | 7.84 | .005 | .79 | .38 | 9.75 | .002 |
| Sport | 3.35 | .02 | 4.29 | .005 | 3.19 | .02 |
| History of concussion education | .00 | .97 | 3.18 | .08 | 2.74 | .10 |
| Time of survey by Group | 34.55 | <.0001 | 5.92 | .02 | 32.25 | <.0001 |
Group = education or control school; Time of survey = postseason or preseason; Gender = females or males; Sport = basketball, football, soccer or wrestling; Time of survey by Group = interaction term of time of survey by group. Type 3 solution for fixed effects is reported.
Concussion reporting and diagnosis during the season
In the education school and control school 43/167 (26%) and 77/222 (35%) participants, respectively, reported that they were hit in the head or body during the season and experienced a headache, dizziness, or confusion. Of the individuals reporting these symptoms, there were fewer athletes in the education school 31/43 (72%) than the control school 68/77 (88%) that reported they continued playing (Chi-Square 5.03, p=.03). In the education and control school, 11/167 (7%) and 13/222 (6%) participants, respectively, reported they were diagnosed with a concussion by an athletic trainer or other health care provider. Of the individuals diagnosed with concussion, a similar number in the education 3/11 (27%) and control schools 3/13 (23%) reported returning to play before their symptoms had resolved (Chi-Square = .06, p=.81).
Discussion
Our findings indicate that a brief, preseason didactic-based concussion educational session likely has minimal benefits. Statistical improvement was noted on a concussion knowledge and self-reported behavior / attitudes survey at the end of the season; however, gains were of the highest magnitude immediately post-education and then declined over time. Although athletes in the education school were more likely to stop playing if they experienced symptoms of concussion compared to a control school, a large number, almost 75%, of athletes in the education school reported that they continued to play despite noting symptoms of concussion. Additionally, approximately 25% of participants that were diagnosed with a concussion during the season in each group reported that they returned to play while still having symptoms. These findings suggest that a didactic preseason concussion education likely has minimal benefits. The effects of the education decline over the season and it is relatively common for student athletes to continue playing through concussion symptoms and to return to play before symptoms resolve. These findings suggest that other factors besides knowledge are likely influencing student-athlete reporting behavior.
With many states requiring student athletes to participate in concussion education prior to sport participation, these findings highlight some of the potential challenges to developing and implementing such programs. Our findings are in agreement with prior research that athletes under report concussion symptoms and many cleared athletes underreport concussion symptoms.(37, 38) Kroshush et al. also found that use of publically available concussion education videos and an informational handout did not significantly change reporting behaviors and reporting behaviors potentially worsened over time.(39) Implementation of these programs may have benefits for knowledge and self-reported behaviors, but that these benefits decline over time.
There are likely a wide variety of factors that influence concussion symptom reporting in athletes, including knowledge and attitudes, internal pressure, concussion history, external pressure and support, perceived outcomes, perceived norms, access to concussion education materials, sports culture, and policies or legislation.(40–42) Improvement in knowledge and attitudes is one aspect that may influence concussion reporting; however, there is a need to develop theory-drive concussion education materials that focus on behavior change and target psychosocial constructs that increase reporting intention.(39, 43) Setting up a culture that emphasizes the importance of reporting concussion and belief that concussions are serious is needed to develop a safe environment for athletes.(44) Future interventions should be developed that focus not only on improving knowledge and attitudes of athletes but also coaches and parents.(45) Improving coach approachability and communication of coaches with athletes about concussion might be a step towards improving the reporting environment.(46)
Our study used a lecture-based format to educate athletes about concussions that is similar to education programs being implemented in many states and further questions the effectiveness of these programs.(47) There were significant improvements in the education school compared to the control school on knowledge and self-reported behaviors, despite the control school reporting more concussion education at baseline. However, although there were mean improvements in knowledge and self-reported behaviors at the end of the season in the education school, it is highly concerning that almost half of the education school participants still reported that they would continue playing if they were exhibiting symptoms of a concussion. Determining the optimal format for delivering educational content to maximize retention and optimize behaviors will be critical.(48) Health behavior change theories used in other areas of health education should be considered for use in concussion education to promote behavior change.(49)
Many athletes in our study reported receiving education on concussion from a variety of sources (parents, coaches, trainers, physicians, and school personnel) at baseline. In adjusted models, prior education was not associated with outcomes. Misconception about concussion by parents, may lead to poor information being passed down to student-athletes;(50) therefore, education of parents, coaches, and school staff may help to improve education about concussion. Because there are a variety of individuals across various settings who provide education on concussion to athletes, concerted efforts to arm a number of individuals with the skills to influence concussion-related behavior change is needed. Through the CDC Heads Up: Concussion program and other local, regional, and state programs, there are resources for parents, clinicians, coaches, and school staff addressing this need.(19, 20, 51–53) However, the impact of these programs on actual concussion reporting behaviors needs to be evaluated.
Limitations
Participants were from one large public school district in the suburbs of Cincinnati, OH, therefore, generalization to other schools locally, regionally or nationally should be considered cautiously. Additionally, athletic trainers were present at each school, thus findings may not generalize to schools without athletic trainers. Conclusions regarding athlete’s participating in spring sports such as baseball, softball, and lacrosse are not possible based on this study. We were unable to determine the nature and extent of education received by individuals previously. The type and characteristics of prior education provided may influence how student athletes responded to the educational intervention. Additionally, because coaches’ knowledge, attitudes, and behaviors were not assessed, the influence of these factors in coaches on athletes’ knowledge, attitudes, and behaviors could not be evaluated. The study population also consisted of primarily males and a higher percentage of females completed the postseason questionnaire, thus potentially biasing the findings. Furthermore, the education program content was tailored to the survey questions used in the study. Although the survey questions were adapted from prior questionnaires commonly used to assess concussion knowledge and behaviors, its external validated and reliability has not been formally assessed. Additionally, since the study focused on self-reported behaviors, there is the potential of recall and reporting bias.
Conclusions
Our findings indicate that a lecture-based, preseason concussion education program provided to adolescent athletes likely has minimal benefits. There are immediate improvements in knowledge and self-reported behaviors, but these benefits decline over time. Future research needs to elucidate the optimal frequency and type of education that will have a significant impact on concussion reporting behavior in student athletes, especially when concussion symptoms are self-identified. Educational programs that are developed using a theoretical basis for changing or adopting a behavior are needed; however, the feasibility of implementing these programs broadly is unclear. A focus on changing the culture of concussion reporting is likely needed as well.
Acknowledgements
This work was supported in part by 1) Ohio Department of Public Safety; 2) National Institutes of Health grant 2K12 HD001097-16 and 3) National Institute of Child Health and Human Development grant 1K23HD074683-01A1. Funding from the above organizations supported the institutions/investigators in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation of the manuscript for publication. Funding organizations did not have a role in review, or approval of the manuscript; and decision to submit the manuscript for publication. Brad Kurowski (Principal investigator) and co-authors had full access to all the data and they take responsibility for the design, data acquisition, integrity of the data, data analysis, and interpretation of the data.
Abbreviations
- CDC
Centers for Disease Control and Prevention
- TBI
Traumatic Brain Injury
Footnotes
Conflicts of interest: The authors do not have conflicts of interested related to the work in this publication. The authors have no financial relationships relevant to this article to disclose.
Meeting presentations: Findings from this study will be presented as a podium presentation at the Injury Free Coalition for Kids conference December 5–7, 2014
Author contribution statement: Each author has made substantial contributions to study design, implementation, analysis, and write up. All authors accept responsibility for reported research, and all authors have participated in the concept and design, analysis and interpretation of data, drafting or revising of the manuscript, and have approved the manuscript as submitted
References
- 1.Gilchrist JTK, Xu L, McGuire LC, Coronado VG. Nonfatal sports and recreation related traumatic brain injuries among children and adolescents treated in emergency departments in the United States, 2001–2009. MMWR. 2011;60(39):1337–1342. [Google Scholar]
- 2.Ruff RM, Iverson GL, Barth JT, Bush SS, Broshek DK, Committee NP. Planning. Recommendations for diagnosing a mild traumatic brain injury: a National Academy of Neuropsychology education paper. Arch Clin Neuropsychol. 2009;24(1):3–10. doi: 10.1093/arclin/acp006. [DOI] [PubMed] [Google Scholar]
- 3.McCrory P, Meeuwisse W, Aubry M, Cantu B, Dvorak J, Echemendia RJ, Engebretsen L, Johnston K, Kutcher JS, Raftery M, et al. Consensus statement on concussion in sport--the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2013;23(2):89–117. doi: 10.1097/JSM.0b013e31828b67cf. Epub 2013/03/13. [DOI] [PubMed] [Google Scholar]
- 4.Theye F, Mueller KA. "Heads up": concussions in high school sports. Clin Med Res. 2004;2(3):165–171. doi: 10.3121/cmr.2.3.165. Epub 2005/06/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webbe FM, Barth JT. Short-term and long-term outcome of athletic closed head injuries. Clinics in sports medicine. 2003;22(3):577–592. doi: 10.1016/s0278-5919(02)00103-5. Epub 2003/07/11. [DOI] [PubMed] [Google Scholar]
- 6.Iverson GL, Gaetz M, Lovell MR, Collins MW. Cumulative effects of concussion in amateur athletes. Brain injury : [BI] 2004;18(5):433–443. doi: 10.1080/02699050310001617352. Epub 2004/06/16. [DOI] [PubMed] [Google Scholar]
- 7.Field M, Collins MW, Lovell MR, Maroon J. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. The Journal of pediatrics. 2003;142(5):546–553. doi: 10.1067/mpd.2003.190. Epub 2003/05/21. [DOI] [PubMed] [Google Scholar]
- 8.Guskiewicz KM, McCrea M, Marshall SW, Cantu RC, Randolph C, Barr W, Onate JA, Kelly JP. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA : the journal of the American Medical Association. 2003;290(19):2549–2555. doi: 10.1001/jama.290.19.2549. Epub 2003/11/20. [DOI] [PubMed] [Google Scholar]
- 9.Eisenberg MA, Andrea J, Meehan W, Mannix R. Time interval between concussions and symptom duration. Pediatrics. 2013;132(1):8–17. doi: 10.1542/peds.2013-0432. Epub 2013/06/12. [DOI] [PubMed] [Google Scholar]
- 10.Cantu RC. Second-impact syndrome. Clin Sports Med. 1998;17(1):37–44. doi: 10.1016/s0278-5919(05)70059-4. Epub 1998/02/26. [DOI] [PubMed] [Google Scholar]
- 11.McCrory PR, Berkovic SF. Second impact syndrome. Neurology. 1998;50(3):677–683. doi: 10.1212/wnl.50.3.677. [DOI] [PubMed] [Google Scholar]
- 12.Covassin T, Stearne D, Elbin R. Concussion history and postconcussion neurocognitive performance and symptoms in collegiate athletes. J Athl Train. 2008;43(2):119–124. doi: 10.4085/1062-6050-43.2.119. Epub 2008/03/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karlin AM. Concussion in the pediatric and adolescent population: "different population, different concerns". PM & R : the journal of injury, function, and rehabilitation. 2011;3(10 Suppl 2):S369–S379. doi: 10.1016/j.pmrj.2011.07.015. Epub 2011/11/09. [DOI] [PubMed] [Google Scholar]
- 14.McCrory P, Davis G, Makdissi M. Second impact syndrome or cerebral swelling after sporting head injury. Current sports medicine reports. 2012;11(1):21–23. doi: 10.1249/JSR.0b013e3182423bfd. Epub 2012/01/13. [DOI] [PubMed] [Google Scholar]
- 15.Giza CC, Kutcher JS, Ashwal S, Barth J, Getchius TS, Gioia GA, Gronseth GS, Guskiewicz K, Mandel S, Manley G, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80(24):2250–2257. doi: 10.1212/WNL.0b013e31828d57dd. Epub 2013/03/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, Kutcher JS, Pana A, Putukian M, Roberts WO, et al. American Medical Society for Sports Medicine position statement: concussion in sport. British journal of sports medicine. 2013;47(1):15–26. doi: 10.1136/bjsports-2012-091941. Epub 2012/12/18. [DOI] [PubMed] [Google Scholar]
- 17.Herring SA, Cantu RC, Guskiewicz KM, Putukian M, Kibler WB, Bergfeld JA, Boyajian-O'Neill LA, Franks RR, Indelicato PA. Concussion (mild traumatic brain injury) and the team physician: a consensus statement--2011 update. Med Sci Sports Exerc. 2011;43(12):2412–2422. doi: 10.1249/MSS.0b013e3182342e64. Epub 2011/11/18. [DOI] [PubMed] [Google Scholar]
- 18.McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorak J, Echemendia RJ, Engebretsen L, Johnston K, Kutcher JS, Raftery M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. British journal of sports medicine. 2013;47(5):250–258. doi: 10.1136/bjsports-2013-092313. Epub 2013/03/13. [DOI] [PubMed] [Google Scholar]
- 19.Chrisman SP, Schiff MA, Rivara FP. Physician concussion knowledge and the effect of mailing the CDC's "Heads Up" toolkit. Clin Pediatr (Phila) 2011;50(11):1031–1039. doi: 10.1177/0009922811410970. Epub 2011/06/08. [DOI] [PubMed] [Google Scholar]
- 20.Sarmiento K, Mitchko J, Klein C, Wong S. Evaluation of the Centers for Disease Control and Prevention's concussion initiative for high school coaches: "Heads Up: Concussion in High School Sports". J Sch Health. 2010;80(3):112–118. doi: 10.1111/j.1746-1561.2010.00491.x. Epub 2010/03/20. [DOI] [PubMed] [Google Scholar]
- 21.O’Donoghue E, Onate J, Van Lunen B, Peterson C. Assessment of high school coaches’ knowledge of sport-related concussions. Athletic Training and Sports Health Care. 2009;1:120–132. [Google Scholar]
- 22.Rivara FP, Schiff MA, Chrisman SP, Chung SK, Ellenbogen RG, Herring SA. The Effect of Coach Education on Reporting of Concussions Among High School Athletes After Passage of a Concussion Law. Am J Sports Med. 2014 doi: 10.1177/0363546514521774. Epub 2014/02/27. [DOI] [PubMed] [Google Scholar]
- 23.Williamson IJ, Goodman D. Converging evidence for the under-reporting of concussions in youth ice hockey. British journal of sports medicine. 2006;40(2):128–132. doi: 10.1136/bjsm.2005.021832. discussion -32. Epub 2006/01/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2004;14(1):13–17. doi: 10.1097/00042752-200401000-00003. Epub 2004/01/09. [DOI] [PubMed] [Google Scholar]
- 25.Sye G, Sullivan SJ, McCrory P. High school rugby players' understanding of concussion and return to play guidelines. British journal of sports medicine. 2006;40(12):1003–1005. doi: 10.1136/bjsm.2005.020511. Epub 2006/11/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5):643–650. doi: 10.1177/03635465000280050401. Epub 2000/10/14. [DOI] [PubMed] [Google Scholar]
- 27.Kaut KP, DePompei R, Kerr J, Congeni J. Reports of head injury and symptom knowledge among college athletes: implications for assessment and educational intervention. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport medicine. 2003;13(4):213–221. doi: 10.1097/00042752-200307000-00004. Epub 2003/07/12. [DOI] [PubMed] [Google Scholar]
- 28.Delaney JS, Lamfookon C, Bloom GA, Al-Kashmiri A, Correa JA. Why University Athletes Choose Not to Reveal Their Concussion Symptoms During a Practice or Game. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2014 doi: 10.1097/JSM.0000000000000112. Epub 2014/06/21. [DOI] [PubMed] [Google Scholar]
- 29.Llewellyn T, Burdette GT, Joyner AB, Buckley TA. Concussion reporting rates at the conclusion of an intercollegiate athletic career. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport medicine. 2014;24(1):76–79. doi: 10.1097/01.jsm.0000432853.77520.3d. Epub 2013/10/26. [DOI] [PubMed] [Google Scholar]
- 30.Delaney JS, Lacroix VJ, Leclerc S, Johnston KM. Concussions among university football and soccer players. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport medicine. 2002;12(6):331–338. doi: 10.1097/00042752-200211000-00003. Epub 2002/12/06. [DOI] [PubMed] [Google Scholar]
- 31.Register-Mihalik JK, Guskiewicz KM, McLeod TC, Linnan LA, Mueller FO, Marshall SW. Knowledge, Attitude, and Concussion-Reporting Behaviors Among High School Athletes: A Preliminary Study. J Athl Train. 2013 doi: 10.4085/1062-6050-48.3.20. Epub 2013/07/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bramley HP, Patrick K, Lehman E, Silvis M. High School Soccer Players With Concussion Education Are More Likely to Notify Their Coach of a Suspected Concussion. Clin Pediatr (Phila) 2011 doi: 10.1177/0009922811425233. Epub 2011/10/19. [DOI] [PubMed] [Google Scholar]
- 33.Kurowski B, Pomerantz WJ, Schaiper C, Gittelman MA. Factors that influence concussion knowledge and self-reported attitudes in high school athletes. J Trauma Acute Care Surg. 2014;77(3 Suppl 1):S12–S17. doi: 10.1097/TA.0000000000000316. Epub 2014/08/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ohio Department of Education. [cited 2014 February 6]; Available from: http://reportcard.education.ohio.gov/Pages/School-Report.aspx?SchoolIRN=019737.
- 35.AIAACADEMY BRAINBOOK. [cited 2012 April 1]. Available from: http://aiaacademy.org/users/login/brainbook. [Google Scholar]
- 36.McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, Cantu R. Consensus statement on concussion in sport - The 3rd international conference on concussion in sport held in Zurich, November 2008. PM & R : the journal of injury, function, and rehabilitation. 2009;1(5):406–420. doi: 10.1016/j.pmrj.2009.03.010. Epub 2009/07/25. [DOI] [PubMed] [Google Scholar]
- 37.Meier TB, Brummel BJ, Singh R, Nerio CJ, Polanski DW, Bellgowan PS. The underreporting of self-reported symptoms following sports-related concussion. J Sci Med Sport. 2014 doi: 10.1016/j.jsams.2014.07.008. Epub 2014/08/26. [DOI] [PubMed] [Google Scholar]
- 38.Miyashita TL, Timpson WM, Frye MA, Gloeckner GW. The impact of an educational intervention on college athletes' knowledge of concussions. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport medicine. 2013;23(5):349–353. doi: 10.1097/JSM.0b013e318289c321. Epub 2013/03/27. [DOI] [PubMed] [Google Scholar]
- 39.Kroshus E, Baugh CM, Hawrilenko M, Daneshvar DH. Pilot Randomized Evaluation of Publically Available Concussion Education Materials: Evidence of a Possible Negative Effect. Health Educ Behav. 2014 doi: 10.1177/1090198114543011. Epub 2014/08/17. [DOI] [PubMed] [Google Scholar]
- 40.Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: Review and application of the socio-ecological framework. Brain injury : [BI] 2014;28(8):1009–1021. doi: 10.3109/02699052.2014.904049. Epub 2014/04/18. [DOI] [PubMed] [Google Scholar]
- 41.Silverberg ND, Lange RT, Millis SR, Rose A, Hopp G, Leach S, Iverson GL. Post-concussion symptom reporting after multiple mild traumatic brain injuries. J Neurotrauma. 2013;30(16):1398–1404. doi: 10.1089/neu.2012.2827. Epub 2013/03/06. [DOI] [PubMed] [Google Scholar]
- 42.Kroshus E, Baugh CM, Daneshvar DH, Viswanath K. Understanding concussion reporting using a model based on the theory of planned behavior. J Adolesc Health. 2014;54(3):269 e2–274 e2. doi: 10.1016/j.jadohealth.2013.11.011. Epub 2014/02/25. [DOI] [PubMed] [Google Scholar]
- 43.Kroshus E, Baugh CM, Daneshvar DH, Nowinski CJ, Cantu RC. Concussion Reporting Intention: A Valuable Metric for Predicting Reporting Behavior and Evaluating Concussion Education. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2014 doi: 10.1097/JSM.0000000000000137. Epub 2014/07/23. [DOI] [PubMed] [Google Scholar]
- 44.Robert G, Frederick PR, Morgan AF, Carol Mason S, editors. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 45.Register-Mihalik JK, Linnan LA, Marshall SW, Valovich McLeod TC, Mueller FO, Guskiewicz KM. Using theory to understand high school aged athletes' intentions to report sport-related concussion: Implications for concussion education initiatives. Brain injury : [BI] 2013;27(7–8):878–886. doi: 10.3109/02699052.2013.775508. Epub 2013/06/26. [DOI] [PubMed] [Google Scholar]
- 46.Chrisman SP, Quitiquit C, Rivara FP. Qualitative study of barriers to concussive symptom reporting in high school athletics. J Adolesc Health. 2013;52(3):330 e3–335 e3. doi: 10.1016/j.jadohealth.2012.10.271. Epub 2013/02/23. [DOI] [PubMed] [Google Scholar]
- 47.Kay MC, Welch CE, Valovich McLeod TC. Positive and Negative Factors that Influence Concussion Reporting Among Secondary School Athletes. J Sport Rehabil. 2014 doi: 10.1123/jsr.2013-0132. Epub 2014/01/25. [DOI] [PubMed] [Google Scholar]
- 48.Provvidenza C, Engebretsen L, Tator C, Kissick J, McCrory P, Sills A, Johnston KM. From consensus to action: knowledge transfer, education and influencing policy on sports concussion. British journal of sports medicine. 2013;47(5):332–338. doi: 10.1136/bjsports-2012-092099. Epub 2013/01/26. [DOI] [PubMed] [Google Scholar]
- 49.Kinzie MB. Instructional design strategies for health behavior change. Patient education and counseling. 2005;56(1):3–15. doi: 10.1016/j.pec.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 50.Mannings C, Kalynych C, Joseph MM, Smotherman C, Kraemer DF. Knowledge assessment of sports-related concussion among parents of children aged 5 years to 15 years enrolled in recreational tackle football. J Trauma Acute Care Surg. 2014;77(3 Suppl 1):S18–S22. doi: 10.1097/TA.0000000000000371. Epub 2014/08/26. [DOI] [PubMed] [Google Scholar]
- 51.Covassin T, Elbin RJ, Sarmiento K. Educating coaches about concussion in sports: evaluation of the CDC's "Heads Up: concussion in youth sports" initiative. J Sch Health. 2012;82(5):233–238. doi: 10.1111/j.1746-1561.2012.00692.x. Epub 2012/04/13. [DOI] [PubMed] [Google Scholar]
- 52.Sawyer RJ, Hamdallah M, White D, Pruzan M, Mitchko J, Huitric M. High school coaches' assessments, intentions to use, and use of a concussion prevention toolkit: Centers for Disease Control and Prevention's heads up: concussion in high school sports. Health Promot Pract. 2010;11(1):34–43. doi: 10.1177/1524839907309377. Epub 2008/04/11. [DOI] [PubMed] [Google Scholar]
- 53.Heads up in 10 years: The anniversity virewbook of CDC's heads up. Center for Disease Control and Prevention; 2013. [cited 2014 May 19]. Available from: http://www.cdc.gov/concussion/pdf/HeadsUp_10YrViewBook-a.pdf. [Google Scholar]