Abstract
Background:
Descriptive epidemiology of total joint replacement procedures is limited to annual procedure volumes (incidence). The prevalence of the growing number of individuals living with a total hip or total knee replacement is currently unknown. Our objective was to estimate the prevalence of total hip and total knee replacement in the United States.
Methods:
Prevalence was estimated using the counting method by combining historical incidence data from the National Hospital Discharge Survey and the Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases from 1969 to 2010 with general population census and mortality counts. We accounted for relative differences in mortality rates between those who have had total hip or knee replacement and the general population.
Results:
The 2010 prevalence of total hip and total knee replacement in the total U.S. population was 0.83% and 1.52%, respectively. Prevalence was higher among women than among men and increased with age, reaching 5.26% for total hip replacement and 10.38% for total knee replacement at eighty years. These estimates corresponded to 2.5 million individuals (1.4 million women and 1.1 million men) with total hip replacement and 4.7 million individuals (3.0 million women and 1.7 million men) with total knee replacement in 2010. Secular trends indicated a substantial rise in prevalence over time and a shift to younger ages.
Conclusions:
Around 7 million Americans are living with a hip or knee replacement, and consequently, in most cases, are mobile, despite advanced arthritis. These numbers underscore the substantial public health impact of total hip and knee arthroplasties.
The incidence of joint replacement procedures is high, with over 1 million total hip and total knee replacement procedures performed each year in the United States1. With the aging of the “baby boomers,” higher rates of diagnosis and treatment of advanced arthritis, and growing demand for improved mobility and quality of life, the annual procedure volumes are projected to increase considerably in the future, making joint replacements the most common elective surgical procedures in the coming decades2,3. Such a large increase in demand is unprecedented and must be addressed with effective planning of health-care services for these individuals, not only during the perioperative period but throughout the lifelong continued care of this population.
To date, studies involving the descriptive epidemiology of total hip and total knee replacement have focused almost exclusively on annual procedure volumes (i.e., incidence)2-9. Although incidence data are informative, they offer an incomplete assessment of the impact of total hip and total knee replacement on the population and the health-care system. The prevalence of individuals who are currently living with an artificial hip or knee joint in the United States is currently unknown. Indeed, the increasing use of joint replacement in younger individuals, coupled with improvements in life expectancy, has created a large pool of individuals with hip and knee replacements in the United States2,10. These individuals not only have specialized needs, but in some cases, will outlive their implants and require expensive revision surgeries with substantial implications related to cost and resource use. Therefore, estimates of prevalence are vital to agencies charged with planning for the provision of health-care services for these individuals. We know of only one study to date that has provided prevalence estimates of total knee replacement11, but the methodology used to estimate prevalence was based on a computer-simulation model of the natural history of osteoarthritis and did not take into account the substantial increase in procedure volumes in recent years5. Therefore, we sought to estimate the current prevalence and historical trends in the prevalence of total hip and total knee replacement in the United States using multiple data sources and accounting for the secular increase in procedure volumes in recent years.
Materials and Methods
The prevalence of total hip or total knee replacement is the proportion of individuals who are alive on a certain date and had total hip or total knee replacement (or both), regardless of how long ago the initial procedure was performed. We used counting methods12,13 to estimate prevalence, starting from 1969 and 1971, when total hip and total knee replacement procedures, respectively, were first performed in the United States. Details of the methods are outlined in the Appendix and briefly summarized below. This study was approved by the institutional review board.
Briefly, incidence (procedure volume) data were obtained from two data sources. For the period of 1990 to 2010, we collaborated with the U.S. Department of Health & Human Services Agency for Healthcare Research and Quality (AHRQ) and relied on the Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases (SID) to estimate total hip and total knee replacement procedure counts by calendar year, state, sex, and single-year age groups. For the period of 1969 to 1989, we relied on the National Hospital Discharge Survey (NHDS) to estimate the annual number of total hip and total knee replacement procedures by calendar year, four major census regions, sex, and single-year age groups14. Calendar-year, state, sex, and single year of age-specific U.S. population estimates from 1969 to 2010 were obtained from the United States Census Bureau15. Historical population mortality data were obtained from the National Center for Health Statistics (NCHS) vital statistics16. We also accounted for procedure-specific relative death rates using published literature17-19 and unpublished regional U.S. data and applied them to calendar-year, state, sex, and single year of age-specific mortality data obtained from the NCHS.
Source of Funding
No external funds were used for the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript. This study was, in part, made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under award number R01AG034676.
Results
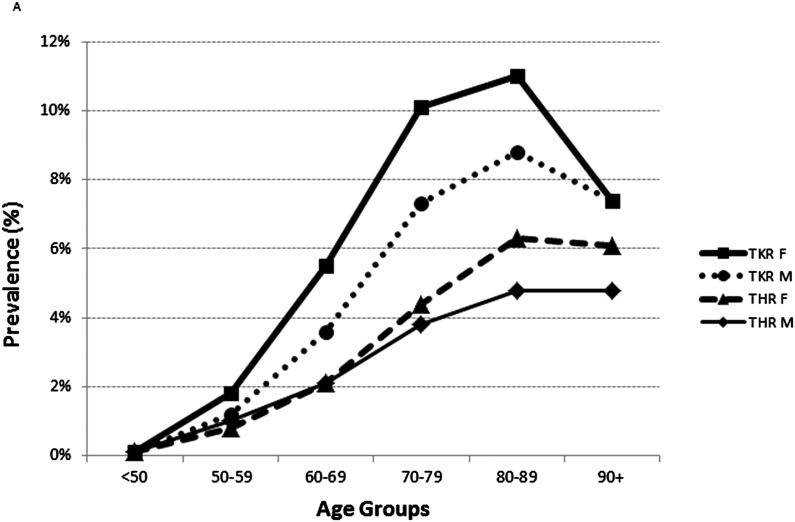
We estimate that the 2010 prevalence of total hip and total knee replacement among the total U.S. population was 0.83% and 1.52%, respectively (Table I and Figs. 1-A and 1-B). The prevalence of total hip and total knee replacement among adults fifty years of age or older was 2.34% and 4.55%, respectively. For both procedures, the prevalence was higher among women than among men. Prevalence increased with age, and more steeply for total knee replacement than for total hip replacement. The prevalence of total hip replacement at fifty years of age was 0.58% and increased to 1.49% at sixty years, 3.25% at seventy years, 5.26% at eighty years, and 5.87% at ninety years of age. The prevalence of total knee replacement at fifty years of age was 0.68% and increased to 2.92% at sixty years, 7.29% at seventy years, 10.38% at eighty years, and 8.48% at ninety years of age. These prevalence estimates corresponded to 2.5 million individuals (1.4 million women and 1.1 million men) with total hip replacement and 4.7 million individuals (3.0 million women and 1.7 million men) with total knee replacement in the United States in 2010 (Table I). Comparing these prevalence estimates with cumulative incidence, we found that about 62% of all individuals who underwent total hip replacement and about 73% of all individuals who underwent total knee replacement in the United States were still alive in 2010. Assuming that roughly 8.5% of these individuals had both procedures (Table II), we estimate that there were about 620,000 individuals (410,000 women and 210,000 men) who had both procedures, corresponding to about 0.2% of the U.S. population in 2010.
TABLE I.
Estimated 2010 Prevalence of Total Hip and Total Knee Replacement in the United States
| Total Hip Replacement |
Total Knee Replacement |
|||
| No. of Individuals | Prevalence* | No. of Individuals | Prevalence* | |
| Overall | 2,552,815 | 0.83 (0.83-0.83) | 4,700,621 | 1.52 (1.52-1.52) |
| Population ≥50 years of age | 2,330,539 | 2.34 (2.34-2.35) | 4,526,451 | 4.55 (4.55-4.56) |
| Sex | ||||
| Women | 1,452,495 | 0.93 (0.92-0.93) | 2,965,541 | 1.89 (1.89-1.89) |
| Men | 1,100,320 | 0.72 (0.72-0.73) | 1,735,080 | 1.14 (1.14-1.14) |
| Age group (yr) | ||||
| <50 | 222,276 | 0.11 (0.11-0.11) | 174,170 | 0.08 (0.08-0.08) |
| 50-59 | 383,517 | 0.91 (0.91-0.91) | 624,468 | 1.48 (1.48-1.49) |
| 60-69 | 625,416 | 2.12 (2.12-2.13) | 1,350,693 | 4.59 (4.58-4.59) |
| 70-79 | 681,136 | 4.10 (4.09-4.11) | 1,463,890 | 8.80 (8.79-8.82) |
| 80-89 | 534,048 | 5.69 (5.68-5.71) | 950,942 | 10.13 (10.11-10.15) |
| ≥90 | 106,422 | 5.77 (5.73-5.80) | 136,458 | 7.40 (7.36-7.44) |
| Age (yr) | ||||
| 50 | 27,006 | 0.58 (0.57-0.59) | 31,553 | 0.68 (0.67-0.69) |
| 60 | 53,809 | 1.49 (1.48-1.50) | 105,432 | 2.92 (2.90-2.94) |
| 70 | 66,972 | 3.25 (3.23-3.28) | 150,071 | 7.29 (7.25-7.33) |
| 80 | 69,294 | 5.26 (5.22-5.30) | 136,690 | 10.38 (10.32-10.43) |
| 90 | 26,269 | 5.87 (5.80-5.94) | 37,970 | 8.48 (8.40-8.57) |
Values are shown as the percentage, with the 95% confidence interval (CI) in parentheses. CIs were calculated assuming a Poisson distribution.
Fig. 1.
A: Age and sex-specific prevalence of total hip replacement (THR) and total knee replacement (TKR) among the total population of the United States in 2010. The lines represent the percentage of the 2010 total U.S. population with total hip and total knee replacement by age group. B: The number of individuals among the 2010 total U.S. population who had undergone total hip replacement (THR) and total knee replacement (TKR) according to age group.
TABLE II.
Estimated Number of Individuals Who Had Both Total Hip and Total Knee Replacement Among the Total U.S. Population in 2010*
| Olmsted County, Minnesota |
United States |
|||||||||
| Age Group (yr) | No. with Either THR or TKR | No.with Both THR and TKR | County Population | % Prevalent Cases with Both Procedures (A) | Prevalence of Both in Olmsted County (B) | Estimated No. with Either THR or TKR | Total 2010 U.S. Population | Estimated No. with Both Procedures (Assuming Prevalence from A)† | Estimated No. (Assuming Prevalence from B)† | |
| Female | <50 | 156 | 12 | 48,814 | 7.69% | 0.02% | 188,850 | 103,577,271 | 14,527 | 25,463 |
| 50-59 | 334 | 21 | 9,707 | 6.29% | 0.22% | 556,055 | 21,559,563 | 34,962 | 46,642 | |
| 60-69 | 577 | 54 | 6,048 | 9.36% | 0.89% | 1,169,996 | 15,427,351 | 109,497 | 137,744 | |
| 70-79 | 554 | 50 | 3,834 | 9.03% | 1.30% | 1,323,605 | 9,178,735 | 119,459 | 119,702 | |
| 80+ | 304 | 36 | 3,247 | 11.84% | 1.11% | 1,179,530 | 7,126,835 | 139,681 | 79,016 | |
| All age groups | 1,925 | 173 | 71,650 | 8.99% | 0.24% | 4,418,036 | 156,869,755 | 418,126 | 408,567 | |
| Male | <50 | 128 | 9 | 48,961 | 7.03% | 0.02% | 207,596 | 105,709,894 | 14,597 | 19,432 |
| 50-59 | 225 | 10 | 9,153 | 4.44% | 0.11% | 451,930 | 20,512,532 | 20,086 | 22,411 | |
| 60-69 | 350 | 27 | 5,432 | 7.71% | 0.50% | 806,113 | 14,029,131 | 62,186 | 69,732 | |
| 70-79 | 350 | 27 | 3,236 | 7.71% | 0.83% | 821,421 | 7,447,964 | 63,367 | 62,143 | |
| 80+ | 123 | 16 | 1,826 | 13.01% | 0.88% | 548,340 | 4,101,693 | 71,329 | 35,940 | |
| All age groups | 1,176 | 89 | 68,608 | 7.57% | 0.13% | 2,835,400 | 151,801,214 | 231,565 | 209,658 | |
| Total | 3,101 | 262 | 140,258 | 8.45% | 0.19% | 7,253,436 | 308,670,969 | 649,691 | 618,225 | |
Estimated based on Olmsted County data and published literature27. THR = total hip replacement, and TKR = total knee replacement.
Estimated numbers differ from the product of table columns because of rounding.
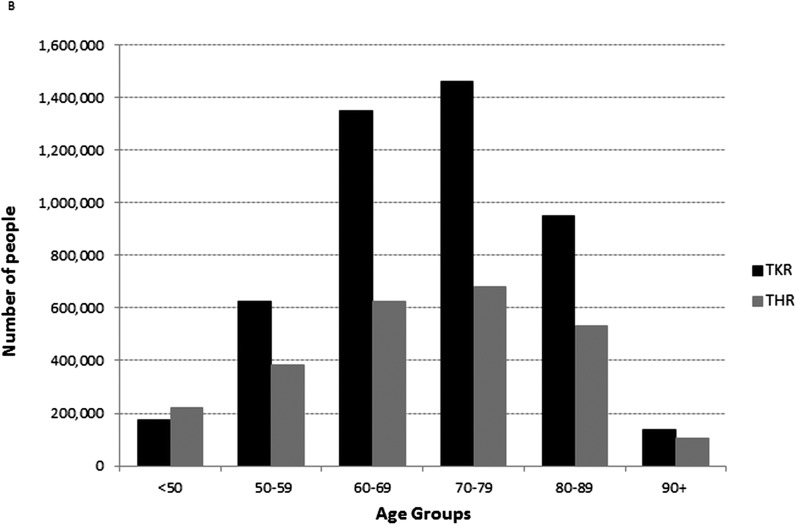
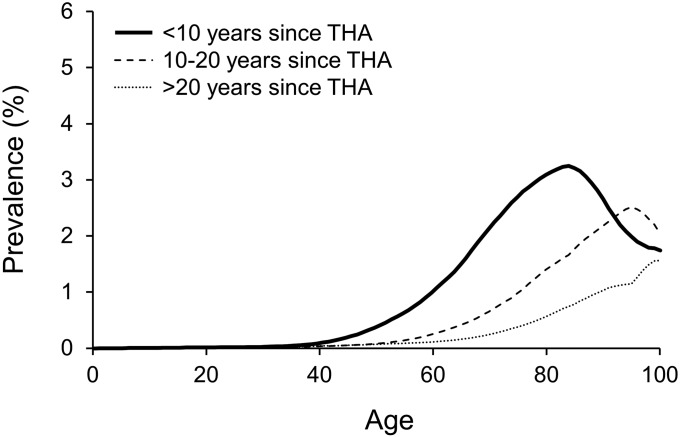
Figures 2-A and 2-B show the age-specific 2010 prevalence of total hip and total knee replacement according to the duration of time since the initial procedure. The majority of the individuals in the prevalence pool (65% of total hip and 72% of total knee replacement patients) had undergone the initial procedure less than ten years earlier (Table III). Although the overall distributions looked similar, the total knee replacement curves shifted to the left, with the nadir of the prevalence curves for less than ten years and ten to twenty years corresponding to younger ages than for total hip replacement. About one-fourth of the total hip replacement patients (24%) and about one-fifth of the total knee replacement patients (21%) had undergone the initial procedure ten to twenty years earlier. In terms of absolute numbers, the number of individuals who were more than twenty years from their initial total hip or total knee replacement was about the same.
Fig. 2.
Age-specific 2010 prevalence of total hip arthroplasty (THA) (Fig. 2-A) and total knee arthroplasty (TKA) (Fig. 2-B) among the total U.S. population according to duration of time since the initial procedure.
TABLE III.
Distribution of Individuals in Prevalence Pool by Age Group and Time Since Initial Procedure
| Total Hip Replacement* |
Total Knee Replacement* |
|||||||
| Age Group (yr) | <10 Yr | 10-20 Yr | >20 Yr | Total No. Hip Arthroplasty | <10 Yr | 10-20 Yr | >20 Yr | Total No. Knee Arthroplasty |
| <50 | 136,395 | 47,721 | 38,160 | 222,276 | 104,308 | 28,968 | 40,894 | 174,170 |
| 50-59 | 280,584 | 64,084 | 38,849 | 383,517 | 537,467 | 47,092 | 39,909 | 624,468 |
| 60-69 | 450,553 | 125,750 | 49,113 | 625,416 | 1,117,588 | 188,681 | 44,424 | 1,350,693 |
| 70-79 | 447,920 | 168,097 | 65,119 | 681,136 | 1,046,717 | 348,568 | 68,605 | 1,463,890 |
| 80-89 | 294,119 | 165,978 | 73,951 | 534,048 | 547,054 | 323,444 | 80,444 | 950,942 |
| ≥90 | 40,754 | 43,969 | 21,699 | 106,422 | 50,865 | 67,476 | 18,117 | 136,458 |
| All | 1,650,325 (65%) | 615,599 (24%) | 286,891 (11%) | 2,552,815 | 3,403,999 (72%) | 1,004,229 (21%) | 292,393 (6%) | 4,700,621 |
Values are presented as the number of individuals, with the percentage of the total in parentheses.
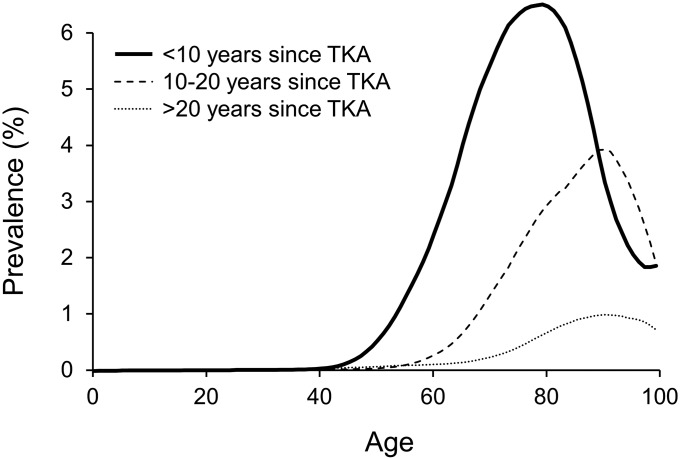
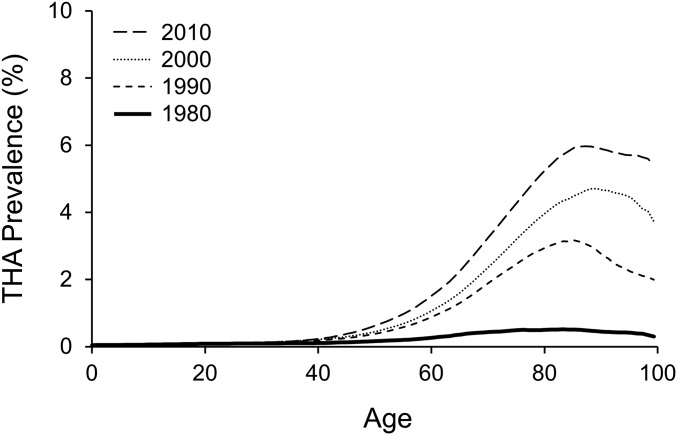
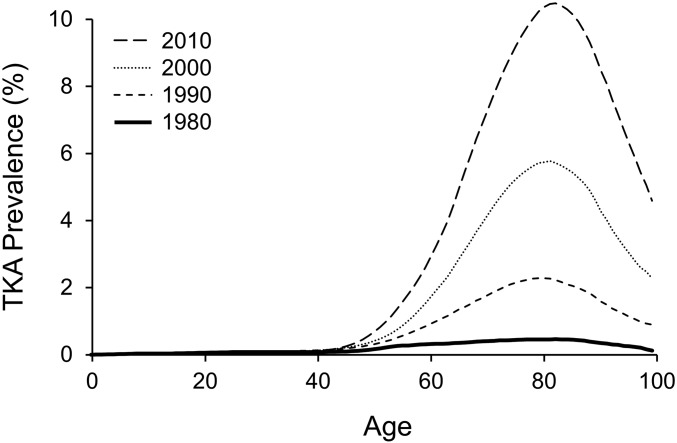
Figures 3-A and 3-B show trends in age-specific prevalence since 1980. As illustrated by the distance between the lines, there was a notable increase in the prevalence of total hip replacement between 1980 and 1990 (Fig. 3-A). The overall prevalence of total hip replacement was 0.11% in 1980, increased fourfold to 0.42% in 1990, and then to 0.57% in 2000 and 0.83% in 2010 (Table IV). The most notable increase in the prevalence of total knee replacement occurred between 2000 and 2010 (Fig. 3-B). The overall prevalence of total knee replacement in 1980 was 0.13% and increased to 0.38% in 1990, 0.80% in 2000, and 1.52% in 2010. The increase in the prevalence of total knee replacement was evident in all age groups but most notably among elderly women (seventy to eighty-nine years of age). There was a shift in prevalence to younger ages over time, as illustrated by the slight leftward shift of the prevalence curves in Figure 3-B.
Fig. 3.
Secular changes in the prevalence of total hip arthroplasty (THA) (Fig. 3-A) and total knee arthroplasty (TKA) (Fig. 3-B) in the total U.S. population between 1980 and 2010.
TABLE IV.
Trends in Age and Sex-Specific Prevalence of Total Hip and Total Knee Replacement Among Total U.S. Population Between 1980 and 2010
| 1980 |
1990 |
2000 |
2010 |
||||||||||
| Age Group (yr) | No. | Population | Prevalence | No. | Population | Prevalence | No. | Population | Prevalence | No. | Population | Prevalence | |
| Total hip replacement | |||||||||||||
| Female | <50 | 27,315 | 83,585,575 | 0.03% | 64,581 | 91,999,727 | 0.07% | 87,150 | 101,110,188 | 0.09% | 99,875 | 103,577,271 | 0.10% |
| 50-59 | 19,008 | 12,175,416 | 0.16% | 58,940 | 11,294,203 | 0.52% | 93,113 | 16,050,005 | 0.58% | 177,522 | 21,559,563 | 0.82% | |
| 60-69 | 33,566 | 10,306,337 | 0.33% | 151,676 | 11,209,278 | 1.35% | 172,543 | 10,799,397 | 1.60% | 329,547 | 15,427,351 | 2.14% | |
| 70-79 | 33,539 | 6,915,806 | 0.49% | 211,015 | 8,315,470 | 2.54% | 303,662 | 9,311,844 | 3.26% | 400,753 | 9,178,735 | 4.37% | |
| 80-89 | 15,620 | 2,919,371 | 0.54% | 131,782 | 3,955,284 | 3.33% | 234,436 | 5,031,903 | 4.66% | 363,080 | 5,798,465 | 6.26% | |
| 90+ | 2,347 | 562,503 | 0.42% | 20,260 | 785,256 | 2.58% | 50,370 | 1,076,556 | 4.68% | 81,718 | 1,328,370 | 6.15% | |
| Male | <50 | 43,860 | 84,020,171 | 0.05% | 80,717 | 93,447,372 | 0.09% | 103,983 | 103,358,063 | 0.10% | 122,401 | 105,709,894 | 0.12% |
| 50-59 | 18,174 | 11,064,189 | 0.16% | 56,198 | 10,507,941 | 0.53% | 100,462 | 15,231,187 | 0.66% | 205,995 | 20,512,532 | 1.00% | |
| 60-69 | 24,049 | 8,589,510 | 0.28% | 107,044 | 9,443,061 | 1.13% | 140,682 | 9,547,191 | 1.47% | 295,869 | 14,029,131 | 2.11% | |
| 70-79 | 16,658 | 4,720,856 | 0.35% | 119,360 | 5,821,430 | 2.05% | 193,706 | 6,954,483 | 2.79% | 280,383 | 7,447,964 | 3.76% | |
| 80-89 | 4,855 | 1,510,125 | 0.32% | 47,830 | 1,964,825 | 2.43% | 101,373 | 2,724,215 | 3.72% | 170,968 | 3,585,161 | 4.77% | |
| 90+ | 566 | 196,201 | 0.29% | 4,872 | 242,645 | 2.01% | 14,158 | 352,497 | 4.02% | 24,704 | 516,532 | 4.78% | |
| Total | 239,557 | 226,566,060 | 0.11% | 1,054,275 | 248,986,492 | 0.42% | 1,595,638 | 281,547,529 | 0.57% | 2,552,815 | 308,670,969 | 0.83% | |
| Total knee replacement | |||||||||||||
| Female | <50 | 22,520 | 83,585,575 | 0.03% | 46,327 | 91,999,727 | 0.05% | 63,053 | 101,110,188 | 0.06% | 88,975 | 103,577,271 | 0.09% |
| 50-59 | 19,267 | 12,175,416 | 0.16% | 65,812 | 11,294,203 | 0.58% | 147,676 | 16,050,005 | 0.92% | 378,533 | 21,559,563 | 1.76% | |
| 60-69 | 28,901 | 10,306,337 | 0.28% | 154,102 | 11,209,278 | 1.37% | 336,293 | 10,799,397 | 3.11% | 840,449 | 15,427,351 | 5.45% | |
| 70-79 | 26,937 | 6,915,806 | 0.39% | 190,024 | 8,315,470 | 2.29% | 512,354 | 9,311,844 | 5.50% | 922,852 | 9,178,735 | 10.05% | |
| 80-89 | 11,069 | 2,919,371 | 0.38% | 91,367 | 3,955,284 | 2.31% | 296,546 | 5,031,903 | 5.89% | 636,571 | 5,798,465 | 10.98% | |
| 90+ | 1,286 | 562,503 | 0.23% | 10,365 | 785,256 | 1.32% | 39,164 | 1,076,556 | 3.64% | 98,161 | 1,328,370 | 7.39% | |
| Male | <50 | 78,715 | 84,020,171 | 0.09% | 91,346 | 93,447,372 | 0.10% | 95,055 | 103,358,063 | 0.09% | 85,195 | 105,709,894 | 0.08% |
| 50-59 | 39,319 | 11,064,189 | 0.36% | 52,850 | 10,507,941 | 0.50% | 108,033 | 15,231,187 | 0.71% | 245,935 | 20,512,532 | 1.20% | |
| 60-69 | 37,036 | 8,589,510 | 0.43% | 113,504 | 9,443,061 | 1.20% | 216,833 | 9,547,191 | 2.27% | 510,244 | 14,029,131 | 3.64% | |
| 70-79 | 23,324 | 4,720,856 | 0.49% | 101,278 | 5,821,430 | 1.74% | 304,289 | 6,954,483 | 4.38% | 541,038 | 7,447,964 | 7.26% | |
| 80-89 | 8,501 | 1,510,125 | 0.56% | 34,138 | 1,964,825 | 1.74% | 129,537 | 2,724,215 | 4.76% | 314,371 | 3,585,161 | 8.77% | |
| 90+ | 954 | 196,201 | 0.49% | 3,560 | 242,645 | 1.47% | 12,865 | 352,497 | 3.65% | 38,297 | 516,532 | 7.41% | |
| Total | 297,829 | 226,566,060 | 0.13% | 954,673 | 248,986,492 | 0.38% | 2,261,698 | 281,547,529 | 0.80% | 4,700,621 | 308,670,969 | 1.52% | |
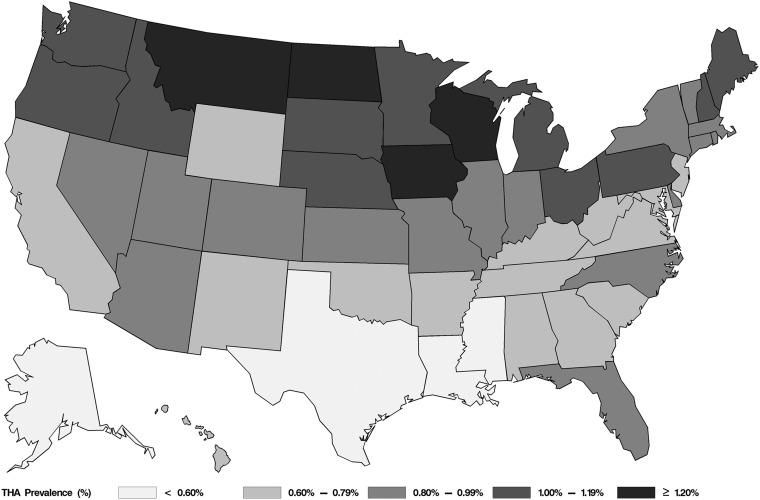
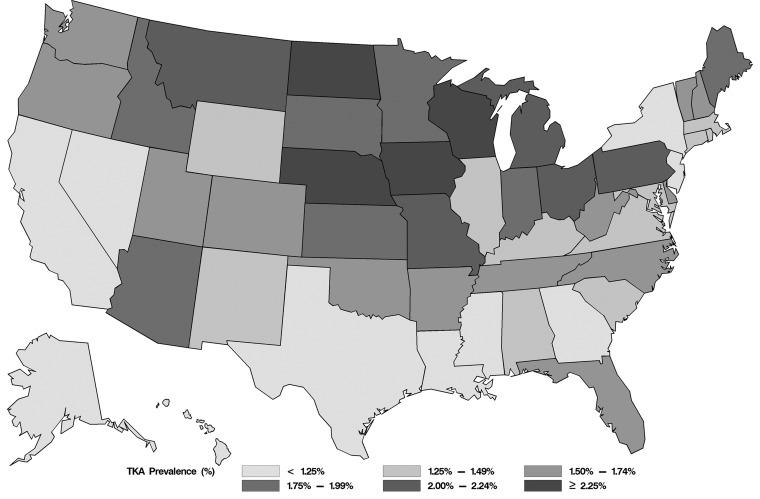
The three states with the highest prevalence of total hip and total knee replacement were Iowa, North Dakota, and Wisconsin (Figs. 4-A and 4-B). The prevalence of total hip replacement in these three states was 1.22% to 1.25%, whereas the national average was 0.83% (Fig. 4-A). The prevalence of total knee replacement in these three states was 2.36% to 2.63%, whereas the national average was 1.52% (Fig. 4-B). States with the highest number of individuals with total hip and total knee replacement were the three states with the largest populations (California, Florida, and Texas), despite a relatively low prevalence. The ranking of individual states was different for total hip and total knee replacements. For example, New York ranked twenty-third in prevalence (0.81%) of total hip replacement but ranked fourth in prevalence (1.09%) of total knee replacement.
Fig. 4.
2010 prevalence of total hip arthroplasty (THA) (Fig. 4-A) and total knee arthroplasty (THA) (Fig. 4-B) in individual states.
Discussion
We estimate that a little over 2% of individuals in the United States were living with a total hip or total knee replacement in 2010. This corresponds to an estimated 7 million people, including 620,000 individuals who underwent both procedures. These numbers underscore the large number of Americans who have benefited from these procedures. Given the success of total hip and knee replacement in improving function and quality of life of individuals with severe arthritis, the current trends will likely continue in the coming decades.
Although there are many studies documenting the rapid increase in incidence of total hip and total knee replacement in the United States, there is only one study that we know of on the prevalence of total knee replacement11. Our prevalence estimates for total knee replacement are about 20% higher than in this earlier study by Weinstein et al. This discrepancy may be due, in part, to statistical methodology, to the inclusion of more recent data in our analysis, and to differences in data sources used to derive incidence. Methodologically, the prior study used a state transition simulation model of the natural history of knee osteoarthritis, with transition estimates derived from multiple data sources. In contrast, we used the counting method, which is a more reliable method than the transition method when data are readily available12. Also, the transition to total knee replacement (i.e., incidence) in the Weinstein study was derived from the Osteoarthritis Initiative and the Multicenter Osteoarthritis Study, two relatively selected patient populations. Individuals included in these cohorts either had osteoarthritis at baseline or were at increased risk of developing osteoarthritis. In other words, incidence estimates were limited to the unique setting and limited duration of these two studies that included only patients with osteoarthritis and may not necessarily reflect the general population and temporal trends. In contrast, we used almost complete national data and accounted for geographic variation in incidence and the substantial rise in procedure volumes in recent years. We also accounted for relative mortality differences, which was not the case in the earlier study. Nevertheless, we believe that the main driver of the higher prevalence estimates in our study was the use of complete national data, reflecting the substantial increase in incidence over time.
The implications of our findings are severalfold. First and foremost, our estimates indicate that total joint replacement is surprisingly more prevalent than several chronic diseases that catch the public’s attention. Overall prevalence is similar to stroke (6.8 million) and myocardial infarction (7.6 million) and much higher than heart failure (5.1 million)20. Clearly, living with a total joint replacement is a remarkably common condition in the United States, a trend which is likely to continue in coming decades as a result of the aging of the “baby boomer” generation and improvements in longevity. Even without a further rise in incidence, simply the aging of the population would result in an estimated 11 million individuals with total hip or knee replacement (4 million total hip and 7.4 million total knee) in 2030 (i.e., applying 2010 prevalence to 2030 population estimates21).
Second, although there has been considerable research and policy focus in recent years on issues that surround access to, and costs and outcomes of, total joint replacement (e.g., Centers for Medicare & Medicaid Services bundled payments and inpatient quality reporting initiatives), much of these efforts are limited to the immediate perioperative period22,23. Yet, the majority of individuals with joint replacement have a relatively long life expectancy and will need many years of specialized follow-up care and radiographic assessments. In fact, our findings indicate that the majority (about 70%) of individuals who underwent joint replacement over the last four decades are still alive today. There is a need for the medical profession and the policy makers to recognize and address the lifelong needs of this population.
Third, in contrast to other chronic diseases, there are essentially no evidence-based guidelines (for physicians or for patients) on subacute and chronic care of individuals with joint replacement. A number of common issues remain unresolved, such as the optimal frequency of clinical and radiographic joint replacement follow-up and how antibiotic prophylaxis for other procedures (e.g., dental) should be managed. Additional research is needed to address these important aspects of the long-term management of individuals with joint replacement.
Fourth, with little progress on the horizon for the prevention of osteoarthritis (the main indication for joint replacement) or effective alternative treatments for advanced osteoarthritis, the demand for total joint replacement is likely to continue to increase in coming decades and will be amplified further with a growing population of individuals undergoing revision surgery. Current research funding and surveillance efforts in the United States have not been commensurate with the growing population impact of total joint replacement. There is a need to facilitate research and ongoing surveillance in order to fill important evidentiary gaps regarding the long-term health and health-care needs of individuals with total hip and total knee replacement, to develop effective models of care, to facilitate patient self-management, and to develop evidence-based, patient-centered guidelines.
Our estimates should be interpreted in light of some potential methodological limitations. The validity of our prevalence estimates relies on the representativeness of data used to derive these estimates, specifically, incidence data from the NHDS and SID, and relative mortality and contralateral procedure data derived from a local population. The dearth of data in earlier years is a potential limitation. Although the SID data cover 97% of all U.S. hospital discharges in recent years, including nearly all community, nonrehabilitation hospitals, data from federal and U.S. Department of Veterans Affairs hospitals and from three states were not included, and data from time periods before 1990 were not available, and therefore, needed to be imputed. Our imputation methodology relied on calendar-year, age, and sex-specific data provided by the AHRQ and did not take into account other factors that may have potentially influenced incidence rates, such as insurance status, race, ethnicity, or comorbidities. NHDS was the only data source regarding procedures prior to 1990, and it was not possible to exclude revision surgeries or obtain actual state-level estimates. Therefore, we assumed that the geographic variation in earlier years was similar to patterns observed in later years. Even if this assumption may not be true, the contribution of individuals who received total hip and total knee replacement prior to 1990 into the 2010 prevalence pool (i.e., individuals who were still alive in 2010) is small, and it is unlikely to have unduly influenced the 2010 prevalence estimates. Although the prevalence ranking of individual states in this study is broadly consistent with the incidence rankings based on data from the Medicare population24 (i.e., states with higher incidence rates also have higher prevalence), there are notable differences. For example, when we examined the incidence ranking of states for total knee replacement in 2008 from the Dartmouth Atlas of Health Care, the three states with the highest incidence in the Medicare population were Minnesota, North Dakota, and Montana24. Yet, these three states ranked eleventh, third, and ninth, respectively, in our total knee replacement prevalence ranking (Fig. 4-B). This suggests that the patterns of geographic variation in procedure rates among younger ages may not be the same as the variation for the elderly Medicare population. Additional studies are needed to examine whether this is indeed the case. Of note, there is a growing population of individuals undergoing joint replacement other than total hip and total knee replacement, such as partial hip or partial knee replacement and replacement of other joints. Although they were not included in our prevalence estimates, their health-care needs are in many ways similar to those of total hip and knee replacement patients. There is an estimated 100,000 partial hip replacement procedures in the United States for hip fractures1. These individuals probably have more complicated and costly health-care needs. Regarding relative mortality data post-total hip and knee replacement, our estimates are almost identical to patterns observed for other large cohorts or national data. Although the local population is less ethnically diverse than the entire U.S. population, mortality rates are similar25,26. Similarly, the contralateral procedure estimates are consistent with those in the published literature27. Finally, state-specific prevalence estimates may not be accurate in certain states with relatively high rates of migration into and out of the state.
In conclusion, the high prevalence of arthritis, the growing demand for increased mobility and quality of life, and the success of joint replacement surgery over the recent decades has resulted in an estimated 7 million individuals living with artificial hips and knees in the United States. Total joint replacement benefits the daily lives of most of these individuals. However, the high prevalence of joint replacement also creates a need to effectively manage the long-term health-care requirements of this population, and to reduce the burden of subsequent complications and reoperations. These needs can be addressed through targeted research and implementation of effective, evidence-based policies.
Appendix
Incidence (Procedure Volume) Data Sources
Two data sources were used to obtain incidence data. For the period of 1990 to 2010, we collaborated with the AHRQ and relied on the SID to estimate total hip and knee replacement procedure counts by calendar year, state, sex, and single-year age groups. SID are a set of databases that include nearly all inpatient discharge data from states participating in the HCUP1,28. We used the SID instead of the Nationwide Inpatient Sample (NIS) in order to reduce sampling error in incidence estimates while capturing state-specific variations in incidence. The SID data collection dates back to 1988, and the number of participating states has increased over time. By 2010, the SID included forty-seven states and about 96% of all U.S. community, nonrehabilitation hospital discharges, regardless of payer (including persons covered by Medicare, Medicaid, and private insurance as well as the uninsured). We identified all hospital discharges using the ICD-9 (International Classification of Diseases, Ninth Revision) codes 81.51 (primary hip replacement) and 81.54 (primary knee replacement). Partial hip replacement (81.52), revision hip replacement (81.53), and revision knee replacement (81.55) procedures were excluded because joint replacement is an irreversible procedure, and a person with joint replacement remains in the prevalence pool irrespective of the number of subsequent revision surgeries.
Contralateral procedures are common for both total hip and knee replacement. In order to avoid the double counting of individuals who had contralateral primary procedures at different hospitalizations, the SID discharge counts were deflated using calendar year, sex, age, and procedure-specific deflation estimates derived from the published literature27 and population-based data from Olmsted County, Minnesota, population. Briefly, owing to the infrastructure created by the Rochester Epidemiology Project29,30, we were able to longitudinally follow all residents with an initial total hip or total knee replacement and capture all subsequent total joint replacement surgeries on contralateral and ipsilateral joints. For each decade, sex, and age-group stratum, we calculated the percentage of individuals who previously had a procedure on the contralateral joint. Our findings indicated that the percentage of contralateral primary procedures at different hospitalizations was similar among males and females. The percentage of contralateral total knee replacement was higher in elderly individuals than in younger individuals, whereas the percentage of contralateral total hip replacement was lower in elderly individuals than in younger individuals. We also observed a calendar-year effect, i.e., contralateral procedures increased over time. In order to account for these trends, the SID procedure counts were deflated by appropriate age-group and time-period-specific deflation factors. Deflation factors for total hip replacement (and corresponding age group) ranged between 0.102 (eighty years or older) and 0.292 (sixty to sixty-nine years) in 1990 to 1999, and 0.184 (eighty years or older) and 0.245 (fifty to fifty-nine years) in 2000 to 2010. Similarly, deflation factors for total knee replacement (and corresponding age group) ranged between 0.00 (less than fifty years) and 0.255 (eighty years or older) for 1990 to 1999, and 0.169 (less than fifty years) and 0.299 (seventy to seventy-nine years) in 2000 to 2010.
The states participating in the SID increased over time from eleven states in 1990 to forty-seven states in 2010. Procedure counts for years prior to each state’s inclusion into the SID were estimated with use of data from all available states during 1990 to 2010. Separate Poisson regression models for total hip replacements and for total knee replacements, including state, sex, age, and calendar-year terms, were used to produce these estimates. Age and calendar year were modeled using smoothing splines to allow for flexible, nonlinear relationships with procedure counts, and the state, sex, age, and calendar-year-specific populations were included as an offset to adjust for the varying population size associated with each procedure count. The predicted values from these models were used to estimate the procedure counts prior to each state’s inclusion into the SID. No SID data were available from three states (Alabama, Delaware, and Idaho) throughout the entire time period. The numbers of procedures in Alabama, Delaware, and Idaho were estimated by applying the Dartmouth Atlas ratios24 for these states to the procedure rates from two other large states (Florida and New York) with continuous SID data throughout the entire 1990 to 2010 period.
Incidence rate estimates for some state, sex, age, and calendar-year-specific intervals were based on small numbers, and their variability was large. To increase the stability of these estimates, gradient boosting machine methods were used13. These machine-learning methods smoothed the trends in incidence rates according to state, sex, age, and calendar year without requiring restrictive assumptions regarding the functional forms of these effects. These models were chosen to avoid concerns about the validity of our estimates related to the modeling assumptions. However, when generalized additive models with smoothing splines were used in place of gradient boosting machines, the resulting prevalence estimates were nearly identical.
For the 1969 to 1989 period, we relied on the NHDS to estimate the annual number of total hip and total knee replacement procedures by calendar year, four major census regions, sex, and single-year age groups14. NHDS was a national probability survey of inpatient discharges from nonfederal, short-stay hospitals in the United States. Total hip and knee replacement procedures were identified using the ICD-8 (Eighth Revision) and ICD-9 codes 81.4, 81.41, and 81.54 (knee), and 81.5, 81.51, and 81.59 (hip), and procedure counts were weighted to produce national estimates. In order to estimate the numbers of procedures in individual states, we assumed that the state-specific variation in incidence between 1969 and 1989 followed the same pattern as in subsequent years. Using 1990 to 2000 ratios derived from the SID and the Dartmouth Atlas24, we distributed the procedure counts to individual states. It was not possible to exclude revision procedures for the 1969 to 1989 period because ICD-9 revision codes were first introduced after October 1989.
General Population Data
Calendar-year, state, sex, and single year of age-specific U.S. population estimates for the 1969 to 2010 period were obtained from the United States Census Bureau31. Historical population mortality data were obtained from the NCHS vital statistics16. We compiled total population counts and the numbers of deceased individuals by calendar year, state, sex, and single-year age groups.
Mortality Data
In addition to incidence, prevalence of total hip and total knee replacement depends on relative patient mortality following surgery, which is not the same as mortality in the general population. Several prior studies suggest that individuals who underwent total hip and knee replacement have lower mortality rates than the general population, attributed mainly to the selection of healthier individuals for surgery17-19. These findings indicate that relative mortality differences should be accounted for in prevalence estimates. We estimated procedure-specific relative death rates (observed versus expected deaths) by the number of years after surgery, sex, and age group using four decades of population data. Estimated relative death rates ranged between 0.65 and 1.18 (for the first year post-surgery) and 0.99 and 1.74 (for fifteen years post-surgery) for total hip replacement, and between 0.40 and 0.48 (for the first year post-surgery) and 0.99 and 1.32 (for fifteen years post-surgery) for total knee replacement. These estimates are consistent with those of previous patient mortality studies from other populations17-19. Relative mortality ratios were then applied to calendar-year, state, sex, and single year of age-specific mortality data obtained from the NCHS.
Estimation of 2010 Prevalence
The 2010 prevalence of total hip and total knee replacement was estimated using the counting method12,13. This direct estimation method counts the number of individuals with a history of total hip and total knee replacement known to be alive (i.e., survivors) on a certain date and adjusts for population mortality and relative mortality differences. Because the prevalence of total hip and total knee replacement was essentially “0” before 1969, no assumptions were needed for the period prior to 1969. We further estimated the prevalence of individuals by duration of time since the initial total hip and knee replacement procedure, i.e., percentage of prevalent individuals who were less than ten years from their initial procedure, ten to twenty years from their procedure, and greater than twenty years from their procedure.
We also estimated the prevalence among individuals who had both hip and knee replacement procedures, i.e., procedures on more than one joint, using estimates from Olmsted County, Minnesota, and the published literature27 (Table II). Briefly, we identified all residents with a history of both hip and knee replacement in 2008. We then calculated the age and sex-specific percentage (column A) and population prevalence (column B) of prevalent individuals with both procedures and applied them to the total population of United States in 2010. Two estimates were obtained (see the last two columns in Table II): one based on the estimated percentage of prevalent cases and the other, based on estimated population prevalence.
Testing and Validation of the Estimation Procedures
We validated our counting method by comparing the estimated prevalence in Minnesota with actual prevalence among eighty-year-old individuals. We first identified all Olmsted County residents who were eighty years old in 2008 and who had a history of hip and knee replacement in their medical records. The comparisons revealed that the estimated prevalence (based on the counting method) was close to the upper limit of the 95% confidence intervals (CIs) for the actual prevalence for both total hip replacement (7.6% [95% CI, 5.3% to 9.8%] compared with an estimated 9.5% at age eighty) and total knee replacement (9.8% [95% CI, 7.3% to 12.3%] compared with an estimated 12.5% at age eighty). We also assessed the impact of relative mortality estimates by producing 2010 prevalence estimates after ignoring the relative mortality differences (i.e., assuming that the mortality of individuals with total hip and knee replacement is identical to that of the general population). This assumption resulted in negligible differences in the overall prevalence estimates. Unless otherwise stated, all prevalence estimates were calculated with the total U.S. population as the denominator.
Acknowledgments
Note: The authors thank the HCUP Partner States that voluntarily contribute their state data to the HCUP, without whom the project and data would not exist. https://www.hcup-us.ahrq.gov/partners.jsp
Footnotes
Investigation performed at the Department of Health Sciences Research and the Department of Orthopedic Surgery, Mayo Clinic, Rochester, Minnesota
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. In addition, one or more of the authors has a patent or patents, planned, pending, or issued, that is broadly relevant to the work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Steiner C, Andrews R, Barrett M, Weiss A. HCUP Projections: Mobility/Orthopedic Procedures 2003 to 2012. 2012. HCUP Projections Report # 2012-03. 2012 Sep 20. U.S. Agency for Healthcare Research and Quality. http://hcup-us.ahrq.gov/reports/projections/2012-03.pdf. Accessed 2015 May 27.
- 2.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009. October;467(10):2606-12. Epub 2009 Apr 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012. September 26;308(12):1227-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ong KL, Mowat FS, Chan N, Lau E, Halpern MT, Kurtz SM. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop Relat Res. 2006. May;446(446):22-8. [DOI] [PubMed] [Google Scholar]
- 5.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007. April;89(4):780-5. [DOI] [PubMed] [Google Scholar]
- 6.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005. July;87(7):1487-97. [DOI] [PubMed] [Google Scholar]
- 7.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009. January;91(1):128-33. [DOI] [PubMed] [Google Scholar]
- 8.Katz BP, Freund DA, Heck DA, Dittus RS, Paul JE, Wright J, Coyte P, Holleman E, Hawker G. Demographic variation in the rate of knee replacement: a multi-year analysis. Health Serv Res. 1996. June;31(2):125-40. [PMC free article] [PubMed] [Google Scholar]
- 9.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003. October 2;349(14):1350-9. [DOI] [PubMed] [Google Scholar]
- 10.Slover J, Zuckerman JD. Increasing use of total knee replacement and revision surgery. JAMA. 2012. September 26;308(12):1266-8. [DOI] [PubMed] [Google Scholar]
- 11.Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, Wright J, Katz JN, Losina E. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am. 2013. March 6;95(5):385-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gail MH, Kessler L, Midthune D, Scoppa S. Two approaches for estimating disease prevalence from population-based registries of incidence and total mortality. Biometrics. 1999. December;55(4):1137-44. [DOI] [PubMed] [Google Scholar]
- 13.Hastie T, Tibshirani R, Friedman JH. The elements of statistical learning. Chapter 10. 2nd ed. New York: Springer; 2009. [Google Scholar]
- 14.Centers for Disease Control and Prevention. National Hospital Discharge Survey. http://www.cdc.gov/nchs/nhds.htm. Accessed 2015 May 27.
- 15.United States Census Bureau. Population and housing unit estimates. [12/9/2013]; Available from: http://www.census.gov/popest/index.html. 2013 Dec 9.
- 16.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed mortality files 1968-2010. CDC WONDER Online Database. http://wonder.cdc.gov/cmf-icd8.html. 2013 Nov 6.
- 17.Lie SA, Engesaeter LB, Havelin LI, Gjessing HK, Vollset SE. Mortality after total hip replacement: 0-10-year follow-up of 39,543 patients in the Norwegian Arthroplasty Register. Acta Orthop Scand. 2000. February;71(1):19-27. [DOI] [PubMed] [Google Scholar]
- 18.Pedersen AB, Baron JA, Overgaard S, Johnsen SP. Short- and long-term mortality following primary total hip replacement for osteoarthritis: a Danish nationwide epidemiological study. J Bone Joint Surg Br. 2011. February;93(2):172-7. [DOI] [PubMed] [Google Scholar]
- 19.Robertsson O, Stefánsdóttir A, Lidgren L, Ranstam J. Increased long-term mortality in patients less than 55 years old who have undergone knee replacement for osteoarthritis: results from the Swedish Knee Arthroplasty Register. J Bone Joint Surg Br. 2007. May;89(5):599-603. [DOI] [PubMed] [Google Scholar]
- 20.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013. January 1;127(1):e6-245. Epub 2012 Dec 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United States Census Bureau. 2012 National population projections. 2014. https://www.census.gov/population/projections/data/national/2012.html. 2014 Mar 1.
- 22.Ghomrawi HMK, Schackman BR, Mushlin AI. Appropriateness criteria and elective procedures—total joint arthroplasty. N Engl J Med. 2012. December 27;367(26):2467-9. [DOI] [PubMed] [Google Scholar]
- 23.Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation (YNHHSC/CORE). Centers for Medicare & Medicaid Services (CMS). 2013 Measures Update and Specifications: Elective Primary Total Hip Arthroplasty (THA) And/Or Total Knee Arthroplasty (TKA) Risk-Standardized Complication Measure (Version 2.0). 2013. March https://www.stratishealth.org/documents/Hip_Knee_Meas_Specs_2013.pdf. Accessed 2015 May 27.
- 24.The Dartmouth Atlas of Health Care online tools: Surgical Procedures: Inpatient Knee Replacement and Inpatient Hip Replacement State Level Trends data. 2013 [cited 2013 April 1]; Available from: http://www.dartmouthatlas.org/.
- 25.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012. December;87(12):1202-13. Epub 2012 Nov 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012. February;87(2):151-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shao Y, Zhang C, Charron KD, Macdonald SJ, McCalden RW, Bourne RB. The fate of the remaining knee(s) or hip(s) in osteoarthritic patients undergoing a primary TKA or THA. J Arthroplasty. 2013. December;28(10):1842-5. [DOI] [PubMed] [Google Scholar]
- 28.HCUP SID Database Documentation. Healthcare Cost and Utilization Project (HCUP). 2014. May Agency for Healthcare Research and Quality. www.hcup-us.ahrq.gov/db/state/siddbdocumentation.jsp. Accessed 2015 May 28.
- 29.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol. 2011. May 1;173(9):1059-68. Epub 2011 Mar 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Pankratz JJ, Brue SM, Rocca WA. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012. December;41(6):1614-24. Epub 2012 Nov 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.United States Census Bureau. Population estimates and projections. http://www.census.gov/popest/index.html. Accessed 2013 Dec 9.