Introduction
Based on the most recent data from 2007 to 2011, the United States (US) Surveillance, Epidemiology and End Results (SEER) Program reports an age-adjusted incidence rate of 7.9 per 100,000 people per year for liver and intrahepatic bile duct cancer, with a corresponding death rate of 5.8 per 100,000 people per year, resulting in a relatively high mortality ratio of 73%. Examination of trends in incidence from the SEER database shows that the age-adjusted incidence rate per year is rising and almost doubled between 1992 and 20111. Similar trends have been observed in Canada, Australia, New Zealand, and Western Europe 2. Further, despite the recent decrease in new cases in Japan, the Philippines and China, East Asia has the highest overall incidence rate in the world2. After East Asia, sub-Saharan Africa has the next highest incidence of hepatocellular carcinoma (HCC) in the world, but due to the limited medical and research infrastructure in this region, data on trends in incidence is very limited3.
Treatment of HCC and cholangiocarcinoma (CCA) is most effective for patients with early stage, localized disease while treatment of advanced liver cancer is merely palliative in nature. Unfortunately, in the US, only 20 to 30% of HCC and CCA cases are diagnosed with early stage disease4, 5. In Taiwan and Japan, where there are comprehensive nationwide programs for early diagnosis and surveillance of individuals at risk for HCC from chronic hepatitis B virus (HBV) and hepatitis C virus (HCV) infection, approximately 70% of HCCs are diagnosed at very early or early stages, resulting in 5 year survival estimates of 50–70%6. In the US, CCA is often diagnosed in advanced stages when disease is incurable7. Thus national and international efforts to reduce the burden or morbidity and mortality from HCC and CCA need to focus on identification of the population at risk and aggressive surveillance using effective screening tools.
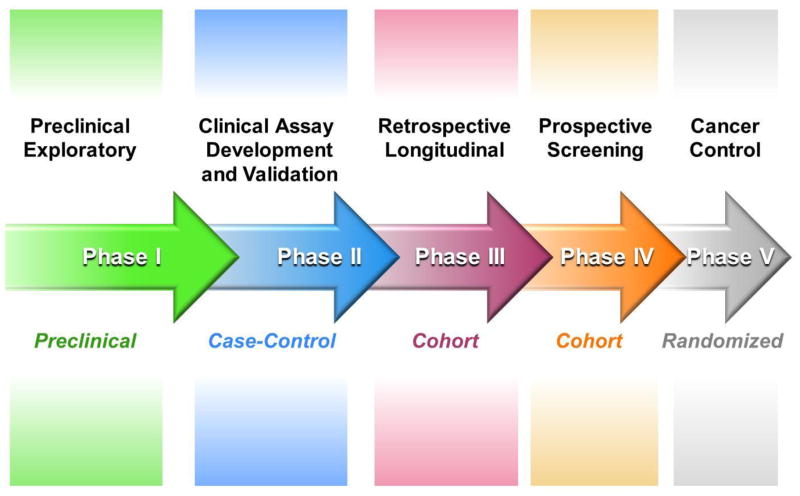
The emerging evidence suggests that biomarkers are optimally used as a complement, rather than a replacement for imaging studies. Biomarkers uniquely may be elevated before there is any evidence of imaging abnormalities and may also guide consideration of what the primary tumor type is, such as HCC versus CCA, or mixed HCC-CCA. Cancer biomarker development is described by Pepe and colleagues as a 5-phase process in which each stage is characterized by study design application (Figure 1)8, 9. In this review we provide an update on the current status of liver and biliary cancer surveillance and describe recent efforts that are taking advantage of novel technologies in next generation DNA sequencing, genome wide methylation and proteomic studies, and advances in metabolomics to usher in a new era of biomarker development. The novel biomarkers in development will hopefully result in substantial improvements in both surveillance and diagnosis of HCC and CCA. Biomarkers discussed in this review, their current stage in biomarker development and clinical applicability are summarized in Table 1 for HCC and in Table 2 for CCA.
Figure 1.
Phases of cancer biomarker development
Table 1.
Currently used and novel biomarkers for surveillance of HCC
| Biomarker | Source | Phase of biomarker development | Application | Suggested cutoffs and clinical utility |
|---|---|---|---|---|
| AFP | Serum | 5 | Risk stratification Diagnosis Prognosis |
10.9 ng/mL for early detection1 59 ng/mL may be optimal for HCV infected patients2 Practice is moving towards looking at AFP measurement trends over time and using models for risk stratification. |
| AFP-L3% | Serum | 2 | Risk stratification Diagnosis Prognosis |
1.7%1 |
| DCP | Serum | 2 | Risk stratification Diagnosis Prognosis |
125 mAU/mL3 |
| OPN | Plasma | 2 | Early detection | 91 ng/mg4 |
| GP73 | Serum | 2 | Early detection Prognosis |
150 μg/L5 |
| Dickkopf-1 | Serum | 2 | Early detection Prognosis |
2.153 ng/mL6 |
| Axl | Serum | 2 | Early detection | 14.05 ng/mL7 |
| Micro-RNA | Serum, plasma or urine | 2 | Diagnosis Prognosis |
NA |
| DNAJB1-PRKACA | Tissue and potentially serum | 1 | Diagnosis of fibrolamellar HCC subtype | NA |
Table 2.
Currently used and novel biomarkers for surveillance of CCA
| Biomarker | Source | Phase of biomarker development | Application | Suggested cutoffs and clinical utility |
|---|---|---|---|---|
| CA19-9 | Serum | 2 | Diagnosis Prognosis |
129 U/mL8,9 |
| CEA | Serum | 2 | Diagnosis | 5.2 ng/mL10 |
| CYFRA 21-1 | Serum or plasma | 2 | Diagnosis Prognosis |
1.5 ng/mL11 |
| MUC5AC | Serum or bile | 2 | Diagnosis Prognosis |
Serum: 10.5 ng/mL12 Bile: 6.25 ng/mL13 Serum-to-bile ratio: 0.8513 |
| Conventional cytology | Bile duct brushings or fine needle aspiration | 4 | Diagnosis | Benign Equivocal (atypical or suspicious) Malignant |
| FISH assay (UroVysion™) | Bile duct brushings | 4 | Diagnosis | Negative: 2 copies of each probe Positive: ≥5 cells with polysomy (>2 copies of at least 2 probes excluding cells with tetrasomy) Equivocal: ≥10 cells with trisomy (3 copies of a single probe) or ≥10 cells with tetrasomy (4 copies of each probe). Tetrasomy can represent replicating cells14–16. |
| PB FISH assay | Bile duct brushings | 3 | Diagnosis | Negative: 2 copies of each probe Positive: ≥5 cells with polysomy (>2 copies of at least 2 probes excluding cells with tetrasomy) Equivocal: ≥10 cells with trisomy (3 copies of a single probe) or ≥10 cells with tetrasomy (4 copies of each probe). Tetrasomy can represent replicating cells14–16. |
| Methylated BMP-3 | Bile | 1 | Early detection | NA |
Marrero JA, Feng Z, Wang Y, Nguyen MH, Befeler AS, Roberts LR, Reddy KR, Harnois D, Llovet JM, Normolle D, Dalhgren J, Chia D, Lok AS, Wagner PD, Srivastava S, Schwartz M. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology 2009;137:110–8.
Gopal P, Yopp AC, Waljee AK, Chiang J, Nehra M, Kandunoori P, Singal AG. Factors that affect accuracy of alpha-fetoprotein test in detection of hepatocellular carcinoma in patients with cirrhosis. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association 2014;12:870–7.
Marrero JA, Su GL, Wei W, Emick D, Conjeevaram HS, Fontana RJ, Lok AS. Des-gamma carboxyprothrombin can differentiate hepatocellular carcinoma from nonmalignant chronic liver disease in american patients. Hepatology 2003;37:1114–21.
Shang S, Plymoth A, Ge S, Feng Z, Rosen HR, Sangrajrang S, Hainaut P, Marrero JA, Beretta L. Identification of osteopontin as a novel marker for early hepatocellular carcinoma. Hepatology 2012;55:483–90.
Cao FF, Yu S, Jiang ZY, Bao YX. Diagnostic accuracy of Golgi protein 73 in primary hepatic carcinoma using ELISA: a systematic review and meta-analysis. Clinical laboratory 2014;60:587–97.
Shen Q, Fan J, Yang XR, Tan Y, Zhao W, Xu Y, Wang N, Niu Y, Wu Z, Zhou J, Qiu SJ, Shi YH, Yu B, Tang N, Chu W, Wang M, Wu J, Zhang Z, Yang S, Gu J, Wang H, Qin W. Serum DKK1 as a protein biomarker for the diagnosis of hepatocellular carcinoma: a large-scale, multicentre study. The Lancet. Oncology 2012;13:817–26.
Reichl P, Fang M, Starlinger P, Staufer K, Nenutil R, Muller P, Greplova K, Valik D, Dooley S, Brostjan C, Gruenberger T, Shen J, Man K, Trauner M, Yu J, Gao CF, Mikulits W. Multicenter analysis of soluble Axl reveals diagnostic value for very early stage hepatocellular carcinoma. International journal of cancer. Journal international du cancer 2014.
Charatcharoenwitthaya P, Enders FB, Halling KC, Lindor KD. Utility of serum tumor markers, imaging, and biliary cytology for detecting cholangiocarcinoma in primary sclerosing cholangitis. Hepatology 2008;48:1106–17.
Levy C, Lymp J, Angulo P, Gores GJ, Larusso N, Lindor KD. The value of serum CA 19–9 in predicting cholangiocarcinomas in patients with primary sclerosing cholangitis. Digestive diseases and sciences 2005;50:1734–40.
Siqueira E, Schoen RE, Silverman W, Martin J, Rabinovitz M, Weissfeld JL, Abu-Elmaagd K, Madariaga JR, Slivka A. Detecting cholangiocarcinoma in patients with primary sclerosing cholangitis. Gastrointestinal endoscopy 2002;56:40–7.
Chapman MH, Sandanayake NS, Andreola F, Dhar DK, Webster GJ, Dooley JS, Pereira SP. Circulating CYFRA 21-1 is a Specific Diagnostic and Prognostic Biomarker in Biliary Tract Cancer. Journal of clinical and experimental hepatology 2011;1:6–12.
Ruzzenente A, Iacono C, Conci S, Bertuzzo F, Salvagno G, Ruzzenente O, Campagnaro T, Valdegamberi A, Pachera S, Bagante F, Guglielmi A. A novel serum marker for biliary tract cancer: diagnostic and prognostic values of quantitative evaluation of serum mucin 5AC (MUC5AC). Surgery 2014;155:633–9.
Danese E, Ruzzenente O, Ruzzenente A, Iacono C, Bertuzzo F, Gelati M, Conci S, Bendinelli S, Bonizzato G, Guglielmi A, Salvagno GL, Lippi G, Guidi GC. Assessment of bile and serum mucin5AC in cholangiocarcinoma: diagnostic performance and biologic significance. Surgery 2014;156:1218–24.
Kipp BR, Stadheim LM, Halling SA, Pochron NL, Harmsen S, Nagorney DM, Sebo TJ, Therneau TM, Gores GJ, de Groen PC, Baron TH, Levy MJ, Halling KC, Roberts LR. A comparison of routine cytology and fluorescence in situ hybridization for the detection of malignant bile duct strictures. The American journal of gastroenterology 2004;99:1675–81.
Barr Fritcher EG, Kipp BR, Halling KC, Clayton AC. FISHing for pancreatobiliary tract malignancy in endoscopic brushings enhances the sensitivity of routine cytology. Cytopathology: official journal of the British Society for Clinical Cytology 2014;25:288–301.
Barr Fritcher EG KB, Voss JS, Brankley SM, Keeney ME, Campion MB, Pestova EV, Sokolova IA, Roberts LR, Gores GJ, ClaBarr Fritcher, E. Guyton AC, Halling KC. The Development of a Tailored Pancreatobiliary Fluorescence in situ Hybridization (FISH) Assay to Improve Detection of Malignancy in Pancreatobiliary Brushings. The Journal of Molecular Diagnostics 2013;15:909.
Hepatocellular carcinoma
HCC is the most common malignancy of the liver. Current practice guidelines from the American Association for the Study of Liver Diseases (AASLD) recommend surveillance for HCC in patients with an expected risk of HCC exceeding 1.5% per year or 0.2% per year in patients with chronic HBV. Based on these recommendations, surveillance for HCC should be offered to all patients with cirrhosis and to hepatitis B carriers who have a family history of HCC, are Asian-born males 40 years or older, are Asian females 50 years or older, or African-born individuals 20 years or older. Individuals with immune active chronic HBV and those with coinfection with HCV or HIV or who have other chronic liver diseases should also be enrolled in surveillance programs10, 11.
Currently used biomarkers: AFP, AFP-L3 and DCP
World-wide, the commonest modalities used for surveillance for HCC in at risk individuals are liver ultrasound and serum alpha fetoprotein (AFP) measurement. AFP is a glycoprotein produced by fetal liver and yolk sac; serum levels are high in utero but normalize to adult values rapidly after birth. High serum AFP values have been shown to occur in different cancers, including HCCs and germ cell tumors. The use of AFP as a screening modality has been controversial, particularly in low to medium incidence regions, but is widespread in high incidence countries, where it is incorporated into most national and regional guidelines. The main objection to the use of AFP is its low sensitivity of only 20–30% for the detection of HCC at an early stage, when it is most amenable to curative treatment. The sensitivity of AFP rises to 50–60% for the detection of intermediate to advanced stage disease12–14. Proponents of the use of AFP argue that while most studies evaluating the performance of AFP have evaluated it in the cross-sectional setting, experienced practitioners typically follow and act on trends and variations in AFP levels, rather than individual measurements alone15. Further, the combination of AFP with ultrasound improves the likelihood of detection of the more diffuse or infiltrating HCCs that do not develop as distinct nodules.
In addition to the AFP, other serum markers in clinical use for HCC surveillance include the lens culinaris binding subfraction of AFP (AFP-L3%) and the des gamma carboxyprothrombin (DCP). AFP-L3 is a glycosylated variant of AFP abnormally increased in HCC. DCP, also known as protein induced by vitamin K absence II (PIVKA-II), is a form of prothrombin generated when there is an acquired defect in post-translational carboxylation. These assays are routinely used in Japan and other Asian countries and are approved for use in risk stratification for HCC by the US Food and Drug Administration. AFP-L3 and DCP have been shown to increase sensitivity and specificity of AFP in diagnosing HCC12, 16, 17.
A number of models have been developed which integrate the results of biomarker assays with different patient clinical and laboratory characteristics to enhance the diagnostic accuracy of biomarkers in specific patient settings. The GALAD model by Johnson et al. includes gender, age, AFP-L3, AFP and DCP as predictors of risk for HCC in the setting of chronic liver disease. This model has been has been validated and has shown consistency in stratifying patients based on risk of HCC18. A similar algorithm, known as BALAD-2, was developed by the same group for accurate prognostication of patients with HCC19. El-Serag et al. recently developed another model using platelet count, alanine aminotransferase (ALT), age and AFP to predict risk for HCC in patients with HCV-induced cirrhosis. In general, patients with high AFP who also had decreased platelet count, decreased ALT, or increased age showed higher risk of HCC. Their model-predicted probability levels showed a very close relationship with raw frequencies of HCC that only deviated in risks higher than 90% where there is no practical significance. This model is yet to be tested on other populations with liver disease due to causes other than HCV and in populations outside of the Veterans Affair (VA) Health system where males predominate20. The recently published ADRESS model can be used for predicting HCC probability in patients with cirrhosis using the variables of age, diabetes, race, cirrhosis etiology, sex and severity of liver dysfunction. Although no biomarkers are included in the model, it can possibly stratify patients with cirrhosis into groups based on their potential surveillance program benefit21. Finally, AFP and DCP biomarkers also have utility in combination with clinical factors for predicting recurrence of HCC after liver transplantation22–24.
Ultrasound
Ultrasound is a widely used tool for both diagnosis and surveillance of various liver and cholestatic diseases and is currently established for surveillance of early stage HCC. AASLD Guidelines recommend HCC surveillance with liver ultrasound every 6 months11. Ultrasound offers clinicians a safe, noninvasive and low cost real-time imaging tool that is widely available. However, ultrasound efficacy is operator dependent and its performance in detecting lesions, especially smaller ones, is impaired. This becomes even more problematic given the increasing prevalence of obesity-related fatty liver disease and cirrhosis in North America, Europe and Asia. Regenerative nodules in cirrhotic livers can be confused with neoplastic masses, leading to additional diagnostic test that are more invasive, have increased costs and can unnecessarily increase patient anxiety. Together, these limitations raise a fundamental problem in relying solely on ultrasound for surveillance of HCC.
A meta-analysis on surveillance performance for detecting HCC on cirrhotic patients via ultrasound reported a pooled sensitivity of 94%, specificity of 94% and a summary receiver operator curve (ROC) plot of 98%. However, these numbers were for detecting HCC at any stage of disease. When only looking at studies that reported detection of early HCC as defined by Milan criteria (one nodule <5 cm or 3 nodules each <3 cm and no gross vascular invasion), ultrasound had a pooled sensitivity of 63%. Adding AFP for detection of early stage HCC increased pooled sensitivity to only 69%. Studies that conducted surveillance in 6-month intervals had a pooled sensitivity for detecting early stage HCC of 70% while studies that conducted surveillance on 12-month intervals had pooled sensitivity of 50%25. In contrast to the use of ultrasound in the setting of research studies, it has been shown that the performance of ultrasound is not as impressive in routine clinical use, with only 44% sensitivity for the detection of HCC. However, in combination with AFP, sensitivity was 66%26. Once a new nodule is identified by ultrasound, a diagnostic algorithm is proposed for definitive non-invasive diagnosis using cross-sectional multiphasic contrast imaging with CT or MRI27.
New biomarkers for HCC
Osteopontin
Osteopontin (OPN) is a phosphoprotein that is measurable in plasma and has been shown to be increased in patients with different types of malignancy including HCC28. A recent meta-analysis comparing the diagnostic potential of OPN to AFP showed that OPN had comparable biomarker characteristics to AFP suggesting its utility as a potential biomarker for HCC29. Moreover, OPN levels have shown to be increased up to 12 months prior to HCC diagnosis, making OPN a potential candidate biomarker for early detection of HCC30, 31. However, data on the use of OPN in combination with AFP or other biomarkers is limited.
Golgi protein 73 (GP73)
GP73 is a transmembrane glycoprotein normally found within the Golgi complex. Increased expression of GP73 has been reported in liver disease, particularly in serum of patients with HCC. Wang et al. recently reported that in HCC cells, GP73 is upregulated in response to the inflammatory modulator IL-1β through induction of the transcription factor epithelium-specific ETS (ESE)-1, which in turn directly binds to and transcriptionally activates GP73. These findings potentially provide a link between inflammation and GP73 activation in the development of HCC32. GP73 can be assayed using western immunoblotting or enzyme-linked immunosorbent assay (ELISA). Initial studies using western immunoblotting suggested that GP73 has high accuracy in detecting HCC, with better sensitivity, specificity and accuracy than AFP, and some ELISA based studies have been positive, however, in general, most studies using ELISA had negative results33–37. It has been suggested that GP73-specific antibodies may interfere with the ELISA test. In addition to aiding in surveillance, GP73 has been evaluated as a biomarker for prognosis of patients with HCC. In a study by Bao et al., increased GP73 expression in HCC tissue samples as compared to non-cancer liver tissue samples was associated with more advanced disease and poor prognosis after surgical resection38.
Dickkopf-1 (DKK1)
DKK1 is a secretory antagonist of the Wnt pathway that is normally expressed in embryonic tissue and has been shown to be upregulated in HCC tissues and increased in the serum of HCC patients as compared to cirrhotic and non-cirrhotic controls39. Furthermore, DKK1 had greater sensitivity and specificity than AFP in a Chinese cohort of HCC compared to patients with chronic HBV and cirrhosis controls. Further, the use of DKK1 and AFP together achieved better accuracy for detecting HCC than either test alone40. Indeed, DKK1 (cutoff of 500 pg/mL) and AFP (cutoff of 20 ng/mL) showed better diagnostic performance than AFP combined with DCP or with OPN41. However, a small Australian cohort showed no significant difference in DKK1 serum levels between HCC patients and age matched, cirrhotic, non-cirrhotic, and HBV controls42.
Recent data suggests that HCC patients with increased serum DKK1 may have poorer overall and relapse-free survival than patients with low DKK143, 44. Moreover, Sunagazaka et al. have suggested that DKK1 may be a potential biomarker for diagnosis of HCC with stem cell features45. Serum levels of DKK1 may have a role in detecting early HCC in patients with negative AFP levels and in defining prognosis for patients with HCC, but further validation using larger cohorts in other populations is needed to confirm the utility of DKK1 in all populations at risk of developing HCC.
Axl
Axl is a receptor tyrosine kinase that has been shown to be overexpressed in many different cancer types, including HCC and to predict poor survival of patients with breast cancer, lung cancer and mesothelioma. Binding of to the extracellular domain (ECD) of Axl to its ligand, growth-arrest specific protein 6, leads to the phosphorylation of downstream oncogenic signaling molecules. Proteolytic processing of the ECD results in the release of an 80 kDa soluble variant of Axl (sAxl) that can be detected in serum. Release of sAxl has been shown to reflect the levels of total Axl in HCC cell lines. A study comparing serum levels of sAxl in patients with HCC to healthy and cirrhotic controls reported a significant increase in patients with HCC, specifically in patients with early stage disease. Patients with breast, ovarian or colorectal cancers and patients with liver metastasis of colorectal cancer showed no changes in serum sAxl levels46. Also, there was no apparent difference between serum sAxl levels of healthy controls and cirrhosis patients. Using cutoffs of 14.05 ng/mL for Axl and 20 ng/mL for AFP, serum Axl outperformed AFP in detecting very early HCC and discriminating very early HCC from liver cirrhosis46.
Micro-RNAs and long non-coding RNAs
With the recent advances in microarray and Next Generation Sequencing technology, microRNAs (miRNAs) and long non-coding RNAs (lnc-RNAs) have been shown to have both diagnostic and therapeutic potential for many diseases including cancer. Increased micro-RNA 21 (miR-21) serum levels have been demonstrated in patients with HCC as compared to chronic hepatitis and normal controls. Although serum miR-21 levels have shown high sensitivity, its specificity is low limiting its effectiveness as a sole marker in diagnosing HCC47. The micro-RNA-200 family has recently been studied in HCC specimens and cirrhosis liver specimens and showed significant downregulation, especially of miR-200a and miR-200b48. Serum micro-RNA 101 (miR-101) and micro-RNA 18a (miR-18a) have also been shown to be increased in HCC patients, making these markers potentially useful for surveillance of HCC in patients with HBV49,50. There are a large number of other miRNAs and lncRNA under evaluation as biomarkers for HCC, however, their utility has not been completely elucidated and the potential of these newer markers remains to be fully explored.
Fibrolamellar HCC
Due to the lack of recognition of patient risk and consequent absence of surveillance, HCCs occurring in non-cirrhotic livers are typically diagnosed at later stages of disease than those developing in patients with underlying cirrhosis. Fibrolamellar HCC is a subtype of HCC that usually develops in noncirrhotic livers and is characterized by highly metastatic behavior, including a propensity to lymph node metastases. Fibrolamellar HCC is traditionally identified by its hypointense central scar on T2-weighted MRI and radiating septa, central calcifications or necrosis. On contrast-enhanced MRI, arterial hyperenhancement of the lesion minus the central scar is characteristic51. Most notably, fibrolamellar HCCs have recently been shown to bear a characteristic fusion protein DNAJB1-PRKACA which potentially has significant diagnostic and therapeutic relevance52–55. Serum AFP is usually not elevated in fibrolamellar HCC, despite the fact that most fibrolamellar HCCs are diagnosed at very advanced stages56.
Cholangiocarcinoma
Cholangiocarcinoma (CCA) can be subclassified into intrahepatic (iCCA), perihilar (pCCA), and distal cholangiocarcinomas (dCCA) based on their anatomic location. Patients with perihilar or distal CCA commonly present with symptoms of biliary tract obstruction such as jaundice, pale stools, dark urine or pruritus, while the clinical presentation of iCCA is non-specific. Patients with advanced iCCA may present with weight loss, malaise, abdominal discomfort, jaundice, hepatomegaly, night sweats or a palpable liver mass57. However, patients with early iCCAs usually have no symptoms; thus it is not uncommon for early iCCAs to be diagnosed incidentally during workup of other diseases. Moreover, it has been shown that iCCA incidence rate is increasing although prognosis remains poor7.
Established risk factors for CCA include primary slcerosing cholangitis (PSC), choledochal cystic disease, hepatobiliary liver flukes and Caroli’s disease, but account for less than a third of CCA cases. Although there is lack of prospective data, patients with PSC have a lifetime prevalence of CCA of approximately 5–10% and a 5-year survival rate of less than 10% and may benefit from cancer surveillance58–60. Surveillance guidelines for early detection of sporadic CCA are yet to be established. This is primarily due to the rarity of cholangiocarcinoma and the lack of data on at-risk populations that would benefit from surveillance. Risk factors for intrahepatic cholangiocarcinoma are similar to those for HCC but with weaker associations. These risk factors include cirrhosis, chronic viral hepatitis, obesity, diabetes and excessive alcohol use61. The recent AASLD guidelines on PSC discussed surveillance but did not make explicit recommendations due to a lack of evidence58.
In 2011, Razumilava et al. recommended surveillance of PSC patients with annual MRI and MRCP or ultrasound and CA19-9. If dominant strictures are found, they recommend ERCP with epithelial brushings using conventional cytology and the UroVysion™ Fluorescence in situ hybridization (FISH) assay and more recently developed Pancreatobiliary FISH assay62. Needless to say, these surveillance recommendations are both invasive and costly, but are currently the most effective strategy for detecting early CCA.
An important consideration in discussions of the feasibility of surveillance for CCA is the concept of aerodigestive cancer or pan-cancer assays. Aerodigestive cancers are the cancers arising from the lungs and upper respiratory tract ranging through the GI tract to the rectum, which have the potential to shed cells that are collected in the digestive tract; these include squamous cell head and neck cancer, lung cancer, esophageal cancer, gastric cancer, CCA, pancreas cancer, small intestinal cancer, and colon cancer. While most of these cancers are relatively uncommon and screening for the individual cancers would not be justified based on their low incidence, the high incidence of colon cancer justifies stool- or blood-based screening. If it is possible to identify specific biomarkers that are characteristic of the other cancer sites, they can potentially be effectively incorporated into a multi-cancer detection panel.
Imaging modalities of utility in the surveillance of PSC patients for CCA and the diagnosis and follow up of CCA patients include MRI/MRCP, ERCP, EUS, and PET-CT scanning. As with HCC, these modalities are critical for accurate assessment of disease presence and severity and they are complemented but not usurped by the advances in diagnostic biomarker technology. Increasingly, biomarkers are providing clues to tumor heterogeneity and allowing individualization and personalization of therapy for CCA, such as by the identification of isocitrate dehydrogenase (IDH) 1 and 2 mutations and fibroblast growth factor receptor 2 (FGFR2) fusions 63–66. Imaging, particularly MRI/MRCP, endoscopic retrograde cholangiopancreatography (ERCP), and endoscopic ultrasound (EUS) also serves as a guide and tool for sampling tumors for tissue through cytology brushing, core needle, or fine needle aspiration biopsies. While PET-CT scanning has not proved to be of substantial utility in HCC, it has been shown to be of utility in the staging of CCA and identification of postsurgical recurrence and distant metastases.
CA19-9 and CEA
Carbohydrate antigen 19-9 (CA19-9) and carcinoembryonic antigen (CEA) are both glycoproteins measurable in serum for which there are clinically available assays. CA19-9 and CEA are the most studied biomarkers for diagnosis of CCA. Current data suggests these markers by themselves cannot be used as the sole criteria for diagnosis of CCA but rather have utility as adjunctive markers in the context of patient factors and with the aid of multiphasic cross-sectional MRI or CT imaging, ERCP with brush cytology and/or forceps biopsy, or percutaneous or EUS-guided biopsy. In patients with a biliary stricture, an increased serum CA19-9 may support the diagnosis of CCA, particularly if the levels are persistently high after drainage of biliary obstruction. However, a negative test does not exclude CCA. A cutoff of 129 U/mL maximizes the utility of CA19-9 for detecting CCA in patients with PSC67–69. Moreover, it has been suggested that the serum CA19-9 is also effective for staging of disease since very high levels (CA19-9 > 1,000U/mL) may be associated with metastatic disease70. In a recently developed clinical staging system for pCCA, CA19-9 is a key differentiation variable for advanced disease71. CEA has demonstrated poor sensitivity and specificity for diagnosing CCA but used in combination with CA19-9, the two markers show better marker diagnostic utility than either biomarker alone in differentiating CCA from benign biliary diseases72.
CYFRA21-1 fragment of cytokeratin 19
In the liver, hepatocytes differentially express cytokeratins 8 and 18 while cholangiocytes express cytokeratins 7 and 19. Cytokeratin 19 can be used to discriminate iCCA from HCC in hepatic masses. However, it is not effective in differentiating tumoral tissue from benign cholangiocytes. CYFRA21-1 is a soluble serum fragment of cytokeratin 19, and a potential marker for detecting CCA via serum electrochemiluminiscent immunoassay (ECLIA). A retrospective study comparing CYFRA21-1 to CEA and CA19-9 in patients with histologically confirmed bile tract cancers showed that CYFRA21-1 had better sensitivity and specificity for detecting iCCA than any of the other biomarkers. Maximal Youden’s indexes were used to determine the cutoff for each of the biomarkers studied (3.27 mg/mL, 76.53 U/mL and 2.70 U/mL for CYFRA21-1, CA19-9 and CEA respectively). In a prospective study of patients with PSC, CYFRA21-1 at a cutoff of 1.5 ng/mL was more specific than CA19-973. Moreover, CYFRA21-1 was an effective predictor of poor prognosis and recurrence after tumor resection74. The utility of CYFRA21-1 for early detection of CCA in patients with PSC is unknown; further studies are required to investigate its performance in this setting.
Mucin 5AC (MUC5AC)
Mucin 5AC is a glycoprotein mucus component that is rarely secreted from nonmalignant biliary tract epithelial cells. Ruzzenente et al. compared serum MUC5AC levels of patients with malignant biliary obstruction to patients with benign biliary obstruction and healthy controls. MUC5AC enhanced the diagnostic accuracy of CA19-9 and CEA. Within patients with malignant disease, high levels of MUC5AC were also associated with poor prognosis75. Measurement of the serum-to-bile MUC5AC ratio resulted in a higher accuracy in detecting CCA from benign biliary disorders76. Current data on MUC5AC is preliminary and should be validated prospectively to ensure effectiveness and test potential cutoffs.
ERCP sampling by brush cytology, intraductal biopsy and FISH assay
Although invasive and expensive, ERCP is invaluable for visualizing and sampling the bile duct epithelium in the setting of strictures suspicious for malignancy. The sensitivity of conventional brush cytology for diagnosis of CCA ranges from 6% to 88% due to heterogeneity between studies in terms of categorization of equivocal results into positive and negative diagnoses and in terms of the populations under study (some studies include patients with masses on imaging while others only enroll PSC patients under surveillance). Furthermore, conventional cytology interpretation is difficult due to the overlapping nature of the cellular features seen in benign and malignant biliary strictures77.
In fluorescent in-situ hybridization (FISH), fluorescently labeled DNA probes are hybridized to cytology preparations in order to detect aneuploidy in cells from biliary stricture brushings or fine needle aspirations. Up until recently, most studies have used the UroVysion™ FISH probe set which was originally optimized for detection of urothelial cancers78, 79 (FISH result and interpretations are summarized in Table 2). Multiple reports show that in up to 60% of patients with negative standard cytology, UroVysion™ FISH can confirm the diagnosis of CCA80–83. In a meta-analysis of patients with PSC, FISH polysomy showed 51% sensitivity and 93% specificity84. Due to the influence of pre-test probability on biomarker performance, it is important not to use FISH in settings where the suspicion of cancer is very low, such as in patients with biliary stone disease. FISH trisomy 7 is sometimes seen and is usually non-specific, although in PSC it may identify patients who eventually will progress to invasive cancer85, 86. Eaton et al. have shown that FISH is useful in identifying PSC patients with multifocal polysomy, a subgroup of patients who were more likely to develop CCA and thus could benefit from close surveillance85. In a cohort of patients with PSC and equivocal biliary cytology (atypical or suspicious), patients with FISH polysomy were 76% more likely to develop a pancreaticobiliary tract malignancy within 2 years of cytology findings (P < 0.001). Most of these cancers turned out to be CCAs (27 were CCA, 2 pancreatic adenocarcinomas and 1 gallbladder cancer)83. Tetrasomy is typically associated with biliary stone disease and not with malignancy.
A new Pancreatobiliary FISH (PB FISH) panel has been optimized for diagnosing malignancy in pancreaticobiliary brushings. Initial results suggest that PB FISH provides an approximately 20% improvement in sensitivity over UroVysion FISH™, reaching sensitivities of up to 77% with a specificity of 96% for detection of malignancy in pancreatobiliary strictures87. Further validation of these initial results is forthcoming.
Methylated Bone Morphogenic Protein 3 (BMP-3)
Recently, Kisiel et al. reported increased promoter methylation of the known tumor suppressor BMP3 in CCA cell lines and resected tumor tissue but not in immortalized cholangiocytes or in matched benign bile tract epithelium. Further studies to validate these results in a larger cohort and in patients with PSC are now needed to determine this biomarker’s clinical applicability to detect early cholangiocarcinoma88. The need for implementing invasive techniques to acquire bile has been a fundamental limitation to the clinical use of bile biomarkers as surveillance for CCA. However, with the availability of the recently approved multi-target stool DNA testing system (Cologuard®) for screening for colorectal polyps and cancer, it is now possible to imagine the potential addition of novel aerodigestive cancer site specific assays to a stool DNA-based test, leading to further population-based bile duct cancer detection in a much more feasible and non-invasive fashion89.
Conclusion
In summary, biomarkers and imaging studies are inherently complementary in the surveillance and diagnosis of hepatobiliary malignancies. Continued advances in the use of both modalities, particularly the ability to combine modalities by using molecular marker binding in imaging studies, holds promise for substantially improving screening for HCC and CCA in the near future. There is a major gap in the availability of appropriately and prospectively collected sample repositories of cohorts of case and control patients with liver and biliary cancers to facilitate the evaluation of novel biomarkers. Efforts to establish these key sample repositories, for example through the US National Cancer Institute Early Detection Research Program, should be intensified.
Acknowledgments
Funding
This publication was made possible by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Footnotes
Conflict of Interest
Maria E. Lozada declares no conflict of interest.
Roongruedee Chaiteerakij declares no conflict of interest.
Dr. Roberts has received research grants from Wako Diagnostics and Inova Diagnostics, developers of serum biomarker tests. He has a current grant from Gilead Sciences, outside the submitted work.
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
Some of the referenced articles by authors do include human participants. All have been approved by Institutional Review Board and were conducted with proper informed consent and following ethics guidelines.
Contributor Information
Maria E. Lozada, Email: Lozada.maria@mayo.edu, Division of Gastroenterology and Hepatology, Mayo Clinic College of Medicine, 200 First Street SW, Rochester, MN, 55905.
Roongruedee Chaiteerakij, Email: Chaiteerakij.roongruedee@mayo.edu, Division of Gastroenterology and Hepatology, Mayo Clinic College of Medicine, 200 First Street SW, Rochester, MN, 55905 and Department of Medicine, Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Thai Red Cross Society, Bangkok 10330, Thailand.
Lewis R. Roberts, Email: Roberts.lewis@mayo.edu, Division of Gastroenterology and Hepatology, Mayo Clinic College of Medicine, 200 First Street SW, Rochester, MN, 55905.
References
Papers of particular interest, published recently, have been highlighted as:
* Of importance
** Of major importance
- 1.Howlader NNA, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER Cancer Statistics Review. Bethesda, MD: National Cancer Institute; 1975–2011. [Google Scholar]
- 2.Center MM, Jemal A. International trends in liver cancer incidence rates. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2011;20:2362–8. doi: 10.1158/1055-9965.EPI-11-0643. [DOI] [PubMed] [Google Scholar]
- 3.Ladep NG, Lesi OA, Mark P, Lemoine M, Onyekwere C, Afihene M, Crossey MM, Taylor-Robinson SD. Problem of hepatocellular carcinoma in West Africa. World journal of hepatology. 2014;6:783–92. doi: 10.4254/wjh.v6.i11.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raza A, Sood GK. Hepatocellular carcinoma review: current treatment, and evidence-based medicine. World journal of gastroenterology: WJG. 2014;20:4115–27. doi: 10.3748/wjg.v20.i15.4115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skipworth JR, Keane MG, Pereira SP. Update on the management of cholangiocarcinoma. Digestive diseases. 2014;32:570–8. doi: 10.1159/000360507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6**.Park JW, Chen M, Colombo M, Roberts LR, Schwartz M, Chen PJ, Kudo M, Johnson P, Wagner S, Orsini LS, Sherman M. Liver International. 2015. Global Patterns of Hepatocellular Carcinoma Management from Diagnosis to Death: the BRIDGE Study. In Press. This is the first large-scale study evaluating trends in HCC management and survival worldwide. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang JD, Kim B, Sanderson SO, Sauver JS, Yawn BP, Larson JJ, Therneau TM, Roberts LR, Gores GJ, Kim WR. Biliary tract cancers in Olmsted County, Minnesota, 1976–2008. The American journal of gastroenterology. 2012;107:1256–62. doi: 10.1038/ajg.2012.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8*.Chaiteerakij R, Addissie BD, Roberts LR. Update on Biomarkers of Hepatocellular Carcinoma. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2013 doi: 10.1016/j.cgh.2013.10.038. This review summarizes stages of biomarker development in the context of HCC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pepe MS, Etzioni R, Feng Z, Potter JD, Thompson ML, Thornquist M, Winget M, Yasui Y. Phases of biomarker development for early detection of cancer. Journal of the National Cancer Institute. 2001;93:1054–61. doi: 10.1093/jnci/93.14.1054. [DOI] [PubMed] [Google Scholar]
- 10.Shoreibah MG, Bloomer JR, McGuire BM, Massoud OI. Surveillance for hepatocellular carcinoma: evidence, guidelines and utilization. The American journal of the medical sciences. 2014;347:415–9. doi: 10.1097/MAJ.0000000000000200. [DOI] [PubMed] [Google Scholar]
- 11.Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marrero JA, Feng Z, Wang Y, Nguyen MH, Befeler AS, Roberts LR, Reddy KR, Harnois D, Llovet JM, Normolle D, Dalhgren J, Chia D, Lok AS, Wagner PD, Srivastava S, Schwartz M. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology. 2009;137:110–8. doi: 10.1053/j.gastro.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singal AG, Marrero JA, Yopp A. Screening process failures for hepatocellular carcinoma. Journal of the National Comprehensive Cancer Network: JNCCN. 2014;12:375–82. doi: 10.6004/jnccn.2014.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. Journal of cancer research and clinical oncology. 2004;130:417–22. doi: 10.1007/s00432-004-0552-0. [DOI] [PubMed] [Google Scholar]
- 15**.Lee E, Edward S, Singal AG, Lavieri MS, Volk M. Improving screening for hepatocellular carcinoma by incorporating data on levels of alpha-fetoprotein, over time. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2013;11:437–40. doi: 10.1016/j.cgh.2012.11.029. This study describes the ehanced utility of AFP patterns over single AFP levels for detecting HCC. [DOI] [PubMed] [Google Scholar]
- 16.Leerapun A, Suravarapu SV, Bida JP, Clark RJ, Sanders EL, Mettler TA, Stadheim LM, Aderca I, Moser CD, Nagorney DM, LaRusso NF, de Groen PC, Menon KV, Lazaridis KN, Gores GJ, Charlton MR, Roberts RO, Therneau TM, Katzmann JA, Roberts LR. The utility of Lens culinaris agglutinin-reactive alpha-fetoprotein in the diagnosis of hepatocellular carcinoma: evaluation in a United States referral population. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2007;5:394–402. doi: 10.1016/j.cgh.2006.12.005. quiz 267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lok AS, Sterling RK, Everhart JE, Wright EC, Hoefs JC, Di Bisceglie AM, Morgan TR, Kim HY, Lee WM, Bonkovsky HL, Dienstag JL. Des-gamma-carboxy prothrombin and alpha-fetoprotein as biomarkers for the early detection of hepatocellular carcinoma. Gastroenterology. 2010;138:493–502. doi: 10.1053/j.gastro.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18*.Johnson PJ, Pirrie SJ, Cox TF, Berhane S, Teng M, Palmer D, Morse J, Hull D, Patman G, Kagebayashi C, Hussain S, Graham J, Reeves H, Satomura S. The detection of hepatocellular carcinoma using a prospectively developed and validated model based on serological biomarkers. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2014;23:144–53. doi: 10.1158/1055-9965.EPI-13-0870. This study developed a new model for detecting HCC in the setting of chronic liver diseases. The model includes biomarkers (AFP, AFP-L3, DCP) and clinical characteristics (gender and age) [DOI] [PubMed] [Google Scholar]
- 19.Fox R, Berhane S, Teng M, Cox T, Tada T, Toyoda H, Kumada T, Kagebayashi C, Satomura S, Johnson PJ. Biomarker-based prognosis in hepatocellular carcinoma: validation and extension of the BALAD model. British journal of cancer. 2014;110:2090–8. doi: 10.1038/bjc.2014.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20*.El-Serag HB, Kanwal F, Davila JA, Kramer J, Richardson P. A new laboratory-based algorithm to predict development of hepatocellular carcinoma in patients with hepatitis C and cirrhosis. Gastroenterology. 2014;146:1249–55e1. doi: 10.1053/j.gastro.2014.01.045. This study developed a model for detecting HCC in the setting of HCV-induced cirrhosis. The model includes biomarkers (AFP, ALT and platelets) and age to predict HCC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21*.Flemming JA, Yang JD, Vittinghoff E, Kim WR, Terrault NA. Risk prediction of hepatocellular carcinoma in patients with cirrhosis: the ADRESS-HCC risk model. Cancer. 2014;120:3485–93. doi: 10.1002/cncr.28832. This study developed a model for HCC risk stratification in patients with cirrhosis. All variables included in this model are clinical characteristics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chaiteerakij RZX, Addissie BD, Mohamed E, Harmsen WS, Theobald JP, Peters BE, Balsanek JG, Ward MM, Giama NH, Moser CD, Oseini AM, Umeda N, Harnois DM, Charlton MR, Yamada H, Satomura S, Algeciras-Schimnich A, Snyder MR, Therneau TM, Roberts LR. Liver Transplantation. Combinations of Biomarkers and Milan Criteria for Predicting Hepatocellular Carcinoma Recurrence after Liver Transplantation. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kashkoush S, El Moghazy W, Kawahara T, Gala-Lopez B, Toso C, Kneteman NM. Three-dimensional tumor volume and serum alpha-fetoprotein are predictors of hepatocellular carcinoma recurrence after liver transplantation: refined selection criteria. Clinical transplantation. 2014;28:728–36. doi: 10.1111/ctr.12373. [DOI] [PubMed] [Google Scholar]
- 24.Dumitra TC, Dumitra S, Metrakos PP, Barkun JS, Chaudhury P, Deschenes M, Paraskevas S, Hassanain M, Tchervenkov JI. Pretransplantation alpha-fetoprotein slope and milan criteria: strong predictors of hepatocellular carcinoma recurrence after transplantation. Transplantation. 2013;95:228–33. doi: 10.1097/TP.0b013e31827743d7. [DOI] [PubMed] [Google Scholar]
- 25.Singal A, Volk ML, Waljee A, Salgia R, Higgins P, Rogers MA, Marrero JA. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Alimentary pharmacology & therapeutics. 2009;30:37–47. doi: 10.1111/j.1365-2036.2009.04014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singal AG, Conjeevaram HS, Volk ML, Fu S, Fontana RJ, Askari F, Su GL, Lok AS, Marrero JA. Effectiveness of hepatocellular carcinoma surveillance in patients with cirrhosis. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2012;21:793–9. doi: 10.1158/1055-9965.EPI-11-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sherman M, Bruix J, Porayko M, Tran T. Screening for hepatocellular carcinoma: the rationale for the American Association for the Study of Liver Diseases recommendations. Hepatology. 2012;56:793–6. doi: 10.1002/hep.25869. [DOI] [PubMed] [Google Scholar]
- 28.Kim J, Ki SS, Lee SD, Han CJ, Kim YC, Park SH, Cho SY, Hong YJ, Park HY, Lee M, Jung HH, Lee KH, Jeong SH. Elevated plasma osteopontin levels in patients with hepatocellular carcinoma. The American journal of gastroenterology. 2006;101:2051–9. doi: 10.1111/j.1572-0241.2006.00679.x. [DOI] [PubMed] [Google Scholar]
- 29.Wan HG, Xu H, Gu YM, Wang H, Xu W, Zu MH. Comparison osteopontin vs AFP for the diagnosis of HCC: a meta-analysis. Clinics and research in hepatology and gastroenterology. 2014;38:706–14. doi: 10.1016/j.clinre.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 30.Shang S, Plymoth A, Ge S, Feng Z, Rosen HR, Sangrajrang S, Hainaut P, Marrero JA, Beretta L. Identification of osteopontin as a novel marker for early hepatocellular carcinoma. Hepatology. 2012;55:483–90. doi: 10.1002/hep.24703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.da Costa AN, Plymoth A, Santos-Silva D, Ortiz-Cuaran S, Camey S, Guilloreau P, Sangrajrang S, Khuhaprema T, Mendy M, Lesi OA, Chang HK, Oh JK, Lee DH, Shin HR, Kirk GD, Merle P, Beretta L, Hainaut P. Osteopontin and latent-TGF beta binding-protein 2 as potential diagnostic markers for HBV-related hepatocellular carcinoma. International journal of cancer Journal international du cancer. 2015;136:172–81. doi: 10.1002/ijc.28953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang F, Long Q, Gong Y, Hu L, Zhang H, Oettgen P, Peng T. Epithelium-Specific ETS (ESE)-1 upregulated GP73 expression in hepatocellular carcinoma cells. Cell & bioscience. 2014;4:76. doi: 10.1186/2045-3701-4-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou Y, Yin X, Ying J, Zhang B. Golgi protein 73 versus alpha-fetoprotein as a biomarker for hepatocellular carcinoma: a diagnostic meta-analysis. BMC cancer. 2012;12:17. doi: 10.1186/1471-2407-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cao FF, Yu S, Jiang ZY, Bao YX. Diagnostic accuracy of Golgi protein 73 in primary hepatic carcinoma using ELISA: a systematic review and meta-analysis. Clinical laboratory. 2014;60:587–97. doi: 10.7754/clin.lab.2013.130312. [DOI] [PubMed] [Google Scholar]
- 35.Tian L, Wang Y, Xu D, Gui J, Jia X, Tong H, Wen X, Dong Z, Tian Y. Serological AFP/Golgi protein 73 could be a new diagnostic parameter of hepatic diseases. International journal of cancer Journal international du cancer. 2011;129:1923–31. doi: 10.1002/ijc.25838. [DOI] [PubMed] [Google Scholar]
- 36.Ozkan H, Erdal H, Tutkak H, Karaeren Z, Yakut M, Yuksel O, Koklu S. Diagnostic and prognostic validity of Golgi protein 73 in hepatocellular carcinoma. Digestion. 2011;83:83–8. doi: 10.1159/000320379. [DOI] [PubMed] [Google Scholar]
- 37.Hu JS, Wu DW, Liang S, Miao XY. GP73, a resident Golgi glycoprotein, is sensibility and specificity for hepatocellular carcinoma of diagnosis in a hepatitis B-endemic Asian population. Medical oncology. 2010;27:339–45. doi: 10.1007/s12032-009-9215-y. [DOI] [PubMed] [Google Scholar]
- 38.Bao YX, Cao Q, Yang Y, Mao R, Xiao L, Zhang H, Zhao HR, Wen H. Expression and prognostic significance of golgiglycoprotein73 (GP73) with epithelial-mesenchymal transition (EMT) related molecules in hepatocellular carcinoma (HCC) Diagnostic pathology. 2013;8:197. doi: 10.1186/1746-1596-8-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang L, Huang J, Jiang M, Zheng X. AFP computational secreted network construction and analysis between human hepatocellular carcinoma (HCC) and no-tumor hepatitis/cirrhotic liver tissues. Tumour biology: the journal of the International Society for Oncodevelopmental Biology and Medicine. 2010;31:417–25. doi: 10.1007/s13277-010-0050-8. [DOI] [PubMed] [Google Scholar]
- 40.Shen Q, Fan J, Yang XR, Tan Y, Zhao W, Xu Y, Wang N, Niu Y, Wu Z, Zhou J, Qiu SJ, Shi YH, Yu B, Tang N, Chu W, Wang M, Wu J, Zhang Z, Yang S, Gu J, Wang H, Qin W. Serum DKK1 as a protein biomarker for the diagnosis of hepatocellular carcinoma: a large-scale, multicentre study. The Lancet Oncology. 2012;13:817–26. doi: 10.1016/S1470-2045(12)70233-4. [DOI] [PubMed] [Google Scholar]
- 41.Lee JHJE, Choi YS, Leissner P, Brechot C, Chung JW, Kim JW, Jeong SH. 1250: Performance of biomarkers for diagnosis of hepatocellular carcinoma –alpha fetoprotein, protein induced by vitamin K absence, osteopontin and Dickkopf-1. Hepatology. 2014;60:92A–196A. [Google Scholar]
- 42.Vongsuvanh RGJ, Iseli TJ, Strasser SI, McCaughan GW, van der Poorten D. 1337: Serum dickkopf-1, osteopontin and midkine as novel biomarkers for the diagnosis and pre-clinical diagnosis of hepatocellular carcinoma. Hepatology. 2014;60:92A–196A. [Google Scholar]
- 43.Yang H, Chen GD, Fang F, Liu Z, Lau SH, Zhang JF, Lau WY, Yang LY. Dickkopf-1: as a diagnostic and prognostic serum marker for early hepatocellular carcinoma. The International journal of biological markers. 2013;28:286–297. doi: 10.5301/jbm.5000015. [DOI] [PubMed] [Google Scholar]
- 44.Huang Y, Yang X, Zhao F, Shen Q, Wang Z, Lv X, Hu B, Yu B, Fan J, Qin W. Overexpression of Dickkopf-1 predicts poor prognosis for patients with hepatocellular carcinoma after orthotopic liver transplantation by promoting cancer metastasis and recurrence. Medical oncology. 2014;31:966. doi: 10.1007/s12032-014-0966-8. [DOI] [PubMed] [Google Scholar]
- 45.Sunagozaka HYT, Oishi N, Hayashi T, Takatori H, Shimakami T, Kitamura K, Arai K, Kagaya T, Sakai Y, Yamashita T, Mizukoshi E, Honda M, Kaneko S. 1253: Serum Dickkopf-1 as a biomarker for the diagnosis of hepatocellular carcinoma with stem cell features. Hepatology. 2014;60:92A–196A. [Google Scholar]
- 46.Reichl P, Fang M, Starlinger P, Staufer K, Nenutil R, Muller P, Greplova K, Valik D, Dooley S, Brostjan C, Gruenberger T, Shen J, Man K, Trauner M, Yu J, Gao CF, Mikulits W. Multicenter analysis of soluble Axl reveals diagnostic value for very early stage hepatocellular carcinoma. International journal of cancer. Journal international du cancer. 2014 doi: 10.1002/ijc.29394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tomimaru Y, Eguchi H, Nagano H, Wada H, Kobayashi S, Marubashi S, Tanemura M, Tomokuni A, Takemasa I, Umeshita K, Kanto T, Doki Y, Mori M. Circulating microRNA-21 as a novel biomarker for hepatocellular carcinoma. Journal of hepatology. 2012;56:167–75. doi: 10.1016/j.jhep.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 48.Dhayat SA, Mardin WA, Kohler G, Bahde R, Vowinkel T, Wolters H, Senninger N, Haier J, Mees ST. The microRNA-200 family--a potential diagnostic marker in hepatocellular carcinoma? Journal of surgical oncology. 2014;110:430–8. doi: 10.1002/jso.23668. [DOI] [PubMed] [Google Scholar]
- 49.Xie Y, Yao Q, Butt AM, Guo J, Tian Z, Bao X, Li H, Meng Q, Lu J. Expression profiling of serum microRNA-101 in HBV-associated chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma. Cancer biology & therapy. 2014;15:1248–55. doi: 10.4161/cbt.29688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li L, Guo Z, Wang J, Mao Y, Gao Q. Serum miR-18a: a potential marker for hepatitis B virus-related hepatocellular carcinoma screening. Digestive diseases and sciences. 2012;57:2910–6. doi: 10.1007/s10620-012-2317-y. [DOI] [PubMed] [Google Scholar]
- 51.Gaddikeri S, McNeeley MF, Wang CL, Bhargava P, Dighe MK, Yeh MM, Dubinsky TJ, Kolokythas O, Lalwani N. Hepatocellular carcinoma in the noncirrhotic liver. AJR American journal of roentgenology. 2014;203:W34–47. doi: 10.2214/AJR.13.11511. [DOI] [PubMed] [Google Scholar]
- 52*.Honeyman JN, Simon EP, Robine N, Chiaroni-Clarke R, Darcy DG, Lim II, Gleason CE, Murphy JM, Rosenberg BR, Teegan L, Takacs CN, Botero S, Belote R, Germer S, Emde AK, Vacic V, Bhanot U, LaQuaglia MP, Simon SM. Detection of a recurrent DNAJB1-PRKACA chimeric transcript in fibrolamellar hepatocellular carcinoma. Science. 2014;343:1010–4. doi: 10.1126/science.1249484. This is the discovery article on the DNA KB1-PRKACA fusion protein in fibrolamellar HCC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53*.Cornella H, Alsinet C, Sayols S, Zhang Z, Hao K, Cabellos L, Hoshida Y, Villanueva A, Thung S, Ward SC, Rodriguez-Carunchio L, Vila-Casadesus M, Imbeaud S, Lachenmayer A, Quaglia A, Nagorney DM, Minguez B, Carrilho F, Roberts LR, Waxman S, Mazzaferro V, Schwartz M, Esteller M, Heaton ND, Zucman-Rossi J, Llovet JM. Unique genomic profile of fibrolamellar hepatocellular carcinoma. Gastroenterology. 2014 doi: 10.1053/j.gastro.2014.12.028. In this recent study, the authors evaluate the prevalence of DNAJB1-PRKACA fusion protein previously described in fibrolamellar HCC. Also, the authors identified 3 distinct molecular classes of fribolamellar HCC with potential implications for diagnosis and treatment strategies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu L, Hazard FK, Zmoos AF, Jahchan N, Chaib H, Garfin PM, Rangaswami A, Snyder MP, Sage J. Genomic analysis of fibrolamellar hepatocellular carcinoma. Human molecular genetics. 2015;24:50–63. doi: 10.1093/hmg/ddu418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Graham RPJL, Knutson D, Kloft-Nelson S, Greipp PT, Waldburger N, Roessler S, Longerich T, Roberts LR, Schirmacher P, Oliveira AM, Halling KC, Torbenson MS. Modern Pathology. DNAJB1-PRKACA is Specific for Fibrolamellar Carcinoma. In Press. [DOI] [PubMed] [Google Scholar]
- 56.Mavros MN, Mayo SC, Hyder O, Pawlik TM. A systematic review: treatment and prognosis of patients with fibrolamellar hepatocellular carcinoma. Journal of the American College of Surgeons. 2012;215:820–30. doi: 10.1016/j.jamcollsurg.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 57.Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, Pawlik TM, Gores GJ. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. Journal of hepatology. 2014;60:1268–89. doi: 10.1016/j.jhep.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 58.Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, Shneider B, Gores GJ. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660–78. doi: 10.1002/hep.23294. [DOI] [PubMed] [Google Scholar]
- 59.Burak K, Angulo P, Pasha TM, Egan K, Petz J, Lindor KD. Incidence and risk factors for cholangiocarcinoma in primary sclerosing cholangitis. The American journal of gastroenterology. 2004;99:523–6. doi: 10.1111/j.1572-0241.2004.04067.x. [DOI] [PubMed] [Google Scholar]
- 60*.Razumilava N, Gores GJ. Classification, diagnosis, and management of cholangiocarcinoma. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2013;11:13–21e1. doi: 10.1016/j.cgh.2012.09.009. quiz e3–4. This is a very thorough review article on advances in classification, diagnosis, staging and treatment of CCA. The authors include diagnostic and management algorithms for patients with suspected CCA by subclassification (intrahepatic, perihilar and distal CCAs) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Palmer WC, Patel T. Are common factors involved in the pathogenesis of primary liver cancers? A meta-analysis of risk factors for intrahepatic cholangiocarcinoma. Journal of hepatology. 2012;57:69–76. doi: 10.1016/j.jhep.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Razumilava N, Gores GJ, Lindor KD. Cancer surveillance in patients with primary sclerosing cholangitis. Hepatology. 2011;54:1842–52. doi: 10.1002/hep.24570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Graham RP, Barr Fritcher EG, Pestova E, Schulz J, Sitailo LA, Vasmatzis G, Murphy SJ, McWilliams RR, Hart SN, Halling KC, Roberts LR, Gores GJ, Couch FJ, Zhang L, Borad MJ, Kipp BR. Fibroblast growth factor receptor 2 translocations in intrahepatic cholangiocarcinoma. Human pathology. 2014;45:1630–8. doi: 10.1016/j.humpath.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 64.Borad MJ, Champion MD, Egan JB, Liang WS, Fonseca R, Bryce AH, McCullough AE, Barrett MT, Hunt K, Patel MD, Young SW, Collins JM, Silva AC, Condjella RM, Block M, McWilliams RR, Lazaridis KN, Klee EW, Bible KC, Harris P, Oliver GR, Bhavsar JD, Nair AA, Middha S, Asmann Y, Kocher JP, Schahl K, Kipp BR, Barr Fritcher EG, Baker A, Aldrich J, Kurdoglu A, Izatt T, Christoforides A, Cherni I, Nasser S, Reiman R, Phillips L, McDonald J, Adkins J, Mastrian SD, Placek P, Watanabe AT, Lobello J, Han H, Von Hoff D, Craig DW, Stewart AK, Carpten JD. Integrated genomic characterization reveals novel, therapeutically relevant drug targets in FGFR and EGFR pathways in sporadic intrahepatic cholangiocarcinoma. PLoS genetics. 2014;10:e1004135. doi: 10.1371/journal.pgen.1004135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu YM, Su F, Kalyana-Sundaram S, Khazanov N, Ateeq B, Cao X, Lonigro RJ, Vats P, Wang R, Lin SF, Cheng AJ, Kunju LP, Siddiqui J, Tomlins SA, Wyngaard P, Sadis S, Roychowdhury S, Hussain MH, Feng FY, Zalupski MM, Talpaz M, Pienta KJ, Rhodes DR, Robinson DR, Chinnaiyan AM. Identification of targetable FGFR gene fusions in diverse cancers. Cancer discovery. 2013;3:636–47. doi: 10.1158/2159-8290.CD-13-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Arai Y, Totoki Y, Hosoda F, Shirota T, Hama N, Nakamura H, Ojima H, Furuta K, Shimada K, Okusaka T, Kosuge T, Shibata T. Fibroblast growth factor receptor 2 tyrosine kinase fusions define a unique molecular subtype of cholangiocarcinoma. Hepatology. 2014;59:1427–34. doi: 10.1002/hep.26890. [DOI] [PubMed] [Google Scholar]
- 67.Levy C, Lymp J, Angulo P, Gores GJ, Larusso N, Lindor KD. The value of serum CA 19-9 in predicting cholangiocarcinomas in patients with primary sclerosing cholangitis. Digestive diseases and sciences. 2005;50:1734–40. doi: 10.1007/s10620-005-2927-8. [DOI] [PubMed] [Google Scholar]
- 68.Charatcharoenwitthaya P, Enders FB, Halling KC, Lindor KD. Utility of serum tumor markers, imaging, and biliary cytology for detecting cholangiocarcinoma in primary sclerosing cholangitis. Hepatology. 2008;48:1106–17. doi: 10.1002/hep.22441. [DOI] [PubMed] [Google Scholar]
- 69.Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet. 2014;383:2168–79. doi: 10.1016/S0140-6736(13)61903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marrero JA. Biomarkers in cholangiocarcinoma. Clinical Liver Disease. 2014;3:101–103. doi: 10.1002/cld.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chaiteerakij R, Harmsen WS, Marrero CR, Aboelsoud MM, Ndzengue A, Kaiya J, Therneau TM, Sanchez W, Gores GJ, Roberts LR. A new clinically based staging system for perihilar cholangiocarcinoma. The American journal of gastroenterology. 2014;109:1881–90. doi: 10.1038/ajg.2014.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Qin XL, Wang ZR, Shi JS, Lu M, Wang L, He QR. Utility of serum CA19-9 in diagnosis of cholangiocarcinoma: in comparison with CEA. World journal of gastroenterology: WJG. 2004;10:427–32. doi: 10.3748/wjg.v10.i3.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chapman MH, Sandanayake NS, Andreola F, Dhar DK, Webster GJ, Dooley JS, Pereira SP. Circulating CYFRA 21-1 is a Specific Diagnostic and Prognostic Biomarker in Biliary Tract Cancer. Journal of clinical and experimental hepatology. 2011;1:6–12. doi: 10.1016/S0973-6883(11)60110-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Huang L, Chen W, Liang P, Hu W, Zhang K, Shen S, Chen J, Zhang Z, Chen B, Han Y, Meng F, DeMorrow S, Yin X, Lai J, Liang L. Serum CYFRA 21-1 in Biliary Tract Cancers: A Reliable Biomarker for Gallbladder Carcinoma and Intrahepatic Cholangiocarcinoma. Digestive diseases and sciences. 2014 doi: 10.1007/s10620-014-3472-0. [DOI] [PubMed] [Google Scholar]
- 75.Ruzzenente A, Iacono C, Conci S, Bertuzzo F, Salvagno G, Ruzzenente O, Campagnaro T, Valdegamberi A, Pachera S, Bagante F, Guglielmi A. A novel serum marker for biliary tract cancer: diagnostic and prognostic values of quantitative evaluation of serum mucin 5AC (MUC5AC) Surgery. 2014;155:633–9. doi: 10.1016/j.surg.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 76.Danese E, Ruzzenente O, Ruzzenente A, Iacono C, Bertuzzo F, Gelati M, Conci S, Bendinelli S, Bonizzato G, Guglielmi A, Salvagno GL, Lippi G, Guidi GC. Assessment of bile and serum mucin5AC in cholangiocarcinoma: diagnostic performance and biologic significance. Surgery. 2014;156:1218–24. doi: 10.1016/j.surg.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 77**.Barr Fritcher EG, Kipp BR, Halling KC, Clayton AC. FISHing for pancreatobiliary tract malignancy in endoscopic brushings enhances the sensitivity of routine cytology. Cytopathology: official journal of the British Society for Clinical Cytology. 2014;25:288–301. doi: 10.1111/cyt.12170. This review article clearly describes the interpretation of the UroVysion FISH assay in the context of cholangiocarcinoma. [DOI] [PubMed] [Google Scholar]
- 78.Kipp BR, Stadheim LM, Halling SA, Pochron NL, Harmsen S, Nagorney DM, Sebo TJ, Therneau TM, Gores GJ, de Groen PC, Baron TH, Levy MJ, Halling KC, Roberts LR. A comparison of routine cytology and fluorescence in situ hybridization for the detection of malignant bile duct strictures. The American journal of gastroenterology. 2004;99:1675–81. doi: 10.1111/j.1572-0241.2004.30281.x. [DOI] [PubMed] [Google Scholar]
- 79.Levy MJ, Oberg TN, Campion MB, Clayton AC, Halling KC, Henry MR, Kipp BR, Sebo TJ, Zhang J, Enders FT, Clain JE, Gleeson FC, Rajan E, Roberts LR, Topazian MD, Wang KK, Gores GJ. Comparison of methods to detect neoplasia in patients undergoing endoscopic ultrasound-guided fine-needle aspiration. Gastroenterology. 2012;142:1112–1121e2. doi: 10.1053/j.gastro.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 80.Fritcher EG, Kipp BR, Halling KC, Oberg TN, Bryant SC, Tarrell RF, Gores GJ, Levy MJ, Clayton AC, Sebo TJ, Roberts LR. A multivariable model using advanced cytologic methods for the evaluation of indeterminate pancreatobiliary strictures. Gastroenterology. 2009;136:2180–6. doi: 10.1053/j.gastro.2009.02.040. [DOI] [PubMed] [Google Scholar]
- 81*.Kipp BR, Barr Fritcher EG, Pettengill JE, Halling KC, Clayton AC. Improving the accuracy of pancreatobiliary tract cytology with fluorescence in situ hybridization: a molecular test with proven clinical success. Cancer cytopathology. 2013;121:610–9. doi: 10.1002/cncy.21303. This is a recent review on the use of FISH for diagnosis of pancreaticobiliary malignancies in which the authors describe its use, review the methods for sampling and summarize the current published data. [DOI] [PubMed] [Google Scholar]
- 82.Kipp BR, Fritcher EG, Clayton AC, Gores GJ, Roberts LR, Zhang J, Levy MJ, Halling KC. Comparison of KRAS mutation analysis and FISH for detecting pancreatobiliary tract cancer in cytology specimens collected during endoscopic retrograde cholangiopancreatography. The Journal of molecular diagnostics: JMD. 2010;12:780–6. doi: 10.2353/jmoldx.2010.100016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Barr Fritcher EG, Voss JS, Jenkins SM, Lingineni RK, Clayton AC, Roberts LR, Halling KC, Talwalkar JA, Gores GJ, Kipp BR. Primary sclerosing cholangitis with equivocal cytology: fluorescence in situ hybridization and serum CA 19-9 predict risk of malignancy. Cancer cytopathology. 2013;121:708–17. doi: 10.1002/cncy.21331. [DOI] [PubMed] [Google Scholar]
- 84.Navaneethan U, Njei B, Venkatesh PG, Vargo JJ, Parsi MA. Fluorescence in situ hybridization for diagnosis of cholangiocarcinoma in primary sclerosing cholangitis: a systematic review and meta-analysis. Gastrointestinal endoscopy. 2014;79:943–950e3. doi: 10.1016/j.gie.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 85.Barr Fritcher EG, Kipp BR, Voss JS, Clayton AC, Lindor KD, Halling KC, Gores GJ. Primary sclerosing cholangitis patients with serial polysomy fluorescence in situ hybridization results are at increased risk of cholangiocarcinoma. The American journal of gastroenterology. 2011;106:2023–8. doi: 10.1038/ajg.2011.272. [DOI] [PubMed] [Google Scholar]
- 86.Eaton JE, Talwalkar JA, Lazaridis KN, Gores GJ, Lindor KD. Pathogenesis of Primary Sclerosing Cholangitis and Advances in Diagnosis and Management. Gastroenterology. 2014;145:521–536. doi: 10.1053/j.gastro.2013.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Barr Fritcher EGKB, Voss JS, Brankley SM, Keeney ME, Campion MB, Pestova EV, Sokolova IA, Roberts LR, Gores GJ, ClaBarr Fritcher E, Guyton AC, Halling KC. The Development of a Tailored Pancreatobiliary Fluorescence in situ Hybridization (FISH) Assay to Improve Detection of Malignancy in Pancreatobiliary Brushings. The Journal of Molecular Diagnostics. 2013;15:909. [Google Scholar]
- 88.Kisiel JB, Li J, Zou H, Oseini AM, Strauss BB, Gulaid KH, Moser CD, Aderca I, Ahlquist DA, Roberts LR, Shire AM. Methylated Bone Morphogenetic Protein 3 (BMP3) Gene: Evaluation of Tumor Suppressor Function and Biomarker Potential in Biliary Cancer. Journal of molecular biomarkers & diagnosis. 2013;4:1000145. doi: 10.4172/2155-9929.1000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ahlquist DA. Multi-Target Stool DNA Test: A New High Bar for Noninvasive Screening. Digestive diseases and sciences. 2014 doi: 10.1007/s10620-014-3451-5. [DOI] [PubMed] [Google Scholar]