Abstract
IMPORTANCE
Little is known about recent trends in rural-urban disparities in youth suicide, particularly sex- and method-specific changes. Documenting the extent of these disparities is critical for the development of policies and programs aimed at eliminating geographic disparities.
OBJECTIVE
To examine trends in US suicide mortality for adolescents and young adults across the rural-urban continuum.
DESIGN, SETTING, AND PARTICIPANTS
Longitudinal trends in suicide rates by rural and urban areas between January 1, 1996, and December 31, 2010, were analyzed using county-level national mortality data linked to a rural-urban continuum measure that classified all 3141 counties in the United States into distinct groups based on population size and adjacency to metropolitan areas. The population included all suicide decedents aged 10 to 24 years.
MAIN OUTCOMES AND MEASURES
Rates of suicide per 100 000 persons.
RESULTS
Across the study period, 66 595 youths died by suicide, and rural suicide rates were nearly double those of urban areas for both males (19.93 and 10.31 per 100 000, respectively) and females (4.40 and 2.39 per 100 000, respectively). Even after controlling for a wide array of county-level variables, rural-urban suicide differentials increased over time for males, suggesting widening rural-urban disparities (1996-1998: adjusted incidence rate ratio [IRR], 0.98; 2008-2010: adjusted IRR, 1.19; difference in IRR, P = .02). Firearm suicide rates declined, and the rates of hanging/suffocation for both males and females increased. However, the rates of suicide by firearm (males: 1996-1998, 2.05; and 2008-2010: 2.69 times higher) and hanging/suffocation (males: 1996-1998, 1.24; and 2008-2010: 1.63 times higher) were disproportionately higher in rural areas, and rural-urban differences increased over time (P = .002 for males; P = .06 for females).
CONCLUSIONS AND RELEVANCE
Suicide rates for adolescents and young adults are higher in rural than in urban communities regardless of the method used, and rural-urban disparities appear to be increasing over time. Further research should carefully explore the mechanisms whereby rural residence might increase suicide risk in youth and consider suicide-prevention efforts specific to rural settings.
Suicide is a serious public health problem. For youths between the ages of 10 and 24 years, suicide was the third leading cause of death in 2010 behind only unintentional injuries and homicide.1 Males are at higher risk, accounting for 81% of suicide deaths in the 10- to 24-year age group. Suicide risk increases with age, with 6% occurring in individuals younger than 15 years, 34% in those between 15 and 19 years, and 60% in young adults aged 20 to 24 years.1
Rates of suicide also vary by rural-urban residence, with higher rates in rural compared with urban areas.2-6 In the most recent comparative analysis of suicide trends among US rural and urban counties, Singh and Siahpush7 examined national mortality data from 1970 to 1997 for 3 age groups: young (15-24 years), working age (25-64 years), and elderly (≥65 years) individuals. Suicide rates among rural men were higher than those of urban men, with rural-urban differences widening over time. Higher rates of suicide attempts have also been reported8 among rural compared with urban adolescents.
To investigate the most recent trends and provide an updated comparison of rural and urban suicide rates in youths, we analyzed national mortality data from January 1, 1996, to December 31, 2010, focusing on adolescents and young adults aged 10 to 24 years. The primary aim of this study was to examine rural and urban differences in youth suicide mortality in the United States over time and stratified by sex. A secondary aim was to explore method-specific trends in youth suicide across the rural-urban continuum.
Methods
Participants and Data Sources
Multiple deidentified cause-of-death data files from January 1, 1996, to December 31, 2010, were obtained from the National Center for Health Statistics National Vital Statistics System.9 Coroners or medical examiners determine the cause of death using available information regarding circumstances surrounding the death. From among all US causes of death, suicides were selected for young people aged 10 to 24 years based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) (external cause codes E950-E959) for January 1, 1996, to December 31, 1998, and the International Statistical Classification of Diseases, Tenth Revision (ICD-10) (external cause codes X60-X84, Y87.0, and U03) for January 1, 1999, to December 31, 2010. Comparability studies of cause of death between ICD-9-CM and ICD-10 indicated no effect on the continuity of suicide data (comparability ratio, 0.996).10 Information was extracted on the number of suicide deaths per year, county of residence, age, sex, and method. Causes of death were grouped into 4 categories: firearm, hanging/suffocation (ie, hanging, suffocation by plastic bag, and suffocation by unspecified means), poisoning (ie, drugs, other solid or liquid substances, gases, and vapors), and other means (eg, fall, cut/pierce, and transportation related). The study was evaluated and determined to be exempt from human subjects review by The Ohio State University Institutional Review Board.
To analyze longitudinal trends in suicide rates by rural and urban areas, we used the 2003 Rural-Urban Continuum Codes (RUCCs) scheme developed by the US Department of Agriculture.11 This variable classifies all 3141 US counties into 9 distinct groups based on population size and adjacency to metropolitan areas (eTable 1 in the Supplement). Because of the small numbers of observations per county (≤20 deaths) within the 2 most rural categories (categories 8 and 9), these categories were collapsed into one unit, hereinafter referred to as the most rural county type. Each suicide decedent was assigned 1 of the 8 RUCC codes based on their county of residence. County assignments were based on the 5-digit federal information processing standard codes.
To examine the effects of the RUCC (our primary independent variable) on suicide mortality, we adjusted for multiple county-level independent variables demonstrated to be associated with suicide.2 These variables included county measures of the proportion of residents with a high school diploma, proportion with a college degree, proportion of black individuals, proportion of Hispanic individuals, per capita income, proportion unemployed, proportion living in poverty, proportion in female-headed households, proportion of females divorced, and population per square mile. We also included the following county-level variables of health service utilization: the number of pediatricians, child psychiatrists, psychiatrists, psychologists, and social workers per 10 000 population and the number of community mental health clinics. All independent variables were obtained from the 2000 US Census Bureau12 and the Area Resource File.13
Statistical Analysis
Negative binomial regression models were used to estimate the suicide incidence rates and the incidence rate ratios (IRRs) along with their 95% CIs separately for males and females. The model included terms for RUCCs, continuous time, and the interaction between the RUCC and time. When estimating rates across methods of suicide, the model included terms for RUCCs, time, the interaction between RUCCs and time, method, the interaction between RUCCs and method, and the interaction between time and method. Aggregate years (eg, 1996-1998 and 1999-2001) were used in the model when populating the tables, and all 15 years were used when estimating the change in the suicide rate over time (ie, slope).
Both the suicide incidence rates and the IRRs were age-adjusted using the 10- to 24-year age composition of the 2000 US population. Results were also adjusted for the independent county-level contextual variables mentioned above. Per capita income and population per square mile were log transformed. We used a risk factor modeling approach to determine which covariates to add to the negative binomial regression model. Only county-level contextual variables that confounded the relationship between the incidence of death and RUCCs were included. Specifically, a confounder was identified when its addition to the model changed any IRR associated with any of the RUCC levels by more than 10% in either direction without considering statistical significance.14 Each county-level contextual variable was entered individually into the regression model to determine whether it confounded the relationship. This approach eliminated the proportion of Hispanic individuals, persons living in poverty, and number of community mental health clinics from the model. All analyses were conducted using Stata, version 13.1.15
Results
From January 1, 1996, to December 31, 2010, a total of 66 595 youths aged 10 to 24 years died by suicide. The most common method was death by firearm (51.1%), followed by hanging/suffocation (33.9%), poisoning (7.9%), and other means (7.1%). Table 1 provides age-adjusted suicide rates for males and females by RUCCs for the 5 study periods, as well as the rate of change in suicide rates (slope) over time. From 2008 to 2010, the age-adjusted suicide rate for males in the most rural counties was 19.93 per 100 000—nearly double the rate of 10.31 per 100 000 in the most urban counties. Male suicide rates decreased significantly over time in urban counties (slope, −0.01; P < .001), but female suicide rates increased over time in the most rural and most urban counties (slope, 0.03 and 0.01; both P = .04). Female suicide rates were higher in rural counties but were substantially lower than male rates across all county types.
Table 1.
Age-Adjusted Suicide Mortality Ratesa
| Residential Location by Sexb | Year | Slope | P Value | ||||
|---|---|---|---|---|---|---|---|
| 1996-1998 | 1999-2001 | 2002-2004 | 2005-2007 | 2008-2010 | |||
| Males | |||||||
| 1 (Most urban) | 11.95 | 11.51 | 11.10 | 10.70 | 10.31 | −0.012 | <.001 |
| 2 | 13.48 | 12.93 | 12.40 | 11.89 | 11.40 | −0.013 | <.001 |
| 3 | 13.69 | 13.37 | 13.05 | 12.75 | 12.45 | −0.008 | .02 |
| 4 | 14.17 | 14.00 | 13.83 | 13.66 | 13.49 | −0.004 | .35 |
| 5 | 13.30 | 13.87 | 14.48 | 15.11 | 15.77 | 0.013 | .07 |
| 6 | 16.51 | 15.66 | 14.86 | 14.09 | 13.37 | −0.016 | <.001 |
| 7 | 17.18 | 17.26 | 17.35 | 17.43 | 17.51 | 0.000 | .95 |
| 8/9 (Most rural) | 18.98 | 19.22 | 19.45 | 19.69 | 19.93 | 0.004 | .54 |
| Females | |||||||
| 1 (Most urban) | 2.18 | 2.23 | 2.28 | 2.33 | 2.39 | 0.008 | .04 |
| 2 | 2.38 | 2.45 | 2.52 | 2.59 | 2.67 | 0.009 | .08 |
| 3 | 2.36 | 2.43 | 2.50 | 2.58 | 2.65 | 0.008 | .27 |
| 4 | 2.38 | 2.37 | 2.37 | 2.37 | 2.37 | 0.000 | .97 |
| 5 | 2.26 | 2.39 | 2.53 | 2.68 | 2.83 | 0.016 | .29 |
| 6 | 2.50 | 2.61 | 2.73 | 2.86 | 2.99 | 0.017 | .08 |
| 7 | 2.75 | 2.94 | 3.14 | 3.36 | 3.59 | 0.023 | .06 |
| 8/9 (Most rural) | 3.19 | 3.46 | 3.75 | 4.06 | 4.40 | 0.032 | .04 |
Population included suicide decedents aged 10 to 24 years.
Suicide rates per 100 000 population: 1 (most urban), counties in metropolitan areas of more than 1 million population; 2, counties in metropolitan areas of 250 000 to 1 million population; 3, counties in metropolitan areas of fewer than 250 000 population; 4, urban population of 20 000 or more, adjacent to a metropolitan area; 5, urban population of 20 000 or more, not adjacent to a metropolitan area; 6, urban population of 2500 to 19 999, adjacent to a metropolitan area; 7, urban population of 2500 to 19 999, not adjacent to a metropolitan area; 8, completely rural or less than 2500 urban population, adjacent to a metropolitan area; and 9, completely rural or less than 2500 urban population, not adjacent to a metropolitan area.
Table 2 provides the IRRs and 95% CIs derived from negative binomial regression for males and females by the RUCCs as well as after adjustment for county-level contextual variables. For males, suicide IRRs were higher in rural compared with urban areas in each of the 5 time periods, and the gap between the most rural and most urban counties widened over time. For example, in age-adjusted models during the periods from 1996 to 1998 and 2008 to 2010, the incidence rates of suicide were 59% and 93% higher, respectively, for male youths living in rural counties compared with those in urban counties (P = .02). This pattern persisted after controlling for contextual-level factors (P = .02). Females showed a similar pattern of higher IRRs in rural counties compared with urban counties, although the rural-urban differentials did not change significantly over time (P = .26, age-adjusted model; and P = .25, contextually adjusted model).
Table 2.
IRRs and 95% CIs by Rural-Urban Continuum, Sex, and Time Perioda
| Residential Location by Sex | IRR (95% CI) | ||||
|---|---|---|---|---|---|
| 1996-1998 | 1999-2001 | 2002-2004 | 2005-2007 | 2008-2010 | |
| Males | |||||
| Unadjusted | |||||
| 1 (Most urban) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2 | 1.13 (1.06-1.20) | 1.12 (1.08-1.17) | 1.12 (1.08-1.16) | 1.11 (1.07-1.16) | 1.11 (1.04-1.17) |
| 3 | 1.15 (1.08-1.22) | 1.16 (1.11-1.21) | 1.18 (1.13-1.22) | 1.19 (1.14-1.25) | 1.21 (1.14-1.29) |
| 4 | 1.19 (1.10-1.28) | 1.22 (1.15-1.28) | 1.25 (1.19-1.30) | 1.28 (1.21-1.35) | 1.31 (1.21-1.41) |
| 5 | 1.11 (1.00-1.24) | 1.20 (1.11-1.30) | 1.30 (1.23-1.39) | 1.41 (1.31-1.52) | 1.53 (1.38-1.70) |
| 6 | 1.38 (1.29-1.48) | 1.36 (1.30-1.43) | 1.34 (1.29-1.39) | 1.32 (1.25-1.39) | 1.30 (1.21-1.39) |
| 7 | 1.44 (1.32-1.57) | 1.50 (1.41-1.59) | 1.56 (1.49-1.64) | 1.63 (1.53-1.73) | 1.70 (1.56-1.85) |
| 8/9 (Most rural) | 1.59 (1.44-1.76) | 1.67 (1.56-1.79) | 1.75 (1.65-1.86) | 1.84 (1.71-1.98) | 1.93 (1.75-2.14) |
| Adjustedb | |||||
| 1 (Most urban) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2 | 0.93 (0.88-0.99) | 0.93 (0.89-0.97) | 0.93 (0.90-0.96) | 0.93 (0.89-0.97) | 0.92 (0.87-0.98) |
| 3 | 0.85 (0.79-0.90) | 0.86 (0.82-0.90) | 0.87 (0.83-0.91) | 0.88 (0.84-0.92) | 0.89 (0.84-0.95) |
| 4 | 0.84 (0.78-0.91) | 0.86 (0.81-0.91) | 0.88 (0.84-0.93) | 0.90 (0.85-0.96) | 0.92 (0.85-1.00) |
| 5 | 0.71 (0.63-0.79) | 0.76 (0.70-0.83) | 0.83 (0.77-0.89) | 0.90 (0.83-0.97) | 0.97 (0.87-1.08) |
| 6 | 0.92 (0.85-0.99) | 0.90 (0.85-0.96) | 0.89 (0.84-0.94) | 0.87 (0.82-0.93) | 0.86 (0.79-0.93) |
| 7 | 0.86 (0.78-0.94) | 0.90 (0.84-0.96) | 0.93 (0.88-0.99) | 0.97 (0.91-1.05) | 1.01 (0.92-1.11) |
| 8/9 (Most rural) | 0.98 (0.88-1.09) | 1.03 (0.95-1.11) | 1.08 (1.00-1.16) | 1.13 (1.04-1.23) | 1.19 (1.07-1.32) |
| Females | |||||
| Unadjusted | |||||
| 1 (Most urban) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2 | 1.09 (0.99-1.21) | 1.10 (1.03-1.18) | 1.11 (1.05-1.17) | 1.11 (1.04-1.19) | 1.12 (1.02-1.23) |
| 3 | 1.08 (0.96-1.22) | 1.09 (1.00-1.19) | 1.10 (1.03-1.17) | 1.11 (1.02-1.20) | 1.11 (0.99-1.24) |
| 4 | 1.09 (0.93-1.28) | 1.07 (0.95-1.19) | 1.04 (0.95-1.14) | 1.02 (0.91-1.14) | 0.99 (0.84-1.16) |
| 5 | 1.04 (0.82-1.32) | 1.07 (0.91-1.27) | 1.11 (0.97-1.27) | 1.15 (0.98-1.35) | 1.19 (0.94-1.49) |
| 6 | 1.15 (0.98-1.34) | 1.17 (1.05-1.31) | 1.20 (1.10-1.31) | 1.23 (1.11-1.36) | 1.25 (1.08-1.45) |
| 7 | 1.27 (1.04-1.53) | 1.32 (1.16-1.51) | 1.38 (1.24-1.53) | 1.44 (1.27-1.63) | 1.50 (1.25-1.80) |
| 8/9 (Most rural) | 1.47 (1.15-1.88) | 1.55 (1.31-1.85) | 1.64 (1.44-1.87) | 1.74 (1.49-2.03) | 1.84 (1.47-2.30) |
| Adjustedb | |||||
| 1 (Most urban) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2 | 0.92 (0.83-1.02) | 0.93 (0.86-1.00) | 0.93 (0.88-0.99) | 0.94 (0.88-1.01) | 0.95 (0.86-1.05) |
| 3 | 0.84 (0.74-0.96) | 0.85 (0.77-0.94) | 0.86 (0.79-0.93) | 0.86 (0.79-0.95) | 0.87 (0.77-0.98) |
| 4 | 0.84 (0.71-1.00) | 0.82 (0.72-0.93) | 0.80 (0.72-0.90) | 0.79 (0.70-0.89) | 0.77 (0.65-0.91) |
| 5 | 0.70 (0.55-0.90) | 0.73 (0.61-0.87) | 0.75 (0.65-0.87) | 0.78 (0.65-0.93) | 0.81 (0.63-1.02) |
| 6 | 0.89 (0.75-1.05) | 0.91 (0.80-1.03) | 0.93 (0.83-1.04) | 0.95 (0.84-1.08) | 0.97 (0.82-1.14) |
| 7 | 0.86 (0.70-1.06) | 0.90 (0.77-1.05) | 0.94 (0.83-1.07) | 0.98 (0.85-1.14) | 1.03 (0.84-1.24) |
| 8/9 (Most rural) | 1.09 (0.84-1.42) | 1.16 (0.96-1.40) | 1.22 (1.05-1.43) | 1.29 (1.09-1.54) | 1.37 (1.08-1.74) |
Abbreviation: IRR, incidence rate ratio.
Population included suicide decedents aged 10 to 24 years.
Models were adjusted for the proportion of persons in the community who were older than 25 years with a high school diploma, proportion of persons older than 25 years with a college degree, proportion of black individuals, per capita income, proportion of the civilian workforce population unemployed, proportion of households headed by women, proportion of females divorced, population per square mile, and the number of pediatricians, child psychiatrists, psychiatrists, psychologists, and social workers per 10 000 population.
Table 3 provides age-adjusted suicide incidence rates for firearm and hanging/suffocation deaths for males and females by the RUCCs (eTable 2 in the Supplement indicates age-adjusted rates of poisoning and other methods). The rate of change (slope) in suicide rates over time by method is also provided for males and females. Overall, death by firearm decreased across all county types for both sexes, but death by hanging/suffocation increased. However, suicide rates by firearm were disproportionately higher in rural compared with urban areas for both males and females. For example, during the period 2008-2010, suicide rates by firearm in males more than doubled from 4.42 per 100 000 in the most urban counties to 11.87 per 100 000 in the most rural counties. Rates of suicide by hanging/suffocation were also higher in rural compared with urban counties for both sexes (Table 3).
Table 3.
Age-Adjusted Mortality Rates for Suicides by Firearm and Hanging/Suffocationa
| Residential Location by Suicide Type and Sex | 1996-1998 | 1999-2001 | 2002-2004 | 2005-2007 | 2008-2010 | Slope | P Value |
|---|---|---|---|---|---|---|---|
| Firearm | |||||||
| Males | |||||||
| 1 (Most urban) | 6.84 | 6.13 | 5.50 | 4.93 | 4.42 | −0.036 | <.001 |
| 2 | 8.44 | 7.54 | 6.74 | 6.03 | 5.39 | −0.037 | <.001 |
| 3 | 8.96 | 8.21 | 7.52 | 6.88 | 6.31 | −0.030 | <.001 |
| 4 | 9.47 | 8.80 | 8.17 | 7.59 | 7.06 | −0.025 | <.001 |
| 5 | 9.25 | 9.11 | 8.97 | 8.83 | 8.70 | −0.007 | .29 |
| 6 | 11.90 | 10.70 | 9.62 | 8.66 | 7.78 | −0.034 | <.001 |
| 7 | 12.14 | 11.54 | 10.97 | 10.42 | 9.91 | −0.019 | <.001 |
| 8/9 (Most rural) | 14.01 | 13.44 | 12.89 | 12.37 | 11.87 | −0.014 | .03 |
| Females | |||||||
| 1 (Most urban) | 0.88 | 0.74 | 0.62 | 0.52 | 0.44 | −0.057 | <.001 |
| 2 | 1.12 | 0.96 | 0.82 | 0.70 | 0.60 | −0.052 | <.001 |
| 3 | 1.24 | 1.08 | 0.93 | 0.80 | 0.69 | −0.051 | <.001 |
| 4 | 1.28 | 1.07 | 0.90 | 0.75 | 0.63 | −0.058 | <.001 |
| 5 | 1.06 | 0.93 | 0.82 | 0.73 | 0.64 | −0.044 | .005 |
| 6 | 1.50 | 1.34 | 1.20 | 1.07 | 0.96 | −0.036 | <.001 |
| 7 | 1.57 | 1.42 | 1.28 | 1.16 | 1.05 | −0.032 | .01 |
| 8/9 (Most rural) | 2.02 | 1.85 | 1.71 | 1.57 | 1.44 | −0.021 | .20 |
| Hanging/Suffocation | |||||||
| Males | |||||||
| 1 (Most urban) | 3.24 | 3.46 | 3.70 | 3.95 | 4.21 | 0.022 | <.001 |
| 2 | 3.58 | 3.81 | 4.05 | 4.31 | 4.59 | 0.022 | <.001 |
| 3 | 3.41 | 3.72 | 4.05 | 4.42 | 4.82 | 0.029 | <.001 |
| 4 | 3.39 | 3.75 | 4.15 | 4.59 | 5.08 | 0.034 | <.001 |
| 5 | 3.07 | 3.60 | 4.22 | 4.94 | 5.80 | 0.052 | <.001 |
| 6 | 3.51 | 3.75 | 4.02 | 4.30 | 4.61 | 0.025 | <.001 |
| 7 | 3.66 | 4.14 | 4.69 | 5.30 | 6.00 | 0.040 | <.001 |
| 8/9 (Most rural) | 4.03 | 4.60 | 5.25 | 6.00 | 6.85 | 0.045 | <.001 |
| Females | |||||||
| 1 (Most urban) | 0.64 | 0.77 | 0.92 | 1.11 | 1.33 | 0.061 | <.001 |
| 2 | 0.64 | 0.79 | 0.96 | 1.17 | 1.43 | 0.066 | <.001 |
| 3 | 0.61 | 0.75 | 0.92 | 1.14 | 1.41 | 0.068 | <.001 |
| 4 | 0.63 | 0.75 | 0.90 | 1.08 | 1.29 | 0.060 | <.001 |
| 5 | 0.59 | 0.74 | 0.93 | 1.18 | 1.48 | 0.074 | <.001 |
| 6 | 0.57 | 0.72 | 0.92 | 1.18 | 1.50 | 0.083 | <.001 |
| 7 | 0.67 | 0.86 | 1.11 | 1.44 | 1.86 | 0.087 | <.001 |
| 8/9 (Most rural) | 0.81 | 1.07 | 1.40 | 1.85 | 2.43 | 0.097 | <.001 |
Suicide rates per 100 000 population aged 10 to 24 years.
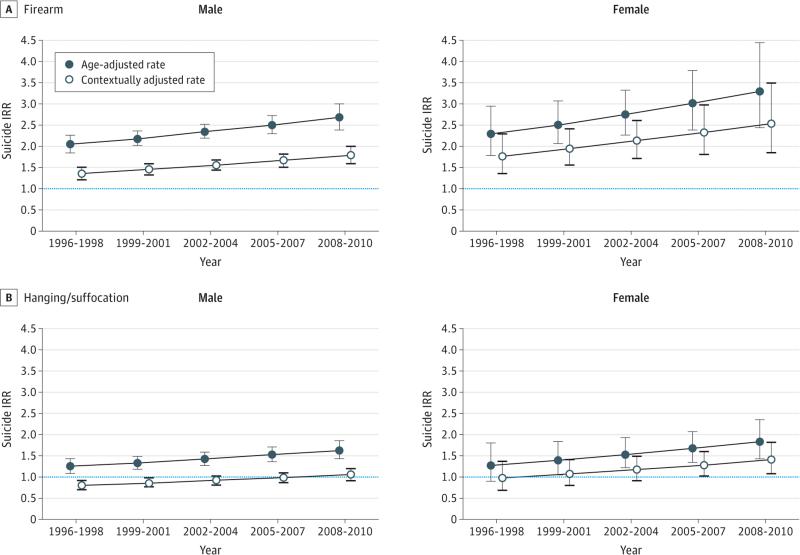
The Figure shows age-adjusted and contextually adjusted IRRs and 95% CIs for the most rural counties compared with the most urban counties for suicide by sex over the 5 time periods. For males, the IRRs for suicide by firearm showed increasing rural-urban differentials across time in both the age-adjusted and contextually adjusted models. For example, in the age-adjusted model during the periods 1996-1998 and 2008-2010, the IRRs for the most rural counties were 2.05 and 2.69 times higher, respectively, than the IRRs for the most urban counties (P = .002). Females showed a similar pattern of increasing rural-urban differentials over the 5 time periods in the age-adjusted and contextually adjusted models (P = .06).
Figure.
Adolescent Suicide Incidence Rate Ratio (IRR) for the Most Rural County Type Relative to the Most Urban County Type for Males and Females by Firearm and Hanging/Suffocation, United States, 1996-2010
The IRRs and 95% CIs for suicide by hanging/suffocation for males and females are shown in the Figure, B (eFigure in the Supplement indicates rates for poisoning and other methods). For males in both the age-adjusted and contextually adjusted models, the rural-urban differentials increased over time (P < .001 for both models). For example, during the periods 1996-1998 and 2008-2010, the age-adjusted IRRs were 1.24 and 1.63 times higher, respectively, in the most rural counties compared with the most urban counties. Females also showed increased rural-urban differentials in the age-adjusted and contextually adjusted models (P = .02 for both).
Discussion
Across the study period from 1996 to 2010, suicide rates for youths in rural areas of the United States were approximately double those in urban areas for both males and females. As expected, suicide rates were higher for males compared with females by a factor of approximately 4 in the present study. Consistent with an earlier report,7 the rural and urban differentials in suicide rates increased significantly over time for males, suggesting widening rural and urban disparities. Male suicide rates significantly declined in the most urban areas during the 15-year study period but remained relatively unchanged in rural areas; however, female suicide rates significantly increased in the most urban and rural areas. Rural-urban disparities persisted even after controlling for a broad array of county-level sociodemographic, economic, and health care system characteristics.
Suicide methods also varied by location, but rural-urban differences were consistent regardless of the method. Overall, rates for suicide by firearm have declined for both males and females, but rates of suicide by hanging/suffocation have increased.16 Rates of suicide by firearm and hanging/suffocation, however, are disproportionately higher in rural areas compared with urban areas. For example, in the most recent time period (2008-2010), the rates for suicide by firearm were between 2.7 and 3.3 times higher for males and females, respectively, in rural areas compared with urban areas. Rates of suicide by hanging/suffocation were 1.6 and 1.8 times higher for males and females, respectively. For suicide by firearm and hanging/suffocation, the rural and urban differential increased significantly for males and females, again suggesting widening rural and urban disparities.
There are several possible explanations for these observed trends. The first involves the limited availability and accessibility of mental health services in rural areas. Although we endeavored to control for the number of health clinicians, real differences in access to care between rural and urban environments remain one plausible explanation for observed rural-urban disparities in the youth suicide rate. Access to mental health care is a long-standing problem in rural communities owing to chronic shortages of clinicians.17 In many rural communities, mental health services and clinicians are not available. Of the 1669 areas federally designated as experiencing a shortage of mental health professionals, more than 85% are in rural areas,18 and more than half of all the counties in the United States (all rural) do not have a practicing psychiatrist, psychologist, or social worker.19 These workforce shortages are even worse for pediatric mental health specialists.20 Because of the relative lack of specialty mental health care, primary care physicians provide a large proportion of mental health care to rural Americans; however, these physicians often feel inadequate and unprepared to diagnosis or treat mental illness.21 Furthermore, primary care physicians who are near retirement age constitute a large proportion of the rural workforce, which is a possible explanation for the increasing workforce shortages in rural areas.22
Many rural residents must travel longer distances to seek health care and often wait longer for appointments. As a result, rural residents may enter care later, with more serious symptoms, and require more expensive and intensive treatments than do their urban peers.23 Compounding the problems of availability and accessibility, rural Americans have lower family incomes and are less likely to have health insurance with mental health benefits.24 Cultural factors also play a significant role in help-seeking behavior, and the stigma associated with mental illness remains a prominent barrier to treatment. Even when services are available, rural residents may not see the need for services owing to low mental health literacy or may be reluctant to use services because of the stigma associated with mental illness and the lack of anonymity in a rural environment.25,26 Rural residents may tend to value self-reliance and individualism, distrust governmental authority, and view help-seeking more negatively than urban residents.27,28
The second possible explanation for the observed trends is geographic and social isolation. The lower population density and wide geography characteristic of rural areas are potentially socially isolating, with less face-to face contact with family, friends, and other support networks. Associated feelings of loneliness and depression could contribute to suicidal behavior. For example, research29 suggests that rural individuals who complete suicide are more likely to have lacked a close intimate relationship than did their urban counterparts. Furthermore, urbanization and lack of employment opportunities have resulted in many residents, particularly the young, leaving rural communities, heightening the degree of isolation for those left behind.25
fAccess to lethal means is another possible factor in the observed trends. The higher suicide rates in rural areas might be attributed in part to greater access to firearms in rural and remote areas. Owning and using firearms is more common among rural residents than among their urban counterparts.27 Rural residents often grow up around guns, have guns in their homes, and use them for hunting, agricultural needs, recreation, or simply because guns are an important part of their culture.25 Suicide is a major cause of gun deaths in rural areas, and evidence suggests that firearm ownership is associated with suicide.30-32 In addition, gun ownership in urban areas is declining but remains stable in rural areas, which may be a contributing factor to the increasing differentials in rural areas.33
The fourth factor in the trends is changing sociodemographic and economic factors. During the past 2 decades, there have been significant sociodemographic and economic changes that may have contributed to the increasing disparities in rural areas. For example, nearly half of nonmetropolitan counties lost population through out-migration and decreased birth rates from 1990 to 2010, with one-third of those counties losing 10% or more of their population; the highest concentration of losses came from the young adult group.34 Population loss weakens the economic infrastructure and is associated with reduced demand and supply for services.34 A declining economy may also have a disproportionately strong effect on rural communities and influence suicide rates. Although both urban and rural areas were affected by the “great recession” of 2007-2009, rural communities were hit especially hard, with high rates of unemployment, loss of jobs, and increasing poverty rates.35 Increasingly fewer people are employed and economic opportunities dwindle, leading to population decline and out-migration of young people.34 These hardships and financial difficulties can precipitate greater feelings of hopelessness, depression, isolation, and substance abuse, with all being risk factors for suicide.
Limitations
This study has some limitations. First, national mortality data may misclassify suicide deaths as accidental or undetermined deaths, leading to underreporting of suicide. This underreporting may be especially true in rural areas owing to the stigma associated with suicide.36,37 However, such misclassification is unlikely to change the results because studies reveal that misclassification in one year tends to occur similarly in subsequent years.38 Second, we were unable to access data on other factors that may have changed within rural and urban counties.
Clinical and Policy Implications
To reduce rural-urban disparities in suicide, community structural factors that affect access to and the availability and acceptability of mental health services must be addressed. Three of the most promising approaches are integrated care services, the use of telemedicine, and school-based interventions.39 Integrating mental health services into primary health care allows provision of physical and mental health services with in the same context, with advantages including familiarity, proximity, ease of access, and relative acceptability for youth and families. Such a model of care might improve early identification of youth at risk, facilitate timely intervention, and provide better monitoring.40 Telemental health, which is the use of technology to provide behavioral health services (eg, broadband Internet and videoconferencing), holds promise in addressing access barriers and has been shown to be effective for the diagnosis, assessment, and treatment of mental health disorders.41 School-based interventions, such as the Signs of Suicide prevention curriculum42 and gatekeeper training,43 may also have potential to reduce suicidal behavior across urban and rural communities. Safe-storage education campaigns or policies designed to restrict access to firearms by young people in rural communities may be particularly salient because where the method of suicide is common, means restriction has led to lower overall suicide rates.44
Conclusions
Across the rural-urban continuum, youth suicide rates are consistently higher in rural compared with urban settings. Rural-urban differences are robust and persistent across the study period regardless of sex and suicide method, but the mechanisms whereby rural residence might increase suicide risk in youth remain elusive. Although low population density per se may be operative, efforts to improve access to mental health services and offer social support at the local level could narrow the gap in risk for youths in rural as opposed to urban settings. Additional study is warranted and of potentially great public health significance.
Supplementary Material
Acknowledgments
Funding/Support: The project described was supported by award number UL1RR025755 from the National Center for Research Resources.
Role of the Funder/Sponsor: The National Center for Research Resources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Fontanella and Mr Phillips had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Fontanella, Phillips, Bridge, Lester, Sweeney, Campo.
Acquisition, analysis, or interpretation of data: Fontanella, Hiance-Steelesmith, Phillips, Lester, Campo.
Drafting of the manuscript: Fontanella, Phillips, Lester, Sweeney, Campo.
Critical revision of the manuscript for important intellectual content: Fontanella, Hiance-Steelesmith, Bridge, Sweeney, Campo.
Statistical analysis: Fontanella, Hiance-Steelesmith, Phillips.
Administrative, technical, or material support: Fontanella, Hiance-Steelesmith, Sweeney, Campo.
Study supervision: Fontanella, Campo.
Conflict of Interest Disclosures: None reported.
Disclaimer: The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources.
Supplemental content at jamapediatrics.com
Contributor Information
Cynthia A. Fontanella, Department of Psychiatry and Behavioral Health, The Ohio State University Wexner Medical Center, Columbus.
Danielle L. Hiance-Steelesmith, College of Social Work, The Ohio State University, Columbus.
Gary S. Phillips, Center for Biostatistics, The Ohio State University, Columbus.
Jeffrey A. Bridge, Center for Innovation in Pediatric Practice, The Research Institute at Nationwide Children's Hospital, Nationwide Children's Hospital, Columbus, Ohio; Department of Pediatrics, The Ohio State University Wexner Medical Center, Columbus.
Natalie Lester, Department of Psychiatry and Behavioral Health, The Ohio State University Wexner Medical Center, Columbus.
Helen Anne Sweeney, Bureau of Research and Evaluation, Ohio Department of Mental Health and Addiction Services, Columbus.
John V. Campo, Department of Psychiatry and Behavioral Health, The Ohio State University Wexner Medical Center, Columbus.
REFERENCES
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control [June 10, 2014];Web-based Injury Statistics Query and Reporting System (WISQARS) http://www.cdc.gov/injury/wisqars.
- 2.Nance ML, Carr BG, Kallan MJ, Branas CC, Wiebe DJ. Variation in pediatric and adolescent firearm mortality rates in rural and urban US counties. Pediatrics. 2010;125(6):1112–1118. doi: 10.1542/peds.2009-3219. [DOI] [PubMed] [Google Scholar]
- 3.Levin KA, Leyland AH. Urban/rural inequalities in suicide in Scotland, 1981-1999. Soc Sci Med. 2005;60(12):2877–2890. doi: 10.1016/j.socscimed.2004.11.025. [DOI] [PubMed] [Google Scholar]
- 4.Middleton N, Gunnell D, Frankel S, Whitley E, Dorling D. Urban-rural differences in suicide trends in young adults: England and Wales, 1981-1998. Soc Sci Med. 2003;57(7):1183–1194. doi: 10.1016/s0277-9536(02)00496-3. [DOI] [PubMed] [Google Scholar]
- 5.Wilkinson D, Gunnell D. Youth suicide trends in Australian metropolitan and non-metropolitan areas, 1988-1997. Aust N Z J Psychiatry. 2000;34(5):822–828. doi: 10.1080/j.1440-1614.2000.00812.x. [DOI] [PubMed] [Google Scholar]
- 6.Singh GK, Azuine RE, Siahpush M, Kogan MD. All-cause and cause-specific mortality among US youth. J Urban Health. 2013;90(3):388–405. doi: 10.1007/s11524-012-9744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh GK, Siahpush M. Increasing rural-urban gradients in US suicide mortality, 1970-1997. Am J Public Health. 2002;92(7):1161–1167. doi: 10.2105/ajph.92.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forrest S. Suicide and the rural adolescent. Adolescence. 1988;23(90):341–347. [PubMed] [Google Scholar]
- 9.National Center for Health Statistics, Centers for Disease Control and Prevention . Multiple Cause of Death, All County Data 1996-2010 From CDC WONDER Database. National Center for Health Statistics; Hyattsville, MD: 2013. Received. [Google Scholar]
- 10.Anderson RN, Miniño AM, Hoyert DL, Rosenberg HM. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. Natl Vital Stat Rep. 2001;49(2):1–32. [PubMed] [Google Scholar]
- 11.US Department of Agriculture [June 10, 2014];Measuring rurality: rural-urban continuum codes. http://webarchives.cdlib.org/sw1wp9v27r/ http:/ers.usda.gov/Briefing/Rurality/RuralUrbCon/. Updated April 28, 2004.
- 12.US Census Bureau [January 23, 2015];Population and housing unit estimates. http://www.census.gov/popest/.
- 13.Health Resources and Services Administration [January 23, 2015];Area Resource File. http://ahrf.hrsa.gov/.
- 14.Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd ed. Wiley; Hoboken, NJ: 2013. chap 4. [Google Scholar]
- 15.StataCorp . Stata Statistical Software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- 16.Bridge JA, Greenhouse JB, Sheftall AH, Fabio A, Campo JV, Kelleher KJ. Changes in suicide rates by hanging and/or suffocation and firearms among young persons aged 10-24 years in the United States: 1992-2006. J Adolesc Health. 2010;46(5):503–505. doi: 10.1016/j.jadohealth.2009.11.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lambert D, Agger MS. Access of rural AFDC Medicaid beneficiaries to mental health services. Health Care Financ Rev. 1995;17(1):133–145. [PMC free article] [PubMed] [Google Scholar]
- 18.Bird DC, Dempsey P, Hartley D. Addressing Mental Health Workforce Needs in Underserved Rural Areas: Accomplishments and Challenges. Maine Rural Health Research Center, Muskie Institute, University of Southern Maine; Portland: 2001. [Google Scholar]
- 19.National Advisory Committee on Rural Health . Sixth Annual Report on Rural Health. Office of Rural Health Policy, Health Resources and Services Administration, Health and Human Services; Rockville, MD: 1993. [Google Scholar]
- 20.New Freedom Commission on Mental Health . Subcommittee on Rural Issues: Background Papers. Dept of Health and Human Services; Rockville, MD: 2004. DHHS publication No. SMA-04-2890. [Google Scholar]
- 21.Gale JA, Lambert D. Mental healthcare in rural communities: the once and future role of primary care. N C Med J. 2006;67(1):66–70. [PubMed] [Google Scholar]
- 22.Rosenblatt RA, Chen FM, Lishner DM, Doescher MP. The Future of Family Medicine and Implications for Rural Primary Care Physician Supply. WWAMI Rural Health Research Center, University of Washington; Seattle, WA: 2012. [Google Scholar]
- 23.Rost K, Fortney J, Fischer E, Smith J. Use, quality, and outcomes of care for mental health. Med Care Res Rev. 2002;59(3):231–265. doi: 10.1177/1077558702059003001. [DOI] [PubMed] [Google Scholar]
- 24.McDonnell K, Fronstin P. EBRI Health Benefits Databook. Employee Benefit Research Institute; Washington, DC: 1999. [Google Scholar]
- 25.Cantrell C, Valley-Gray S, Cash RE. Suicide in rural areas: risk factors and prevention. In: Smalley KB, Warren JC, Rainer JP, editors. Rural Mental Health. Springer; New York, NY: 2012. pp. 213–228. [Google Scholar]
- 26.Judd F, Cooper AM, Fraser C, Davis J. Rural suicide—people or place effects? Aust N Z J Psychiatry. 2006;40(3):208–216. doi: 10.1080/j.1440-1614.2006.01776.x. [DOI] [PubMed] [Google Scholar]
- 27.Hirsch JK. A review of the literature on rural suicide. Crisis. 2006;27(4):189–199. doi: 10.1027/0227-5910.27.4.189. [DOI] [PubMed] [Google Scholar]
- 28.Hoyt DR, Conger RD, Valde JG, Weihs K. Psychological distress and help seeking in rural America. Am J Community Psychol. 1997;25(4):449–470. doi: 10.1023/a:1024655521619. [DOI] [PubMed] [Google Scholar]
- 29.Isometsä E, Heikkinen M, Henriksson M, Marttunen M, Aro H, Lönnqvist J. Differences between urban and rural suicides. Acta Psychiatr Scand. 1997;95(4):297–305. doi: 10.1111/j.1600-0447.1997.tb09635.x. [DOI] [PubMed] [Google Scholar]
- 30.Dresang LT. Gun deaths in rural and urban settings: recommendations for prevention. J Am Board Fam Pract. 2001;14(2):107–115. [PubMed] [Google Scholar]
- 31.Branas CC, Nance ML, Elliott MR, Richmond TS, Schwab CW. Urban-rural shifts in intentional firearm death. Am J Public Health. 2004;94(10):1750–1755. doi: 10.2105/ajph.94.10.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brent DA, Bridge J. Firearms availability and suicide. Am Behav Sci. 2003;46(30):1192–1210. [Google Scholar]
- 33.Wright JD, Jasinski JL, Lanier DN. Crime, punishment, and social disorder: crime rates and public opinion over more than three decades. In: Marsden PV, editor. Social Trends in American Life. Princeton University Press; Princeton, NJ: 2012. pp. 146–176. [Google Scholar]
- 34.McGranahan D, Cromartie J, Wojan T. Economic Research Report No. 35. US Dept of Agriculture; Washington, DC: 2010. Nonmetropolitan outmigration counties: some are poor, many are prosperous. pp. 1–24. [Google Scholar]
- 35.Kusmin L, Hertz T. Rural America at a Glance, 2010 ed. US Dept of Agriculture; Washington, DC: 2010. Economic Information Bulletin No. 6. [Google Scholar]
- 36.Beeson PG. Some notes and data on rural suicide. Rural Mental Health. 2000;23:13–15. [Google Scholar]
- 37.Saunderson T, Haynes R, Langford IH. Urban-rural variations in suicides and undetermined deaths in England and Wales. J Public Health Med. 1998;20(3):261–267. doi: 10.1093/oxfordjournals.pubmed.a024767. [DOI] [PubMed] [Google Scholar]
- 38.Mohler B, Earls F. Trends in adolescent suicide: misclassification bias? Am J Public Health. 2001;91(1):150–153. doi: 10.2105/ajph.91.1.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smalley KB, Warren JC. The current state of rural mental health. In: Smalley KB, Warren JC, Rainer JP, editors. Rural Mental Health. Springer; New York, NY: 2012. pp. 3–16. [Google Scholar]
- 40.Kane CF, Ennis JM. Health care reform and rural mental health: severe mental illness. Community Ment Health J. 1996;32(5):445–462. doi: 10.1007/BF02251045. [DOI] [PubMed] [Google Scholar]
- 41.Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013;19(6):444–454. doi: 10.1089/tmj.2013.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aseltine RH, Jr, DeMartino R. An outcome evaluation of the SOS suicide prevention program. Am J Public Health. 2004;94(3):446–451. doi: 10.2105/ajph.94.3.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.King KA, Smith J. Project SOAR: a training program to increase school counselors’ knowledge and confidence regarding suicide prevention and intervention. J Sch Health. 2000;70(10):402–407. doi: 10.1111/j.1746-1561.2000.tb07227.x. [DOI] [PubMed] [Google Scholar]
- 44.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.