Abstract
Coronal fractures of the femoral condyle (Hoffa fracture) are rare injuries but can be managed with satisfactory outcome if properly treated. We discuss an unusual case of a young adult male presenting with 9 month old neglected Hoffa fracture with pain, stiffness and limitation of knee movement, managed with sandwich bone grafting technique.1
Keywords: Hoffa, Femoral condyle, Intraarticular fracture, Sandwich bone grafting
1. Introduction
Unicondylar fractures of femoral condyle were first described by Hoffa1 in 1904. This is a rare injury in adults and reports illustrating management of non-union Hoffa fracture are even more rare. Poor outcome is usual with nonoperative management.2–5 Appropriate approach to a patient with Hoffa fracture should be atraumatic anatomic reduction of fracture fragments rigid enough to allow early aggressive range of motion exercises. We discuss the unusual case of a young adult male presenting with 9 month old non-union Hoffa fracture initially treated with conservative management by osteopaths. This case illustrates the approach to a case of non-union Hoffa fracture with good functional outcome as evident from high Knee Society scores.6
2. Case report
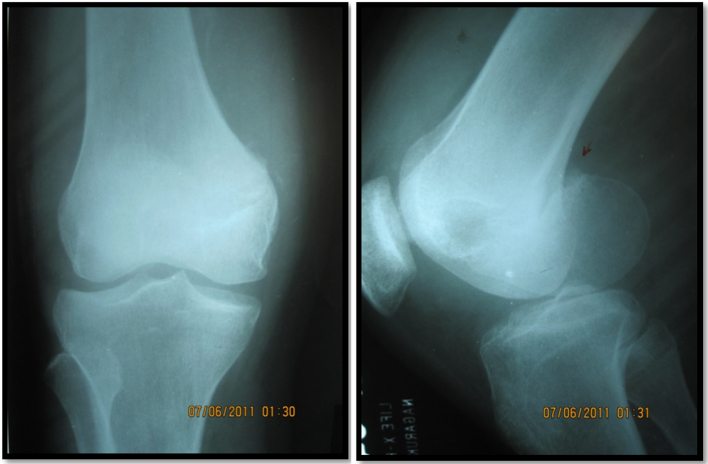
A 16-year-old male patient presented to us with chief complaints of pain in the left knee for last 9 months following trauma 9 months ago. The history of antecedent trauma was significant. Following the initial insult patient was unable to stand or walk himself due to intense pain and swelling around the left knee. He was taken to some osteopaths where he received some indigenous treatment. No radiograph was taken. Irregular intake of painkillers, crepe bandage application and alternate hot and cold fomentation decreased the intensity of his pain but it was never completely painfree. Gradually he developed stiffness of the left knee joint interfering with his daily activities. On taking radiograph (Fig. 1) we found coronal fracture of left medial femoral condyle with smoothening of fracture lines. Diagnosis now stands out to be a case of 9 month old non-union Hoffa fracture in a 16-year-old male patient with limitation of joint movement. History and clinical examination did not reveal any findings suggestive of any other joint involvement. After detailed counselling about the present scenario and probable guarded prognosis we prepared the patient for operative intervention as per protocol in our institute.
Fig. 1.
Preoperative radiograph.
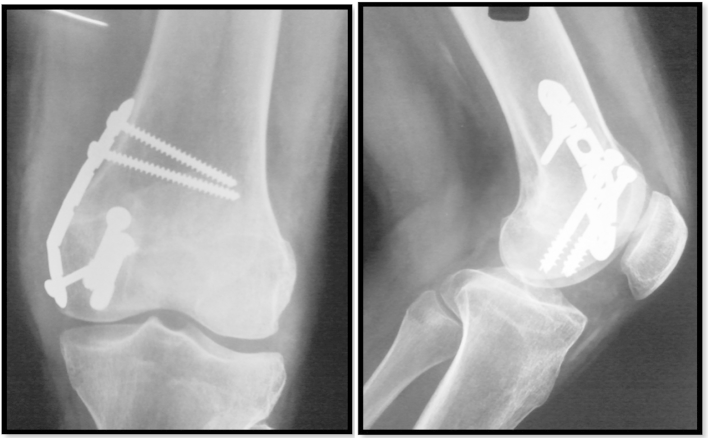
We planned for open reduction and internal fixation with bone grafting by a sandwich technique (Fig. 2).
Fig. 2.
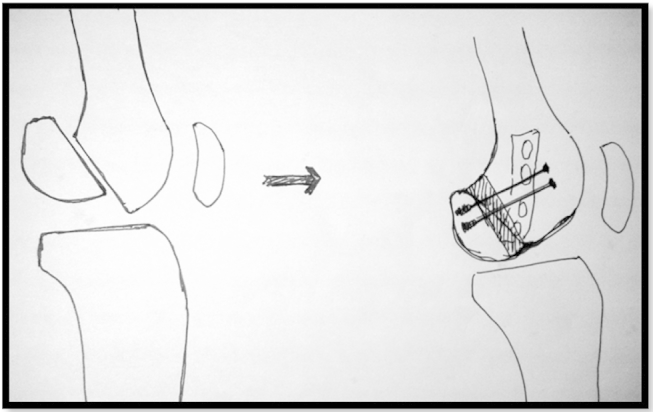
Operative technique with interposition bone graft, lag screw and neutralisation plate.
Medial subvastus approach was chosen. After joint inspection, the fracture fragments are separated with a bone spreader and debrided. A rough idea regarding the amount of bone resorption at the fracture site is obtained and approximately a 10 × 30 × 10 mm sized corticocancellous bonegraft was harvested from the iliac crest. The fracture is anatomically reduced and held compressed with Weber bone clamps. Bonegraft was interposed in between the fracture fragments. Two 6.5 mm partially threaded cannulated cancellous screws are applied starting at a level commensurate with the highest point of the trochlear notch, directed perpendicular to the fracture plane in lag mode. A 6 hole 3.5 mm recon plate was applied as neutralisation plate. Tourniquette time was 75 min and blood loss was less than 100 ml. Active assisted range of motion exercises of knee joint was started from the first postoperative day. Weight bearing was restricted for initial 8 weeks but gradual protected weight bearing was started from 10th week onwards as radiographic evidence of union was present. There was no postoperative infection and till date the active range of motion of left knee joint is 0 ͦto 150 ͦ; painless, no muscle spasm, no crepitus, arc of motion is smooth and. At 1.5-year follow-up, patient is leading his normal day to day activities without any functional limitations with radiological evidence of union (Fig. 3) and full functional range of motion (Fig. 4) with Knee Society score 173 out of 200 points at the final follow-up.
Fig. 3.
1.5 years radiological follow-up.
Fig. 4.
Full range of motion at 1.5 years follow-up.
3. Discussion
Hoffa fractures are rare injuries, and lateral fractures are more common than medial fractures. They usually occur as isolated injuries to involved femur, but bilateral Hoffa fracture7 and unilateral bicondylar8 Hoffa fracture have been reported. In addition, Hoffa fracture with supracondylar intercondylar (AO/OTA 33C) femur fracture have been observed9, and reporting authors highlights the need for preoperative detection of Hoffa fracture to select appropriate fixation method for supracondylar fracture femur.
The specific mechanism of injury that produce Hoffa fracture is unknown, but a shearing force on posterior femoral condyle is postulated10. Lewis et al.4 argued that axial load to the lateral femoral condyle with the knee in 90 ͦ or more of flexion produces posterior tangential fracture patterns. Four of seven patients in their series were riding motorcycle at the time of injury, placing the knee in 90 ͦ of flexion and positioning lateral femoral condyle to an impact. In Hoffa fracture, knee movements particularly weight bearing causes high shear forces along the fracture plane, making nonoperative management unpredictable and adequate stabilisation challenging.
Examination invariably will identify effusion but varus and valgus instability may be subtle. The neurovascular status should be assessed as in high energy knee injuries. Initially anteroposterior and lateral radiographs may be unimpressive, because Hoffa fractures, especially when nondisplaced, are difficult to detect11. On the anteroposterior radiograph, the foreshortened fractured condyle may lead to appearance of varus or valgus malalignment. On a true lateral view, the femoral condyles are not superimposed and this may be misinterpreted as a poor radiographic view of normal knee. Oblique radiograph may be helpful; if standard radiographic views do not confirm and define the fracture, a CT scan is necessary.
In an attempt to predict which coronal plane fracture of the femoral condyle would progress to avascular necrosis, Letenneur et al.3 proposed dividing fracture in three types, based on distances of fracture line from posterior cortex of femoral shaft. A subsequent report from lewis et al.4 failed to validate this classification. The AO comprehensive classification of long bone fracture and OTA fracture compendium identify the unicondylar coronal fracture but provide little information about prognosis or treatment12,13 .
Although it is generally accepted that surgical stabilisation is necessary to achieve satisfactory function following Hoffa fracture3–6, a few reports in the literature which describe operative treatment, do not outline clearly a straightforward, dependable treatment approach and they vary considerably in view of surgical approach, postoperative protocol and outcome measures. There is a dearth of specific information on the preferred management of this fracture in several popular orthopaedic fracture management texts14–16. We found 18 articles concerning management of Hoffa fracture; 5 of these reports simply included Hoffa fracture as a part of series of unicondylar distal femur fracture. The report of Lewis et al.4 on seven coronal fracture of lateral femoral condyle represents the largest single group of patients studied, but only five patients were treated operatively. They used either medial parapatellar arthrotomy or direct lateral approach between iliotibial band biceps tendon to expose the fracture and two nonparallel screws to fix it. Postoperatively, patients were placed in cylindrical cast for 2–6 weeks depending stability achieved intraoperatively. All five fractures, treated surgically, healed and at final follow-up (average 13 months), knee range of motion averaged 110 ͦ(95 ͦ to 135 ͦ).
Two reports of arthroscopically assisted reduction and internal fixation of femoral condyle fracture have been published10,17. Wallenbock and lendeski10 reported a series of 24 intraarticular knee fractures that they treated by arthroscopically assisted reduction and internal fixation, which included two Hoffa fractures. Although noting that the technique of arthroscopically assisted reduction is demanding, they reported good early results. They did not describe specifically the technique and outcome of the patients with coronal fractures. McCarthy and Parker17 described a patient with sagittal plane lateral femoral condyle fracture. Although their fixation do not achieve a rigid compression18, they cited reduced soft tissue dissection, blood loss, and operative time and a faster recovery time after arthroscopic management as advantage over formal open reduction. It is difficult to conclude from these two reports that arthroscopically assisted reduction and internal fixation has any clear advantage over open technique.
Ostermann et al.19 emphasise fracture compression and rigid fixation to allow immediate postoperative knee motion in their report on long term (average 68 months) results of 29 unicondylar femur fracture, of which six were Hoffa fracture. They did not describe their surgical approach and outcome of the patient with Hoffa fracture, but they noted that 23 of 27 patients available for follow up had excellent result.
Manfredini et al.5 surgically treated 9 patients with unicondylar femur fracture six of which were Hoffa fracture, using a variety of open reduction and internal fixation technique. Four patients with unicondylar femur fracture were treated nonoperatively in casts. Amongst the patients treated surgically 16 were available for follow up at a mean of 60 months, 11 had a good or excellent results and 5 have fair or poor results. The 4 patients treated nonoperatively had unfavourable outcome, with 3 fair and 1 poor result.
Liebergall et al.20 described a lateral approach to the knee, using an osteotomy of Gerdy's tubercle, in treatment of lateral condyle coronal fracture, but did not offer any outcome data on this single case. The author argued that osteotomy permits improved visualisation for open reduction and internal fixation.
A cadaveric study compared the stiffness and load to failure of 3.5 mm cortical lag screw, 4.5 cortical lag screws, and 6.5 mm cancellous screws used to fix experimentally created Hoffa fractures21. There was no difference in stiffness between any of the groups, but the load to failure was significantly higher for screw 6.5 mm compared with 3.5 mm screws. The investigator questioned whether that result was clinically significant and noted that smaller screws, such as 3.5 mm cortical screw, may be much easier to fit around a rigid implant if such fixation is necessary, as in the case of a supracondylar femur fracture with an associated Hoffa fracture.
Commonly referred orthopaedics fracture management text books offer a paucity of information regarding the surgical management of Hoffa fracture. One major text does not even mention this fracture pattern. Muller and Allgower's Manual of Internal Fixation15 include a diagram of Hoffa fracture fixed with 2 anteroposterior screws but does not offers a text description. Schatzker and Tile16 described the Hoffa fracture pattern and noted that nonoperative treatment of Hoffa fracture lead to poor function but otherwise did not offer a management approach.
Our single case report of operatively treated isolated Hoffa fracture non-union is unique in that, in contrast to reports of Lewis et al. and Manfredini et al.5, we employ a standard surgical approach to the fracture and achieve rigid fixation with optimally positioned lag screw placed perpendicular to fracture plane. We believe that medial subvastus approach provide the visualisation of fracture and articular surface necessary for achieving a perfect anatomic reduction and exposure to compress and rigidly fix the fracture with multiple lag screws. The excellent fracture stability thus achieved allows for unrestricted immediate range of motion of the joint, minimizing the risk of postoperative joint ankylosis. As more fractures are managed with limited open and percutaneous technique, the Hoffa fracture pattern stands out as one that is still managed best by a “low-tech’’ formal open reduction and classic lag screw fixation. In our hands, this method led to uniformly good result without complication.
Conflicts of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Hoffa A. Leharbuch der frackturen und luxationen. Stugert: Verleg Von Ferdinand enke. 1904:451. [Google Scholar]
- 2.Letennuer J., Labour P.E., Rogez jm. Fracture de Hoffa; a propose de 20 observation. Ann Chir. 1978;32:213–219. [PubMed] [Google Scholar]
- 3.Lewis S.L., Pozo J.L., Muirhead-allwood W.F.G. Coronal fracture of the lateral femoral condyle. J bone Jt Surg Br. 1989;71:118–120. doi: 10.1302/0301-620X.71B1.2914979. [DOI] [PubMed] [Google Scholar]
- 4.Manfredini M., Gildone A., Ferrante R. Unicondylar femoral fracture: therapeutic strategy and long term results. Acta Orthop Belg. 2001;67:132–138. [PubMed] [Google Scholar]
- 5.McDonough P.W., Bernstein Rm. Non-union off fracture in a child. J Orthop Trauma. 2000;14:519–521. doi: 10.1097/00005131-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Insall J.N., Dorr L.D., Scott R.D. Rational of the knee society clinical rating system. Clin Orthop. 1989;248:13–14. [PubMed] [Google Scholar]
- 7.Heushen U.A., Gohring U., Meeder P.J. Die Beidseitige Hoffa – fraktureine Raritat. Aktuelle Traumatol. 1994;24:83–86. [PubMed] [Google Scholar]
- 8.Zeebregts C.J., Zimmerman K.W., ten duis H.J. Operative treatment of a unilateral bicondylar fracture femur. Acta Chir Belg. 2000;100:1104–1106. [PubMed] [Google Scholar]
- 9.Baker B.J., Escobebo E.M., Nork S.E. Hoffa fracture: a common association with high energy supracondylar fracture of distal femur. AJR Am J Roentgenol. 2002;178:994. doi: 10.2214/ajr.178.4.1780994. [DOI] [PubMed] [Google Scholar]
- 10.Wallenbock E., Ledinski C. Indication and limits of arthroscopic management of intraarticular fracture of knee joint. Aketuelle Traumatol. 1993;23:97–101. [German] [PubMed] [Google Scholar]
- 11.Allman K.H., Altehoefer C., Wildanger G. Hoffa fracture – a radiological diagnostic approach. J Belge Radiol. 1996;79:201–202. [PubMed] [Google Scholar]
- 12.Muller M.E., Nazarian S., Koch P., Schatzker J. Springer–Verlag; Berlin: 1990. The Comprehensive Classification of Fracture of Long Bones. 145–145. [Google Scholar]
- 13.Orthopaedic Trauma Association Committee for Coding and Classification Fracture and dislocation compendium: distal femur. J Orthop Trauma. 1996;10:45. [PubMed] [Google Scholar]
- 14.Browner B.D., Jupiter J.B., Levine A.M. 2nd ed. WB Saunders; Philadelphia, PA: 1998. Skeletal Trauma. [Google Scholar]
- 15.Muller M.E., Allgower M., Schneider R. 3rd ed. Springer–Verlag; New York, NY: 1995. Manual of Internal Fixation; p. 549. [Google Scholar]
- 16.Schatzer J., Tile M. 2nd ed. Springer–Verlag; Berlin: 1996. The Rationale of Operative Care; pp. 390–391. [Google Scholar]
- 17.McCarthy J.J., Parker R.D. Arthroscopic reduction and internal fixation of a displaced intraarticular lateral femoral condyle fracture of the knee. Arthroscopy. 1996;12:224–227. doi: 10.1016/s0749-8063(96)90016-x. [DOI] [PubMed] [Google Scholar]
- 18.Stem R.E. Comment arthroscopy. 1996;12:760–761. [Google Scholar]
- 19.Ostermann P.A., Hahn M.P., Ekkemkamp A. Monocondylar frakturen des femur. Chirung. 1997;68:72–76. doi: 10.1007/s001040050153. [DOI] [PubMed] [Google Scholar]
- 20.Liebergall M., Wilber J.H., Mosheiff R. Gerdy's tubercle osteotomy for treatment of coronal fracture of the lateral femoral condyle. J Orthop Trauma. 2000;14:214–215. doi: 10.1097/00005131-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Becker P.L., Staford P.R., Goulet R. Presented at the 67th Annual Meeting of the American Academy of Orthopaedic Surgeons. March15–19, 2000. Comparative analysis for the fixation of coronal distal intra articular femur fracture. [Google Scholar]