Abstract
Objective
To assess the potential benefit of digital health interventions (DHI) on cardiovascular disease outcomes (CVD events, all-cause mortality, hospitalizations) and risk factors compared to non-DHI interventions.
Patients and Methods
We conducted a systematic search of PubMed, MEDLINE, EMBASE, Web of Science, OVID, CINHAL, ERIC, PsychInfo, Cochrane, and CENTRAL from January 1, 1990 and January 21, 2014. Included studies examined any element of DHI (telemedicine, web-based strategies, email, mobile phones, mobile applications, text messaging, and monitoring sensors) and CVD outcomes or risk factors. Two reviewers independently evaluated study quality utilizing a modified version of the Cochrane Collaboration risk assessment tool. Authors extracted CVD outcomes and risk factors for CVD such as weight, BMI, blood pressure, and lipids from 51 full-text articles that met validity and inclusion criteria.
Results
DHI significantly reduced CVD outcomes (RR=0.61, (95% CI, 0.45–0.83), P=.002; I2=22%). Concomitant reductions in weight (−3.35 lbs, (95% CI, −6.08 lbs, −1.01 lbs); P=.006; I2=96%) and BMI (−0.59 kg/m2, (95% CI, −1.15 kg/m2, −0.03 kg/m2); P=.04; I2=94%) but not blood pressure (+4.95 mmHg, (95% CI, −4.5 mmHg, 14.4 mmHg); P=.30; I2=100%) were found in these DHI trials compared to usual care. Framingham 10 year risk percentages were also significantly improved (−1.24%; 95% CI −1.73%, −0.76%; n=6; P<0.001; I2=94%). Results were limited by heterogeneity not fully explained by study population (primary or secondary prevention) or DHI modality.
Conclusions
Overall, these aggregations of data provide evidence that DHI can reduce CVD outcomes and have a positive impact on risk factors for CVD.
Keywords: cardiovascular disease, outcomes, digital health, mobile health, prevention, weight loss, MACE
Introduction
Cardiovascular disease (CVD) is the primary cause for morbidity and mortality, and is associated with markedly rising health care costs in the United States 1. Approximately one in three deaths can be attributed to CVD 1,2, and over 90% of CVD morbidity and mortality to preventable risk factors 3. According to 2012 statistics, poor diet, smoking, and lack of physical activity continue to account for an overwhelming majority of CVD and death 4 with the cost of CVD to the US approaching $200 billion per year 1. What is more, the average hospitalization for acute coronary syndrome (ACS) is estimated to cost roughly $20,000 with repeat events costing up to two and three times the original amount 5. Clearly, better interventions to improve CVD prevention, both primary and secondary, are needed.
Internet and smart phone use has grown exponentially in the past decade, opening up the possibility that these increasingly prevalent technological tools could improve health. Digital health interventions (DHI), including such modalities as telemedicine, web-based strategies, email, mobile phones, mobile applications, text messaging, and monitoring sensors, are the most recent iteration of an effort to shift health care burden outside of the walls of medical institutions, and improve individualized care through positive behavior change theory 6. Although prior studies have suggested benefits of DHI in focused areas such as smoking cessation 7, behavior patterns 8, physical activity 9, HbA1c 10, blood pressure 11, and weight loss 12, evidence concerning the benefit of DHI on CVD risk factors, let alone CVD outcomes such as CVD events, hospitalizations, and all-cause mortality, is lacking. With nearly 50,000 healthcare related apps now available for download 13, and numerous internet-based DHI solutions available, the benefit of DHI on CVD prevention and outcomes, both primary and secondary, merits reexamination.
The purpose of this systematic review and meta-analysis was to inclusively review randomized controlled trials (RCTs) and cohort studies incorporating DHI for the prevention of CVD outcomes (CVD events including myocardial infarction, stroke, revascularization, hospitalizations, and all-cause mortality) and modification of risk factors for CVD such as weight, BMI, blood pressure, cholesterol, glucose, and Framingham Risk Scores (FRS). We aim to establish the potential benefit of DHI on both primary and secondary CVD prevention, and identify future needs in DHI and CVD research.
Methods
Data Sources and Searches
This systematic review was conducted in accordance with PRISMA guidelines 14. We included all RCTs and observational/cohort studies published between January 1, 1990 and January 21, 2014 that examined any element of DHI (telemedicine, web-based strategies, email, mobile phones, mobile applications, text messaging, and monitoring sensors) and impact on CVD. We intentionally and broadly included any studies of adult patients seeking CVD prevention to present a comprehensive overview of DHI studies analyzing CVD outcomes (CVD events, hospitalizations, or all-cause mortality) and modification of risk factors for CVD such as weight, BMI, blood pressure, cholesterol, glucose, and FRS regardless of type of healthcare provider or healthcare setting. Control interventions included usual care following standard guidelines, and could involve non-DHI intervention (such as paper instructions or telephone calls) or no active intervention beyond usual care. We excluded studies in which the intervention lasted less than a month in order to assess long-term impact and sustainability, studies that did not report any CVD risk factors, redundant studies which were repeated in the literature without new data presented, protocol manuscripts, reviews, studies only including usability or adherence data, pediatric studies, and studies where the intervention involved the healthcare provider, rather than the patient.
Our search strategy was performed with the assistance of a medical librarian, and included the databases PubMed, MEDLINE, EMBASE, Web of Science, OVID, CINAHL, ERIC, PsychInfo, Cochrane, and CENTRAL over the specified dates. We included the search terms mobile health, mobile, mhealth, digital health, eHealth, internet, telemedicine, web, smartphone, cardiovascular, cardiac, prevention, outcomes, mortality, morbidity, event, Framingham, blood pressure, weight, BMI, waist circumference, glucose, lipids, cholesterol, smoking, tobacco, quality of life, emergency department, visits, hospitalizations, rehospitalizations, office visits, phone calls, cost, cost of care, and ROI. This strategy identified 574 relevant abstracts with an additional 14 references identified through bibliography searches and personal contacts (Figure 1). Most articles were in English, and those in Spanish, Polish, and German were translated for review.
Figure 1.
PRISMA schematic for study selection.
Study Selection
Two reviewers (RJW and NMC) assessed each of the identified abstracts. Full text versions of potentially eligible studies, categorized for inclusion by either reviewer, were requested (n=73). The two reviewers worked independently to evaluate the full text reports for study inclusion and disagreements were reconciled by consensus. Agreement on study inclusion was high, with kappa = 0.92.
Data Extraction and Quality Assessment
Extracted data included study participant demographics (age, gender, prior internet use, education level, socioeconomic status, race, comorbidities, and baseline markers of CVD), the DHI they received (frequency, type, and duration), and the control intervention. DHIs were identified as involving telemedicine, web-based strategies, email, mobile phones, mobile applications, SMS text messaging, and monitoring sensors. Control comparisons were heterogeneous and could include a non-DHI intervention or usual care. CVD outcomes included CVD events including myocardial infarction, stroke, or revascularization, hospitalizations, and all-cause mortality. Risk factors for CVD included weight, BMI, blood pressure, cholesterol, (total cholesterol, LDL-cholesterol, HDL-cholesterol, and triglycerides), glucose, and FRS.
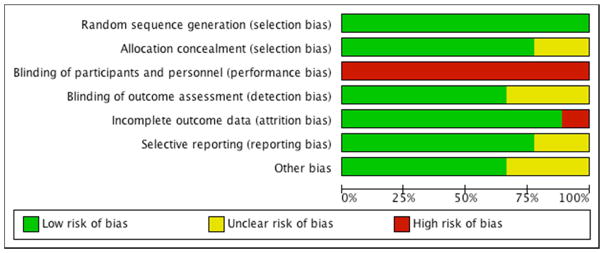
Risk of bias and methodological quality was assessed independently by two authors (RJW and CSC) using a modified version of the Cochrane Collaboration risk assessment tool 15 (Supplementary Figure 1). To evaluate the quality of non-randomized studies, we assessed blinding of the outcome assessors to arm assignment in relation to the outcomes of CVD outcomes and CVD surrogates, comparability of outcome assessment, and completeness of follow-up. The latter criteria followed a revised Newscastle–Ottawa quality assessment tool for observational studies16 (Supplementary Figure 1) which emphasized proper definition of the CVD pertinent to the study, legitimate DHI intervention, and reasonable follow up. One study (Nolan, 2012) was considered an observational study as the randomization scheme was compromised due to unintentional cross-over of the participants forcing the authors to report the data in separate, non-randomized cohorts. Finally, a study by Wister et al 17 allowed separation of studies for primary and secondary prevention.
Data Synthesis and Analysis
When possible, we generated meta-analytic estimates of treatment effect using pooled relative risks and random-effects models. Analyses were performed using RevMan v.5.2 (The Cochrane Collaboration; Oxford, UK). We measured heterogeneity for each outcome across studies using the I2 test 18. When standard deviations were missing for a study, imputation of the mean standard deviation of the group for that particular variable was utilized in no more than two values per variable. Imputation of more than two standard deviations was not required for any analysis.
To explore causes of inconsistency in study findings and subgroup-treatment interactions, we planned subgroup analyses comparing results by patient population (primary prevention versus secondary prevention) and DHI subtype (telemedicine, web-based, email reminders, SMS texting, mobile application, and data monitoring). Random effects methods utilizing Mantel-Haenszel methods for combining results across studies were undertaken as part of the RevMan 5.2 software package 18. Sensitivity analyses controlling for workplace versus healthcare delivered DHI were performed as were sensitivity analyses removing the two observational, non-randomized studies.
We contacted all authors with a prepopulated form including data for verification and missing data for their completion. Of the original 49 authors contacted, 28 returned correspondence with either verification of reported data, or the addition of missing or incomplete data. There was no impact of the funding source on the design, execution, or analysis of the study.
Results
Fifty-one studies met criteria for full-text review and were included in the systematic review with nine studies providing analyzable CVD outcome data. A summary table of studies reporting CVD outcomes is presented in Table 1. Risk of bias among studies reporting CVD outcomes was predominantly low apart from a consistent lack of participant blinding (Table 2) with a funnel plot included (Supplementary Figure 2).
Table 1.
RCTs reporting CVD outcomes with DHI (n=9)
| Study ID | Duration (mo) | Total N | DHI N | Study Population | DHI | Findings |
|---|---|---|---|---|---|---|
| Appel, 201126 | 24 | 415 | 139 | Primary Prevention, Hypertension | Web-based | Larger, healthcare site obesity intervention delivered remotely or in person significantly reduced weight (−4.6 kg and −5.1 kg, respectively) vs. controls. No impact on CVD events, rehospitalizations, or all-cause mortality. |
| Blasco 201227 | 12 | 203 | 102 | Secondary Prevention | SMS text, Smart Phone | Healthcare secondary prevention trial showing improved secondary prevention outcomes (repeat CVD events, rehospitalizations, or all-cause mortality; RR = 1.4; 95% CI = 1.1–1.7) with telemonitoring and SMS text. |
| Dendale, 201228 | 6 | 160 | 80 | Secondary Prevention, Heart Failure | Telephone, Data Monitoring | Healthcare-delivered telemonitoring service in HF patients showed significantly reduced all-cause mortality (P=.01) but did not reduce hospitalizations per patient (0.24 vs. 0.42, P=.06). |
| Frederix, 201329 | 4.5 | 80 | 40 | Secondary Prevention | Email, SMS text, Data Monitoring | Body sensor data-monitoring in CR patients improved exercise capacity (26.88+220.33 ml/min vs. 285.89+385.44 ml/min, P=.014) and improvements in rehospitalizations. |
| Green, 200930 | 12 | 778 | 520 | Primary Prevention | Telephone, Web-based | Hypertensive patients assigned to usual care vs. a web-based or telephone-based intervention showed those using the web-based platform had a greater percentage of achieving target BP (55% vs. 39%; 95% CI, 49%–62%; P < .001). Increased adverse events in intervention group. |
| Reid, 201231 | 12 | 223 | 115 | Secondary Prevention | Web-based | Internet-based data monitoring for physical activity in post-MI patients showed significant improvements in physical activity and QOL compared to usual care. The intervention had a small, non-significant effect on hard CVD outcomes. |
| Scherr, 200920 | 6 | 120 | 54 | Secondary Prevention, Heart Failure | Telephone, SMS text, Data Monitoring | Data monitoring in patients with recent decompensated HF showed a high attrition rate; yet a 50% reduction in CVD endpoints and hospitalizations with a mean improvement in NYHA class by one category in the treatment group. |
| Southard, 200332 | 6 | 104 | 53 | Secondary Prevention | Web-based | Internet-based secondary prevention tool reduced CVD endpoints (15.7% vs. 4.6%) and provided a significant cost savings. The intervention group had a more robust weight loss (−3.68 lbs. vs. 0.47 pounds, P =.003), with no other surrogate markers of CVD achieving statistical significance. |
| Vernooij, 201233 | 12 | 330 | 164 | Secondary Prevention | Web-based | Clinic-based online risk factor improvement tool showed a significant reduction in Framingham scores (−14%; −25% to − 2%) after 12 months in patients randomized to the intervention. No significant reduction in CVD events, death, and hospitalizations in DHI group. |
Table 2.
Risk of bias for outcomes studies:
Assessment of risk of bias based validity assessment tool used by authors (Supplementary Figure 1) for the nine studies with CVD outcomes analyzed. The x-axis represents the percentage of studies which were found to be of low (green), unclear (yellow), or high (red) risk of bias.
|
Thirty-nine studies focused on primary CVD prevention (Supplementary Table 1A) and 13 studies primarily involved secondary CVD prevention (Supplementary Table 1B) (one study fit into both categories separately). The total number of patients included was 23,962, with 13,618 assigned to DHI and 10,344 to control groups. Mean age (SD) for all of the participants in the studies was 54.0 (9.4) years with a majority of the participants being Caucasian and 54% male. Five studies evaluated a solely female population, and two focused only on male participants. Socioeconomic status, geographical information, and prior internet usage were not universally reported. Additionally, the timeframe of a majority of studies was between 6 and 12 months, and most studies were published within the past decade. RCTs were blinded with specific mention of study personnel blinded to allocation and grouping during the study and to data analysis, with the exception of three studies 19–21.
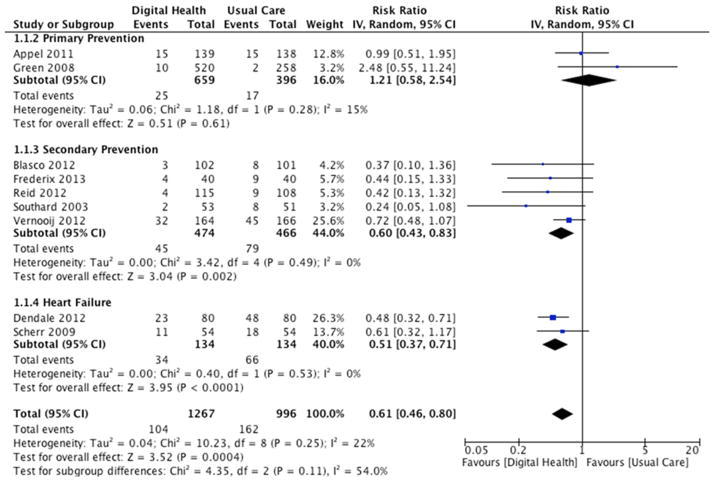
CVD outcomes including myocardial infarction, stroke, revascularization, hospitalizations, and all-cause mortality were abstracted from 9 RCTs (2 primary prevention studies, 2 involving patients with heart failure (HF), and 5 secondary prevention studies). The 1267 participants in the DHI arms had 104 events, and the 996 participants in the usual care arms had 162 combined events. Overall, DHI significantly reduced CVD outcomes (RR=0.61, (95% CI, 0.46–0.80); P<0.001; I2=22%; Figure 2). Subgroup analyses showed no interaction between the primary prevention (no prior CVD diagnosis), secondary prevention (known prior CVD diagnosis), and HF groups (P=.11). When the outcome “hospitalizations” was removed from the combined endpoint there remained a 52% reduction in CVD events/deaths that was not statistically significant (RR=0.48, (95% CI, 0.21–1.11); p=0.09). In addition, DHI was associated with a significant reduction in Framingham 10 year risk percentages in the 6 studies reporting FRS data (−1.24%; 95% CI −1.73%, −0.76%; P<0.001; I2=94%).
Figure 2.
CVD Outcomes and DHI.
The effect of DHI in Primary Prevention Studies
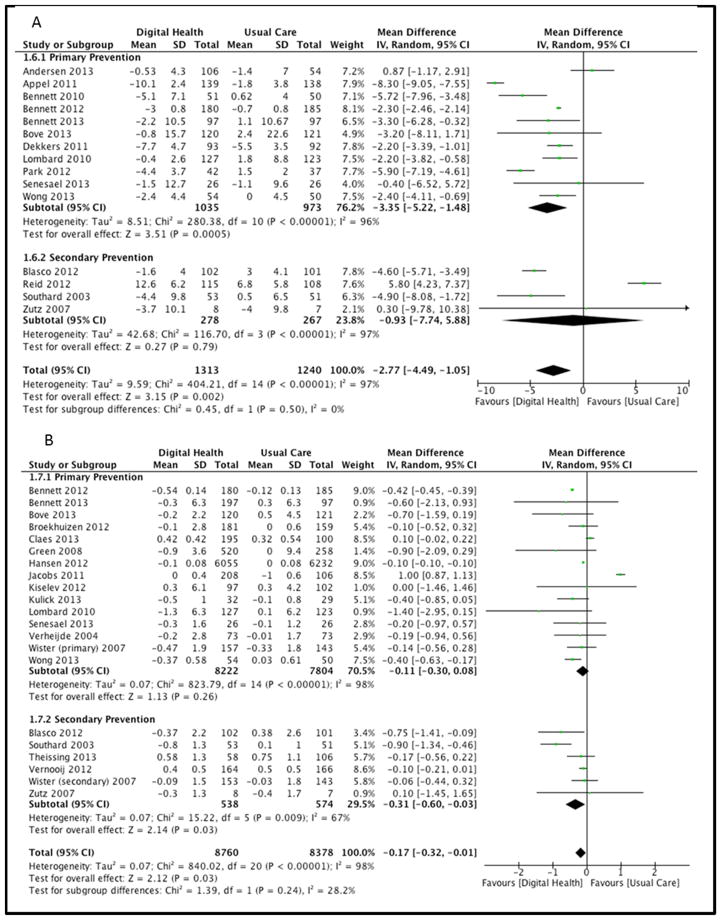
Separate subgroup analyses of primary prevention studies (n=2) were unable to provide statistical evidence of a positive effect on CVD outcomes (RR=1.21, (95% CI, 0.58–2.54); P=.61; I2=15%; Figure 2). Eleven primary prevention studies showed a significant reduction in weight (−3.35 lbs (95%CI −5.22 lbs, −1.48 lbs), P<0.001, I2=96%; Figure 3a), but not BMI (n=15) (mean difference = −0.11 kg/m2, (95% CI, −0.30 kg/m2, 0.08 kg/m2); P=.26; I2=98%; Figure 3b). When the three workplace intervention studies were removed from the pooled analysis, there was a significant reduction in BMI in primary prevention populations (n=12), (mean difference = −0.29 kg/m2, (95% CI, −0.5 kg/m2, −0.09 kg/m2); P=.006; I2=98%). We found a significant reduction in systolic blood pressure (SBP) among primary prevention studies (n=23), (mean difference = −2.12 mmHg, (95% CI, −4.15 mmHg, −0.09 mmHg); P=.04; I2=100%; Supplementary Figure 3) which failed to maintain a statistically significant reduction when two observational studies were removed in sensitivity analysis (mean difference = −1.31 mmHg, (95% CI, −3.43 mmHg, 0.80 mmHg); P=.22; I2=100%).
Figure 3.
Figure 3a: Weight and DHI.
Figure 3b: BMI and DHI.
There was insufficient evidence to show a positive impact on triglyceride levels (n=7) (mean difference = −9.06 mg/dL, (95% CI, −22.7 mg/dL, 4.6 mg/dL); P=.19; I2=99%); however, we found significant reductions in total cholesterol (n=13) (mean difference = −5.39 mg/dL, (95% CI, −9.80 mg/dL, −0.99 mg/dL); P=.02; I2=98%; Supplementary Figure 4a), LDL cholesterol (n=8) (mean difference = −4.96 mg/dL, (95% CI, −8.54 mg/dL, −1.38 mg/dL); P=.007; I2=95%; Supplementary Figure 4b), and glucose (n=6) (mean difference = −1.38 mg/dL, (95% CI, −2.13 mg/dL, −0.63 mg/dL); P<0.001; I2=81%) in primary prevention populations.
The effect of DHI in Secondary Prevention Studies
Subgroup analyses of secondary prevention studies showed significant impact of DHI on CVD outcomes (RR=0.60, (95% CI, 0.43–0.83); P=.002; I2=0%; Figure 2). Pooled data from four secondary prevention trials demonstrated no improvement in weight (−0.93 lbs (95%CI −7.74 lbs, 5.88 lbs), P=.79, I2=97%; Figure 3a), but did show significant reductions in BMI (n=6) (mean difference = −0.31 kg/m2, (95% CI, −0.60 kg/m2, −0.03 kg/m2); P=.03; I2=67%; Figure 3b). We found no improvement in SBP in secondary prevention DHI trials (mean difference = 1.98 mmHg, (95% CI, −1.05 mmHg, 5.01 mmHg); P=.20; I2=94%; Supplementary Figure 3).
Similarly, there was no positive impact on triglyceride levels (n=5) (mean difference = −17.19 mg/dL, (95% CI, −49.45 mg/dL, 15.07 mg/dL); P=.30; I2=99%), total cholesterol (n=6) (mean difference = −1.80 mg/dL, (95% CI, −6.23 mg/dL, 2.64 mg/dL); P=.43; I2=94%; Supplementary Figure 4a), LDL cholesterol (n=5) (mean difference = −10.43 mg/dL, (95% CI, −21.69 mg/dL, 0.83 mg/dL); P=.07; I2=100%; Supplementary Figure 4b), or glucose (n=4) (mean difference = 0.45 mg/dL, (95% CI, −9.68 mg/dL, 10.58 mg/dL); P=.93; I2=100%) in secondary prevention populations.
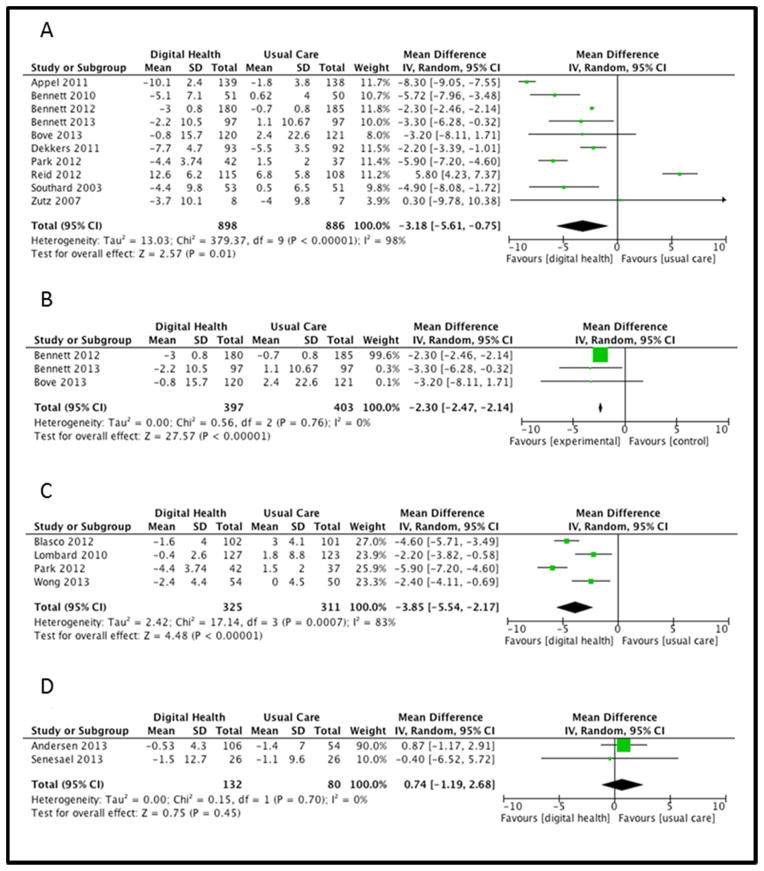
The impact of various DHI modalities on risk factors for CVD
When we evaluated individual DHI modalities and their effects on risk factors for CVD, we found significant reductions in weight in studies which incorporated three modalities including web-based (−3.18 lbs (95%CI −5.61 lbs, −0.75 lbs), P=.01; I2=98%; Figure 4A), telemedicine (−2.30 lbs (95%CI −2.47 lbs, −2.14 lbs), P<0.001; I2=0%; Figure 4B), and SMS text (−3.85 lbs (95%CI −5.54 lbs, −2.17 lbs), P<0.001; I2=83%; Figure 4C) with email interventions showing no significant reduction in weight (0.74 lbs (95%CI −1.19 lbs, 2.68 lbs), P=.45; I2=0%; Figure 4D). Web-based modalities also had a beneficial impact on SBP (−2.63 mmHg, 95% CI −5.04 mmHg, −0.23 mmHg; p=0.03 I2=100%). Studies that incorporated data monitoring (n=5) reported no weight outcomes, and showed a significant benefit only in reducing diastolic blood pressure (−3.08 mmHg, 95% CI −4.8 mmHg, −1.36 mmHg; P<0.001; I2=0%).
Figure 4.
Figure 4a: Web-based DHI and weight loss:
Figure 4b: Telehealth-based DHI and weight loss:
Figure 4c: SMS Text-based DHI and weight loss:
Figure 4d: Email-based DHI and weight loss:
Discussion
This systematic review and meta-analysis demonstrates that digital health has a beneficial effect on CVD risk factors and outcomes. Applying an inclusive definition of DHI broadly applied to studies ranging from two to 36 months, we found a CVD morbidity and all-cause mortality benefit for secondary CVD prevention and heart failure groups, with primary prevention populations showing benefit with regard to weight loss, BMI, SBP, total cholesterol, and LDL cholesterol. However, there was no clear benefit of DHI in primary prevention populations for CVD outcomes, although a reduction in Framingham risk scores was seen in our pooled analyses. In subgroup analysis by DHI subtype, there was particular benefit seen for web-based, telemedicine, and SMS texting DHI approaches, with insufficient data to support a benefit for email DHI.
As noted previously, prior literature on DHI and CVD-related outcomes has been limited. A recent systematic review of PubMed for mobile health and secondary CVD prevention over the prior ten years identified three studies without any quantitative results 22. Other systematic reviews have shown the efficacy of DHI on certain specific risk factors for CVD. Whittaker et al 7 showed improvements in smoking cessation across a wide variety of studies. Furthermore, additional work has shown DHI to positively affect behavior patterns 8 and physical activity 9. Liang et al 10 showed reductions of nearly 0.5% in HbA1c in 22 studies evaluating mobile phone program or text messaging tactics on participants with diabetes. Uhlig et al showed a favorable change in blood pressure at six months in 26 separate studies 11, yet they noted a lack of improvement in blood pressure at 12 months. A separate meta-analysis of 36 weight loss studies found that 71% of the studies reported some form of weight loss, although participant and intervention heterogeneity precluded a summary estimate of weight loss achieved through DHI 12.
In this systematic review and meta-analysis, we note a nearly 40% relative risk reduction in CVD outcomes with DHI, with particular impact on secondary CVD prevention and in patients with heart failure. This level of risk reduction surpasses other prevalent, guideline-based preventative measures such as statins 23, aspirin 24, or blood pressure reduction with beta-blockade 25. Furthermore, the absolute risk reduction in events was 6.5% in our pooled analysis and 7.5% in secondary prevention populations. This translates into a number needed to treat of 14 and 16 patients, respectively, also surpassing reported absolute benefits of other guideline-based measures. As DHI use does not directly reduce CVD risk, these observed benefits likely reflect increased adherence to evidence-based preventative therapies such as statins, aspirin, or beta-blockers.
We found significant improvements in the risk factors of weight loss, BMI, blood pressure, and LDL-cholesterol in patients seeking primary prevention of CVD. These improvements in risk factors did not translate into an improvement in CVD outcomes in primary prevention studies, at least partly owing to lower risk populations and lack of long-term follow up. Conversely, we found significant reductions in these events in secondary prevention studies despite a lack of consistent reductions in CVD risk factors in secondary prevention studies. This heterogeneity in results is not readily explained by existing studies, and should prompt future DHI research focusing on furthering our understanding of the variables determining success of specific DHI in specific populations.
Limitations
In an attempt to be inclusive in assessing the impact of DHI on CVD, we collected data utilizing multiple DHI modalities applied in multiple populations. Therefore, as noted previously heterogeneity in study results was present secondary to variation in study populations, DHI types, comparator groups, and lengths of follow up. Heterogeneity in these analyses was not explained by DHI modality or study design. Despite this heterogeneity, the data demonstrate an overall benefit of DHI for CVD prevention. However, the observed level of heterogeneity precludes definitive conclusions regarding specific DHIs that should be clinically applied to CVD prevention at the present time.
In addition, this analysis was unable to assess behavior change and motivational techniques, either of which could impact the outcomes of trials or be a contributor to DHI efficacy. Research attempting to better assess these issues will be vital in future work. Despite these limitations, the existing studies confirm that technological advances such as DHI can have a positive impact on preventative cardiovascular medicine.
Conclusion
The data synthesized and analyzed in this systematic review show a net benefit of DHI on overall CVD outcomes (CVD events, hospitalizations, and all-cause mortality) compared to usual care. These gains are largely driven by improvements in CVD outcomes among higher risk populations such as patients with HF or those targeting secondary CVD prevention. DHI were also associated with improvement in risk factors for CVD in primary studies, suggesting the potential for positive impact of DHI in a wide variety of participants and settings. Further research is needed to determine the most effective DHI modalities and to better understand the determinants of their success in specific cardiovascular risk populations.
Supplementary Material
Supplementary Table 1
A) Primary CVD Prevention (39):
B) Secondary CVD Prevention (13):
Supplementary Figure 1: Validity Assessment Tools:
Supplementary Figure 2: Funnel plot for CVD outcomes among primary and secondary prevention along with heart failure.
Supplementary Figure 3: Systolic Blood Pressure and DHI.
Supplementary Figure 4a: Total-Cholesterol and DHI.
Supplementary Figure 4b: LDL-Cholesterol and DHI.
Acknowledgments
Funding for this project was provided by National Institute of Health (NIH Grants HL-92954 and AG-31750 and the Mayo Foundation
This work was supported by funding from the BIRD foundation as well as the National Institute of Health (NIH Grants HL-92954 and AG-31750) and the Mayo Foundation. There was no direct role of the funding agencies in this study or manuscript.
The authors would like to thank the CTSA program of Mayo Clinic including the faculty and staff of CTSC 5740 (Drs. Murad, and Montori as well as Ms. Welsh) for their guidance. We would also like to show great appreciation toward the 28 authors who returned contact in an effort to improve the validity of our data extraction and assessment.
Abbreviations
- ACS
Acute Coronary Syndrome
- BMI
Body Mass Index
- CVD
Cardiovascular Disease
- DHI
Digital Health Intervention
- FRS
Framingham Risk Score
- HF
Heart Failure
- RCT
Randomized Controlled Trial
- ROI
Return on Investment
Footnotes
All authors contributed to the work, and have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Roger V, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:188–197. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 2.Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y American Heart Association Statistics Committee and Stroke Statistics. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee, Circulation. Circulation. 2008;117:e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 3.Yusef S, Hawkins S, Ounpus S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effects of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case controlled study. Lancet. 2004;342:937– 952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 4.Go A, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:143–152. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 5.Pfuntner A, Wier LM, Steiner C. HCUP Statistical Brief #146. Agency for Healthcare Research and Quality; Rockville, MD: Jan, 2013. Costs for Hospital Stays in the United States, 2010. [PubMed] [Google Scholar]
- 6.Pagoto SaBGG. How behavioral science can advance digital health. Transl Behav Med. 2013;3:271–276. doi: 10.1007/s13142-013-0234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whittaker R, McRobbie H, Bullen C, Borland R, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2012:11. doi: 10.1002/14651858.CD006611.pub3. [DOI] [PubMed] [Google Scholar]
- 8.Webb T, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12:e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fanning J, Mullen SP, McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res. 2012;14:e161. doi: 10.2196/jmir.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liang X, Wang Q, Yang X, Cao J, Chen J, Mo X, Huang J, Wang L, Gu D. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med. 2011;28:455–463. doi: 10.1111/j.1464-5491.2010.03180.x. [DOI] [PubMed] [Google Scholar]
- 11.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-Measured Blood Pressure Monitoring in the Management of Hypertension: A Systematic Review and Meta-analysis. Ann Intern Med. 2013;159:185–194. doi: 10.7326/0003-4819-159-3-201308060-00008. [DOI] [PubMed] [Google Scholar]
- 12.Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28:320–329. doi: 10.1097/JCN.0b013e318250a3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gauntlet C, Aitken M. Patient Apps for Improved Healthcare: From Novelty to Mainstream. Parsippany, NJ: The IMS Institute; 2013. [Google Scholar]
- 14.Moher DLA, Tetzlaff J, Altman DG The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med. 2009:151. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 15.Higgins J, Altman D. Cochrane Handbook (Version 5) Sections relating to new risk-of-bias tool. 2007 Available from: http://www.cochrane-smg.org/
- 16.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2007 Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm.
- 17.Wister A, Loewen N, Kennedy-Symonds H, McGowan B, McCoy B, Singer J. One-year follow-up of a therapeutic lifestyle intervention targeting cardiovascular disease risk. CMAJ. 2007;177:859–865. doi: 10.1503/cmaj.061059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins J, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McManus R, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, Kaambwa B, Banting M, Bryan S, Little P, Williams B, Hobbs FD. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376:163–172. doi: 10.1016/S0140-6736(10)60964-6. [DOI] [PubMed] [Google Scholar]
- 20.Scherr D, Kastner P, Kollmann A, Hallas A, Auer J, Krappinger H, Schuchlenz H, Stark G, Grander W, Jakl G, Schreier G, Fruhwald FM Mobitel Investigators. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. Journal of Medical Internet Research. 2009;11:e34. doi: 10.2196/jmir.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheridan S, Draeger LB, Pignone MP, Keyserling TC, Simpson RJ, Rimer B, Bangdiwala SI, Cai JW, Gizlice Z. A randomized trial of an intervention to improve use and adherence to effective coronary heart disease prevention strategies. BMC Health Services Research. 2011;11:331. doi: 10.1186/1472-6963-11-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beatty A, Fukuoka Y, Whooley MA. Using mobile technology for cardiac rehabilitation: a review and framework for development and evaluation. J Am Heart Assoc. 2013;2:e000568. doi: 10.1161/JAHA.113.000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor F, Ward K, Moore HMT, Burke M, Smith Davey, George Casas JP, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Heart Group Cochrane Database of Systematic Reviews; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A Antithrombotic Trialists’ (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–1860. doi: 10.1016/S0140-6736(09)60503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Law M, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Appel L, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, Miller ER, III, Dalcin A, Jerome GJ, Geller S, Noronha G, Pozefsky T, Charleston J, Reynolds JB, Durkin N, Rubin RR, Louis TA, Brancati FL. Comparative effectiveness of weight-loss interventions in clinical practice. New England Journal of Medicine. 2011;365:1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blasco A, Carmona M, Fernandez-Lozano I, Salvador CH, Pascual M, Sagredo PG, Somolinos R, Munoz A, Garcia-Lopez F, Escudier JM, Mingo S, Toquero J, Monivas V, Gonzalez MA, Fragua JA, Lopez-Rodriguez F, Monteagudo JL, Alonso-Pulpon L. Evaluation of a telemedicine service for the secondary prevention of coronary artery disease. Journal of Cardiopulmonary Rehabilitation & Prevention. 2012;32:25–31. doi: 10.1097/HCR.0b013e3182343aa7. [DOI] [PubMed] [Google Scholar]
- 28.Dendale P, De Keulenaer G, Troisfontaines P, Weytjens C, Mullens W, Elegeert I, Ector B, Houbrechts M, Willekens K, Hansen D. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. European Journal of Heart Failure. 2012;14:333–340. doi: 10.1093/eurjhf/hfr144. [DOI] [PubMed] [Google Scholar]
- 29.Frederix I, Driessche NV, Hansen D, Berger J, Bonne K, Alders T, Dendale P. Increasing the medium-term clinical benefits of hospital-based cardiac rehabilitation by physical activity telemonitoring in coronary artery disease patients. Eur J Prev Cardiol. 2013 doi: 10.1177/2047487313514018. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 30.Green BB, Anderson ML, Cook AJ, et al. A trial of web-based dietitian care for hypertension control: Weight loss effects on blood pressure. Journal of Clinical Hypertension. 2012:14. [Google Scholar]
- 31.Reid R, Morrin LI, Beaton LJ, Papadakis S, Kocourek J, McDonnell L, Slovinec D’Angelo ME, Tulloch H, Suskin N, Unsworth K, Blanchard C, Pipe AL. Randomized trial of an internet-based computer-tailored expert system for physical activity in patients with heart disease. European Journal of Preventive Cardiology. 2012;19:1357–1364. doi: 10.1177/1741826711422988. [DOI] [PubMed] [Google Scholar]
- 32.Southard B, Southard DR, Nuckolls J. Clinical trial of an Internet-based case management system for secondary prevention of heart disease. Journal of Cardiopulmonary Rehabilitation. 2003;23:341–348. doi: 10.1097/00008483-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Vernooij J, Kaasjager HA, van der Graaf Y, Wierdsma J, Grandjean HM, Hovens MM, de Wit GA, Visseren FL SMARTStudy Group. Internet based vascular risk factor management for patients with clinically manifest vascular disease: randomised controlled trial. BMJ. 2012;344:e3750. doi: 10.1136/bmj.e3750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andersen L, Sundstrup E, Boysen M, Jakobsen MD, Mortensen OS, Persson R. Cardiovascular Health Effects of Internet-Based Encouragements to Do Daily Workplace Stair-Walks: Randomized Controlled Trial. Journal of Medical Internet Research. 2013;15:e127. doi: 10.2196/jmir.2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bennett G, Herring SJ, Puleo E, Stein EK, Emmons KM, Gillman MW. Web-based weight loss in primary care: a randomized controlled trial. Obesity. 2010;18:308–313. doi: 10.1038/oby.2009.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bennett G, Warner ET, Glasgow RE, Askew S, Goldman J, Ritzwoller DP, Emmons KM, Rosner BA, Colditz GA Be Fit, Be Well Study Investigators. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med. 2012;172:565–574. doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bennett G, Foley P, Levine E, Whiteley J, Askew S, Steinberg DM, Batch B, Greaney ML, Miranda H, Wroth TH, Holder MG, Emmons KM, Puleo E. Behavioral treatment for weight gain prevention among black women in primary care practice: a randomized clinical trial. JAMA Intern Med. 2013;173:1770–1777. doi: 10.1001/jamainternmed.2013.9263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bove A, Homko CJ, Santamore WP, Kashem M, Kerper M, Elliott DJ. Managing hypertension in urban underserved subjects using telemedicine--a clinical trial. American Heart Journal. 2013;165:615–621. doi: 10.1016/j.ahj.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 39.Broekhuizen K, van Poppel MN, Koppes LL, Kindt I, Brug J, van Mechelen W. No significant improvement of cardiovascular disease risk indicators by a lifestyle intervention in people with familial hypercholesterolemia compared to usual care: results of a randomised controlled trial. BMC Research Notes. 2012;5:181. doi: 10.1186/1756-0500-5-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Claes N, Jacobs N, Clays E, Schrooten W, De Bourdeaudhuij I. Comparing the effectiveness of two cardiovascular prevention programmes for highly educated professionals in general practice: a randomised clinical trial. BMC Cardiovasc Disord. 2013:13. doi: 10.1186/1471-2261-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Colkesen E, Ferket BS, Tijssen JG, Kraaijenhagen RA, van Kalken CK, Peters RJ. Effects on cardiovascular disease risk of a web-based health risk assessment with tailored health advice: a follow-up study. Vascular Health & Risk Management. 2011;7:67–74. doi: 10.2147/VHRM.S16340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dekkers J, van Wier MF, Ariens GA, Hendriksen IJ, Pronk NP, Smid T, van Mechelen W. Comparative effectiveness of lifestyle interventions on cardiovascular risk factors among a Dutch overweight working population: a randomized controlled trial. BMC Public Health. 2011;11:49. doi: 10.1186/1471-2458-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frisch S, Zittermann A, Berthold HK, Gotting C, Kuhn J, Kleesiek K, Stehle P, Kortke H. A randomized controlled trial on the efficacy of carbohydrate-reduced or fat-reduced diets in patients attending a telemedically guided weight loss program. Cardiovascular Diabetology. 2009;8:36. doi: 10.1186/1475-2840-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goessens BM, Visseren FL, de Nooijer J, et al. A pilot-study to identify the feasibility of an Internet-based coaching programme for changing the vascular risk profile of high-risk patients. Patient Education & Counseling. 2008;73:67–72. doi: 10.1016/j.pec.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 45.Hansen A, Gronbaek M, Helge JW, Severin M, Curtis T, Tolstrup JS. Effect of a Web-Based Intervention to Promote Physical Activity and Improve Health Among Physically Inactive Adults: A Population-Based Randomized Controlled Trial. Journal of Medical Internet Research. 2012;14:e145. doi: 10.2196/jmir.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jacobs N, De Bourdeaudhuij I, Thijs H, Dendale P, Claes N. Effect of a cardiovascular prevention program on health behavior and BMI in highly educated adults: a randomized controlled trial. Patient Education & Counseling. 2011;85:122–126. doi: 10.1016/j.pec.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 47.Joo N, Kim BT. Mobile phone short message service messaging for behaviour modification in a community-based weight control programme in Korea. Journal of Telemedicine and Telecare. 2007;13:416–420. doi: 10.1258/135763307783064331. [DOI] [PubMed] [Google Scholar]
- 48.Kim C, Kang S. Development and a pilot test of an internet-based cardiovascular risk reduction program for Korean male workers with metabolic syndrome. CIN: Computers, Informatics, Nursing. 2013;31:157–166. doi: 10.1097/NXN.0b013e3182812829. [DOI] [PubMed] [Google Scholar]
- 49.Kiselev A, Gridnev VI, Shvartz VA, Posnenkova OM, Dovgalevsky PY. Active ambulatory care management supported by short message services and mobile phone technology in patients with arterial hypertension. Journal of the American Society of Hypertension. 2012;6:346–355. doi: 10.1016/j.jash.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 50.Kulick D, Langer RD, Ashley JM, Gans KM, Schlauch K, Feller C. Live well: a practical and effective low-intensity dietary counseling intervention for use in primary care patients with dyslipidemia - a randomized controlled pilot trial. BMC Family Practice. 2013;14:59. doi: 10.1186/1471-2296-14-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lieber S, Redberg RF, Blumenthal RS, Gandhi A, Robb KJ, Mora S. A national interactive web-based physical activity intervention in women, evaluation of the american heart association choose to move program 2006–2007. American Journal of Cardiology. 2012;109:1754–1760. doi: 10.1016/j.amjcard.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 52.Logan A, Irvine MJ, McIsaac WJ, Tisler A, Rossos PG, Easty A, Feig DS, Cafazzo JA. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension. 2012;60:51–57. doi: 10.1161/HYPERTENSIONAHA.111.188409. [DOI] [PubMed] [Google Scholar]
- 53.Lombard C, Deeks A, Jolley D, Ball K, Teede H. A low intensity, community based lifestyle programme to prevent weight gain in women with young children: cluster randomised controlled trial. British Medical Journal. 2010;341:c3215. doi: 10.1136/bmj.c3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marquez Contreras E, De La Figuera Von Wichmann M, Gil Guillen V, Ylla-Catala A, Figueras M, Balana M, Naval J. Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phones (HTA-ALERT). [Spanish] Eficacia de una intervencion informativa a hipertensos mediante mensajes de alerta en el telefono movil (HTA-ALERT) Atencion Primaria. 2004;34:399–405. doi: 10.1016/S0212-6567(04)78922-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McTigue K, Conroy MB, Hess R, Bryce CL, Fiorillo AB, Fischer GS, Milas NC, Simkin-Silverman LR. Using the internet to translate an evidence-based lifestyle intervention into practice. Telemedicine and e-Health. 2009;15:851–858. doi: 10.1089/tmj.2009.0036. [DOI] [PubMed] [Google Scholar]
- 56.Nolan R, Upshur RE, Lynn H, Crichton T, Rukholm E, Stewart DE, Alter DA, Chessex C, Harvey PJ, Grace SL, Picard L, Michel I, Angus J, Corace K, Barry-Bianchi SM, Chen MH. Therapeutic benefit of preventive telehealth counseling in the Community Outreach Heart Health and Risk Reduction Trial. Am J Cardiol. 2011;107:690–696. doi: 10.1016/j.amjcard.2010.10.050. [DOI] [PubMed] [Google Scholar]
- 57.Nolan R, Liu S, Shoemaker JK, Hachinski V, Lynn H, Mikulis DJ, Wennberg RA, Moy Lum-Kwong M, Zbib A. Therapeutic benefit of internet-based lifestyle counselling for hypertension. Canadian Journal of Cardiology. 2012;28:390–396. doi: 10.1016/j.cjca.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 58.Park M, Kim HS. Evaluation of mobile phone and Internet intervention on waist circumference and blood pressure in post-menopausal women with abdominal obesity. International Journal of Medical Informatics. 2012;81:388–394. doi: 10.1016/j.ijmedinf.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 59.Rossi M, Nicolucci A, Pellegrini F, Bruttomesso D, Di Bartolo P, Marelli G, Dal Pos M, Galetta M, Horwitz D, Vespasiani G. Interactive Diary for Diabetes: A Useful and Easy-to-Use New Telemedicine System to Support the Decision-Making Process in Type 1 Diabetes. Diabetes Technology & Therapeutics. 2009;11:19–24. doi: 10.1089/dia.2008.0020. [DOI] [PubMed] [Google Scholar]
- 60.Rossi M, Perozzi C, Consorti C, Almonti T, Foglini P, Giostra N, Nanni P, Talevi S, Bartolomei D, Vespasiani G. An Interactive Diary for Diet Management (DAI): A New Telemedicine System Able to Promote Body Weight Reduction, Nutritional Education, and Consumption of Fresh Local Produce. Diabetes Technology & Therapeutics. 2010;12:641–647. doi: 10.1089/dia.2010.0025. [DOI] [PubMed] [Google Scholar]
- 61.Senesael E, Borgermans L, Van De Vijver E, Devroey D. Effectiveness of a quality improvement intervention targeting cardiovascular risk factors: are patients responsive to information and encouragement by mail or post? Vascular Health & Risk Management. 2013;9:13–20. doi: 10.2147/VHRM.S39919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stuckey M, Russell-Minda E, Read E, Munoz C, Shoemaker K, Kleinstiver P, Petrella R. Diabetes and Technology for Increased Activity (DaTA) study: results of a remote monitoring intervention for prevention of metabolic syndrome. Journal of diabetes science and technology. 2011;5:928–935. doi: 10.1177/193229681100500416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thiboutot J, Sciamanna CN, Falkner B, Kephart DK, Stuckey HL, Adelman AM, Curry WJ, Lehman EB. Effects of a Web-Based Patient Activation Intervention to Overcome Clinical Inertia on Blood Pressure Control: Cluster Randomized Controlled Trial. Journal of Medical Internet Research. 2013;15:20–39. doi: 10.2196/jmir.2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Verheijden M, Bakx JC, Akkermans R, van den Hoogen H, Godwin NM, Rosser W, van Staveren W, van Weel C. Web-based targeted nutrition counselling and social support for patients at increased cardiovascular risk in general practice: randomized controlled trial. J Med Internet Res. 2004;6:e44. doi: 10.2196/jmir.6.4.e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wakefield B, Holman JE, Ray A, Scherubel M, Adams MR, Hillis SL, Rosenthal GE. Effectiveness of home telehealth in comorbid diabetes and hypertension: a randomized, controlled trial. Telemed J E Health. 2011;17:254–261. doi: 10.1089/tmj.2010.0176. [DOI] [PubMed] [Google Scholar]
- 66.Widmer R, Allison TG, Keane B, Dallas A, Lerman LO, Lerman A. Using an online, personalized program reduces cardiovascular risk factor profiles in a motivated, adherent population of participants. Am Heart J. 2014:167. doi: 10.1016/j.ahj.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 67.Wong C, Fung CSC, Siu SC, Lo YYC, Wong KW, Fong DYT, Lam CLK. A short message service (SMS) intervention to prevent diabetes in Chinese professional drivers with pre-diabetes: A pilot single-blinded randomized controlled trial. Diabetes Research and Clinical Practice. 2013;102:158–166. doi: 10.1016/j.diabres.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 68.Korzeniowska-Kubacka I, Dobraszkiewicz-Wasilewska B, Bilińska M, Rydzewska E, Piotrowicz Two models of early cardiac rehabilitation in male patients after myocardial infarction with preserved left ventricular function: comparison of standard out-patient versus hybrid training programmes. Kardiol Pol. 2011;69:220–226. [PubMed] [Google Scholar]
- 69.Lee Y, Hur SH, Sohn J, Lee HM, Park NH, Cho YK, Park HS, Yoon HJ, Kim H, Nam CW, Kim YN, Kim KB. Impact of home-based exercise training with wireless monitoring on patients with acute coronary syndrome undergoing percutaneous coronary intervention. Journal of Korean Medical Science. 2013;28:564–568. doi: 10.3346/jkms.2013.28.4.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Maric B, Kaan A, Araki Y, Ignaszewski A, Lear SA. The use of the Internet to remotely monitor patients with heart failure. Telemedicine Journal & E-Health. 2010;16:26–33. doi: 10.1089/tmj.2009.0094. [DOI] [PubMed] [Google Scholar]
- 71.Theissing J, Deck R, Raspe H. Liveonline aftercare in patients with abdominal obesity in cardio-diabetological rehabilitation: findings of a randomized controlled study. Rehabilitation. 2013;52:153–154. doi: 10.1055/s-0033-1345190. [DOI] [PubMed] [Google Scholar]
- 72.Zutz A, Ignaszewski A, Bates J, Lear SA. Utilization of the internet to deliver cardiac rehabilitation at a distance: a pilot study. Telemedicine Journal & E-Health. 2007;13:323–330. doi: 10.1089/tmj.2006.0051. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1
A) Primary CVD Prevention (39):
B) Secondary CVD Prevention (13):
Supplementary Figure 1: Validity Assessment Tools:
Supplementary Figure 2: Funnel plot for CVD outcomes among primary and secondary prevention along with heart failure.
Supplementary Figure 3: Systolic Blood Pressure and DHI.
Supplementary Figure 4a: Total-Cholesterol and DHI.
Supplementary Figure 4b: LDL-Cholesterol and DHI.