Abstract
Objective
US Hispanics/Latinos have high prevalence of obesity and related comorbidities. We compared overall and central obesity measures in associations with cardiometabolic outcomes among US Hispanics/Latinos.
Methods
Multivariable regression assessed cross-sectional relationships of six obesity measures with cardiometabolic outcomes among 16,415 Hispanics/Latinos aged 18-74 years.
Results
BMI was moderately correlated with waist-to-hip ratio (WHR; women, r=0.37; men, r=0.58) and highly correlated with other obesity measures (r≥0.87) (P<0.0001). All measures of obesity were correlated with unfavorable levels of glycemic traits, blood pressure, and lipids, with similar r-estimates for each obesity measure (P<0.05). Multivariable-adjusted prevalence ratios (PRs) for diabetes (women, 6.7 [3.9, 11.5]; men, 3.9 [2.2, 6.9]), hypertension (women, 2.4 [1.9, 3.1]; men, 2.5 [1.9, 3.4]), and dyslipidemia (women, 2.1 [1.8, 2.4]; men, 2.2 [1.9, 2.6]) were highest for individuals characterized as overweight/obese (BMI≥25kg/m2) and abnormal WHR (women, ≥0.85; men, ≥0.90), compared to those with normal BMI and WHR (P<0.0001). Among normal-weight individuals, abnormal WHR was associated with increased cardiometabolic condition prevalence (P<0.05), particularly diabetes (women, PR=4.0 [2.2, 7.1]; men, PR=3.0 [1.6, 5.7]).
Conclusions
Obesity measures were associated with cardiometabolic risk factors to a similar degree in US Hispanics/Latinos. WHR is useful to identify individuals with normal BMI at increased cardiometabolic risk.
Keywords: Hispanics, cardiovascular risk, diabetes, epidemiology, central obesity
Introduction
Obesity has become a major public health problem in the US, where over 35% of adults are obese (1). In particular, US Hispanics/Latinos, who are the fastest growing and largest minority group in the US, are disproportionately affected by obesity and related chronic diseases (1, 2). Recent data from the baseline examination of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), a population-based cohort of US Hispanics/Latinos conducted between 2008 and 2011, estimated that 37% of men and 43% of women are obese (body mass index [BMI] ≥30 kg/m2) (3), with high prevalence of diabetes and metabolic syndrome as well (4, 5).
BMI has been the most widely used measure to describe overall obesity in epidemiological studies, but this index fails to distinguish body composition and to indicate body fat distribution. Alternatively, waist circumference (WC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR), which describe body fat distribution, have been used to measure central obesity. Although it has been demonstrated that each of these commonly used measures of obesity is associated with diabetes, hypertension, dyslipidemia and cardiovascular diseases (CVD) (6, 7, 8), controversy remains about the superiority of any one measure over others. Another approach to measuring body fat is bioelectrical impedance analysis, which is an efficient and safe method for field epidemiologic studies. (9, 10, 11) Accordingly, percent body fat (%BF) and fat mass index (FMI) have been also used as indices of obesity (11, 12, 13, 14).
Several studies have compared BMI, WC, and WHR in their associations with cardiometabolic outcomes in US Hispanics/Latinos and yielded various results (15, 16, 17, 18, 19). For example, Zhu et al.(16) reported that WC might be a better indicator of cardiometabolic risk than BMI in 3 racial/ethnic groups including Mexican Americans, while Ghandehari et al. (17) suggested that BMI might be a better marker of cardiometabolic risk than WC in US Hispanics. In addition, another study found that measures of overall and central obesity were similar in predicting diabetes in a multi-ethnic cohort that included Hispanics (18). These inconsistent findings might be due to relatively small sample size of US Hispanic/Latino participants. In addition, previous studies included mostly Mexican Americans and body fat-related measures (%BF, FMI) have not been well-studied in populations of US Hispanics/Latinos. Moreover, it remains unclear whether BMI and other obesity measures assessed in combination could provide additional information in the identification of Hispanics/Latinos at increased cardiometabolic risk. Because of high correlations between obesity measures, large studies are needed to cross-classify individuals by more than one obesity measure. Therefore,in the current study, we aimed to evaluate six obesity measures (BMI, WC, WHR, WHtR, %BF, and FMI) and their associations with major cardiometabolic diseases, including diabetes, hypertension, and dyslipidemia, as well as several cardiometabolic traits (glycemic traits, blood pressure, and blood lipids) among 9835 women and 6580 men of diverse Hispanic backgrounds from the HCHS/SOL. Furthermore, we also examined cardiometabolic diseases and related traits according to normal and abnormal categories of obesity measures.
Methods
Participants
The HCHS/SOL is a population-based cohort study of Hispanic/Latino adults aged 18-74 years living in 4 U.S. urban centers (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA). The goal of HCHS/SOL is to determine the role of acculturation in the prevalence and development of disease, and to identify disease risk factors of importance in Hispanic/Latino communities. Participants were recruited using a 2-stage area probability sampling design as described in detail previously (20, 21). Of 39,384 individuals who met eligibility criteria, 41.7% were enrolled, representing 16,415 persons from 9,872 households. Baseline interviews were conducted in English or Spanish at in-person clinic visits during 2008-2011. The study was approved by the Institutional Review Boards at each field center, and all participants gave written informed consent.
Obesity measures
Measurements of weight, %BF, and fat mass were obtained from the Tanita body composition analyzer (model TBF-300A; Tanita Corporation, Arlington Heights, IL). Height and waist and hip circumference were measured to the nearest centimeter based on a standard protocol (www.cscc.unc.edu/hchs). Body weight was measured to the nearest 0.1 kg. BMI was calculated as weight in kilograms divided by height in meters squared. FMI was calculated as fat mass in kilograms divided by height in meters squared. Participants with a BMI 18.5-25.0 kg/m2 were defined as having a normal weight (normal BMI) and those with a BMI≥25 kg/m2 were defined as being overweight/obese (abnormal BMI). WC, WHR and %BF were dichotomized based on standard cutoffs for women (high WC, ≥80 cm; high WHR, ≥0.85; high %BF, ≥30%) and men (high WC, ≥90 cm; high WHR, ≥0.90; high %BF, ≥25%) (14).
Cardiometabolic risk factors
After a 5-minute rest period, 3 seated blood pressure measurements were obtained with an automatic sphygmomanometer; the second and third readings were averaged. Blood samples (fasting and after a 2-hour oral glucose load) were collected and processed according to standardized protocols (www.cscc.unc.edu/hchs). Total serum cholesterol was measured using a cholesterol oxidase enzymatic method and high-density lipoprotein (HDL) cholesterol with a direct magnesium/dextran sulfate method. Plasma glucose was measured using a hexokinase enzymatic method (Roche Diagnostics). Low-density lipoprotein (LDL) cholesterol was calculated using the Friedewald equation (22). Hemoglobin A1c (HbA1c) was measured using a Tosoh G7 Automated HPLC Analyzer (Tosoh Bioscience). Fasting insulin was measured using two commercial immunoassays (ELISA, Mercodia AB, Uppsala, Sweden; and sandwich immunoassay on a Roche Elecsys 2010 Analyzer, Roche Diagnostics, Indianapolis, IN); early measures conducted with the Mercodia assay were calibrated, and values were equivalent to the Roche method. Homeostatic model assessment of insulin resistance (HOMA-IR) was computed the following equation: fasting glucose × fasting insulin / 405 (23).
Participants were instructed to bring all prescription and nonprescription medications taken in the past month. Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg, diastolic blood pressure (DBP) ≥90 mmHg, or antihypertensive medication use (24). Diabetes was defined according to the American Diabetes Association (ADA) as at least one of the following: fasting glucose ≥126 mg/dL, 2-hour-postload glucose ≥200 mg/dL, HbA1c ≥6.5%, or antidiabetic medication use (25). Dyslipidemia was defined as at least one of the following: LDL-cholesterol ≥160 mg/dL, HDL-cholesterol <50 mg/dL for women and <40 mg/dL for men, triglycerides ≥200 mg/dL, or taking lipid-lowering drugs (26).
Covariate assessment
Self-reported questionnaires were used to collect information on age, Hispanic/Latino background, place of birth/nativity (inside versus outside the US 50 states plus the District of Columbia), education level, health insurance status, medical history, annual household income, smoking status, alcohol consumption, and combined work, travel, and leisure physical activity. Total physical activity was assessed using the Global Physical Activity Questionnaire developed by the World Health Organization (http://www.who.int/chp/steps/GPAQ/en/index.html).
Statistical analysis
In accordance with procedures standard to large population-based studies (27), all reported values were non-response adjusted, trimmed, and calibrated by age, sex, and Hispanic/Latino background (national heritage) to the characteristics of each field center's target population from the 2010 Census. All analyses also account for cluster sampling and stratification in the sample selection. Although no HCHS/SOL participants were excluded from the entire analysis, several observations were excluded from variable-specific analyses due to incomplete data, or for the following reasons: plasma cardiometabolic markers treated as missing for those not fasting at least 8 hours (n=294); BMI, WHtR and FMI treated as missing for those not able to stand erect for height measurement (n=157); FMI and %BF treated as missing for those not meeting data quality control (n=188).
Correlations between obesity measures were assessed using weighted age-adjusted partial Pearson correlation coefficients. Weighted age-adjusted partial Pearson correlations were also computed between obesity measures and cardiometabolic markers among those not taking antidiabetic medications, antihypertensive medications, or lipid-lowering drugs (7060 women and 4961 men). Triglycerides, fasting insulin and HOMA-IR were natural logarithm-transformed before analysis. Means of cardiometabolic markers for the target population of Hispanics/Latinos in the 4 HCHS/SOL communities were calculated using survey linear regression weighted least square. To evaluate the associations of obesity measures with prevalent hypertension, diabetes, and dyslipidemia, prevalence ratios were derived from survey Poisson regression models with robust variance estimation. Besides taking into account the survey design and survey weights, these analyses were adjusted for age, Hispanic/Latino background, field center, nativity, education level, health insurance status, annual household income, smoking, alcohol consumption, and physical activity. In addition, agreement of normal and abnormal categories of obesity measures was assessed by the Cohen's kappa statistic. Analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC) and SUDAAN release 11.0.1 (RTI International, Research Triangle Park, NC).
Results
Participant characteristics
Sex-specific characteristics of the study population are shown in Table 1. The mean age was 41.8 years in women and 40.3 years in men. The largest group was of Mexican background (38% of women; 36% of men), followed by those of Cuban (18% of women; 22% of men) and Puerto Rican (15% of women; 17% of men) backgrounds. Greater than 75% of women and men were overweight, 22% of women and men had hypertension, 16% of women and 14% of men had diabetes, and 59% of women and 52% of men had dyslipidemia. Data on prevalence of overweight/obesity, hypertension, diabetes and dyslipidemia across study sites are shown in Table S1, and data on prevalence of these cardiometabolic outcomes have been previously published elsewhere (3, 4).
Table 1.
Weighted characteristics of Hispanic/Latino women and men from four U.S. urban centers, 2008-2011*
| Women | Men | |
|---|---|---|
| No. of participants | 9835 | 6580 |
| Age, mean year (SE) | 41.8 (0.3) | 40.3 (0.3) |
| Hispanic background, n (%) | ||
| Central American | 1049 (7%) | 683 (7%) |
| Cuban | 1250 (18%) | 1098 (22%) |
| Dominican | 963 (11%) | 510 (8%) |
| Mexican | 4022 (38%) | 2450 (36%) |
| Puerto Rican | 1589 (15%) | 1139 (17%) |
| South American | 635 (5%) | 437 (5%) |
| Others, more than one, or not reported | 327 (5%) | 263(4%) |
| Nativity (within 50 states), n (%) | 1604 (21%) | 1259 (25%) |
| Less than high school education, n (%) | 3768 (33%) | 2439 (32%) |
| Annual household income ($), n (%) | ||
| < 20,000 | 4622 (46%) | 2585 (38%) |
| 20,000-50,000 | 3426 (34%) | 2693 (40%) |
| >50,000 | 754 (9%) | 847 (15%) |
| Not reported | 1033 (11%) | 455 (8%) |
| Health insurance, n (%) | 5065 (52%) | 3107 (47%) |
| Current smoking, n (%) | 1486 (16%) | 1680 (27%) |
| Alcohol consumption, n (%) | ||
| Not current drinker | 6097 (59%) | 2503 (37%) |
| Low-risk drinker | 3420 (37%) | 3497 (54%) |
| At-risk drinker † | 279 (4%) | 549 (9%) |
| Physical activity, mean MET-min/day (SE) | 447 (13) | 1004 (27) |
| Hypertension, n (%) | 2691 (22%) | 1784 (22%) |
| Diabetes, n (%) | 1994 (16%) | 1224 (14%) |
| Dyslipidemia, n (%) | 5962 (59%) | 3630 (52%) |
| Obesity measures, median (IQR) | ||
| Body mass index, kg/m2 | 28.8 (25.2, 33.3) | 28.3 (25.3, 31.8) |
| Waist circumference, cm | 95 (86, 104) | 97 (88, 106) |
| Waist-to-hip ratio | 0.90 (0.84, 0.94) | 0.94 (0.90, 0.99) |
| Waist-to-height ratio | 0.61 (0.55, 0.67) | 0.57 (0.52, 0.62) |
| Fat mass index | 11.1 (8.3, 14.4) | 7.7 (5.7, 10.2) |
| Body fat percent, % | 39 (33, 44) | 27 (22, 32) |
| Cardiometabolic markers, median (IQR) | ||
| Systolic blood pressure, mmHg | 112 (103, 125) | 121 (113, 130) |
| Diastolic blood pressure, mmHg | 69 (63, 77) | 72 (65, 80) |
| LDL-cholesterol, mg/dl | 114 (93, 140) | 119 (95, 144) |
| HDL-cholesterol, mg/dl | 50 (42, 59) | 43 (37, 50) |
| Triglycerides, mg/dl | 101 (70, 147) | 117 (79, 178) |
| Fasting glucose, mg/dl | 92 (86, 99) | 96 (90, 103) |
| 2-h glucose, mg/dl | 113 (94, 138) | 105 (87, 130) |
| Fasting insulin, mU/L | 10.6 (6.9, 16.2) | 9.9 (6.0, 15.9) |
| HOMA-IR | 2.5 (1.6, 4.0) | 2.5 (1.5, 4.2) |
| Hemoglobin A1c, % | 5.4 (5.2, 5.8) | 5.4 (5.2, 5.7) |
Values (except No.) are weighted for study design and nonresponse and age standardized to Census 2010 US characteristics of the target population.
Women: ≥7 drinks/week; Men: ≥14 drinks/week. SE, standard error; MET, metabolic equivalent; IQR, interquartile range.
Correlations of obesity measures with cardiometabolic markers
As shown in Table 2, there were high correlations among all obesity measures (except WHR) in women (r≥0.78) and men (r≥0.84). WHR showed moderate correlations with BMI (r=0.34 in women; r=0.58 in men), %BF (r=0.34 in women; r=0.56 in men) and FMI (r=0.35 in women; r=0.58 in men). All correlations among obesity measures were statistically significant (P < 0.0001).
Table 2. Age-adjusted partial Pearson correlation coefficients between obesity measures and cardiometabolic markers in Hispanic/Latino women and men*.
| Women | Men | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| BMI | WC | WHR | WHtR | %BF | FMI | BMI | WC | WHR | WHtR | %BF | FMI | |
| Obesity measures | ||||||||||||
| WC | 0.87 | - | - | - | - | - | 0.91 | - | - | - | - | - |
| WHR | 0.34 | 0.61 | - | - | - | - | 0.58 | 0.72 | - | - | - | - |
| WHtR | 0.87 | 0.96 | 0.62 | - | - | - | 0.92 | 0.95 | 0.74 | - | - | - |
| %BF | 0.90 | 0.84 | 0.34 | 0.78 | - | - | 0.88 | 0.84 | 0.56 | 0.85 | - | - |
| FMI | 0.94 | 0.85 | 0.35 | 0.82 | 0.98 | - | 0.94 | 0.88 | 0.58 | 0.89 | 0.96 | - |
| Cardiometabolic makers | ||||||||||||
| Systolic blood pressure | 0.09 | 0.08 | 0.06 | 0.08 | 0.09 | 0.09 | 0.13 | 0.12 | 0.10 | 0.12 | 0.14 | 0.13 |
| Diastolic blood pressure | 0.32 | 0.27 | 0.10 | 0.26 | 0.32 | 0.33 | 0.35 | 0.34 | 0.26 | 0.34 | 0.35 | 0.35 |
| LDL-cholesterol | 0.09 | 0.07 | 0.06 | 0.09 | 0.11 | 0.09 | 0.15 | 0.16 | 0.15 | 0.17 | 0.21 | 0.16 |
| HDL-cholesterol | -0.29 | -0.31 | -0.27 | -0.31 | -0.28 | -0.29 | -0.30 | -0.29 | -0.25 | -0.28 | -0.29 | -0.27 |
| Triglycerides | 0.26 | 0.29 | 0.29 | 0.30 | 0.28 | 0.26 | 0.31 | 0.31 | 0.31 | 0.33 | 0.33 | 0.30 |
| Fasting glucose | 0.11 | 0.14 | 0.16 | 0.15 | 0.08 | 0.10 | 0.10 | 0.11 | 0.14 | 0.11 | 0.10 | 0.10 |
| 2-h glucose | 0.20 | 0.18 | 0.17 | 0.22 | 0.16 | 0.18 | 0.21 | 0.21 | 0.20 | 0.25 | 0.23 | 0.23 |
| Fasting insulin | 0.54 | 0.52 | 0.33 | 0.51 | 0.54 | 0.55 | 0.59 | 0.61 | 0.47 | 0.60 | 0.59 | 0.59 |
| HOMA-IR | 0.53 | 0.52 | 0.34 | 0.51 | 0.52 | 0.53 | 0.58 | 0.60 | 0.48 | 0.59 | 0.59 | 0.58 |
| Hemoglobin A1c | 0.17 | 0.18 | 0.19 | 0.20 | 0.12 | 0.15 | 0.12 | 0.13 | 0.16 | 0.13 | 0.11 | 0.12 |
Values are weighted to the target population and adjusted for age; participants receiving medications for hypertension, diabetes, or dyslipidemia were excluded from the analysis for all cardiometabolic markers; all correlations statistically significant P<0.002.
BMI, body mass index; WC, waist circumference; WHR, waist-to-hip ratio; WHtR, waist-to-height ratio; %BF, percent body fat; FMI, fat mass index.
All obesity measures were positively correlated with systolic blood pressure, diastolic blood pressure, LDL-cholesterol, triglycerides, fasting glucose, 2-hour glucose, fasting insulin, HOMA-IR and HbA1c, and inversely correlated with HDL-cholesterol (Table 2; all P < 0.002). The correlation coefficients of different obesity measures with each cardiometabolic marker were generally similar, except for WHR which showed slightly weaker correlations with fasting insulin and HOMA-IR compared with other obesity measures.
Associations of obesity measures with diabetes, hypertension and dyslipidemia
All obesity measures were positively associated with prevalence of diabetes (PR=1.41 to 1.54 in women and PR=1.37 to 1.53 in men per SD increment), hypertension (PR=1.17 to 1.31 in women and PR=1.29 to 1.36 in men per SD increment) and dyslipidemia (PR=1.17 to 1.20 in women and PR=1.21 to 1.26 in men per SD increment) in both women and men, after adjustment for age, demographic and socioeconomic variables, and lifestyle factors (Table 3; all P < 0.0001). The PRs for each cardiometabolic condition with 1 SD increment in most obesity measures were similar in both women and men.
Table 3. Prevalence ratios (95% confidence intervals) for hypertension, diabetes and dyslipidemia with one standard deviation increase in obesity measures in Hispanic/Latino women and men*.
| Diabetes | Hypertension | Dyslipidemia | |
|---|---|---|---|
| Women | |||
| BMI | 1.43 (1.36, 1.51) | 1.31 (1.26, 1.36) | 1.17 (1.14, 1.20) |
| WC | 1.47 (1.40, 1.55) | 1.29 (1.24, 1.34) | 1.19 (1.16, 1.22) |
| WHR | 1.54 (1.46, 1.62) | 1.17 (1.12, 1.23) | 1.19 (1.16, 1.23) |
| WHtR | 1.49 (1.41, 1.57) | 1.29 (1.24, 1.34) | 1.20 (1.17, 1.22) |
| %BF | 1.46 (1.35, 1.59) | 1.30 (1.23, 1.38) | 1.20 (1.16, 1.24) |
| FMI | 1.41 (1.33, 1.49) | 1.30 (1.25, 1.35) | 1.17 (1.15, 1.20) |
| Men | |||
| BMI | 1.44 (1.36, 1.53) | 1.36 (1.30, 1.42) | 1.22 (1.19, 1.26) |
| WC | 1.48 (1.39, 1.57) | 1.34 (1.28, 1.41) | 1.24 (1.20, 1.27) |
| WHR | 1.53 (1.42, 1.66) | 1.29 (1.22, 1.37) | 1.26 (1.22, 1.30) |
| WHtR | 1.49 (1.40, 1.59) | 1.35 (1.29, 1.42) | 1.24 (1.20, 1.27) |
| %BF | 1.37 (1.28, 1.48) | 1.36 (1.29, 1.44) | 1.25 (1.21, 1.29) |
| FMI | 1.38 (1.30, 1.47) | 1.34 (1.29, 1.40) | 1.21 (1.17, 1.24) |
Adjusted for age, sampling scheme of the Hispanic Community Health Study /Study of Latinos (HCHS/SOL), Hispanic background, field center, nativity, education level, health insurance status, annually household income, smoking, alcohol consumption, and physical activity.
BMI, body mass index; SD, standard deviation; WC, waist circumference; WHR, waist-to-hip ratio; WHtR, waist-to-height ratio; %BF, percent body fat; FMI, fat mass index.
In addition, associations between obesity measures and cardiometabolic diseases were, in general, consistent across Hispanic/Latino background groups (Table S2 and Table S3). Effect estimates were qualitatively similar for all associations of interest, with a few nominally statistically significant tests for interaction (P for interaction < 0.05). Possible heterogeneity in associations was only observed for WHR and dyslipidemia, and WHtR and Hypertension in men, with a P for interaction < 0.01.
Agreement of normal and abnormal categories of obesity measures
Table 4 shows the agreement of normal and abnormal categories of BMI, WC, WHR and %BF in women and men. Among overweight/obese women defined by BMI criteria, 99% were classified as abnormal by WC criteria, 80% were classified as abnormal by WHR criteria, and 98% were classified as abnormal by %BF criteria. However, among normal weight women defined by BMI criteria, 60% were classified as abnormal by WC criteria, 50% were classified as abnormal by WHR criteria, and 41% were classified as abnormal by %BF criteria. Among overweight/obese men defined by BMI criteria, 78% were classified as abnormal by WC criteria, 84% were classified as abnormal by WHR criteria, and 79% were classified as abnormal by %BF criteria. Among normal weight men defined by BMI criteria, a small proportion of individuals were classified as abnormal by WC criteria (7%) or %BF criteria (6%), but 40% were classified as abnormal by WHR criteria. Cohen's kappa statistic indicates that WC criteria (K=0.48 in women and 0.57 in men) and %BF criteria (K=0.65 in women and 0.59 in men) had moderate agreement with BMI criteria, and WHR criteria had fair-to-moderate agreement with BMI criteria (K=0.28 in women and 0.41 in men).
Table 4. Overlap among participants classified as normal or abnormal by BMI, WC, WHR and %BF*.
| Normal WC | Abnormal WC | Normal WHR | Abnormal WHR | Normal %BF | Abnormal %BF | |
|---|---|---|---|---|---|---|
| Women | ||||||
| Normal weight | 630 (40) | 1229 (60) | 810 (50) | 1048 (50) | 947 (59) | 879 (41) |
| Overweight/obese | 76 (1) | 7690 (99) | 1373 (20) | 6391 (80) | 127 (2) | 7421 (98) |
| Cohen's kappa (95% CI) | 0.48 (0.45, 0.52) | 0.28 (0.24, 0.31) | 0.65 (0.62, 0.68) | |||
| Men | ||||||
| Normal weight | 1201 (93) | 110 (7) | 663 (60) | 648 (40) | 1178 (94) | 86 (6) |
| Overweight/obese | 1006 (22) | 4126 (78) | 627 (16) | 4501 (84) | 948 (21) | 4023 (79) |
| Cohen's kappa (95% CI) | 0.57 (0.54, 0.60) | 0.41 (0.38, 0.44) | 0.59 (0.56, 0.62) | |||
Values are n (%); all percentages in this table are weighted to account for the sampling scheme of the Hispanic Community Health Study /Study of Latinos (HCHS/SOL).
Normal weight: 18.5≤BMI<25 kg/m2; Overweight/obese: BMI≥25 kg/m2.
Normal WC: <94 cm in men/<80 cm in women; Abnormal WC: ≥94 cm in men/≥80 cm in women.
Normal WHR: <0.90 in men/<0.85 in women; Abnormal WHR: ≥0.9 in men/≥0.85 in women.
Normal %BF: <25% in men/<30% in women; Abnormal %BF: ≥25% in men/≥30% in women.
BMI, body mass index; WC, waist circumference; WHR, waist-to-hip ratio; %BF, percent body fat; CI, confidence interval.
Cardiometabolic risk according to normal and abnormal categories of obesity measures
After adjustment for age, demographic and socioeconomic variables, and lifestyle factors, PRs for diabetes, hypertension, and dyslipidemia differed across subgroups classified by BMI and other obesity measures (Table 5). The PRs for cardiometabolic diseases were the highest among those with both abnormal BMI and another obesity measure. In both women and men, the highest PRs (95% CI) for diabetes (6.70 [3.91, 11.48] in women; 3.91 [2.22, 6.88] in men), hypertension (2.40 [1.87, 3.07] in women; 2.52 [1.87, 3.40] in men), and dyslipidemia (2.10 [1.83, 2.41] in women; 2.22 [1.89, 2.61] in men) were observed among overweight/obese individuals with abnormal WHR. Notably, abnormal WHR was also significantly associated with increased PRs of all three cardiometabolic diseases in normal-weight women and men, with a remarkably high PR of diabetes (3.99 [2.23, 7.41] in women; 3.04 [1.63, 5.66] in men).
Table 5. Prevalence ratios (95% confidence intervals) for hypertension, diabetes and dyslipidemia by normal and abnormal categories of BMI and WC, WHR or %BF *.
| Normal WC | Abnormal WC | Normal WHR | Abnormal WHR | Normal %BF | Abnormal %BF | |
|---|---|---|---|---|---|---|
| Women | ||||||
| Diabetes | ||||||
| Normal weight | Ref | 2.74 (1.48, 5.06) | Ref | 3.99 (2.23, 7.14) | Ref | 2.00 (1.33, 3.01) |
| Overweight/obese | 2.70 (0.69, 10.66) | 4.73 (2.68, 8.37) | 3.59 (2.00, 6.45) | 6.70 (3.91, 11.48) | 2.49 (1.15, 5.41) | 3.27 (2.24, 4.77) |
| Hypertension | ||||||
| Normal weight | Ref | 1.28 (0.97, 1.69) | Ref | 1.40 (1.07, 1.82) | Ref | 1.31 (0.99, 1.74) |
| Overweight/obese | 0.89 (0.41, 1.91) | 2.22 (1.71, 2.87) | 1.96 (1.44, 2.66) | 2.40 (1.87, 3.07) | 2.07 (1.16, 3.67) | 2.16 (1.69, 2.77) |
| Dyslipidemia | ||||||
| Normal weight | Ref | 1.47 (1.23, 1.75) | Ref | 1.50 (1.29, 1.74) | Ref | 1.11 (0.94, 1.32) |
| Overweight/obese | 1.50 (1.06, 2.12) | 2.05 (1.74, 2.42) | 1.63 (1.40, 1.91) | 2.10 (1.83, 2.41) | 1.51 (1.19, 1.92) | 1.66 (1.45, 1.90) |
| Men | ||||||
| Diabetes | ||||||
| Normal weight | Ref | 1.36 (0.75, 2.47) | Ref | 3.04 (1.63, 5.66) | Ref | 1.39 (0.75, 2.59) |
| Overweight/obese | 0.96 (0.67, 1.38) | 1.85 (1.44, 2.37) | 1.61 (0.76, 3.43) | 3.91 (2.22, 6.88) | 1.35 (0.96, 1.89) | 1.71 (1.33, 2.19) |
| Hypertension | ||||||
| Normal weight | Ref | 1.42 (1.06, 1.89) | Ref | 1.76 (1.30, 2.38) | Ref | 2.30 (1.73, 3.06) |
| Overweight/obese | 1.13 (0.90, 1.41) | 1.85 (1.57, 2.18) | 1.38 (0.93, 2.03) | 2.52 (1.87, 3.40) | 1.42 (1.14, 1.77) | 2.03 (1.69, 2.44) |
| Dyslipidemia | ||||||
| Normal weight | Ref | 1.40 (1.08, 1.81) | Ref | 1.51 (1.24, 1.83) | Ref | 1.60 (1.24, 2.07) |
| Overweight/obese | 1.31 (1.14, 1.50) | 1.89 (1.67, 2.13) | 1.56 (1.29, 1.89) | 2.22 (1.89, 2.61) | 1.31 (1.14, 1.51) | 1.91 (1.69, 2.15) |
Adjusted for age, sampling scheme of the Hispanic Community Health Study /Study of Latinos (HCHS/SOL), Hispanic/Latino background, field center, nativity, education level, health insurance status, annual household income, smoking, alcohol consumption, and physical activity.
Normal weight: 18.5≤BMI<25 kg/m2; Overweight/obese: BMI≥25 kg/m2.
Normal WC: <94 cm in men/<80 cm in women; Abnormal WC: ≥94 cm in men/≥80 cm in women.
Normal WHR: <0.90 in men/<0.85 in women; Abnormal WHR: ≥0.90 in men/≥0.85 in women.
Normal %BF: <25% in men/<30% in women; Abnormal %BF: ≥25% in men/≥30% in women.
BMI, body mass index; WC, waist circumference; WHR, waist-to-hip ratio; %BF, percent body fat.
Consistently, individuals with both abnormal BMI and WHR had the most adverse cardiometabolic risk factor profile (Figure 1). Moreover, individuals with normal BMI and abnormal WHR had significantly higher levels of diastolic blood pressure (men only), LDL-cholesterol (men only), triglycerides, 2-hour glucose, and fasting insulin (all P < 0.05), and lower levels of HDL cholesterol (P< 0.01) compared with those with both normal BMI and WHR. Individuals with abnormal BMI and normal WHR had significantly more adverse levels of most of these cardiometabolic makers compared with those with both normal BMI and WHR.
Figure 1.
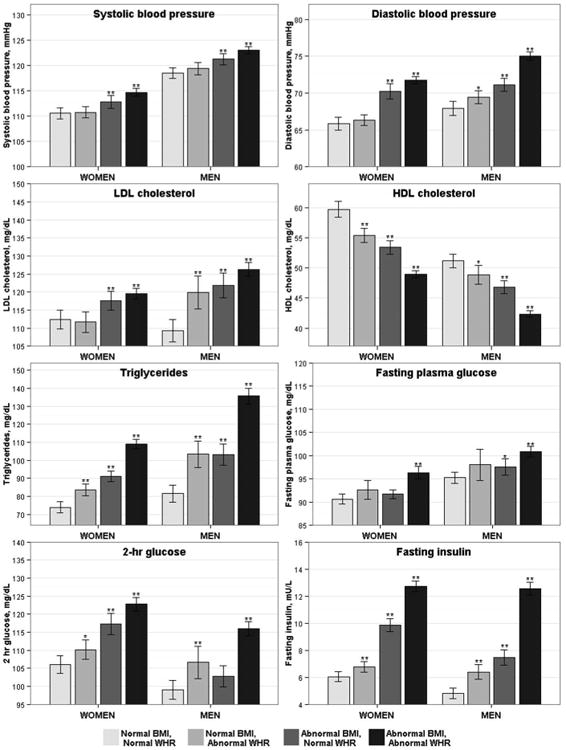
Mean (95% confidence interval) values of cardiometabolic biomarkers according to normal and abnormal categories of BMI and WHR.
Values are adjusted for age, sampling scheme of the Hispanic Community Health Study /Study of Latinos (HCHS/SOL), Hispanic background, field center, nativity, education level, health insurance status, annual household income, smoking, alcohol consumption, and physical activity. Participants receiving medications for hypertension, diabetes, or dyslipidemia were excluded from the analysis for all cardiometabolic markers. Significant differences in means between the groups: **P<0.01 and *P<0.05 for comparison with the normal BMI and normal WHR group. Normal BMI: 18.5≤BMI<25 kg/m2; Abnormal BMI: BMI≥25 kg/m2. Normal WHR: <0.90 in men/<0.85 in women; Abnormal WHR: ≥0.9 in men/≥0.85 in women. BMI, body mass index; WHR, waist-to-hip ratio.
Results according to normal and abnormal categories of BMI and WC or %BF are show Figures S1 and S2. Similarly, individuals with both abnormalities had the most adverse cardiometabolic risk factor profile (P < 0.0001), and those with one abnormality had a significantly more adverse cardiometabolic risk factor profile compared with those with both normal obesity measures (P < 0.05).
Discussion
In this population-based cohort of over 16,000 US Hispanic/Latino women and men, we found that different obesity measures, including BMI, WC, WHR, WHtR, %BF and FMI, were all significantly associated with higher prevalence of diabetes, hypertension and dyslipidemia, as well as unfavorable cardiometabolic markers. The magnitudes of associations of BMI with cardiometabolic risk factors were similar to those of central obesity measures (WC, WHR and WHtR) and direct measurements of body fat (%BF and FMI), with none of the obesity measures showing a particularly stronger association. However, the agreement of normal and abnormal categories of BMI and other obesity measures were moderate, and individuals with abnormalities of both BMI and another obesity measure had particularly high cardiometabolic risk.
In the present study of US Hispanics/Latinos, the obesity measure that was most strongly associated with different cardiometabolic risk factors varied across risk factors, and in instances where one obesity measure may have been superior to others the differences were small. Our data are, in general, consistent with previous results in Hispanic populations(15, 16, 17, 18, 19) as well as in diverse ethnic groups (6). Several meta-analyses of cross-sectional and prospective data have suggested broad similarities in the magnitudes of associations of different obesity measures with major cardiometabolic diseases (hypertension, diabetes and dyslipidemia) (28, 29, 30, 31, 32), although slight differences between BMI and central obesity measures in the associations with diabetes were observed (29, 30, 32).Taken together, our data and previous findings suggest general consistency in the magnitudes of associations of different obesity measures with cardiometabolic risk factors. Any possible differences that were suggested by our analyses comparing individual obesity metrics, moreover, are unlikely to be of practical relevance for the use of these measures in clinical settings. Thus, the most important question might be how to best identify subgroups of individuals with excessive cardiometabolic risk using a combination of obesity measures, rather than which obesity measure alone is a stronger or better indicator for major cardiometabolic risk factors.
Prior studies on different obesity measures and cardiometabolic risk factors conducted in the US Hispanics/Latinos have largely examined individuals of Mexican background (15, 16, 17, 18, 19). With the diverse representation of Hispanics/Latinos in the HCHS/SOL, we were able to examine these associations across Hispanic/Latino backgrounds. In general, our data show consistent positive associations between different obesity measures and cardiometabolic risk factors across these background groups. We found little evidence of effect modification by Hispanic/Latino background, with a few nominally statistically significant tests for interaction. However, given the complexity of the biological and cultural diversity within the US Hispanics/Latinos, more studies are needed to investigate potential differences in these associations across Hispanic/Latino backgrounds. It is not surprising that most overweight/obese (abnormal BMI) individuals were classified as abnormal WC or abnormal WHR, and individuals in this subgroup had the most adverse CVD risk factor profile. This is in line with a recent study suggesting that either BMI or WC could identify the same individuals at increased cardiometabolic risk associated with excess adiposity (33). However, interestingly, a large proportion of normal weight individuals were classified as abnormal WHR for both women (50%) and men (40%). Moreover, abnormal WHR were significantly associated with higher prevalences of all three major cardiometabolic diseases, particularly diabetes (adjusted PR=3.99 for women and 3.05 for men) among normal weight individuals, suggesting that WHR measurement is informative and facilitates the identification of a subgroup of normal weight people at increased risk for diabetes and other cardiometabolic diseases. WHR may also reflect a ratio of trunk/abdominal fat and leg fat deposits, and a number of studies have demonstrated that trunk/abdominal fat is unfavorably associated with cardiometabolic risk factors, whereas leg fat is favorably associated with cardiometabolic risk factors (34, 35, 36, 37, 38, 39). A previous large-scale analysis showed that BMI and central obesity measures, particular WHR, assessed in combination could improve CVD risk prediction, and it is not surprising that the improvement was modest when data on conventional CVD risk factors (blood pressure, blood lipids, and diabetes, which are major mediators of adiposity and CVD (40)) were included (8).
Another finding of our study is that more direct measures of overall adiposity, FMI and %BF did not show stronger associations with cardiometabolic risk factors than BMI. Indeed, BMI was very highly correlated with FMI (r=0.94) and %BF (r≥0.88), suggesting that they may serve as alternate proxy measures of overall obesity. However, we only observed moderate agreement between normal and abnormal categories of BMI and %BF. Greater than 41% of normal weight women had abnormal %BF (≥30%), and those women were more likely to have hypertension, diabetes, and dyslipidemia as well as adverse cardiometabolic traits. These findings indicate that %BF, measured by bioelectrical impedance analysis which is a feasible and efficient method in large epidemiological studies (9, 10), is useful to identify normal weight people with excess adiposity at high cardiometabolic risk.
To the best of our knowledge, this is the largest study to date to evaluate different obesity measures and their relationships with major cardiometabolic risk factors as well as multiple cardiometabolic biomarkers among US Hispanics/Latinos. Our study population is a representative sample of Hispanic/Latino individuals of diverse backgrounds in 4 US communities, and multiple covariates were adjusted in our analyses. Nevertheless, our findings are limited to the nature of cross-sectional data and hence a lack of data on incident CVD events. However, conventional CVD risk factors examined in the current study appear to largely explain the excess obesity-related CVD risk (40). In addition, we used cut-off values for abnormal obesity measures that were originally derived from non-Hispanic white populations, since insufficient data are available to derive cut-offs for Hispanic populations. Finally, although we have included multiple measures for overall and central obesity, our study lacked data on precise measurements of regional fat distribution measured by computed tomography or magnetic resonance imaging. However, these approaches are expensive and time-consuming, which may be impractical for large epidemiological studies.
In conclusion, our study shows that overall and central obesity measures were all associated with diabetes and other cardiometabolic diseases, as well as adverse cardiometabolic traits, and they performed similarly in their magnitudes of associations with cardiometabolic risk factors in US Hispanic/Latino women and men. As increases in other obesity measures (such as WHR) are also associated with CVD risk factors regardless of body weight, BMI alone may be insufficient as the only obesity measure to indicate increased cardiometabolic risk, particularly in those with normal weight. BMI and other obesity measures assessed in combination are useful to identify individuals at increased cardiometabolic risk, particularly of diabetes risk, associated with excess adiposity.
Supplementary Material
Figure S1. Mean (95% confidence interval) values of cardiometabolic markers according to normal and abnormal categories of BMI and WC.
Figure S2. Mean (95% confidence interval) values of cardiometabolic markers according to normal and abnormal categories of BMI and %BF.
Table S1. Prevalence of major cardiovascular disease risk factors among Hispanics/Latinos residing in 4 US urban centers, the Hispanic Community Health Study/Study of Latinos, 2008-2011*
Table S2. Among women, weighted prevalence ratios (95% CIs) for hypertension, diabetes, and dyslipidemia associated with one standard deviation increase in obesity measures, stratified by Hispanic/Latino background*
Table S3. Among men, weighted prevalence ratios (95% CIs) for hypertension, diabetes, and dyslipidemia associated with one standard deviation increase in obesity measures, stratified by Hispanic/Latino background*
Study Importance.
What is already known about this subject?
Increased levels of adiposity are related to poor cardiometabolic biomarker profiles and adverse cardiovascular health outcomes.
Several measures have been developed to improve the assessment of overall and central adiposity, and therefore inform interventions to reduce cardiovascular risk.
U.S. Hispanics/Latinos are disproportionately affected by obesity and cardiovascular disease relative to their non-Hispanic White counterparts.
What does this study add?
We show among a novel, population-based sample of 16,000 Hispanics/Latinos that several measures of obesity are highly correlated with one another, and are related to cardiovascular risk factors to a similar degree.
Even among individuals of normal body weight, Hispanic/Latino men and women with waist-to-hip ratios above clinical thresholds are much more likely to have prevalent hypertension, adverse lipid profiles, and particularly diabetes.
Acknowledgments
The authors thank the staff and participants of HCHS/SOL for their important contributions. A complete list of staff and investigators has been provided by Sorlie P., et al. in Ann Epidemiol. 2010;20:642-649 and is also available on the study website http://www.cscc.unc.edu/hchs/.
Funding: The baseline examination of the Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contributed to the HCHS/SOL first funding period through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the NIH Office of Dietary Supplements.
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA : the journal of the American Medical Association. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, et al. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation. 2014;130:593–625. doi: 10.1161/CIR.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA : the journal of the American Medical Association. 2012;308:1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schneiderman N, Llabre M, Cowie CC, Barnhart J, Carnethon M, Gallo LC, et al. Prevalence of Diabetes Among Hispanics/Latinos From Diverse Backgrounds: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Diabetes Care. 2014;37:2233–2239. doi: 10.2337/dc13-2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heiss G, Snyder ML, Teng Y, Schneiderman N, Llabre MM, Cowie C, et al. Prevalence of Metabolic Syndrome Among Hispanics/Latinos of Diverse Background: The Hispanic Community Health Study/Study of Latinos. Diabetes Care. 2014;37:2391–2399. doi: 10.2337/dc13-2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huxley R, Mendis S, Zheleznyakov E, Reddy S, Chan J. Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk[mdash]a review of the literature. Eur J Clin Nutr. 2009;64:16–22. doi: 10.1038/ejcn.2009.68. [DOI] [PubMed] [Google Scholar]
- 7.Qiao Q, Nyamdorj R. Is the association of type II diabetes with waist circumference or waist-to-hip ratio stronger than that with body mass index? Eur J Clin Nutr. 2010;64:30–34. doi: 10.1038/ejcn.2009.93. [DOI] [PubMed] [Google Scholar]
- 8.Emerging Risk Factors C. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barbosa-Silva MC, Barros AJ, Wang J, Heymsfield SB, Pierson RN., Jr Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Am J Clin Nutr. 2005;82:49–52. doi: 10.1093/ajcn.82.1.49. [DOI] [PubMed] [Google Scholar]
- 10.Sun SS, Chumlea WC, Heymsfield SB, Lukaski HC, Schoeller D, Friedl K, et al. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr. 2003;77:331–340. doi: 10.1093/ajcn/77.2.331. [DOI] [PubMed] [Google Scholar]
- 11.Bohm A, Heitmann BL. The use of bioelectrical impedance analysis for body composition in epidemiological studies. Eur J Clin Nutr. 2013;67 Suppl 1:S79–85. doi: 10.1038/ejcn.2012.168. [DOI] [PubMed] [Google Scholar]
- 12.VanItallie TB, Yang MU, Heymsfield SB, Funk RC, Boileau RA. Height-normalized indices of the body's fat-free mass and fat mass: potentially useful indicators of nutritional status. Am J Clin Nutr. 1990;52:953–959. doi: 10.1093/ajcn/52.6.953. [DOI] [PubMed] [Google Scholar]
- 13.Kyle UG, Schutz Y, Dupertuis YM, Pichard C. Body composition interpretation. Contributions of the fat-free mass index and the body fat mass index. Nutrition. 2003;19:597–604. doi: 10.1016/s0899-9007(03)00061-3. [DOI] [PubMed] [Google Scholar]
- 14.Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes. 2010;34:791–799. doi: 10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]
- 15.Wei M, Gaskill SP, Haffner SM, Stern MP. Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans--a 7-year prospective study. Obesity research. 1997;5:16–23. doi: 10.1002/j.1550-8528.1997.tb00278.x. [DOI] [PubMed] [Google Scholar]
- 16.Zhu S, Heymsfield SB, Toyoshima H, Wang Z, Pietrobelli A, Heshka S. Race-ethnicity-specific waist circumference cutoffs for identifying cardiovascular disease risk factors. Am J Clin Nutr. 2005;81:409–415. doi: 10.1093/ajcn.81.2.409. [DOI] [PubMed] [Google Scholar]
- 17.Ghandehari H, Le V, Kamal-Bahl S, Bassin SL, Wong ND. Abdominal obesity and the spectrum of global cardiometabolic risks in US adults. International journal of obesity. 2009;33:239–248. doi: 10.1038/ijo.2008.252. [DOI] [PubMed] [Google Scholar]
- 18.MacKay MF, Haffner SM, Wagenknecht LE, D'Agostino RB, Jr, Hanley AJ. Prediction of type 2 diabetes using alternate anthropometric measures in a multi-ethnic cohort: the insulin resistance atherosclerosis study. Diabetes care. 2009;32:956–958. doi: 10.2337/dc08-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herrera VM, Casas JP, Miranda JJ, Perel P, Pichardo R, Gonzalez A, et al. Interethnic differences in the accuracy of anthropometric indicators of obesity in screening for high risk of coronary heart disease. International journal of obesity. 2009;33:568–576. doi: 10.1038/ijo.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lavange LM, Kalsbeek WD, Sorlie PD, Aviles-Santa LM, Kaplan RC, Barnhart J, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry. 1972;18:499–502. [PubMed] [Google Scholar]
- 23.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 24.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA : the journal of the American Medical Association. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes care. 2010;33 Suppl 1:S62–69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 27.Benedict C, Axelsson T, Soderberg S, Larsson A, Ingelsson E, Lind L, et al. Fat mass and obesity-associated gene (FTO) is linked to higher plasma levels of the hunger hormone ghrelin and lower serum levels of the satiety hormone leptin in older adults. Diabetes. 2014;63:3955–3959. doi: 10.2337/db14-0470. [DOI] [PubMed] [Google Scholar]
- 28.Vazquez G, Duval S, Jacobs DR, Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiologic reviews. 2007;29:115–128. doi: 10.1093/epirev/mxm008. [DOI] [PubMed] [Google Scholar]
- 29.Huxley R, James WPT, Barzi F, Patel JV, Lear SA, Suriyawongpaisal P, et al. Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obesity Reviews. 2008;9:53–61. doi: 10.1111/j.1467-789X.2007.00439.x. [DOI] [PubMed] [Google Scholar]
- 30.Decoda Study G, Nyamdorj R, Qiao Q, Lam TH, Tuomilehto J, Ho SY, et al. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity. 2008;16:1622–1635. doi: 10.1038/oby.2008.73. [DOI] [PubMed] [Google Scholar]
- 31.Barzi F, Woodward M, Czernichow S, Lee CM, Kang JH, Janus E, et al. The discrimination of dyslipidaemia using anthropometric measures in ethnically diverse populations of the Asia-Pacific Region: the Obesity in Asia Collaboration. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2010;11:127–136. doi: 10.1111/j.1467-789X.2009.00605.x. [DOI] [PubMed] [Google Scholar]
- 32.Savva SC, Lamnisos D, Kafatos AG. Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes, metabolic syndrome and obesity : targets and therapy. 2013;6:403–419. doi: 10.2147/DMSO.S34220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abbasi F, Blasey C, Reaven GM. Cardiometabolic risk factors and obesity: does it matter whether BMI or waist circumference is the index of obesity? The American Journal of Clinical Nutrition. 2013;98:637–640. doi: 10.3945/ajcn.112.047506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boorsma W, Snijder MB, Nijpels G, Guidone C, Favuzzi AM, Mingrone G, et al. Body composition, insulin sensitivity, and cardiovascular disease profile in healthy Europeans. Obesity. 2008;16:2696–2701. doi: 10.1038/oby.2008.433. [DOI] [PubMed] [Google Scholar]
- 35.Van Pelt RE, Evans EM, Schechtman KB, Ehsani AA, Kohrt WM. Contributions of total and regional fat mass to risk for cardiovascular disease in older women. American journal of physiology Endocrinology and metabolism. 2002;282:E1023–1028. doi: 10.1152/ajpendo.00467.2001. [DOI] [PubMed] [Google Scholar]
- 36.Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer CD, Yudkin JS, et al. Trunk fat and leg fat have independent and opposite associations with fasting and postload glucose levels: the Hoorn study. Diabetes care. 2004;27:372–377. doi: 10.2337/diacare.27.2.372. [DOI] [PubMed] [Google Scholar]
- 37.Sakai Y, Ito H, Egami Y, Ohoto N, Hijii C, Yanagawa M, et al. Favourable association of leg fat with cardiovascular risk factors. Journal of internal medicine. 2005;257:194–200. doi: 10.1111/j.1365-2796.2004.01432.x. [DOI] [PubMed] [Google Scholar]
- 38.Williams MJ, Hunter GR, Kekes-Szabo T, Snyder S, Treuth MS. Regional fat distribution in women and risk of cardiovascular disease. Am J Clin Nutr. 1997;65:855–860. doi: 10.1093/ajcn/65.3.855. [DOI] [PubMed] [Google Scholar]
- 39.Wu H, Qi Q, Yu Z, Sun Q, Wang J, Franco OH, et al. Independent and opposite associations of trunk and leg fat depots with adipokines, inflammatory markers, and metabolic syndrome in middle-aged and older Chinese men and women. J Clin Endocrinol Metab. 2010;95:4389–4398. doi: 10.1210/jc.2010-0181. [DOI] [PubMed] [Google Scholar]
- 40.Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. The Lancet. 383:970–983. doi: 10.1016/S0140-6736(13)61836-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Mean (95% confidence interval) values of cardiometabolic markers according to normal and abnormal categories of BMI and WC.
Figure S2. Mean (95% confidence interval) values of cardiometabolic markers according to normal and abnormal categories of BMI and %BF.
Table S1. Prevalence of major cardiovascular disease risk factors among Hispanics/Latinos residing in 4 US urban centers, the Hispanic Community Health Study/Study of Latinos, 2008-2011*
Table S2. Among women, weighted prevalence ratios (95% CIs) for hypertension, diabetes, and dyslipidemia associated with one standard deviation increase in obesity measures, stratified by Hispanic/Latino background*
Table S3. Among men, weighted prevalence ratios (95% CIs) for hypertension, diabetes, and dyslipidemia associated with one standard deviation increase in obesity measures, stratified by Hispanic/Latino background*


