Abstract
Background
Ulnar impaction syndrome (UIS) is a common cause of ulnar wrist pain. Patients may be candidates for surgical intervention if nonoperative options are ineffective. At our institution, ulnar shortening osteotomy is the preferred procedure to manage this disorder. The purpose of this study was to present patient reported outcomes and complication rates of ulnar shortening osteotomy (USO) at mid-term follow-up.
Methods
A retrospective chart review of 72 patients (75 wrists) obtained from our institutional database was performed. At a mean 32 months postoperatively, telephone interviews (n = 53) were performed for all patients who were available for follow-up. The patient-rated wrist evaluation (PRWE), a validated outcome tool, was completed and complications were reviewed.
Results
Patient-rated outcomes were favorable; however, complications were frequent and included: delayed union (10/75, 13.3 %), nonunion (6/75, 8 %), and complex regional pain syndrome (5/75, 6.7 %). Ten patients (13.3 %) required revision surgery. Thirty-four patients (45.3 %) required hardware removal with 4/30 (11.4 %) of these patients experiencing refracture. Smokers (mean PRWE 67.1) and patients with workers’ compensation claims (mean PRWE 64.9) reported higher residual pain and disability than their counterparts (mean PRWE 28.0; 25.2).
Conclusions
General outcome measures were favorable. Smokers and patients with workers’ compensation claims experienced significantly poorer outcomes. However, the incidence of nonunion and delayed union was higher than most reports in the literature. Furthermore, we demonstrated a high refracture rate (11.4 %) following removal of hardware.
Keywords: Ulnar shortening osteotomy, Workers compensation, Smoking, Nonunion, PRWE
Introduction
Ulnar impaction syndrome (UIS) occurs when the ulnar head abuts the TFCC and carpus resulting in ulnar-sided wrist pain, tears in the TFCC and lunotriquetral ligaments and degenerative changes on the ulnar head and adjacent carpus [3, 14]. This syndrome is the source of pain and dysfunction particularly in patients performing repetitive movements of the hand and wrist. If nonoperative treatments fail, surgical treatment options for UIS include wafer resection and ulnar shortening osteotomy (USO) [37]. The wafer resection may be performed arthroscopically and is considered minimally invasive [2]. However, this technique accesses the ulnar head through a concomitant TFCC tear, cannot address issues with ulnocarpal instability, and has limits to the amount of shortening that can be achieved. The USO is capable of larger corrections of ulnar positive variance and may improve ulnocarpal stability by indirectly tensioning the ulnocarpal ligaments. However, the USO is more invasive and carries with it the risk of hardware irritation, delayed union, and nonunion [2, 9, 36]. Favorable outcomes have been reported with both techniques [9, 36].
There is a paucity of research examining complications and mid-term outcomes of USO in large patient populations. For example, Moser et al. reported on outcomes in 73 wrists, but patient follow-up was a mean of 7.8 months [29]. Similarly, Tatabe et al. achieved a mean follow-up of 11 years; however, this study had a sample size of 30 [33]. The purpose of this study is to assess complication rates and mid-term patient reported outcomes of USO with a valid patient-rated measure in a large cohort of patient with UIS.
Patients and Methods
Ethics approval was obtained from our institutional review board. The operating room and billing databases at our tertiary care center, specializing in hand surgery, were reviewed from 2006–2011 to identify eligible patients. Eighty-seven USOs in 84 patients were identified. Exclusion criteria included less than 1 year of follow-up (n = 12) and age less than 18.
The remaining 72 patients underwent retrospective chart review. Demographic data was obtained including age, gender, osteotomy type, smoking status, diabetes, other contributory health concerns, and workers’ compensation claims. The underlying etiology for UIS was determined as either idiopathic or post-traumatic. Post-operative complications including nonunion, delayed union, infection, chronic regional pain syndrome (CRPS), hardware irritation requiring removal, and fracture following removal of hardware were obtained. CRPS was diagnosed using previously established criteria [16]. Delayed union was defined as the absence of callous formation on radiographic analysis by 12 weeks following surgery [15]. Nonunions were confirmed with CT scan by the absence of any bridging callous at a minimum of 16 weeks following surgery and ongoing pain at the osteotomy site [20, 32]. In the event of a nonunion, the patient’s initial incision was utilized. The nonunion site was debrided and bone grafting from the distal radius, iliac crest, or allomatrix (Wright Medical Technologies, USA) was used in addition to revising the hardware.
Following retrospective chart review, patients were telephoned in order to administer the patient-rated wrist evaluation (PRWE), a validated outcome tool for patient pain and disability. A total of 51 patients (53 wrists) participated. One patient refused to participate and 21 patients could not be contacted. In addition to the administering of the PRWE, patients were also asked whether they had experienced any postoperative complications to ensure all complications were captured. Patient PRWE scores were collected as a pain score, function score, and total score. Variables potentially affecting complication rates and outcomes including smoking, gender, WSIB claims, osteotomy type, and diagnosis were then analyzed.
Four fellowship trained hand surgeons performed the 75 USOs in the series. Patients undergoing USO were given regional or general anesthetic. A 3.5-mm low contact dynamic compression plate (Dupuy-Synthes Corporation, West Chester, PA) was used in all cases. The goal of surgery was to restore a 2 mm negative ulnar variance. Either a transverse osteotomy (n = 57) or a 45° oblique osteotomy (n = 18) was utilized based on the surgeon’s preference. Osteotomies were performed by utilizing a reciprocating saw with normal saline irrigation. Patients were placed in a forearm cast for a period of 6–12 weeks. Between groups, comparisons were performed using an independent Student’s t test for continuous variables and a chi-square test for categorical variables. Statistical significance was considered for results with p < 0.05.
Results
Analysis of Complications
Seventy-five USOs were performed in 72 patients. Demographic information is listed in Table 1. There were 26 males and 46 females in the series. The mean age at the time of procedure was 43.9 years (SD 13.1) with a mean follow-up of 32.0 months (range 12–75.3; SD 19.9). Twenty-five patients were involved in workers’ compensation claims, and 24 patients had a diagnosis of post-traumatic UIS.
Table 1.
Demographic information for patients undergoing ulnar shortening osteotomy
| Total patient group (n = 75) (%) | Outcome score group (n = 53) (%) | |
|---|---|---|
| Age (years) | 43.9 (SD 13.1) | 44.7 (SD 12.4) |
| Male | 25 (33.3) | 17 (32.1) |
| Female | 47 (62.7) | 36 (68.0) |
| Follow-up (months) | 32.0 (SD 19.9) | 36.0 (SD 19.4) |
| Idiopathic UIS | 51 (68.0) | 37 (70.0) |
| Post-traumatic UIS | 24 (32.0) | 16 (30.2) |
| Workers compensation | 25 (33.3) | 20 (37.7) |
| Transverse osteotomy | 57 (76.0) | 43 (81.1) |
| Oblique osteotomy | 18 (24.0) | 10 (18.9) |
| Smoker | 24 (32.0) | 17 (32.1) |
| Diabetes | 0 (0.0) | 0 (0.0) |
Complications of USO are listed in Table 2. The incidence of nonunion was 8 % (6/75) (diagnosed at mean of 33 weeks) and delayed union was 13.3 % (10/75) with a mean time to union of 24.1 weeks (SD 15.2) in these patients. An Exogen external bone stimulator (Smith and Nephew, Memphis TN) was utilized in three cases of delayed union. There was no significant difference in nonunion or delayed union rate between smokers and nonsmokers (p = 0.18; p = 0.58). The incidence of CRPS was 6.7 % (5/75). One patient (1.3 %) in the series developed an infection requiring irrigation and debridement and intravenous antibiotics.
Table 2.
Complications of ulnar shortening osteotomy
| n (%) | |
|---|---|
| Nonunion | 6 (8) |
| Delayed union | 10 (13.3) |
| Exogena low-intensity pulsed ultrasound | 3 (4) |
| Infection | 1 (1.3) |
| CRPS | 5 (6.7) |
| Removal of hardware (ROH) | 34 (45.3) |
| Fracture following ROH | 4 (11.4) |
| Reoperation (excluding ROH) | 10 (13.3) |
CRPS chronic regional pain syndrome
aSmith and Nephew, United Kingdom
Complications following the transverse (n = 57) and oblique osteotomy (n = 18) groups were compared. There were six nonunions and six delayed unions in the transverse osteotomy group compared to zero nonunions and four delayed unions in the oblique osteotomy group. However, this was not statistically significant (p = 0.15; p = 0.20). Similarly, there were five episodes of CRPS in the transverse osteotomy group and zero in the oblique osteotomy group. Again, this was not statistically significant (p = 0.19).
The incidence of hardware irritation resulting in removal of hardware (ROH) was 45.3 % (34/75). The mean time to ROH from time of USO was 1.1 year (SD 0.65). Of this group, 11.4 % (4/35) experienced fracture following ROH. The mean time from ROH to fracture was 12.8 weeks (range 4.0–22.5). The mean time from USO to ROH in these four patients was 1.2 years (range 1.0–1.3). Two of the patients who were refractured ultimately went on to nonunion requiring revision surgery with iliac crest bone graft while the other two patients healed with cast immobilization.
The overall incidence of reoperation, excluding ROH, was 13.3 % (10/75). Surgeries include six for nonunion, two for nonunion following fracture, one for pre-existing DRUJ instability, and one for infection. Gender, diagnosis, or workers’ compensation claims were not found to be a statistically significant factor with respect to any complication.
Patient-Rated Outcome Measure
Fifty-one patients (53 wrists) prospectively underwent telephone interview to obtain the PRWE outcome score. Demographic information for this subgroup is demonstrated in Table 1. The mean age in this group was 44.7 (SD 12.4) with a mean follow-up of 36.0 months (SD 19.7). There were no significant demographic differences between these patients and those that were not available for prospective follow-up. Only one additional complication of CRPS was identified during telephone interview, thus indicating the validity of our records in capturing all complications.
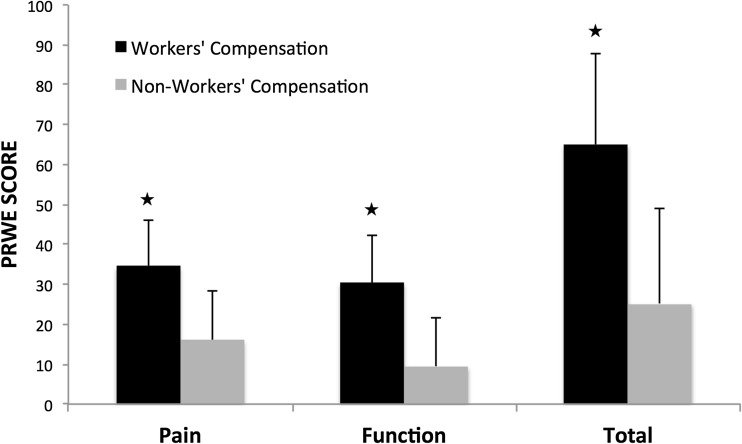
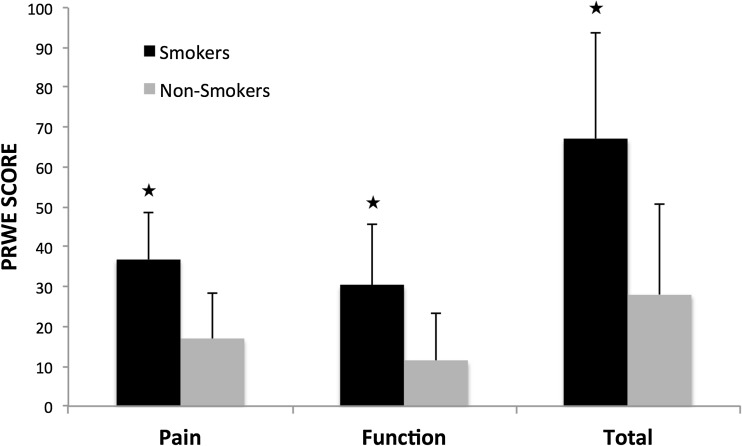
The mean PRWE score in this group was 40.2 (SD 30.3). Patients with workers’ compensation claims (n = 20) had significantly poorer PRWE scores (total mean score 64.9; SD 22.8) than non-WSIB claims (total mean score 25.2; SD 23.8; p < 0.001) (Fig. 1). There were no significant demographic differences between these groups. Similarly, Fig. 2 demonstrates that smokers (n = 17) had significantly poorer PRWE scores (total mean score 67.1; SD 26.5) than nonsmokers (total mean score 28.0; SD 22.9; p = < 0.001).
Fig. 1.
Histogram demonstrating mean pain, function, and total patient-rated wrist evaluation (PRWE) scores in workers’ compensation versus non-workers’ compensation patients undergoing ulnar shortening osteotomy. Standard deviation bars indicate the 95 % confidence interval. *p < 0.05; indicates significance
Fig. 2.
Histogram demonstrating mean pain, function, and total patient-rated wrist evaluation (PRWE) scores in smokers versus nonsmokers undergoing ulnar shortening osteotomy. Standard deviation bars indicate the 95 % confidence interval. *p < 0.05; indicates significance
Patients sustaining complications (n = 14) did not report higher pain or disability (total mean score 50.9; SD 33.3) compared to patients without complications (total mean score 36.3; SD 28.6; p = 0.12). With further analysis, there was also no significant difference in patients sustaining nonunions and delayed unions compared to patients experiencing union (p = 0.42). Gender, primary diagnosis, and hardware removal did not have a statistically significant effect on PRWE score (p = 0.57; p = 0.47; p = 0.65).
Discussion
We present mid-term data for a large cohort of patients undergoing USO with mean of 32 months follow-up. We also include outcome data with a response rate of approximately 70 %. We used the patient-rated wrist evaluation (PRWE) score as our outcome tool for patients undergoing USO. The PRWE has previously been validated and is used to quantify patient-rated wrist pain and disability [4, 23]. The benefit of the PRWE compared to other measures, such as the disability of arm, shoulder, and hand (DASH), is that it is more sensitive to change and eliminates a potential source of bias in the event that the patient has corresponding proximal arm pathology [19].
The incidence of nonunion and delayed union in the current study is 8 and 13.3 %, respectively, which are higher rates than most seen in the literature. Studies currently quote a 0–18 % incidence of nonunion [6, 8, 10, 26, 35, 38]. However, the sample sizes of these studies are relatively small and may not accurately represent this cohort of patients. Smokers in the current study demonstrated no significant difference in incidence of nonunion compared to nonsmokers but we were underpowered to detect differences in this subgroup. A study by Chen et al. demonstrated that 30 % of smokers compared to 0 % of nonsmokers developed a nonunion [7]. Furthermore, smokers took an average of 3 months longer than nonsmokers to heal. Studies have also demonstrated that patients receiving an oblique osteotomy may have a lower risk of nonunion as well as decreased time to union [6, 8, 26, 31]. While we did not observe any nonunions in patients receiving oblique osteotomies, this association was not statistically significant, although this comparison is likely underpowered.
We demonstrate a 45.3 % incidence of hardware removal in our patient sample. This is comparable to other studies in the literature [6, 30]. Four patients experienced a fracture following removal hardware. These patients underwent removal of their hardware at a mean of 1.2 years following USO. Two of these patients required reoperation consisting of open reduction internal fixation with iliac crest bone graft. Pomerance demonstrated a 2.5 % incidence of refracture following ROH (mean time to ROH, 6.6 months) in USO patients [30]. In a study by Mih et al., 11.3 % of patients refractured following ROH (mean time to ROH, 19 months) from various forearm pathologies [25]. Unfortunately, there is no consensus in the literature for the optimal time of hardware removal.
The incidence of CRPS in the current study was 6.7 %, similar to that seen in the literature [1, 22]. Each of these patients required follow-up with either a neurologist or anesthesiologist specialized in chronic pain syndromes. We could not determine any factors that significantly increased the risk of developing CRPS within our patient group.
Fifty-one patients (53 wrists) underwent telephone interview to obtain PRWE scores. Subgroup analysis demonstrated that both smokers and workers’ compensation patients had significantly worse outcomes than their counterparts. Studies have demonstrated that workers’ compensation (WC) patients experience poorer outcomes in various fields including joint replacement, rotator cuff repair, and carpal tunnel release [12, 13, 18, 21]. Furthermore, WC patients require more preoperative clinic visits and diagnostic testing [11]. Many studies have also demonstrated that smokers experience more perioperative complications and poorer outcomes compared to nonsmokers [5, 17, 24, 27, 28, 34]. Although smokers in the current study did not have a significant increase in complications, they did experience significantly poorer PRWE scores.
There are several limitations in the current study. We were not able to obtain preoperative PRWE scores so could not determine the extent of improvement between pre- and postoperative assessment. Furthermore, PRWE outcome scores were only available on 53 of 75 wrists. Despite this, we believe the results obtained from this sample represent the outcomes of the entire group. The study may have been underpowered to detect differences in subgroup analyses such as nonunion rates in smokers. We observed similar complication rates compared to those seen in the literature except for a higher incidence of nonunion and delayed union. We also demonstrated that smokers and WSIB patients experience significantly poorer results from USO. The results of the current study indicate that the oblique osteotomy demonstrates a trend toward better union rates and that smokers and workers’ compensation patients should be counseled as to the likelihood of poorer outcomes with USO.
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval
The University of Western Ontario Research Ethics Board for Health Sciences Research Involving Human Subjects (HSREB)
Ethics Approval Number
18912E
Conflict of Interest
Raghav Rajgopal declares that he has no conflict of interest.
James Roth declares that he has no conflict of interest.
Graham King declares that he has no conflict of interest.
Ken Faber MD declares that he has no conflict of interest.
Ruby Grewal declares that she has no conflict of interest.
Statement of Human and Animal Rights
Ethical approval was obtained from the institutional review board. No experimentation was performed on human or animal subjects.
Statement of Informed Consent
No identifying patient information was used in this manuscript. No writing assistance was provided.
Footnotes
James Roth is deceased and therefore signatures and forms will be unavailable for him.
References
- 1.Baek GH, Chung MS, Lee YH, et al. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. J Bone Joint Surg Am. 2005;87(12):2649–54. doi: 10.2106/JBJS.D.02983. [DOI] [PubMed] [Google Scholar]
- 2.Berger, R. Hand Surgery, Volume I. Lippincott Williams & Wilkins, 2004;375–376.
- 3.Cerezal L, del Piñal F, Abascal F, et al. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics. 2002;22(1):105–21. doi: 10.1148/radiographics.22.1.g02ja01105. [DOI] [PubMed] [Google Scholar]
- 4.Changulani M, Okonkwo U, Keswani T, et al. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop. 2008;1:1–6. doi: 10.1007/s00264-007-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheadle WG. Risk factors for surgical site infection. Surg Infect (Larchmt) 2006;7(Suppl 1):S7–11. doi: 10.1089/sur.2006.7.s1-7. [DOI] [PubMed] [Google Scholar]
- 6.Chen NC, Wolfe SW. Ulna shortening osteotomy using a compression device. J Hand Surg [Am] 2003;28:88–93. doi: 10.1053/jhsu.2003.50003. [DOI] [PubMed] [Google Scholar]
- 7.Chen F, Osterman AL, Mahony K. Smoking and bony union after ulna-shortening osteotomy. Am J Orthop. 2001;30:486–9. [PubMed] [Google Scholar]
- 8.Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg [Am] 1993;18(1):46–53. doi: 10.1016/0363-5023(93)90243-V. [DOI] [PubMed] [Google Scholar]
- 9.Constantine KJ, Tomaino MM, Herndon JH, et al. Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. J Hand Surg [Am] 2000;25(1):55–60. doi: 10.1053/jhsu.2000.jhsu025a0055. [DOI] [PubMed] [Google Scholar]
- 10.Darlis NA, Ferraz IC, Kaufmann RW, et al. Step-cut distal ulnar-shortening osteotomy. J Hand Surg [Am] 2005;30(5):943–8. doi: 10.1016/j.jhsa.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 11.Day CS, Alexander M, Lal S, et al. Effects of workers' compensation on the diagnosis and surgical treatment of patients with hand and wrist disorders. J Bone Joint Surg Am. 2010;92(13):2294–9. doi: 10.2106/JBJS.I.00158. [DOI] [PubMed] [Google Scholar]
- 12.De Beer J, Petruccelli D, Gandhi R, et al. Primary total knee arthroplasty in patients receiving workers' compensation benefits. Can J Surg. 2005;48(2):100–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Duncan SF, Calandruccio JH, Merritt MV, et al. A comparison of workers' compensation patients and nonworkers' compensation patients undergoing endoscopic carpal tunnel release. Hand Surg. 2010;15(2):75–80. doi: 10.1142/S0218810410004655. [DOI] [PubMed] [Google Scholar]
- 14.Friedman SL, Palmer AK. The ulnar impaction syndrome. Hand Clin. 1991;7(2):295–310. [PubMed] [Google Scholar]
- 15.Handoll HH, Pearce P. Interventions for treating isolated diaphyseal fractures of the ulna in adults. Cochrane Database Syst Rev. 2012;13:6. doi: 10.1002/14651858.CD000523.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;8(4):326–31. doi: 10.1111/j.1526-4637.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 17.Hawn MT, Houston TK, Campagna EJ, et al. The attributable risk of smoking on surgical complications. Ann Surg. 2011;254(6):914–20. doi: 10.1097/SLA.0b013e31822d7f81. [DOI] [PubMed] [Google Scholar]
- 18.Henn RF, 3rd, Kang L, Tashjian RZ, et al. Patients with workers' compensation claims have worse outcomes after rotator cuff repair. J Bone Joint Surg Am. 2008;90(10):2105–13. doi: 10.2106/JBJS.F.00260. [DOI] [PubMed] [Google Scholar]
- 19.Kim JK, Park ES. Comparative responsiveness and minimal clinically important differences for idiopathic ulnar impaction syndrome. Clin Orthop Relat Res. 2013;471(5):1406–11. doi: 10.1007/s11999-013-2843-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kloen P, Wiggers JK, Buijze GA. Treatment of diaphyseal non-unions of the ulna and radius. Arch Orthop Trauma Surg. 2010;130(12):1439–45. doi: 10.1007/s00402-010-1071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koljonen P, Chong C, Yip D. Difference in outcome of shoulder surgery between workers’ compensation and nonworkers’ compensation populations. Int Orthop. 2009;33(2):315–20. doi: 10.1007/s00264-007-0493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loh YC, Van Den Abbeele K, Stanley JK, et al. The results of ulnar shortening for ulnar impaction syndrome. J Hand Surg (Br) 1999;24(3):316–20. doi: 10.1054/jhsb.1999.0062. [DOI] [PubMed] [Google Scholar]
- 23.MacDermid JC, Richards RS, Donner A, et al. Responsiveness of the short form-36, disability of the arm, shoulder, and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg [Am] 2000;2:330–40. doi: 10.1053/jhsu.2000.jhsu25a0330. [DOI] [PubMed] [Google Scholar]
- 24.McRae S, Leiter J, Walmsley C, et al. Relationship between self-reported shoulder function/quality of life, body mass index, and other contributing factors in patients awaiting rotator cuff repair surgery. J Shoulder Elbow Surg. 2011;20(1):57–61. doi: 10.1016/j.jse.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Mih AD, Cooney WP, Idler RS, et al. Long-term follow-up of forearm bone diaphyseal plating. Clin Orthop Relat Res. 1994;299:256–8. [PubMed] [Google Scholar]
- 26.Mizuseki T, Tsuge K, Ikuta Y. Precise ulna-shortening osteotomy with a new device. J Hand Surg [Am] 2001;26:931–9. doi: 10.1053/jhsu.2001.26201. [DOI] [PubMed] [Google Scholar]
- 27.Moller AM, Villebro N, Pedersen T, et al. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet. 2002;359:114–7. doi: 10.1016/S0140-6736(02)07369-5. [DOI] [PubMed] [Google Scholar]
- 28.Moller AM, Pedersen T, Villebro N, et al. Effect of smoking on early complications after elective orthopaedic surgery. J Bone Joint Surg (Br) 2003;85-B:178–81. doi: 10.1302/0301-620X.85B2.13717. [DOI] [PubMed] [Google Scholar]
- 29.Moser VL, Gohritz A, Kitzinger HB, et al. Ulna shortening osteotomy using a new 7 hole gliding plate : results from 73 cases. Acta Orthop Belg. 2012;78(3):317–22. [Google Scholar]
- 30.Pomerance J. Plate removal after ulnar shortening osteotomy. J Hand Surg [Am] 2005;30(5):949–53. doi: 10.1016/j.jhsa.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 31.Rayhack JM, Gasser SI, Latta LL, et al. Precision oblique osteotomy for shortening of the ulna. J Hand Surg [Am] 1993;18:908–18. doi: 10.1016/0363-5023(93)90065-B. [DOI] [PubMed] [Google Scholar]
- 32.Ring D, Allende C, Jafarnia K, Allende BT, Jupiter JB. Ununited diaphyseal forearm fractures with segmental defects: plate fixation and autogenous cancellous bone-grafting. J Bone Joint Surg Am. 2004;86-A(11):2440–5. [PubMed] [Google Scholar]
- 33.Tatebe M, Shinohara T, Okui N, et al. Clinical, radiographic, and arthroscopic outcomes after ulnar shortening osteotomy: a long-term follow-up study. J Hand Surg [Am] 2012;37(12):2468–74. doi: 10.1016/j.jhsa.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Thangarajah T, Prasad PSV, Narayan B. Surgical site infections following open reduction and internal fixation of ankle fractures. Open Orthop J. 2009;3:56–60. doi: 10.2174/1874325000903010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Sanden S, De Smet L. Ulnar shortening after failed arthroscopic treatment of triangular fibrocartilage complex tears. Chir Main. 2001;20(5):332–6. doi: 10.1016/S1297-3203(01)00055-5. [DOI] [PubMed] [Google Scholar]
- 36.Vandenberghe L, Degreef I, Didden K, et al. Ulnar shortening or arthroscopic wafer resection for ulnar impaction syndrome. Acta Orthop Belg. 2012;78(3):323–6. [PubMed] [Google Scholar]
- 37.Watanabe A, Souza F, Vezeridis PS, et al. Ulnar-sided wrist pain. II. Clinical imaging and treatment. Skelet Radiol. 2010;39(9):837–57. doi: 10.1007/s00256-009-0842-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wehbe MA, Cautilli DA. Ulnar shortening using the AO small distractor. J Hand Surg [Am] 1995;20:959–64. doi: 10.1016/S0363-5023(05)80143-1. [DOI] [PubMed] [Google Scholar]