INTRODUCTION
The Institute of Medicine’s National Cancer Policy Board report warns that the healthcare workforce is inadequate to meet the rising demand for cancer care.1 Nurses comprise the largest proportion of the oncology workforce, yet retention is a persistent challenge. Therefore, strategies to improve the work environments of nurses are essential to promote staff retention, stabilize workloads, and effectively deliver high quality, safe patient care. These strategies include capturing nurses’ perspectives on how to retain an adequate workforce, how to strengthen practice environments, and improve patient safety. Such data can be collected, analyzed, and applied by nursing leaders to support evidence-based executive decisions.
Recent measurement advances have enabled researchers to document the variation in nursing practice environments across institutions.2 Unfavorable practice environments are associated with several adverse outcomes, including job dissatisfaction, intention to leave current position, and increased accidental exposure to hazardous drugs.3,4 While variation in working conditions are documented across institutions, no studies to date have examined variation within institutions. Such an approach would enable institutions to correct deficiencies and learn from best practices within health care organizations. Similarly, the perspectives of nursing leaders and advanced practice nurses, such as nurse practitioners and clinical nurse specialists, have not been studied.
The Dana-Farber Cancer Institute (DFCI) employs approximately 329 registered nurses and 76 nurse practitioners. Ambulatory care volume at DFCI and three satellites was 216,150 patient visits in fiscal year 2014. DFCI is one of the few ambulatory care-based facilities that is recognized by the American Nurses’ Credentialing Center Magnet Recognition Program® for nursing excellence.5 The DFCI Nursing and Patient Care Services (NPCS) department leadership team supports the measurement and improvement of practice environments to support the delivery of excellent patient care. The institution collects and submits data to the National Database of Nursing Quality Indicators.6 However, these measures focus on acute care indicators and many measures do not apply directly to ambulatory oncology settings. Therefore, the NPCS department launched a one-year project to assess the nursing practice environments and performance of behaviors that support patient safety, and several nursing outcomes including nurse satisfaction and intention to leave. The leadership team plans to use the data to identify and prioritize interventions to strengthen the practice environments within specific units. The methods and study findings have great relevance to the large number of ambulatory oncology settings in the United States, where the bulk of cancer care is delivered. The objective of this paper is to examine the patterns and correlates of the work environment for nurses and nurse practitioners working in a National Cancer Institute-designated Comprehensive Cancer.
METHODS
This descriptive study employed a web-based survey of registered nurses and advanced practice nurses employed by DFCI to address three research objectives: (1) To examine nurse-reported outcomes throughout the institution, (2) to examine how the practice environment of registered nurses in our institution correlates with these outcomes, and (3) to identify variation in practice environments and the presence or absence of behaviors congruent with patient safety across units. Given the project’s impetus to motivate quality improvement and our omission of personal identifiers from the survey, the institutional review board deemed the study exempt from review and waived the need for signed, informed consent.
Sample and Setting
Individuals employed or contracted by DFCI and working within the main campus in Boston or one of three off-site satellite locations who hold a registered nurse license were invited to participate in the survey. The institution’s human resources database identified 403 individuals with an active registered nurse license. These nurses were employed across 13 units, which included the three satellite locations.
Survey and Measures
Qualtrics (Provo, UT), an encrypted, secure cloud-based survey management platform, was used to conduct the study. Dillman’s Tailored Design method7 guided the questionnaire design, introductory cover letter, and reminder scripts to potential participants. Because all measures had been previously assessed for validity and reliability, graduate students conducted pilot testing to assure items could be completed with ease on the web-based platform; these tests confirmed the survey took approximately ten minutes to complete. To encourage participation, all units received snack baskets and a signed card from the Chief Nurse Executive and one of the investigators with no direct management responsibilities. Participation rates were monitored by the study staff and unit directors with low participation rates were encouraged to remind staff to complete the questionnaire. Surveys were distributed and collected over a three month period between November 2013 and January 2014 and included the following measures, which have all been used in prior studies and have documented validity and reliability:
Quality of Care. Nurses were asked to rate the quality of patient care delivered on their unit: poor, fair, good, or excellent.8 Consistent with prior studies,8 The proportion of nurses who endorsed excellent care is reported.
Intention to Leave. Nurses were asked to indicate their intention to stay in their current position. Three answer choices were available: no plans to leave, plan to leave within six months, or plan to leave within one year.9 We report the number of nurses who plan to stay in their current position for at least one year.
Job Satisfaction. Nurses were asked their satisfaction with their current position. Five answer choices were available: very dissatisfied, dissatisfied, neutral, satisfied, or very satisfied.8 We report the proportion of nurses who reported they were satisfied or very satisfied with their current position.
Safety Organizing Scale. This scale captures behaviors theorized to support a safety culture and measures actions that improve patient safety.10 Previously assessed for validity and reliability, nine items are scored on a range of 1–7 (1 = behavior not at all present, 7 = behavior present to a very great extent). Higher scores reflect more frequent performance of safety behaviors. Items include, “When errors happen, we discuss how we could have prevented them.” Cronbach’s alpha in this sample was 0.92.
-
Practice Environment Scale of the Nursing Work Index (PES-NWI). The original scale11 was revised and validated for use in ambulatory oncology settings.2 Nurses were asked to indicate their agreement on the presence of 23 features that support professional nursing practice. Cronbach’s alpha in this sample was 0.94. There are six subscales:
Medical Assistant Support (e.g., medical assistants contribute to smooth patient flow)
Foundations for Quality of Care (e.g., nursing care is based on a patient-centered approach)
Nurse Manager Ability, Leadership, and Support (e.g., manager supports nurses during physician conflict)
Participation in Practice Affairs (e.g., nurses are asked to serve on committees, select equipment)
Collegial Nurse-Physician Relationships (e.g., a lot of teamwork between nurses and physicians)
Staffing and Resource Adequacy (e.g., enough staff and resources to deliver care)
In addition to these six subscales, all 23 items are averaged to construct a composite score. Items are scored from 1–5 (1 = strongly disagree, 5 = strongly agree). Subscale scores that exceed 3.0 indicate agreement the features are present.
The Safety Organizing Scale and the modified Practice Environment Scale of the Nursing Work Index subscales were calculated for each unit by taking the subscale values for each nurse and calculating the mean value across all nurses within one unit. Data summaries were prepared for the entire institution and for individual units.
Demographic information was collected from participants, and included years of experience, educational preparation, certifications, and gender. Participants were also asked to identify their principal function (direct care nurse or non-direct care nurse). Direct care nurses were asked about their primary role (registered nurse or nurse practitioner) and to identify their unit or satellite location. To support confidentiality, unit identification was optional and non-direct care nurses, the majority of whom were administrators, were not asked to identify a unit. To measure workloads, direct care nurses were also asked the number of patients to whom they provided care on their last shift.
Data Analysis
After descriptive statistics were examined, multivariable logistic regression models were estimated to examine the factors associated with job satisfaction, intention to leave, and perceived quality of care. We next examined factors associated with higher scores on the Safety Organizing Scale, which would reflect more frequent performance of behaviors that epitomize high-reliability organizations; this was performed using multivariable linear regression. Standard errors from all regression models were adjusted for clustering of nurses within units. Finally, to examine variation in practice environments within the institution, unit-level means and 95% Confidence Intervals (CIs) of the Safety Organizing Scale and composite measure of the PES-NWI were examined. Results were considered statistically significant at P < .05.
RESULTS
Of 403 eligible participants, 319 (79.2%) surveys were returned and 259 (64.3%) completed the entire survey. Sample characteristics are shown in Table 1. The sample reported a mean (SD) of 7.1 (6.4) years of experience in their current position. Most held full-time positions, and functioned as registered nurses in direct care roles (n=252); 42 (13.2%) were nurse practitioners. The mean (SD) number of patients cared for on the last shift was 10.2 (8.6).
Table 1.
Sample Characteristics
| Analytic Sample (n=319) |
|
|---|---|
|
|
|
| Mean (SD) | |
|
|
|
| Age (years) | 48.2 (11.8) |
| Nursing experience (years) | 22.7 (11.5) |
| Current role experience (years) | 7.1 (6.4) |
| Last shift workload (number of patients) | 10.2 (8.6) |
|
|
|
| n (%) | |
|
|
|
| Job Status | |
| Full-time | 228 (71.5) |
| Part-time | 62 (19.4) |
| Per-diem, contingent, agency | 9 (2.8) |
| Not reported | 20 (6.3) |
| Primary Role | |
| Direct patient care | 252 (79.9) |
| Not direct care | 47 (14.7) |
| Not reported | 20 (6.3) |
| Job Title | |
| Registered nurse | 203 (63.6) |
| Nurse practitioner | 42 (13.2) |
| Not reported | 74 (23.2) |
| Highest education completed | |
| Undergraduate Degree | 191 (60.0) |
| Graduate Degree | 100 (31.3) |
| Not reported | 28 (8.8) |
Note: Undergraduate Degree included: diploma, associates or bachelors degree in any field. Graduate Degree included masters or doctoral degree in any field.
Patterns and Correlates of Nurse-Reported Outcomes
Institution-wide outcomes are shown in Table 2. Excellent quality of care was reported by 57.7% of the sample. The majority of nurses reported they were satisfied (37.3%) or very satisfied (32.0%) with their current position, and 8.2% stated intentions to leave their current position within one year.
Table 2.
Nurse-reported outcomes (N=319)
| n (%) | |
|---|---|
| Quality of care | |
| Fair | 7 (2.2) |
| Good | 85 (26.6) |
| Excellent | 184 (57.7) |
| Not reported | 43 (13.5) |
| Current job satisfaction | |
| Very dissatisfied | 0 (0) |
| Dissatisfied | 15 (4.7) |
| Neutral | 40 (12.5) |
| Satisfied | 119 (37.3) |
| Very satisfied | 102 (32.0) |
| Not reported | 43 (13.5) |
| Intention to stay in current position | |
| No plan to leave | 247 (77.4) |
| Leave within one year | 19 (6.0) |
| Leave within six months | 7 (2.2) |
| Not reported | 46 (14.4) |
The relationship between practice environment reports and four outcomes (quality of care, job satisfaction, and intention to stay in current position, safety organizing behaviors are shown in Table 3. The first three outcomes were assessed with logistic regression, while safety organizing behaviors were assessed using linear regression. All models were adjusted for clustering of nurses within units.
Table 3.
Factors associated with selected nurse outcomes and performance of safety behaviors (n=194)
| Variable | 1. Excellent quality of care | 2. Intent to stay > 1 year | 3. Satisfied/very satisfied in current job | 4. Safety Organizing Scale (Behaviors) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | B | SE | P | |
| PES-NWI subscales, revised for ambulatory oncology | ||||||||||||
| Medical Assistant Support | 1.05 | 0.60 to 1.83 | .87 | 1.42 | 0.89 to 2.27 | .14 | 0.83 | 0.53 to 1.31 | .43 | 0.14 | 0.08 | .10 |
| Foundations for Quality of Care | 3.32 | 1.88 to 5.88 | <.001 | 0.63 | 0.25 to 1.62 | .34 | 3.04 | 0.70 to 13.23 | .14 | 0.64 | 0.10 | <.001 |
| Nurse Manager Ability, Leadership, and Support | 0.84 | 0.39 to 1.81 | .66 | 0.52 | 0.28 to 1.00 | .05 | 1.73 | 1.15 to 2.62 | .01 | 0.14 | 0.09 | .13 |
| Participation in Practice Affairs | 1.62 | 0.48 to 5.44 | .43 | 6.38 | 2.04 to 19.93 | <.001 | 2.59 | 1.15 to 5.83 | .02 | 0.18 | 0.07 | .01 |
| Collegial Nurse-Physician Relationships | 3.11 | 1.97 to 4.91 | <.001 | 1.83 | 1.25 to 2.67 | <.001 | 1.99 | 1.17 to 3.40 | .01 | 0.26 | 0.10 | .01 |
| Staffing and Resource Adequacy | 1.32 | 0.83 to 2.10 | .25 | 1.36 | 0.79 to 2.35 | .27 | 2.23 | 1.49 to 3.34 | <.001 | −0.07 | 0.06 | .21 |
| Last shift workload | 1.00 | 0.97 to 1.02 | .87 | 1.00 | 0.94 to 1.05 | .85 | 0.98 | 0.94 to 1.02 | .42 | 0.00 | 0.01 | .68 |
| Role | ||||||||||||
| Registered Nurse | Ref | Ref | Ref | Ref | ||||||||
| Nurse Practitioner | 1.01 | 0.23 to 4.48 | .99 | 1.75 | 0.36 to 8.49 | .49 | 0.99 | 0.24 to 4.11 | .99 | −0.37 | 0.16 | .02 |
PES-NWI: Practice Environment Scale of the Nursing Work Index. All models were adjusted for clustering of nurses within units.
When correlates of excellent quality of care were examined, significant variables included the presence of Foundations for Quality of Care (OR 3.32., 95% CO 1.88 to 5.88) and Collegial Nurse-Physician Relations (OR 3.11, 95% CI 1.97 to 4.91). Factors significantly associated with intention to stay in current position included Participation in Practice Affairs (OR 6.38, 95% CI 2.04 to 19.93) and Collegial Nurse-Physician Relations (OR 1.83, 95% CI 1.25 to 2.67). Significant factors associated with job satisfaction were Nurse Manager Ability, Leadership, and Support (OR 1.73, 95% CI 1.15 to 2.62), Participation in Practice Affairs (OR 2.59, 95% CI 1.15 to 5.83), Collegial Nurse-Physician Relations (OR 1.99, 95% CI 1.17 to 3.40), and Staffing and Resource Adequacy (OR 2.23, 95% CO 1.49 to 3.34).
Higher scores on the Safety Organizing Scale – which reflects more frequent performance of safety behaviors – were significantly associated with Foundation for Quality of Care (Beta coefficient 0.64, SE 0.10, p < .001), Participation in Practice Affairs (Beta coefficient 0.18, SE 0.07, p = .01), Collegial Nurse-Physician Relations (Beta coefficient 0.26, SE 0.10, p = .01). Compared with registered nurses, nurse practitioners reported significantly lower scores on the Safety Organizing Scale (Beta coefficient, −0.37, SE 0.16, p = .02).
Variation in Practice Environments and Safety Organizing Behaviors Across Units
The Figure shows the mean scores and corresponding 95% CIs on the Safety Organizing Scale and the PES-NWI composite for DFCI and for all 13 reporting units, which includes the three satellite locations. Substantial variation is observed on both measures across the units. The mean scores on the Safety Organizing Scale across units ranged from 4.35 to 5.70 on a 7-point scale. Unit “M” scored significantly higher on the Safety Organizing Scale than the institutional mean. The unit-level means on the PES-NWI composite ranged from 3.20 to 4.11 on a 5-point scale. Unit “L” scored significantly higher on the PES-NWI composite than the institution mean, while unit “B” scored significantly lower.
Figure.
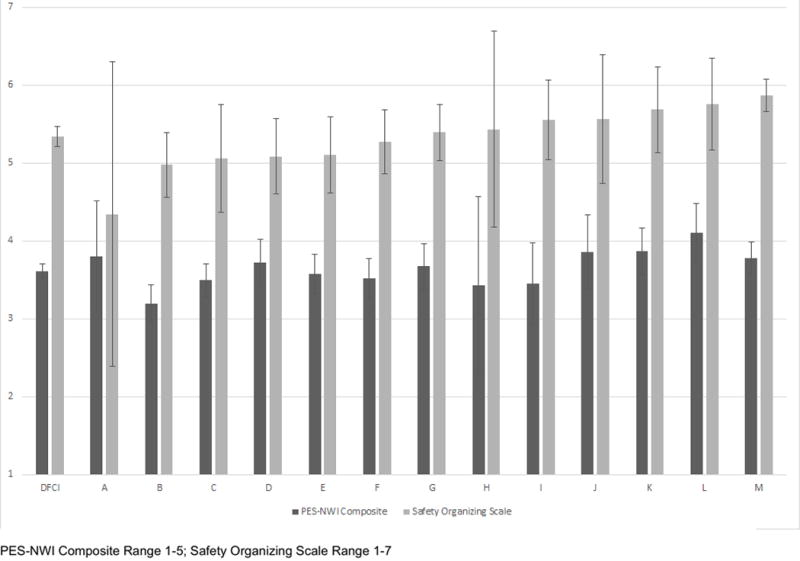
Variation in Safety Organizing Scale and PES-NWI composite scores by unit or satellite. Unit-level means of the PES-NWI composite scale (dark gray) and the Safety Organizing Scale (light gray) are displayed for each unit, with corresponding 95% Confidence Intervals. The first paired columns on the left reflect the mean values for the entire institution. Corresponding units differ significantly from the institutional mean on both the PES-NWI and the Safety Organizing Scale.
DISCUSSION
This study of practice environments, job outcomes, and safety behaviors surveyed all registered nurses employed in a National Cancer Institute-designated Comprehensive Cancer Center. In this sample of direct care and non-direct care nurses, registered nurses, advanced practice nurses, and nursing leaders, the practice environment was favorable. Nurse-reported outcomes, including quality of care, job satisfaction, and intention to leave current position, were similar to those reported in other samples.2–4 Several features of the practice environment were significantly associated with positive outcomes. When these variables were examined across units within the institution, substantial variation occurred. These findings have important implications for the leadership of ambulatory cancer centers.
Favorable reports of collegial nurse-physician relationships were significantly correlated with all four outcomes studied. In context with reported literature, others have confirmed these findings in oncology settings.12 In the previous study,12 nurse-physician relationships were significantly associated with job outcomes for oncology nurses, but not other nursing specialties. While it is reassuring that nurse-physician relationships were rated well across the institution, certain units scored below the midpoint (results not shown). Given this factor’s importance to nurse-reported outcomes, strengthening the relationships between nurse-physician relationships is an important priority. Participation in practice affairs was significantly associated with three outcomes. Prior work has documented the importance of control over work as a key determinant of health care worker job satisfaction and high-functioning teams.13
We did not observe major differences between registered nurses and nurse practitioners. However, the lower scores in the Safety Organizing Scale for nurse practitioners is a new finding. The prior work by Vogus and Sutcliffe focused on registered nurses in inpatient settings.10 In our institution, nurse practitioners often work closely with one or a handful of physicians; rarely do they work closely with other nurse practitioners or registered nurses. It is possible that the work roles assumed by nurse practitioners make them less apt to demonstrate and or depend on these behaviors, such as anticipating potential problems, learning from mistakes, to get their work done effectively. In contract, registered nurses, the majority of whom in our sample administer treatments directly to patients, may need to employ these behaviors on a more frequent basis. However, we continue to converse with our nurse practitioners on ways to increase their teamwork and how to promote behaviors congruent with high reliability organizations.
Unit-level summaries of the data reported here were shared with clinical nurse directors. The summaries report the data distilled to each unit, and compare the unit results with the rest of the institution. We have identified units with more favorable reports and those with less favorable reports. At the institutional level, we have identified participation in practice affairs as the key leadership priority for the next year. Despite having a mature nursing shared governance model in place throughout the organization,14 the findings suggest we have significant room to improve the structure and capacity for nurses and nurse practitioners to be truly engaged and involved in unit and organization level priority setting and decision making. Clinical nurse directors will share the data with their staff and solicit suggestions for improvements. Units that performed well on elements will be asked to share their experiences with others. It is the goal of this work to use the data to drive management changes that support those factors crucial to creating and maintaining an environment that is conducive to the delivery of high quality safe care and promotes high functioning teams in our facility.
LIMITATIONS
There are several important limitations to this initiative. One limitation is the relatively few numbers of responses from nurses in several units, which limits the ability to compare differences within units. The range of respondents per unit was 7–31 nurses. This is due in part to a large variation in unit size and also the decision to enable participants to complete questionnaires without identifying their unit. Fewer respondents may lead to less reliable results in these units. In addition, outcomes from the perspective of patients, other providers, and clinical data were not considered. Correlating these data with patient outcomes is an important next step. The sample demographics may not be consistent with the population of oncology nurses employed in ambulatory settings. Unfortunately, national demographic data on these nurses is not available. These limitations are presented alongside the strengths of a web-based survey with remarkably high response rates and the measures that were assessed favorably for validity and reliability in prior studies.2–4, 10 Importantly, the perspectives of advanced practice nurses and nurses who work outside of direct care roles are included.
CONCLUSIONS AND IMPLICATIONS FOR NURSING PRACTICE
Our institution was motivated to evaluate nurses’ perspectives of their practice environments and safety behaviors to maintain the adequacy of the workforce, support our mission to strengthen professional nursing practice, promote delivery of high quality safe patient care and support data-driven leadership methods. Our work ahead includes boosting nurses’ decision making throughout the institution, supporting positive nurse-physician relationships, and working with units with less favorable scores to strengthen their environments based on their own data. Empirical measurement of the nursing care delivery is a useful technique to prioritize interventions to assure the excellence of patient care.
Acknowledgments
Thank you to Patti Branowicki, Lori Buswell, Anne Gross and the other nursing directors for their support of conducting this survey in their clinical practice settings and to Kara Lacey for her assistance in survey deployment.
Research Support: None
Footnotes
Prior Presentations: None
Disclaimers: None
Contributor Information
Christopher R. Friese, University of Michigan School of Nursing, Ann Arbor, MI.
Mary Lou Siefert, Dana-Farber Cancer Institute, Boston, MA.
Kaitlin Thomas-Frost, Simmons College Department of Nursing Family Nurse Practitioner Program, Boston, MA.
Stacy Walker, Simmons College Department of Nursing Family Nurse Practitioner Program, Boston, MA.
Patricia Reid Ponte, Dana-Farber Cancer Institute, Boston, MA.
References
- 1.Levit L, Smith AP, Benz EJ, et al. Ensuring quality cancer care through the oncology workforce. J Oncol Pract. 2010;6(1):7–11. doi: 10.1200/JOP.091067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friese CR. Practice environments of nurses employed in ambulatory oncology settings: measure refinement. Oncol Nurs Forum. 2012;39(2):166–172. doi: 10.1188/12.ONF.166-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friese CR, Himes-Ferris L, Frasier MN, et al. Structures and processes of care in ambulatory oncology settings and nurse-reported exposure to chemotherapy. BMJ Qual Saf. 2012;21(9):753–759. doi: 10.1136/bmjqs-2011-000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Friese CR, Himes-Ferris L. Nursing practice environments and job outcomes in ambulatory oncology settings. J Nurs Adm. 2013;43(3):149–54. doi: 10.1097/NNA.0b013e318283dc3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Nurses Credentialing Center. Magnet Program Overview. http://www.nursecredentialing.org/Magnet. Accessed October 20, 2014.
- 6.National Database of Nursing Quality Indicators. About NDNQI. http://www.nursingquality.org/About-NDNQI. Accessed October 20, 2014.
- 7.Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2. New York, NY: Wiley and Sons; 2007. [Google Scholar]
- 8.Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 9.Lake ET. Advances in understanding and predicting nurse turnover. Res Sociol Health Care. 1998;15:147–171. [Google Scholar]
- 10.Vogus TJ, Sutcliffe KM. The Safety Organizing Scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007;45(1):46–54. doi: 10.1097/01.mlr.0000244635.61178.7a. [DOI] [PubMed] [Google Scholar]
- 11.Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Heal. 2002;25(3):176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 12.Friese CR. Nurse practice environments and outcomes: Implications for oncology nursing. Oncol Nurs Forum. 2005;32(4):765–772. doi: 10.1188/05.ONF.765-772. [DOI] [PubMed] [Google Scholar]
- 13.Bunnell CA, Gross AH, Weingart SN, et al. High performance teamwork training and systems redesign in outpatient oncology. BMJ Qual Saf. 2013;22(5):405–413. doi: 10.1136/bmjqs-2012-000948. [DOI] [PubMed] [Google Scholar]
- 14.Ponte P, Gross A, Winer E, Connaughton M, Hassinger J. Implementing an interdisciplinary governance model in a comprehensive cancer center. Oncol Nurs Forum. 2007;34(3):611–616. doi: 10.1188/07.ONF.611-616. [DOI] [PubMed] [Google Scholar]


