Abstract
Background
Adults with intellectual disabilities have increased early mortality compared with the general population. However, their extent of multimorbidity (two or more additional conditions) compared with the general population is unknown, particularly with regards to physical ill-health, as are associations between comorbidities, neighbourhood deprivation, and age.
Methods
We analysed primary health-care data on 1,424,378 adults registered with 314 representative Scottish practices. Data on intellectual disabilities, 32 physical, and six mental health conditions were extracted. We generated standardised prevalence rates by age-groups, gender, and neighbourhood deprivation, then calculated odds ratio (OR) and 95 % confidence intervals (95 % CI) for adults with intellectual disabilities compared to those without, for the prevalence, and number of condition.
Results
Eight thousand fourteen (0.56 %) had intellectual disabilities, of whom only 31.8 % had no other conditions compared to 51.6 % without intellectual disabilities (OR 0.26, 95 % 0.25–0.27). The intellectual disabilities group were significantly more likely to have more conditions, with the biggest difference found for three conditions (10.9 % versus 6.8 %; OR 2.28, 95 % CI 2.10–2.46). Fourteen physical conditions were significantly more prevalent, and four cardiovascular conditions occurred less frequently, as did any cancers, and chronic obstructive pulmonary diseases. Five of the six mental health conditions were significantly more prevalent. For the adults with intellectual disabilities, no gradient was seen in extent of multimorbidity with increasing neighbourhood deprivation; indeed findings were similar in the most affluent and most deprived areas. Co-morbidity increased with age but is highly prevalent at all ages, being similar at age 20–25 to 50–54 year olds in the general population.
Conclusions
Multi-morbidity burden is greater, occurs at much earlier age, and the profile of health conditions differs, for adults with intellectual disabilities compared with the general population. There is no association with neighbourhood deprivation; people with intellectual disabilities need focussed services irrespective of where they live, and at a much earlier age than the general population. They require specific initiatives to reduce inequalities.
Electronic supplementary material
The online version of this article (doi:10.1186/s12875-015-0329-3) contains supplementary material, which is available to authorized users.
Keywords: Intellectual disabilities, Mental retardation, Multi-morbidity, Physical health, Mental health, Inequalities, Deprivation
Background
Adults with intellectual disabilities are thought to experience health inequalities and earlier age of death compared with the general population [1]. However, there is little reported information on their wider experience of multimorbidity/comorbidity (two or more conditions additional to the intellectual disabilities) in this population across the adult lifespan. Comorbidity is clinically important, as it may require a different management approach to the care of an individual disease, and may introduce pharmacological contraindications. There is increasing awareness of its clinical importance, due to the relatively recent studies of multi-morbidity in the general population showing that it starts to become more common over the age of 50 and increases in the elderly [2]. In people with intellectual disabilities, rates of individual disorders have been previously reported, for example, a point-prevalence of 40 % for additional mental ill-health [3], 30 % for epilepsy [4], and 50 % for gastro-oesophageal reflux disorder [5]. This might suggest that multi-morbidity would be a particular problem for this population, but we have only been able to find two previous studies on the topic, both of which were focussed only on older people with intellectual disabilities [6, 7]. Both reported high rates of multimorbidity/comorbidity; 71 % in 695 older persons with intellectual disabilities [6], and 80 % in 1047 older persons receiving paid support [7]. These studies did not drawn direct comparisons with rates in the general population living in the same areas, nor at the same age.
The extent of multimorbidity is higher in the general population living in more deprived neighbourhoods [2]. It is therefore important to examine if this is also true for people with intellectual disabilities, since this would indicate higher needs in this population which may need specific organisation to meet. Both children and adults with intellectual disabilities are more likely to live in more deprived areas [8–11]. However, the impact this has on their health and health care has been little studied [10].
This study was undertaken to quantify the extent of recorded ill-health and comorbidity experienced by adults with intellectual disabilities compared with the general population, and to measure the associations between neighbourhood deprivation, age, and comorbidity in adults with intellectual disabilities.
Methods
We used data from the Primary Care Clinical Informatics Unit at the University of Aberdeen for all 1,424,378 registered patients aged 18 and over, who were alive and permanently registered with one of 314 Scottish general practices on March 31, 2007 [12]. The dataset is representative of the whole Scottish population in terms of age, sex, and socioeconomic deprivation, with a more detailed explanation available elsewhere [2].
Data on the presence of intellectual disabilities, 32 common chronic physical health conditions and six mental health conditions were extracted (definitions are provided in Additional file 1: Appendix 1). We defined intellectual disabilities using a set of Read Codes based on definitions used by NHS Scotland Information Services and from the Quality & Outcomes Framework (Additional file 1: Appendix 2).
Neighbourhood deprivation was measured using the Carstairs deprivation score divided into quintiles (from most affluent to most deprived) [13]. The Carstairs score is based on postcode of residence and is widely used in healthcare research as a measure of socioeconomic status.
To control for differences between the two populations in age, gender and deprivation levels we adopted a similar approach to that undertaken in previous papers [14, 15] and generated standardised prevalence rates by age groups (18 to 24 years; 25 to 34; 35 to 44; 45 to 54; 55 to 64; 65 to 74 and 75 and over), gender, and deprivation quintile using the direct method. These age-gender-deprivation standardised rates were then used to calculate odds ratio (ORs) and 95 % confidence intervals (95 % CI) for the adults with intellectual disabilities compared to those without (controls), for the prevalence of 32 physical conditions and six mental health conditions, as well as by the number of overall conditions and the number of physical and mental health conditions.
We report by age group and gender, differences between those with and without intellectual disabilities in the percentage of individuals with two or more physical conditions and two or more mental health conditions. We used t tests to analyse differences between groups and one-way analysis of variance for differences across age groups and deprivation quintiles. For all statistical analyses, a p-value less than 0 · 05 was considered statistically significant. All analyses were performed in Stata version 13.
We also compared the extent of monitoring of blood pressure in the over 50 years with and without intellectual disabilities to see if there were any monitoring/recording differences. Blood pressure measurement is routinely conducted in practices at this age.
The NHS Grampian Research Ethics Service approved the anonymous use of these data for research purposes.
Results
Demographics
There were 8014 (0.56 % of the sample) patients with a Read Code for intellectual disabilities recorded (Table 1). This is similar to previously reported prevalence rates from another area of Scotland where there was rigorous checking of the population [2]. Men were over-represented in the intellectual disabilities group compared to controls (56.4 vs. 49.1 % for controls; p < 0.001). Individuals with recorded intellectual disabilities were on average younger (mean age 43.1 vs. 48.0 years for controls; p < 0.001), with only 11.4 % aged 65 or over compared to 20.6 % of controls. The adults with intellectual disabilities were also more likely to live in areas of high social deprivation, with just over a quarter (25.3 %) with intellectual disabilities resident in the most deprived quintile of postcodes compared to 17.8 % of controls (p < 0.001).
Table 1.
Age, gender, and deprivation status, intellectual disabilities versus controls
| Variable | Intellectual disabilities | No intellectual disabilities |
|---|---|---|
| Number (%) | Number (%) | |
| Total (%) | 8014 (0.6 %) | 1,416,364 (99.4 %) |
| Gender (% male) | 4518 (56.4 %) | 694,911 (49.1 %) |
| Mean Age (sd) | 43.1 (15.8) | 48.0 (18.3) |
| Age group | ||
| 18–24 | 1192 (14.9) | 150,501 (10.6) |
| 25–34 | 1419 (17.7) | 227,977 (16.1) |
| 35–44 | 1811 (22.6) | 277,182 (19.6) |
| 45–54 | 1639 (20.5) | 252,155 (17.8) |
| 55–64 | 1116 (13.9) | 218,217 (15.4) |
| 65–74 | 593 (7.4) | 154,687 (10.9) |
| 75 and above | 244 (3.0) | 135,645 (9.6) |
| Deprivation Quintile | ||
| Least Deprived | 959 (11.9) | 271,070 (19.1) |
| 2 | 1421 (17.7) | 302,733 (21.4) |
| 3 | 1849 (23.0) | 320,398 (22.6) |
| 4 | 1757 (21.9) | 269,627 (19.0) |
| Most Deprived | 2028 (25.3) | 252,536 (17.8) |
All difference significant at p < 0.001
Comorbidities
Overall, 31.8 % of individuals with intellectual disabilities had no other conditions compared to 51.6 % of controls with no recorded condition (Table 2). The intellectual disabilities group were significantly more likely to have more of all the specified number of conditions after standardising for age, sex and social deprivation, with the smallest difference found for one condition (intellectual disabilities 27.5 % vs. controls 21.3 %; OR 1.48, 95 % CI 1.41–1.55), and the biggest difference found for three conditions (intellectual disabilities 10.9 % vs. controls 6.8; OR 2.28, 95 % (CI 2.10–2.46) (Table 2).
Table 2.
Prevalence and odds ratio for number and type of comorbidities (standardised by age, gender, and deprivation score)
| Intellectual disabilities | No Intellectual disabilities | Odds ratio (95 % CI) (standardised by age, gender and deprivation) | |
|---|---|---|---|
| N (prevalence %) | N (prevalence %) | ||
| N = 8014 (0.6 %) | N = 1,416,364 (99.4 %) | ||
| Total number of morbiditiesa | |||
| None | 2552 (31.8) | 731,181 (51.6) | 0.26 (0.25–0.27) |
| One | 2207 (27.5) | 301,743 (21.3) | 1.48 (1.41–1.55) |
| Two | 1498 (18.7) | 162,371 (11.5) | 2.13 (1.99–2.26) |
| Three | 874 (10.9) | 96,256 (6.8) | 2.28 (2.10–2.46) |
| Four | 471 (5.9) | 57,231 (4.0) | 2.07 (1.87–2.29) |
| Five or more | 412 (5.1) | 67,582 (4.8) | 1.60 (1.44–1.79) |
| Total number of physical conditions | |||
| None | 3087 (38.5) | 799,884 (56.5) | 0.27 (0.25–0.29) |
| One | 2397 (29.9) | 294,613 (20.8) | 1.79 (1.71–1.80) |
| Two | 1428 (17.8) | 149,477 (10.5) | 2.50 (2.34–2.66) |
| Three | 631 (7.9) | 83,016 (5.9) | 1.96 (1.79–2.15) |
| Four | 309 (3.9) | 45,587 (3.3) | 1.76 (1.56–1.99) |
| Five or more | 162 (2.0) | 43,787 (3.1) | 0.95 (0.81–1.12) p = 0.59 |
| Total number of mental health conditionsa | |||
| None | 5878 (73.4) | 1,205,242 (85.1) | 0.42 (0.40–0.44) |
| One | 1577 (19.7) | 160,958 (11.4) | 2.10 (1.99–2.23) |
| Two | 471 (5.9) | 43,232 (3.1) | 2.26 (2.05–2.48) |
| Three or more | 88 (1.1) | 6932 (0.5) | 2.43 (1.96–3.00) |
One-way analysis of variance
All difference significant at p < 0.001 except where marked
aExcluding intellectual disabilities
When restricting analysis only to physical health comorbidities the adults with intellectual disabilities were far less likely to have no physical conditions (intellectual disabilities 38.5 % vs. controls 56.5 %; OR 0.27, 95 % CI 0.25–0.29) and more likely to have one to four physical conditions, with the biggest difference found for two physical conditions (intellectual disabilities 17.8 % vs. controls 10.5 %; OR 2.50, 95 % CI 2.34–2.66), but there were no differences found for five or more conditions.
People with intellectual disabilities were less likely to have no recorded mental health condition compared to controls (intellectual disabilities 73.4 % vs. controls 85.1 %; OR 0.42, 95 % CI 0.40–0.44) and twice as likely to have one, two and three or more mental health conditions, than people with no intellectual disabilities.
Physical health individual conditions
For the intellectual disabilities group, 14 out of 32 physical conditions were significantly more prevalent relative to controls, 11 were significantly less prevalent, with 7 conditions showing no significant differences (Table 3). The largest differences, after standardisation for age, sex and deprivation, were for epilepsy (OR 31.03, 95 % CI 29.23–32.92) constipation (OR 11.19, 95 % CI 10.97–12.68) and visual impairment (OR 7.81, 95 % CI 6.86–8.89). Five further conditions were more than twice as likely to be prevalent in those with intellectual disabilities compared to controls (hearing loss, eczema, dyspepsia, thyroid disorders and Parkinson’s Disease or Parkinsonism). Of the eleven conditions for which the relative prevalence for the adults with intellectual disabilities was lower, four were cardiovascular related (coronary heart disease OR 0.43, 95 % CI 0.37–0.51, peripheral vascular disease OR 0.44, 95 % CI 0.33–0.60, hypertension OR 0.72, 95 % CI 0.66–0.78 and atrial fibrillation OR 0.83, 95 % CI 0.61–0.98). Lower prevalence in those with intellectual disabilities also included any cancer over the last 5 years (OR 0.69, 95 % CI 0.58–0.83) and chronic obstructive pulmonary diseases (OR 0.84, 95 % CI 0.73–0.97).
Table 3.
Actual prevalence rates, and standardised odds ratios for individual physical conditions. Conditions are ordered by size of standardised odds ratio (largest to smallest)
| Condition | Intellectual disabilities | No Intellectual disabilities | Odds ratio (95 % CI) (standardised by age, gender and deprivation score) |
|---|---|---|---|
| Number (%) | Number (%) | ||
| Epilepsy | 1508 (18.8) | 10,876 (0.8) | 31.03 (29.23–32.92) |
| Constipation | 1118 (14.0) | 35,298 (2.5) | 11.19 (10.97–12.68) |
| Visual impairment | 258 (3.2) | 8120 (0.6) | 7.81 (6.86–8.89) |
| Parkinson’s disease and Parkinsonism | 28 (0.4) | 2713 (0.2) | 2.83 (1.95–4.13) |
| Hearing loss | 657 (8.2) | 54,077 (3.8) | 2.81 (2.59–3.06) |
| Dyspepsia | 822 (10.3) | 78,382 (5.5) | 2.46 (2.28–2.65) |
| Psoriasis or eczema | 132 (1.7) | 10,237 (0.7) | 2.42 (2.03–2.87) |
| Thyrotoxicosis/thyroid disorders inc hypothyroidism | 629 (7.9) | 71,314 (5.0) | 2.36 (2.173–2.58) |
| Bronchiectasis | 20 (0.3) | 2794 (0.2) | 1.68 (1.08–2.61) p = 0.02 |
| Diabetes | 531 (6.6) | 74,300 (5.3) | 1.63 (1.49–1.79) |
| Migraine | 59 (0.7) | 9192 (0.7) | 1.32 (1.02–1.71) p = 0.03 |
| Active asthma | 575 (7.2) | 83,930 (5.9) | 1.26 (1.16–1.38) |
| Painful condition | 695 (8.7) | 125,436 (8.9) | 1.20 (1.10–1.30) |
| Stroke or transient ischaemic attack | 171 (2.1) | 36,374 (2.6) | 1.19 (1.02–1.37) p = 0.02 |
| Glaucoma | 72 (0.9) | 15,847 (1.1) | 1.17 (0.92–1.48) p = 0.18 |
| Chronic kidney disease | 135 (1.7) | 33,431 (2.4) | 1.11 (0.93–1.32) p = 0.22 |
| Heart failure | 82 (1.0) | 18,817 (1.3) | 1.11 (0.89–1.43) p = 0.33 |
| Irritable bowel syndrome | 248 (3.1) | 51,889 (5.7) | 0.97 (0.86–1.11) p = 0.74 |
| Chronic obstructive pulmonary diseases (COPD) | 209 (2.6) | 52,898 (3.7) | 0.84 (0.73–0.97) |
| Atrial fibrillation | 71 (0.9) | 23,905 (1.7) | 0.83 (0.61–0.98) p = 0.03 |
| Viral hepatitis | 7 (0.1) | 1168 (0.1) | 0.82 (0.39–1.74) p = 0.62 |
| Inflammatory bowel disease | 40 (0.5) | 9711 (0.7) | 0.82 (0.60–1.13) p = 0.23 |
| Hypertension | 774 (9.7) | 233,540 (16.5) | 0.72 (0.66–0.78) |
| Any new cancer in the last 5 years | 131 (1.6) | 43,533 (3.1) | 0.69 (0.58–0.83) |
| Prostate disease | 41 (0.5) | 15,192 (1.1) | 0.60 (0.44–0.82) p = 0.01 |
| Inflammatory arthritis and related conditions inc gout | 151 (2.2) | 57,857 (4.1) | 0.57 (0.48–0.67) |
| Cirrhosis/chronic liver disease/alcoholic liver disease | 7 (0.1) | 2605 (0.2) | 0.49 (0.23–1.04) p = 0.06 |
| Multiple sclerosis | 9 (0.1) | 3838 (0.3) | 0.49 (0.25–0.96) p = 0.03 |
| Diverticular disease | 66 (0.8) | 33,747 (2.4) | 0.49 (0.39–0.63) |
| Peripheral vascular disease (PVD) | 46 (0.7) | 23,194 (1.6) | 0.44 (0.33–0.60) |
| Chronic sinusitis | 24 (0.3) | 9141 (0.6) | 0.44 (0.26–0.62) |
| Coronary heart disease | 160 (2.0) | 81,307 (5.7) | 0.43 (0.37–0.51) |
One way analysis of variance
All differences significant at p < 0.001 except where stated
Mental health conditions
Table 4 highlights that the adults with intellectual disabilities had significantly higher prevalence for five of the mental health conditions with no significant difference found for anorexia/bulimia. The biggest difference after standardisation for age, sex and deprivation was for schizophrenia/bipolar (OR 7.16, 95 % CI 6.49–7.89), followed by anxiety (OR 2.62, 95 % CI 2.41–2.84). The highest prevalence for a mental health condition was found for depression with prevalence 15.8 % for those with intellectual disabilities compared to 10.1 % of controls (OR 1.88, 95 % CI 1.76–2.00). (The lower prevalence of dementia in the raw data is because the proportion of people with intellectual disabilities who have dementia is small, given the age distribution of people with intellectual disabilities. However the OR is standardized for age, and so reflects the fact that people with intellectual disabilities, particularly Down syndrome, experience dementia at a much earlier age than the general population.)
Table 4.
Prevalence and odds ratios for individual mental health conditions (standardised by age, gender, and deprivation score). Conditions are ordered by size of odds ratio (largest to smallest)
| Condition | Intellectual disabilities | No Intellectual disabilities | Odds ratio (95 % CI) (standardised by age, gender and deprivation) |
|---|---|---|---|
| total number (prevalence) | total number (prevalence) | ||
| Schizophrenia (and related non-organic psychosis) or bipolar disorder | 448 (5.6) | 12,045 (0.9) | 7.16 (6.49–7.89) |
| Anxiety & other neurotic, stress related & somatoform disorders | 649 (8.1) | 55,077 (3.9) | 2.62 (2.41–2.84) |
| Dementia | 84 (0.8) | 11,612 (1.1) | 2.22 (1.78–2.77) |
| Depression | 1267 (15.8) | 142,676 (10.1) | 1.88 (1.76–2.00) |
| Anorexia or bulimia | 37 (0.5) | 5269 (0.4) | 1.31 (0.95–1.82) p = 0.09 |
| Alcohol misuse | 304 (3.8) | 42,060 (3.0) | 1.18 (1.05–1.33) |
One way analysis of variance
All difference significant at p < 0.001 except where stated
Effect of deprivation
Figure 1 shows the percentage of individuals with two or more physical conditions and two or more mental health conditions by deprivation quintile after age and sex standardisation. Prevalence is higher in the intellectual disabilities group for both physical and mental health conditions across all quintiles. A clear gradient is seen for the general population in whom the percentage with two or more conditions increases as the extent of neighbourhood deprivation increases. No such gradient is seen for the adults with intellectual disabilities; indeed the proportion with two or more physical health conditions, or two or more mental health conditions, is similar in both the most affluent and most deprived areas.
Fig. 1.
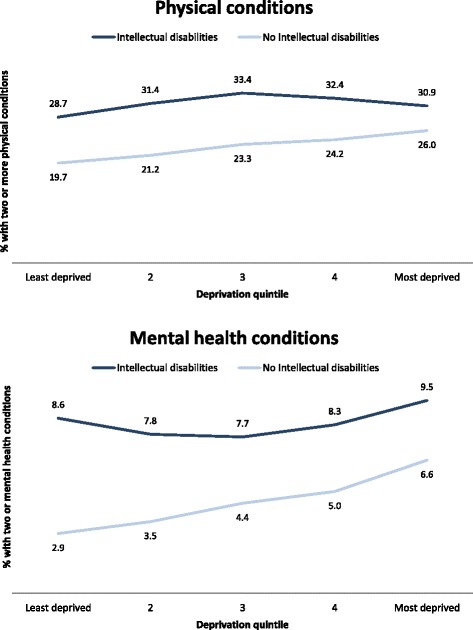
Proportion of people with two or more physical conditions, and two or more mental health conditions (excluding intellectual disabilities) by deprivation quintile (standardised by age and sex)
Effect of age and gender
Figure 2 shows the percentage of individuals with two or more physical conditions by age group and gender after standardisation by deprivation. Prevalence is higher in the intellectual disabilities group for both men and women for all age groups with the exception of those aged 75 and above for males. Differences peak at 45–49 for males and 50–54 for females. Women have higher rates for both groups across all ages. In the adults with intellectual disabilities, co-morbidity increased with age but is highly prevalent at all ages, with its extent at age 20–25 being similar to that of 50–54 year olds in the general population.
Fig. 2.
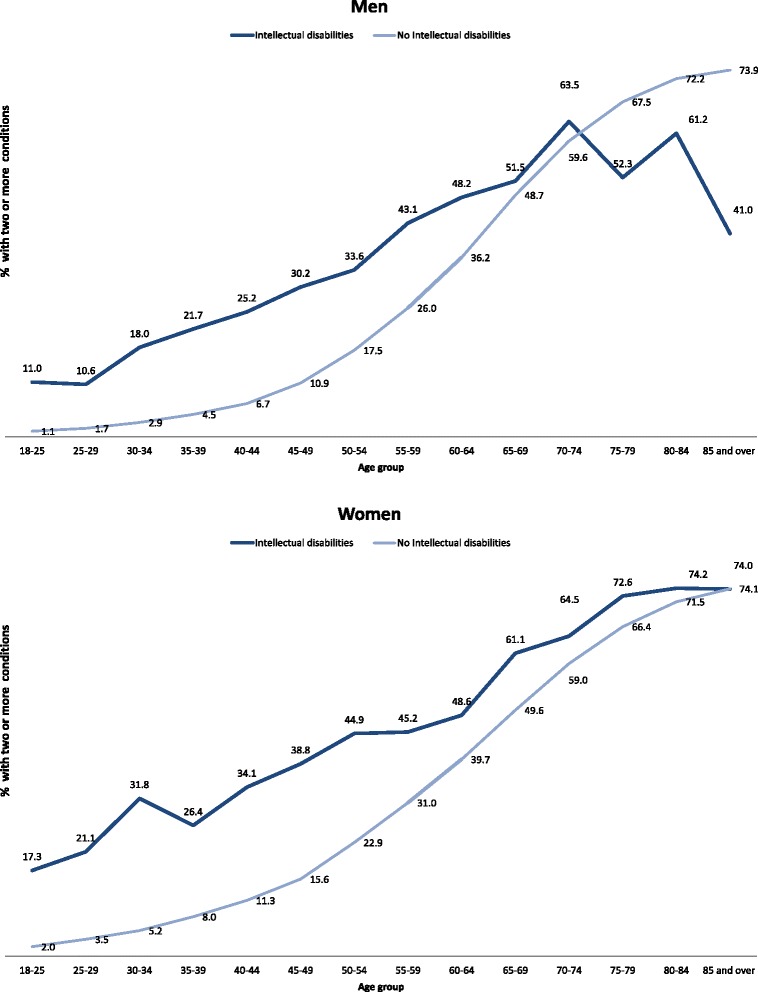
Proportion of people with two or more physical conditions by gender and age group (standardised by deprivation)
Figure 3 shows the percentage of individuals with two or more mental health conditions by age group and gender, after standardisation by deprivation. A similar trend was found as with physical conditions, with prevalence consistently higher in the intellectual disabilities group for both men and women, and higher rates in women for both groups across all ages.
Fig. 3.
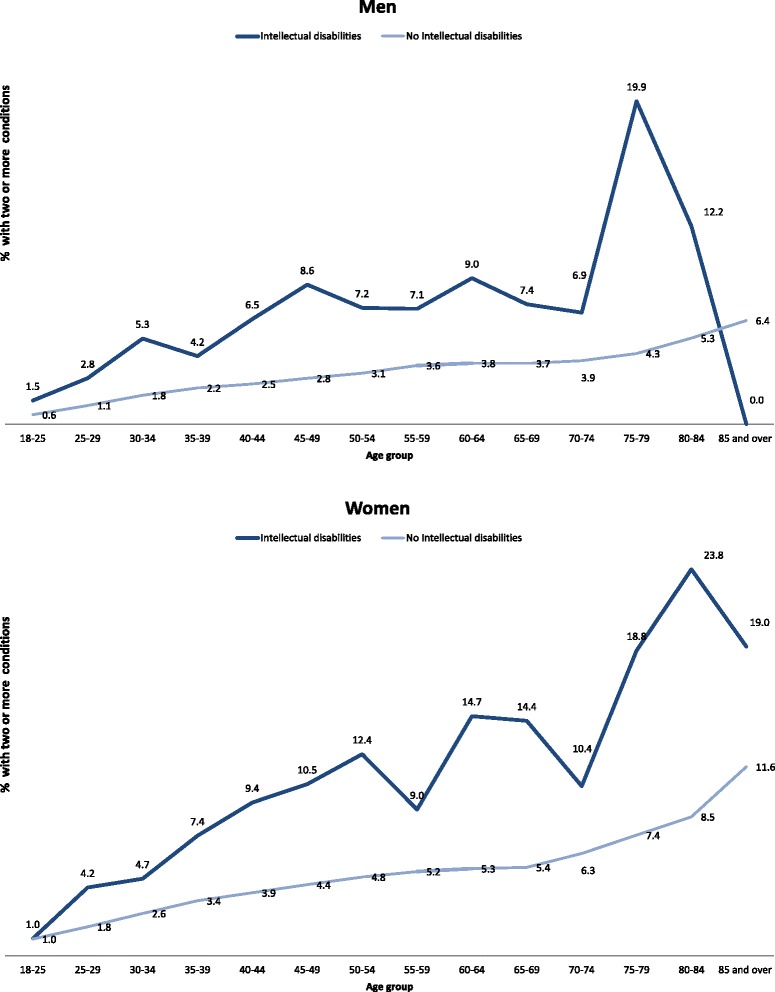
Proportion of people with two or more mental health conditions by gender and age group (standardised by deprivation)
Monitoring/recording
There was no difference in blood pressure monitoring in our population; 83.3 % of the people with intellectual disabilities aged 50 and over had a blood pressure recorded in the previous three years compared to 84.9 % of those without intellectual disabilities.
Discussion
Key results
The extent of multi-morbidity experienced by adults with intellectual disabilities, and its direct comparison with the general population, is a novel and important finding, with implications for services, including the age at which they are likely to be needed. Consequently, any policy initiatives or guidelines on multi-morbidity need to be relevant at a much earlier age in people with intellectual disabilities. This difference has not been previously reported. Morbidity burden and multimorbidity is higher in the population with intellectual disabilities than in the general population, due to higher rates of some physical conditions, for example epilepsy, gastro-intestinal disorders, and sensory impairments, and higher rates of a range of mental health conditions. Whereas multi-morbidity is common in the general population only in older age groups, particularly those aged 50–54 and older, it is common in all age groups in adults with intellectual disabilities. The pattern of disease also differs from the general population with some conditions being less common, such as cardiovascular disease. Additionally, prevalence of multi-morbidity did not follow the typical gradient seen in the general population across areas of increasing neighbourhood deprivation, importantly highlighting that services are equally needed in all areas.
Two previous studies from the Netherlands and Ireland have reported high rates of multimorbidity in older people with intellectual disabilities [6, 7], and we also found this, and extended this finding down the age range to all adults with intellectual disabilities.
Strengths and limitations
Scottish GP practices have held a register of people with intellectual disabilities since a change in their contract introducing pay-for-performance, which precedes the data extraction this study used. Intellectual disability is a lifetime diagnosis, and once coded at birth or in childhood this remains on the medical record indefinitely. The sample with intellectual disabilities appears to be representative, and benefits from its very large size. As expected, compared with people without intellectual disabilities, there were more men, they were younger, and they were more likely to live in deprived areas. Rates of morbidity were compared with the general population registered at the same general practices, and standardised by age, gender, and neighbourhood deprivation. It is possible that some people with intellectual disabilities were not coded as such, for example people with Down syndrome, however the prevalence of the population identified is similar to that reported for adults with intellectual disabilities in a recent meta-analysis of prevalence studies (0.5 %) [16], and the odds ratio for dementia for the intellectual disabilities group compared with the general population suggests people with Down syndrome, who have dementia at a much earlier age than the general public, were included.
There may be under-reporting of health conditions in the population with intellectual disabilities. This may be so for conditions that are not overtly obvious to paid carers, or where carers attribute the effects of conditions to other reasons. The similarity in extent of blood pressure recording in the population with intellectual disabilities compared with the general population is reassuring in this regard. If there was under-reporting, then the difference between the two groups would be even more marked than that we report, and the key message of our paper still stands i.e. that multi-morbidity is markedly more common in adults with intellectual disabilities than in the general population, and occurs at a much younger age.
Problem behaviours, which occur in 22.5 % of adults with intellectual disabilities [17] were not included in the study, due to the lack of suitable Read codes for these disorders, hampering their recording/consistent recording. Comparable problem behaviours are rare in the general population, hence the extent of the difference in multimorbidity would have been greater if these could have been included. We also did not include autism and attention deficit hyperactivity disorder, both of which are known to be more common in people with intellectual disabilities than in the general population. Conditions are coded during routine health care, including primary care encounters and based on letters from secondary care, and there could be some variation between practices.
We do not have information on type of accommodation/support the people with intellectual disabilities had.
Interpretation of findings
Some causes of intellectual disabilities also cause physical and/or mental ill-health, for example Down syndrome is associated with thyroid disorder and sensory impairments; however, Down syndrome accounts for only about 15 % of the population with intellectual disabilities. Adults with intellectual disabilities are also more likely to lead sedentary lives and not exercise [18], have more mobility problems [19], obesity [20], and are less likely to eat healthily [21] than the general public, and about a quarter take antipsychotic drugs [22], which may contribute to some of these conditions. They are also more likely to be prescribed multiple drugs, which can adversely affect health through side-effects and drug interactions [21]. They do not always have the knowledge or understanding to make healthy choices, and are reliant on others for support and communication. These issues are often compounded by difficulties accessing the health services they need.
Eleven of the conditions were recorded statistically less commonly in adults with intellectual disabilities than in the general population. The lower rates of smoking and alcohol use among the population with intellectual disability may well account for several of these conditions being diagnosed at a lower frequency, particularly cardiovascular disease and chronic obstructive pulmonary disease. The majority of adults with intellectual disabilities do not drink alcohol at all, although some do misuse it, and at a slightly higher rate than the general population in this study.
Despite the higher prevalence of comorbidity experienced by the adults with intellectual disabilities, the extent of their morbidities may be under-recorded. Mental and physical health conditions may be unrecognised, under-investigated and untreated [23–26], with ill-heath presenting late, at more severe stages of disease progression which may be less responsive to treatment. Chronic disease monitoring is also less well addressed [27, 28]. Several factors are implicated, such as limited verbal communication skills, impaired mobility, and problem behaviours. People with intellectual disabilities are reliant on carers recognising they may have a problem and seeking help, and dependent upon carers communicating effectively within the team, and indeed across care teams (e.g. day care team and home care team). Sometimes, health conditions are misattributed by paid carers or health professionals as being part of the adult’s intellectual disabilities (diagnostic overshadowing), and not addressed for this reason. These problems are compounded across the entire lifecourse, rather than just being due to communication problems in late life.
The apparent drop-off in the rate of multimorbidity in men aged 75 and older is likely to be a reflection of the very small numbers in these age groups. Most people with intellectual disabilities do not live to such old ages [29, 30], so these individuals are the “healthy survivors”. Older people with intellectual disabilities typically have milder intellectual disabilities than those who die earlier, and people with milder intellectual disabilities are likely to have fewer health problems than people with more severe intellectual disabilities. Of the total of 4518 men with intellectual disabilities in the study, there were only 60 (1.32 %) aged 75–79, 32 (0.71 %) aged 80–84, and 16 (0.35 %) aged 85 or older. This compares with 24,831 (3.57 %) aged 75–79 out of the total of 694,911 men without intellectual disabilities, 15,921 (2.29 %) aged 80–84, and 11,017 (1.59 %) aged 85 or older.
The lack of association between neighbourhood deprivation and multimorbidity in this population is likely to be due to area based measures of deprivation not accurately reflecting the relative degree of affluence or poverty experienced by people with intellectual disabilities, in the face of the extensive difficulties they have to cope with in life. Many adults with intellectual disabilities are not integrated within their communities. They do not necessarily have shared values and lifestyles with their local community. Rented accommodation in which adults with intellectual disabilities are placed with individual tenancies, or shared tenancies with other adults with intellectual disabilities, tend to be in less affluent areas. One can speculate that their paid carers are more likely to live in the local area, but the adult may still have regular contact with family, whom they grew up with and who may have different levels of affluence and lifestyles compared to the area their adult child with intellectual disabilities now lives in. The interaction of these factors is likely to be complex. Additionally, some of the more congregate care style of housing is more likely to be in affluent areas where there are larger houses; but large group living can result in less individual time from paid carers who are shared by several adults, and less time for community integration. Very few adults with intellectual disabilities have paid employment, so are likely to be of low socio-economic status, and dependant on state benefits, regardless of the area they live in.
Generalisability of findings
The broader dataset is representative of the Scottish population in terms of age, sex, and deprivation [12]. Intellectual disabilities was found in 0.56 % of the sample. This is slightly higher than the 0.5 % recorded in GP registers for pay-for-performance, reflecting that we used a somewhat broader set of Read Codes (http://www.isdscotland.org/Health-Topics/General-Practice/Quality-And-Outcomes-Framework/ Accessed 23.12.14.). As expected, there were more men than women with intellectual disabilities (as more boys than girls are born with intellectual disabilities), a smaller proportion at older age groups than in the general population (due to premature death [29, 30]), and more lived in areas of neighbourhood deprivation. This suggests that the sample with intellectual disabilities is representative of the Scottish population, and hence that these findings are generalisable.
Conclusions
This study is important as it demonstrates, in a very large cohort, the increased burden of multi-morbidity experienced by adults with intellectual disabilities compared with the general population, and with much earlier age of onset. Their extent of co-morbidity at age 20–25 is similar to that of the general population aged 50–54. Additionally, their profile of health conditions differs from the general population and does not have the same associations with neighbourhood deprivation. There may also be under-recording of some conditions due to access difficulties, including carers not recognising problems nor seeking health care, and conditions not being diagnosed or managed appropriately [30]. The implication is that policy initiatives to benefit the majority of the population (i.e. the general population) are unlikely to equally benefit the population with intellectual disabilities, despite their greater overall morbidity. Examples include focussing initiatives and resources in areas of greatest neighbourhood deprivation, and smoking cessation programmes. Assumptions about people with intellectual disabilities’ health profiles and determinants of health cannot necessarily be drawn from the general population. Reducing the health inequality gap will require specific initiatives for adults with intellectual disabilities, and we have demonstrated that people with intellectual disabilities need focussed services irrespective of where they live, and from an early age. This presents challenges for primary care, and highlights a potentially key role for paid carers in supporting access to and across services.
Acknowledgements
The data contained herein were provided by the Primary Care Clinical Informatics Unit (PCCIU) at the University of Aberdeen. The views in this publication are not necessarily the views of the University of Aberdeen, its agents, or employees. The original study which created the data was funded by Scottish Government Chief Scientist Office Applied Research Programme Grant 07/01.
Abbreviations
- CI
Confidence intervals
- NHS
National Health Service
- OR
Odds ratio
Additional file
Appendix 1: Data dictionary. Appendix 2: Read Codes used to define the presence of intellectual disability (DOCX 21 kb)
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
S-AC conceived the study and planned it with FS, SM and JM. GMcL carried out the analysis with support from AMcC. SM and BG conceived and conducted the original study which created the data used in this analysis. All authors were involved in drafting the manuscript or revising it critically for important intellectual content. S-AC is the guarantor. All authors read and approved the final manuscript.
Contributor Information
Sally-Ann Cooper, Email: Sally-Ann.Cooper@Glasgow.ac.uk.
Gary McLean, Email: Gary.McLean@Glasgow.ac.uk.
Bruce Guthrie, Email: B.Guthrie@Dundee.ac.uk.
Alex McConnachie, Email: Alex.McConnachie@Glasgow.ac.uk.
Stewart Mercer, Email: Stewart.Mercer@Glasgow.ac.uk.
Frank Sullivan, Email: Frank.sullivan@nygh.on.ca.
Jill Morrison, Email: Jill.Morrison@Glasgow.ac.uk.
References
- 1.NHS Health Scotland . People with Learning Disabilities in Scotland: The Health Needs Assessment Report. Scotland, Glasgow: NHS; 2004. [Google Scholar]
- 2.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 3.Cooper S-A, Smiley E, Morrison J, Allan L, Williamson A. Prevalence of and associations with mental ill-health in adults with intellectual disabilities. Br J Psychiatr. 2007;190:27–35. doi: 10.1192/bjp.bp.106.022483. [DOI] [PubMed] [Google Scholar]
- 4.Airaksinen EM, Matilainen R, Mononen T, Mustonen K, Partanen J, Jokela V, Halonen P. A population-based study on epilepsy in mentally retarded children. Epilepsia. 2000;4:1214–20. doi: 10.1111/j.1528-1157.2000.tb00328.x. [DOI] [PubMed] [Google Scholar]
- 5.Böhmer CJ, Niezen-de Boer MC, Klinkenberg-Knol EC, Deville WL, Nadorp JH, Meuwissen SG. The prevalence of gastroesophageal reflux disease in institutionalized intellectually disabled individuals. Am J Gastroenterol. 1999;94:804–10. doi: 10.1111/j.1572-0241.1999.00854.x. [DOI] [PubMed] [Google Scholar]
- 6.McCarron M, Swinburne J, Burke E, McGlinchey E, Carroll R, McCallion P. Patterns of multimorbidity in an older population of persons with an intellectual disability: results from the intellectual disability supplement to the Irish longitudinal study on aging (IDS-TILDA) Res Development Disabilit. 2013;34:521–7. doi: 10.1016/j.ridd.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 7.Hermans H, Evenhuis HM. Multimorbidity in older adults with intellectual disabilities. Res Development Disabilit. 2014;35:776–83. doi: 10.1016/j.ridd.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 8.Emerson E, Graham H, Hatton C. Household income and health status in children and adolescents in Britain. European J Public Health. 2006;16:354–60. doi: 10.1093/eurpub/cki200. [DOI] [PubMed] [Google Scholar]
- 9.Leonard H, Petterson B, De Klerk N, Zubrick SR, Glasson E, Sanders R, Bower C. Association of sociodemographic characteristics of children with intellectual disability in Western Australia. Soc Sci Med. 2005;60:1499–513. doi: 10.1016/j.socscimed.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Cooper S-A, McConnachie A, Allan L, Melville C, Smiley E, Morrison J. Neighbourhood deprivation, health inequalities, and service use of adults with intellectual disabilities. Cross-sectional study. J Intellect Disabilit Res. 2011;55:313–23. doi: 10.1111/j.1365-2788.2010.01361.x. [DOI] [PubMed] [Google Scholar]
- 11.Morgan CL, Ahmed Z, Kerr MP. Health care provision for people with a learning disability: record linkage study of epidemiology and factors contributing to hospital care uptake. B J Psychiatr. 2000;176:37–41. doi: 10.1192/bjp.176.1.37. [DOI] [PubMed] [Google Scholar]
- 12.Elder R, Kirkpatrick M, Ramsay W, MacLeod M, Guthrie B, Sutton M, Watt G. Measuring quality in primary medical services using data from SPICE. Edinburgh: Information and Statistics Division: NHS National Services Scotland; 2007. [Google Scholar]
- 13.Carstairs V, Morris R. Deprivation and health in Scotland. Aberdeen: Aberdeen University Press; 1991. [Google Scholar]
- 14.Smith DJ, Martin DJ, McLean G, Langan Martin J, Guthrie B, Mercer SW. Multimorbidity in bipolar disorder and under treatment of cardiovascular disease: cross sectional study. BMC Medicine. 2013;11:263–274. doi: 10.1186/1741-7015-11-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Court H, McLean G, Guthrie B, Mercer S, Smith D. Visual impairment is associated with physical and mental comorbidities in older adults: a cross-sectional study. BMC Medicine. 2014;12:181. doi: 10.1186/s12916-014-0181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev Disabil. 2011;32:419–36. doi: 10.1016/j.ridd.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 17.Jones S, Cooper S-A, Smiley E, Allan L, Williamson A, Morrison J. Prevalence of, and factors associated with, problem behaviours in adults with intellectual disabilities. Journal of Nervous and Mental Diseas. 2008;196:678–86. doi: 10.1097/NMD.0b013e318183f85c. [DOI] [PubMed] [Google Scholar]
- 18.Finlayson J, Jackson A, Cooper S-A, Morrison J, Melville C, Smiley E, Allan J, Mantry D. Understanding predictors of low physical exercise in adults with intellectual disabilities. J Applied Res Intellect Disabilit. 2009;22:236–247. doi: 10.1111/j.1468-3148.2008.00433.x. [DOI] [Google Scholar]
- 19.Finlayson J, Morrison J, Jackson A, Mantry D, Cooper S-A. Injuries, falls, and accidents in the population of adults with intellectual disabilities. J Intellect Disabilit Res. 2010;54:966–80. doi: 10.1111/j.1365-2788.2010.01319.x. [DOI] [PubMed] [Google Scholar]
- 20.Melville C, Cooper S-A, Morrison J, Allan L, Smiley E, Williamson A. The prevalence and determinants of obesity in adults with intellectual disabilities. J Applied Res Intellect Disabilit. 2008;21:425–437. doi: 10.1111/j.1468-3148.2007.00412.x. [DOI] [Google Scholar]
- 21.Draheim CC, Stanish HI, Williams DP, McCubbin JA. Dietary intake of adults with mental retardation who reside in community settings. Am J Ment Retard. 2007;2007(112):392–400. doi: 10.1352/0895-8017(2007)112[0392:DIOAWM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Doan TN, Lennox NG, Taylor-Gomez M, Ware RS. Medication use among Australian adults with intellectual disability in primary healthcare settings: a cross-sectional study. J Intellect Dev Disabil. 2013;2013(38):177–81. doi: 10.3109/13668250.2013.778968. [DOI] [PubMed] [Google Scholar]
- 23.Beange H, McElduff A, Baker W. Medical disorders of adults with learning disabilities: A population study. Am J Ment Retard. 1995;99:595–604. [PubMed] [Google Scholar]
- 24.Kapell D, Nightingale B, Rodriguez A, et al. Prevalence of chronic medical conditions in adults with mental retardation: comparison with the general population. Ment Retard. 1998;36:269–79. doi: 10.1352/0047-6765(1998)036<0269:POCMCI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Baxter H, Lowe K, Houston H, Jone G, Felce D, Kerr M. Previously unidentified morbidity in patients with intellectual disability. Br J General Practice. 2006;56:93–98. [PMC free article] [PubMed] [Google Scholar]
- 26.Felce D, Baxter H, Lowe K, et al. The impact of repeated health checks for adults with intellectual disabilities. J Applied Res Intellectual Disabilities. 2008;21:585–96. doi: 10.1111/j.1468-3148.2008.00441.x. [DOI] [Google Scholar]
- 27.Chauhan U, Kontopantelis E, Campbell S, Jarrett H, Lester H. Hypothesis: Health checks in primary care for adults with intellectual disabilities: how extensive should they be? J Intellectual Disabilities Res. 2010;54:479–86. doi: 10.1111/j.1365-2788.2010.01263.x. [DOI] [PubMed] [Google Scholar]
- 28.Cooper S-A, Morrison J, Allan L, McConnachie A, Melville C, Baltzer M, McArthur L, Lammie C, Greenlaw N, Grieves E, Fenwick E. Practice nurse health checks for adults with intellectual disabilities: a cluster design randomised controlled trial. Lancet Psychiatry. 2014;1:511–521. doi: 10.1016/S2215-0366(14)00078-9. [DOI] [PubMed] [Google Scholar]
- 29.Tyrer F, Smith LK, McGrother CW. Mortality in adults with moderate to profound intellectual disability: a population–based study. J Intellect Disabilit Res. 2007;51:520–7. doi: 10.1111/j.1365-2788.2006.00918.x. [DOI] [PubMed] [Google Scholar]
- 30.Pauline Heslop P, Blair P, Fleming P, Hoghton M, Marriott A, Russ L. Confidential Inquiry into premature deaths of people with learning disabilities (CIPOLD). Final report; 2013. http://www.bris.ac.uk/media-library/sites/cipold/migrated/documents/fullfinalreport.pdf accessed 16.1.15.


