Abstract
Introduction:
Like many other people based professions, communications skills are essential to medical practice also. Traditional medical teaching in India does not address communication skills which are most essential in dealing with patients. Communication skills can be taught to medical students to increase clinical competence.
Objective:
To teach basic communication and counseling skills to fourth-year undergraduate students to increase their clinical competence.
Methodology:
A total of 48, fourth-year MBBS students participated in the study. They were given training in basic communication and counseling skills and taught the patient interview technique according to Calgary–Cambridge guide format. Improvement in communication was assessed by change in pre- and post-training multiple choice questions, clinical patient examination, and Standardized Patient Satisfaction Questionnaire (SPSQ) scores.
Results and Analysis:
About 88% of the students in the sample were convinced of the importance of learning communication skills for effective practice. Almost 90% students were communicating better after training, as tested by improved SPSQ. As judged by Communication Skill Attitude Scale, student's positive attitude toward learning communication skill indicated that there is a necessity of communication skill training during undergraduate years.
Conclusion:
The ability to communicate effectively is a core competency for medical practitioners. Inculcating habits of good communications skill during formative years will help the medical students and future practitioners. Regular courses on effective communication should be included in the medical school curriculum.
Keywords: Calgary–Cambridge model, clinical competency, communication skills, counseling, medical students
INTRODUCTION
Like many other people based professions, communications skills are essential for medical practice. It is a backbone over which lot of areas of patient care rests such as, first contact patient interviews, probing for associated and additional problems, counseling the patient, explaining treatment options, its complications and advising follow-up. It is also necessary for explaining risks to the patient, counseling in case of bereavement or mishap, providing information about a surgical procedure its complications, taking an informed consent, and lot more other areas of patient care. Traditional medical teaching imparts students with theoretical and practical knowledge of diseases processes and gives them education about diagnostic and treatment modalities, but does not address communication skills which are most essential in dealing with patients.[1,2] Good communications and counseling techniques can be taught and practiced to increase clinical competence.[3] Physician's interpersonal and communication skills have a significant impact on patient care and correlate with improved healthcare outcomes.[4]
Better communication between doctor and patient builds confidence, improves compliance, and reduces mistakes and mishaps, thereby reducing malpractice suits. If knowledge of medicine, surgical skill, and clinical acumen is the craft of medical practice, the communications skills are the fine arts! Professionalism, which is an integral part of good medical practice, also demands effective communication skills along with knowledge, skill, competence and ethics.[5,6,7] Association of American Medical Colleges Cincinnati, expert panel identified seven components considered to be fundamental to all encounters between clinician and patient: The key components are – build the relationship, open the discussion, gather information, understand the patient's perspective, share information, reach agreement on problems and plans, provide closure. These can be taught to the students during the communication training program using the framework of Calgary–Cambridge patient interview model.[5,7]
There are certain misconceptions about teaching communications to medical students, like communication skills are not considered teachable, or the skills acquired during training period tends to decline over time.[2] Students and teachers feel that these would be learned and improved with experience. Improving communication skills requires faculty and students to possess self-awareness, interpersonal sensitivity, and willingness to be self-reflective.[3] In spite of the aforesaid hurdles, it is a foregone conclusion that the practice of medicine requires more than just communication skills, but good communications is necessary for effective practice. The communication skills training can be incorporated in undergraduate training.
Keeping these points in mind, the current project work was started with objectives of - to teach basic communication and counseling skills to fourth-year undergraduate students to improve their overall clinical competence, performance on clinical patient examination (CPX) and patient interview skills as directed by Calgary–Cambridge model.
METHODOLOGY
A total of 48 final year MBBS students in two batches of 24 students each underwent a 3-day training program in communication and counseling skills. The training program was well-structured. Assessment of student's preexisting knowledge of communication skills was carried out by a precourse questionnaire - Communication Skill Attitude Scale (CSAS) - originally developed by Rees and Sheard.[8,9,10] Their scores from the questionnaire (CSAS) were considered in analyzing the utility of communication skill training during undergraduate years. The training module for teaching communication skills [Table 1] included: Importance of communication in medical practice; training in basic communication and counseling skills through lectures, small group discussion and role plays; training in patient interview skills by Calgary–Cambridge observation guide [Figure 1]; practice the acquired skills on standardized patients and through role plays; assessment of improvement in student's performance in patient interview skills through CPX, Objective Structured Clinical Examination (OSCE) and by Standardized Patient Satisfaction Questionnaire (SPSQ) before and after training program by using a five point checklist scoring system with 0, 1, 2 score for each point with maximum score of 10 for CPX and SPSQ; and analysis of students’ retention of knowledge about communication by posttraining multiple choice questions (MCQs). Analysis was done by compiling the results of pre- and post-CSAS and SPSQ.
Table 1.
Schedule for communication training program
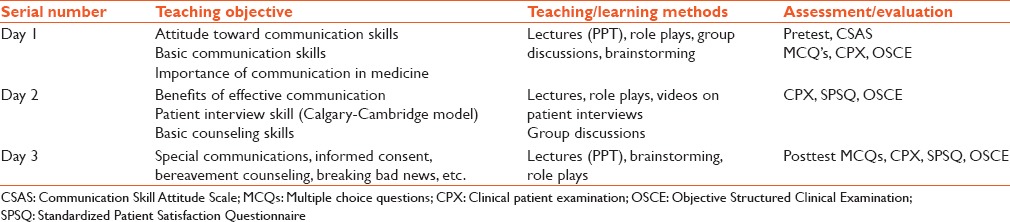
Figure 1.
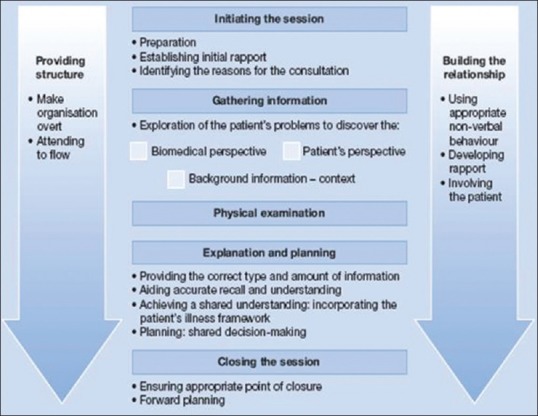
Calgary–Cambridge model
RESULTS
Students’ attitude toward learning communication skills was assessed by precourse CSAS questionnaire. Eighty-two percent of students were convinced about the utility of soft skills in medical practice. A total of 78.1% had a positive attitude toward learning communications skills, 11.3% students displayed negative attitude, and 10.6% were neutral [Figure 2]. Student's performance, as judged during OSCE and CPX on simulated patients, improved significantly after training, as judged by improved SPSQ scores [Figure 3]. Patients gave positive feedback in posttraining encounters as seen by improved score in SPSQ. Almost 90% of students were satisfied with a teaching program, and the majority of them understood the importance of having good communication skills in medical practice. The students scored well (88–92%) on posttraining MCQs suggesting an adequate retention of knowledge.
Figure 2.
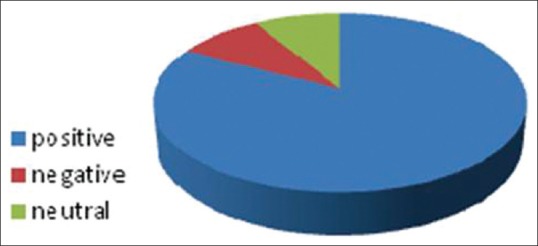
Attitude of the students toward communications skills. CSAS: Communication Skill Attitude Scale
Figure 3.
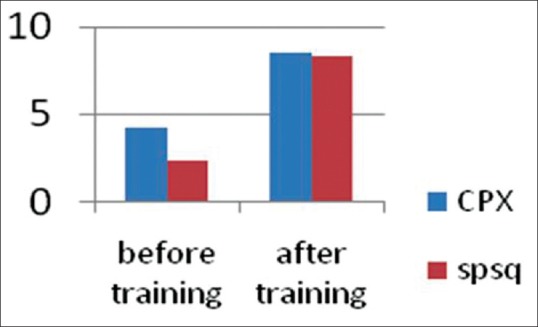
Comparison of pre and post training CPX/SPSQ scores. SPSQ: Standardized Patient Satisfaction Questionnaire, CPX: Clinical patient examination)
DISCUSSION
Good communication skills are an asset in medical practice. Effective communication wins the physician the confidence and compliance of patients and helps build a healthy doctor–patient relationship. These essential soft skills can be learned during the formative years and practiced to perfection over the years. We tried to establish these points by the above project. Students develop communication skills by observing their seniors, teachers and mentors and then practice. Though systematic teaching of these skills is challenging during formative years, training in communication during clinical posting can bring these skills to life and allow students and faculty to see their relevance.[3] Wright et al., studied students attitude toward learning these skills and compared the attitudes in first- and fourth-year students, found that that fourth-year medical students do not differ from first-year medical students in terms of attitudes toward communication skills training, but they have significantly higher confidence scores about communicating with patients.[11] This study indicates that the positive attitude increases by perceived relevance of the skills by the students.[8] In the present study, the subjects were fourth-year students, and we found a significantly higher number of students had a positive attitude toward learning communication skills. This is due to the fact that these students are in contact with the patients during clinical posting and begin to understand the importance of effective communication. Keeping the focus on the results of this study we found our findings were in agreement with earlier studies done by Wright et al.
Haq et al. in her paper describes the content and methods used to teach communication skills to medical students. Suggested curriculum projects should be designed to improve medical students’ communication skills during the undergraduate years, which they can refine and practice throughout the MBBS course and later.[12] The present project was designed to understand the utility of teaching communication skills to medical students. Aspegren in his guide on communication skills stated that communication skills can be taught at courses, are learnt, but are easily forgotten if not maintained by practice. The most effective point in time to learn these at medical school is probably during the clinical posting. After a short training, doctors can be effective as teachers.[3] We tried to focus our training courses for the fourth-year students and found that these skills can be taught and learned and practiced to improve clinical competence, the training in our teaching module was done by the faculty doctors. Medical students interpersonal and communication skills are a fundamental dimension of their clinical competence.[13]
Despite an increasing awareness of importance communication skills in modern medical practice Indian Medical Collages have not incorporated the training in their curricula. Best teaching practices and evaluation methods to improve the skills of medical students, to communicate optimally with patients, families, and health team members can be incorporated in undergraduate years.[14] In our project, we found that student’ skills and confidence in communicating with patients increased after training.
Yedidia et al. while studying Effect of communications training on medical student performance concluded that communications curricula using an established educational model significantly improved third-year students overall communications competence, as well as their skills in relationship building, organization and time management, patient assessment etc., and increased clinical competence.[1] These findings were similar to our observations. In a study done by Joekes et al., where students received a curriculum that included communication skills training integrated into a “professional development” vertical module, noticed that students receiving the professional development training showed significant improvements in certain communication skills and achieved higher ratings for use of silence, not interrupting the patient, and keeping the discussion relevant, compared to students receiving the traditional curriculum.[2] We observed a similar increase in the use of verbal and nonverbal communication skills by our students after the training.
Deveugele et al. in their efforts to teach communication skills to medical students used various methods like group discussions in small groups (10–15 students), with focus on role playing with colleagues and simulated patients and showing videotapes of real consultations etc., observed a positive effect in the communication skills of students.[10] Karlberg and Lindgren incorporated a continuous and structured training in communication skills during the early phase of medical studies. As a result of these programs, they noticed significantly higher satisfaction in medical encounters among patients. This study highlights the fact that including patient-oriented communication skill teaching for undergraduate medical students improves their competency, increases patient satisfaction and clinical outcome. These results agree with our findings.[15] Based on our observations we found that there is a utility of communications skills training in the formative years. These soft skills can be imparted to medical students by the faculty, practiced to increase competency, used to build doctor-patient relationships and enhance health outcomes.[6]
CONCLUSION
The ability to communicate effectively is a core competency for medical practitioners. Advantages of effective communication cannot be emphasized enough. Inculcating habits of good communications skill during formative years will help the medical students and future practitioners. Communication skill training during formative years is a positive investment for the better future health of the society. Regular courses on effective communication should be included in the medical school curriculum.
Acknowledgments
I would like to acknowledge the support provided by the Principal, Head of the Department of Obstetrics and Gynecology, and the Ethics Committee, without their encouragement the project would not have been successful. I appreciate the contributions of my fellow colleagues and the students who participated in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yedidia MJ, Gillespie CC, Kachur E, Schwartz MD, Ockene J, Chepaitis AE, et al. Effect of communications training on medical student performance. JAMA. 2003;290:1157–65. doi: 10.1001/jama.290.9.1157. [DOI] [PubMed] [Google Scholar]
- 2.Joekes K, Noble LM, Kubacki AM, Potts HW, Lloyd M. Does the inclusion of ‘professional development’ teaching improve medical students’ communication skills? BMC Med Educ. 2011;11:41. doi: 10.1186/1472-6920-11-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aspegren K. BEME Guide No 2: Teaching and learning communication skills in medicine – A review with quality grading of articles. Med Teach. 1999;21:563–70. doi: 10.1080/01421599978979. [DOI] [PubMed] [Google Scholar]
- 4.Rider EA, Hinrichs MM, Lown BA. A model for communication skills assessment across the undergraduate curriculum. Med Teach. 2006;28:e127–34. doi: 10.1080/01421590600726540. [DOI] [PubMed] [Google Scholar]
- 5.Hausberg MC, Hergert A, Kröger C, Bullinger M, Rose M, Andreas S. Enhancing medical students’ communication skills: Development and evaluation of an undergraduate training program. BMC Med Educ. 2012;12:16. doi: 10.1186/1472-6920-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modi JN, Anshu, Gupta P, Singh T. Teaching and assessing professionalism in the Indian context. Indian Pediatr. 2014;51:881–8. doi: 10.1007/s13312-014-0521-x. [DOI] [PubMed] [Google Scholar]
- 7.Nataša M, Bakić-Mirić, Nikola M. Successful doctor-patient communication and rapport building as the key skills of medical practice. Facta Univ Ser Med Biol. 2008;15:74–9. [Google Scholar]
- 8.Neupane MS, Neupane HC, Adhikari S, Aryal B. Attitude Towards learning communication skills in medical students of Chitwan Medical College, Chitwan, Nepal. Int J Pharm Biol Arch. 2012;3:1058–61. [Google Scholar]
- 9.Rees C, Sheard C. The relationship between medical students’ attitudes towards communication skills learning and their demographic and education-related characteristics. Med Educ. 2002;36:1017–27. doi: 10.1046/j.1365-2923.2002.01333.x. [DOI] [PubMed] [Google Scholar]
- 10.Deveugele M, Derese A, De Maesschalck S, Willems S, Van Driel M, De Maeseneer J. Teaching communication skills to medical students, a challenge in the curriculum? Patient Educ Couns. 2005;58:265–70. doi: 10.1016/j.pec.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Wright KB, Bylund C, Ware J, Parker P, Query JL, Jr, Baile W. Medical student attitudes toward communication skills training and knowledge of appropriate provider-patient communication: A comparison of first-year and fourth-year medical students. Med Educ Online. 2006:11–8. doi: 10.3402/meo.v11i.4594. [DOI] [PubMed] [Google Scholar]
- 12.Haq C, Steele DJ, Marchand L, Seibert C, Brody D. Integrating the art and science of medical practice: Innovations in teaching medical communication skills. Fam Med. 2004;36(Suppl):S43–50. [PubMed] [Google Scholar]
- 13.Chessman AW, Blue AV, Gilbert GE, Carey M, Mainous AG., 3rd Assessing students communication and interpersonal skills across evaluation settings. Med Stud Educ. 2003;35:643–8. [PubMed] [Google Scholar]
- 14.Main CJ, Buchbinder R, Porcheret M, Foster N. Addressing patient beliefs and expectations in the consultation. Best Pract Res Clin Rheumatol. 2010;24:219–25. doi: 10.1016/j.berh.2009.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karlberg L, Lindgren C. Communication skills in the encounter with patients – current examination subject for medical students. Beneficial educational investment. Lakartidningen. 2004;101:3072–4. 3076. [PubMed] [Google Scholar]


