Abstract
Context:
We believe that there is significant educational deficit amongst interns regarding up-to-date formal knowledge and skills on healthcare-associated infections (HAIs) which might compromise patient safety. This urgently requires curriculum innovations to ensure their formal training on HAIs prevention and control.
Aim:
Education of interns to improve their knowledge and skills toward HAIs prevention and control.
Subjects and Methods:
This pilot study was conducted in interns using a multimodal approach consisting of a combination of videos, PowerPoint presentation, and hands-on demonstration to provide applied and practical teaching on prevention and control of HAIs. Pre- and post-test assessment of knowledge, attitude, and skills was carried out by multiple choice questions, 5-point Likert scale, and Objective Structured Practical Examination respectively.
Statistical Analysis Used:
Paired t-test
Results:
A statistically significant improvement in the overall score rates between pre- and post-test of intern's was seen, suggesting that educational programs have a positive effect. Intern's felt benefitted from interventions focused on HAIs prevention and control and hoped that such sessions are integrated in the regular undergraduate curriculum. A majority of the students felt that their learning style assessment matched well with their own perception of learning preference.
Conclusions:
Assessment drives learning; hence strengthening the contribution of health-care workers to HAIs prevention programs should include measures that enhance knowledge, improve skills and develop appropriate attitudes, resulting in safety and quality of patient care.
Keywords: Assessment, healthcare-associated infections, health-care workers, objective structured physical examination
INTRODUCTION
Healthcare-associated infections (HAIs) are defined as those that develop during hospitalization but are neither present nor incubating upon the patient's admission to the hospital; generally for those infections that occur more than 48–72 h after admission and within 10 days after hospital discharge.[1] Of every 100 hospitalized patients at any given time, 7 in developed and 10 in developing countries will acquire at least one HAI.[2] HAIs are a man-made medical crisis that equally affect patients, health-care workers (HCWs) and entire health-care system leading to increased morbidity, mortality, duration of hospital stay, health-care costs, multi-drug resistance, and safety risk to HCWs. Unfortunately, our existing medical curriculum has not accorded sufficient emphasis on applied aspects of HAIs. This reflects in reduced compliance by medicos on HAIs prevention and control guidelines, leading to devastating consequences. In order to ensure that the doctors of the future are safe practitioners, it is essential that they have the relevant knowledge and skills which inform their attitude leading to appropriate professional behavior. This study is an initiative to educate interns to improve their knowledge attitude and skills toward HAIs prevention and control.
SUBJECTS AND METHODS
The study was conducted at a tertiary care medical college and hospital in North India. The study was carried out with the intern's presently undergoing their rotatory internship. Exemption status for the study was obtained from the Institutional Ethical Committee. Twenty-one interns gave their consent to participate in the study. The purpose of the study was explained as per the ethical guidelines of Helsinki, and intern's were requested to fill the questionnaires after assuring them of the fact that the results had no impact on their final grades in internship. The participation of intern's was voluntary, and the questionnaires were kept anonymous. In order to measure baseline knowledge, attitude and skills regarding hand hygiene and HAI, all the participants were administered multiple choice questions based questionnaires for assessment of HAIs related knowledge component. To evaluate the attitude, participants completed a 30-item survey using a 5-point Likert scale. Skills were assessed by introducing Objective Structured Physical Examination (OSPE). A brief presentation was made to introduce the OSPE as an assessment tool. We used a multimodal intervention approach that included a professional 10 min video specifically designed to sensitize HCWs to want to comply with the World Health Organization's (WHO) concept of “Five Moments for Hand Hygiene.”[3] Another video showed how HAIs spread from HCWs to patients and the importance of “Break the chain” concept. A PowerPoint presentation documented how HAI occur, the magnitude of the problem and prevention strategies. The novel hands-on workshop focused on practical skills associated with HAIs. The participants were given a live demonstration on how to perform hand hygiene, venepuncture/phlebotomy, personal exposure prophylaxis and biomedical waste management. The program concluded with a post- test and program evaluation. A comparison between the pre- test results and the post- test results was used to assess improvement regarding HAI and hand hygiene compliance.
The primary outcome of the study was to change participants’ knowledge and skills regarding HAI and hand hygiene and to influence positively their practice. A pre and post questionnaire with 5-point Likert scale was used to get an insight of interns and faculty into their awareness, attitude and motivation after being exposed to the OSPE. The total number of responses was collected, and data was processed and analyzed using EpiInfo™ 7 (WHO) and Microsoft Excel-97 software. Comparison of pre- and post-test scores was made by paired t-test and the significance level (P value) was set at 0.001.
RESULTS
A total of 42 intern's who were posted in clinical departments in hospital premises were invited to participate in the study. Twenty-one students (50.0%) agreed to participate and subsequently were enrolled in the study. The participating intern's included 6 males (28.57%) and 15 females (71.42%). Virtually every participant correctly identified the importance of hand hygiene before feeding a patient, as well as acknowledging that fatigue or workload is not acceptable reasons to ignore hand hygiene. In addition, participants recognized that brief random contact with patient linen does contaminate hands, it is okay to remind a colleague or a superior to clean their hands before patient contact; and not maintaining proper hand hygiene impacts your family. Question: “What is the most frequent source of germs responsible for HAIs?” had low pre- test scores (28.57%), and even fewer participants answered it correctly on the post- test (9.50%). A statement that received less correct answers after the intervention was: “Clostridium difficile (the cause of antibiotic-associated diarrhea) is readily killed by alcohol-based hand hygiene products.” The statement that most participants selected incorrectly on the pre- test (42.80%) and improved the most on the post- test (90.47%) was Q4 “Which of the following infections can be potentially transmitted from patients to clinical staff if appropriate glove use and hand hygiene are not performed?”
A total of 17 (80.90%) of participants correctly identified color codes used in biomedical waste segregation and disposal in the pre-test. After the hands-on session, all the 21 participants answered correctly. However, there was no change in the pre- and post-test scores on the question based on the maximum time limit for the treatment of biomedical waste.
The questionnaire to assess workshop satisfaction showed that the majority of items were scored at nearly 90%, suggesting that participants thought the program improved their knowledge and skills related to hand hygiene and HAI.
A comparison of pre- and post-test results showed a statistically highly significant improvement in the HAIs associated knowledge [Tables 1 and 2], attitude, and skills [Table 3] as assessed by OSPE.
Table 1.
Comparison of means of pre- and post-test scores on assessing knowledge, attitude and skills
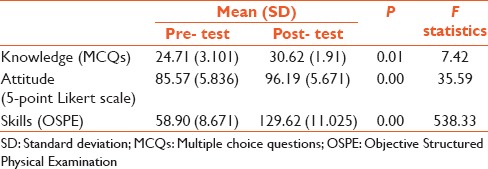
Table 2.
Comparison of means of pre- and post-test correct scores on knowledge related to hand hygiene

Table 3.
Comparison of means of pre- and post-test scores for HAI associated skills as assessed by individual OSPEs

DISCUSSION
Recent studies have reported that the hand hygiene and other practices of HCWs might be related to workload, stress and the physical environment.[4,5,6] However, it has also been suggested that poor hand hygiene compliance is related to bad habits and can be controlled with the combination of education and training.[3,4,5,6]
While there are many studies and interventions that have assessed the knowledge base of medicos, there is a much smaller body of literature on attitudes and behaviors. For example, in a French study of 350 students, including 107 medical students, nursing students had a better overall score compared to medical students in the knowledge of hand hygiene, standard precautions, and HAIs.[7] In Birmingham, UK, medical students were assessed for their knowledge of certain aspects of HAIs, of which 48% participated.[8] This study assessed knowledge of hand hygiene, the color of clinical waste bags, the use of gloves, the disposal of sharps, venepuncture, and needle stick injuries. Just under half felt that not enough emphasis was placed on infection prevention and control, 50% knew when they should return to the wards after being ill with diarrhea and 83% knew what action to take in the event of a needle stick injury.[8] A survey of 31 of 38 (82%) medical schools in the UK and the Republic of Ireland revealed that HAIs as a quality and safety issue was covered in only 60% of medical schools, but that waste, personal equipment, and standard precautions were assessed in 60–67% of medical schools.[9] In Thailand, none of 12 medical school directors surveyed expressed themselves satisfied with the teaching on HAIs but the survey itself subsequently resulted in modifications in two of these.[10] Again, in an assessment of knowledge of nearly 500 medical students in Iran, scores were approximately 66%.[11] Practice rather than knowledge alone is a better assessment of on-going behavior and in a study of medical students carrying out their final medical exams, only 9% of students used an alcohol hand gel on day,[7] before there was a notice instructing this, compared with 27% after a notice had been put up in the examination area on day 2.[4] Forty per cent of these medical students felt that their compliance with hand hygiene was at least 80%, whereas observed practice indicated otherwise.[4]
In the existing medical curriculum, the topic of HAIs is taught through a didactic lecture on facts related to the etiology, pathogenesis and control measures. However, there is neither a module which involves practical training of students to acquire skills of hand washing and waste disposal nor any method to evaluate these skills. The evaluation of knowledge regarding HAIs is, therefore, a matter of chance depending on questions in this topic appearing in the theory paper, while practical skills are not evaluated at all. This creates a big lacuna in the formative years of undergraduate studies, as the students are likely to underestimate the importance of these preventive measures. A likely outcome is a noncompliance to proper hand washing and safe waste disposal in their future clinical practice, leading to the spread of HAIs rather than to their prevention. Therefore an immense need to introduce an innovative methodology to train and evaluate 2nd year undergraduates for the acquisition of practical skills for the prevention of HAIs was felt. An OSPE was thought to be best suited for a systematic assessment of various steps involved. This was described in 1975 and in greater detail in 1979 by Harden and his group from Dundee and has become a popular tool for evaluation with the inherent advantages of being a practical, reliable and valid alternative for objective assessment of practical skills.[12,13]
The study results produced a statistically highly significant improvement in the overall score rates between pre- and post-test assessment of intern's suggesting that educational programs have a positive effect on the knowledge, attitudes, and skills associated with HAIs. It helped us to identify the weak areas related to HAI in our setting. This interaction also motivated the intern's to try newer methods of learning, and they reported feeling benefitted from this change. The results suggest that intern's might not have had sufficient formal knowledge of HAI; therefore, medical schools might need to re-evaluate the way they teach hand hygiene and the placement of the course in the curriculum. One major limitation of the present study was the study population. We couldn’t have a significant number of participants because of tight and scattered (half of them were posted in peripheral health-care centers) roster of intern's and many of them were preparing for postgraduate exams. Furthermore, we were not able to test and assess key HAI events like catheter-associated urinary tract infections and intravascular catheter-associated bloodstream infections because of ethical and practical reasons. The recent global increase in HAI rates suggests that there is a critical need for improved periodic education and training of HCWs. Compliance to practices resulting in decreased HAIs is a multifactorial problem that involves knowledge and behavior. Educational awareness and frequent reminders are critical to maintaining high rates of compliance with these practices. It is clear that much work needs to be done to enhance and improve the education of medicos following graduation to improve practice and behavior toward HAIs. At present, this area is not adequately prioritized, and there is insufficient training and assessment of practice and attitudes that would emphasize its importance. It is high time that a module on HAIs should be formally integrated in the undergraduate curriculum. Also, there is scope for regular interventions like CMEs and workshops that would underpin many international initiatives such as the WHO campaign on hand hygiene. Consequently, we must strive to educate our medicos on the importance of this area by improving both undergraduate and postgraduate medical education to enhance ultimately the quality and safety of patient care. Sustained and continuous interventions like this will decrease the educational deficit amongst interns regarding up-to-date formal knowledge and skills on HAIs leading to a positive professional attitude by the time they leave the college and become practitioners.
Acknowledgments
We gratefully acknowledge the guidance and help provided by the FAIMER faculty at Christian Medical College, Ludhiana, FAIMER Fellows, Faculty, demonstrators and para-medical staff at Department of Microbiology, Government Medical College, Jammu. We are also thankful to Dr. Rakesh Bahl for performing statistical analysis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Horan TC, Gaynes RP. Surveillance of nosocomial infections. In: Mayhall CG, editor. Hospital Epidemiology and Infection Control. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 1659–702. [Google Scholar]
- 2.WHO Health Care-associated Infections Fact Sheet. [Last accessed on 2015 Jul 16]. Available from: http://www.who.int/gpsc/country_work/gpsc_ccisc_fact_sheet_en.pdf .
- 3.Guide to the Implementation of the WHO Multimodal Hand Hygiene Improvement Strategy. [Last revised on 2009 Aug; Last accessed on 2015 July]. Available from: http://www.who.int/gpsc/5may/tools/WHO_IER_PSP_2009.02_eng.pdf .
- 4.McHugh SM, Hill AD, Humphreys H. Preventing healthcare-associated infection through education: Have surgeons been overlooked? Surgeon. 2010;8:96–100. doi: 10.1016/j.surge.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Tavolacci MP, Ladner J, Bailly L, Merle V, Pitrou I, Czernichow P. Prevention of nosocomial infection and standard precautions: Knowledge and source of information among healthcare students. Infect Control Hosp Epidemiol. 2008;29:642–7. doi: 10.1086/588683. [DOI] [PubMed] [Google Scholar]
- 6.Tavolacci MP, Ladner J, Bailly L, Merle V, Pitrou I, Czernichow P. Prevention of nosocomial infection and standard precautions: Knowledge and source of information among healthcare students. Infect Control Hosp Infect. 2008;29:642–7. doi: 10.1086/588683. [DOI] [PubMed] [Google Scholar]
- 7.Humphreys H, Richards J. Undergraduate and postgraduate medical education on the prevention and control of healthcare-associated infection. More progress is needed. Int J Infect Control. 2011;7:i2. [Google Scholar]
- 8.Graf K, Chaberny IF, Vonberg RP. Beliefs about hand hygiene: A survey in medical students in their first clinical year. Am J Infect Control. 2011;39:885–8. doi: 10.1016/j.ajic.2010.08.025. [DOI] [PubMed] [Google Scholar]
- 9.Hunt DC, Mohammudally A, Stone SP, Dacre J. Hand-hygiene behaviour, attitudes and beliefs in first year clinical medical students. J Hosp Infect. 2005;59:371–3. doi: 10.1016/j.jhin.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Z, Yamamoto T, Wu XN, Moji K, Cai GX, Kuroiwa C. Educational intervention for preventing bloodborne infection among medical students in China. J Hosp Infect. 2010;75:47–51. doi: 10.1016/j.jhin.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 11.Tucker A, Phillips WR. Medical students and infection control: Risks and precautions. Tokai J Exp Clin Med. 1999;24:169–76. [PubMed] [Google Scholar]
- 12.Harden RM, Stevenson M, Downie WW, Wilson GM. Assessment of clinical competence using objective structured examination. Br Med J. 1975;1:447–51. doi: 10.1136/bmj.1.5955.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harden RM, Gleeson FA. Assessment of clinical competence using an objective structured clinical examination (OSCE) Med Educ. 1979;13:41–54. [PubMed] [Google Scholar]


