Abstract
Longitudinal outcomes following stress or trauma diagnoses are receiving attention, yet population-based studies are few. The aims of the present cohort study were to examine the cumulative incidence of traumatic events and psychiatric diagnoses following diagnoses of severe stress and adjustment disorders categorized using International Classification of Diseases, Tenth Revision, codes and to examine associations of these diagnoses with all-cause mortality and suicide. Data came from a longitudinal cohort of all Danes who received a diagnosis of reaction to severe stress or adjustment disorders (International Classification of Diseases, Tenth Revision, code F43.x) between 1995 and 2011, and they were compared with data from a general-population cohort. Cumulative incidence curves were plotted to examine traumatic experiences and psychiatric diagnoses during the study period. A Cox proportional hazards regression model was used to examine the associations of the disorders with mortality and suicide. Participants with stress diagnoses had a higher incidence of traumatic events and psychiatric diagnoses than did the comparison group. Each disorder was associated with a higher rate of all-cause mortality than that seen in the comparison cohort, and strong associations with suicide were found after adjustment. This study provides a comprehensive assessment of the associations of stress disorders with a variety of outcomes, and we found that stress diagnoses may have long-lasting and potentially severe consequences.
Keywords: cohort studies, stress disorders, traumatic, suicide
Outcomes following stress or trauma diagnoses are receiving more attention, but population-based longitudinal studies of people with these diagnoses are few. The International Classification of Diseases, Tenth Revision (ICD-10), includes 5 diagnoses that could be given following a stressful or traumatic event: acute stress reaction (a diagnosis given in the immediate aftermath of the event), posttraumatic stress disorder (PTSD) (a diagnosis given following a traumatic event and a timed period of nonrecovery), adjustment disorders (a diagnosis given after a stressful event and a timed period of nonrecovery), and 2 general diagnoses (other reactions to severe stress and reactions to severe stress, unspecified). These general diagnoses are given to people who experience distress following a stressful or traumatic event but who do not meet the full diagnostic criteria for another disorder (1).
Of these disorders, PTSD has been the most frequently studied to date. Research on retraumatization among people with PTSD has been focused largely on sexual trauma and intimate-partner violence and has consistently shown that people with PTSD who have had these experiences have a higher risk of retraumatization (2–5). In a study of US military veterans, Orcutt et al. (6) also found that PTSD after combat exposure is associated with later traumatic life events.
Strong evidence for an association between PTSD and other psychiatric diagnoses exists as well. It is widely held that depression and PTSD are highly comorbid, as are PTSD and substance abuse and dependence (7, 8), and that depression and alcohol abuse are potential sequelae of traumatic experiences and PTSD in general (9–11). Given this, it is not surprising that PTSD has been cited as resulting in marked costs to individuals and society (11). Other diagnoses that may be given following stressful or traumatic events, such as adjustment disorder, have received less attention in the literature, and it is not clear whether the findings summarized above for PTSD are generalizable to other stress disorders.
In addition to research on retraumatization or psychiatric comorbidity, there is a small but compelling literature on the association between all-cause mortality and death from suicide following one of these diagnoses. PTSD was associated with a higher rate of all-cause mortality in large cohort studies of US veterans in both unadjusted and adjusted analyses (12–14), although this association was null after adjustment for relevant confounders in one of the studies (14). We know of no studies in which all-cause mortality has been examined among people diagnosed with other stress disorders. Suicide has been associated with PTSD and other stress disorders, including acute stress reaction and adjustment disorders, in a small number of population-based case-control studies (15–18). An association between PTSD and suicide has also been shown among US veterans (19).
Given the paucity of literature on outcomes following stress disorder diagnoses other than PTSD in longitudinal cohort studies and the limited knowledge about whether the longitudinal course of other stress disorders is similar to what has been observed for PTSD, we examined various sequelae of these diagnoses. Specifically, we examined the cumulative incidence of traumatic events and psychiatric diagnoses following incident diagnoses of reaction to severe stress or adjustment disorder as indicated by ICD-10 codes F43.x (1). We also examined the associations of stress diagnoses with all-cause mortality and suicide.
METHODS
We previously published a detailed description of the creation of the cohort with stress or adjustment disorders that was used in this study (20). In brief, the cohort contains any Danish-born resident of Denmark over the age of 15 years who received an ICD-10 diagnosis of reaction to severe stress or adjustment disorder at an inpatient or outpatient psychiatric clinic between January 1, 1995, and December 31, 2011 (n = 101,663). We excluded patients who received a stress diagnosis only in a non–psychiatric treatment setting because disorder severity among these people could differ from that among participants who received treatment from a psychiatric specialist. In addition, we created a matched comparison cohort of Danish-born residents of Denmark who had not received a formal diagnosis of reaction to severe stress or adjustment disorder at the time that their matched stress cohort member was diagnosed (n =508,315). Members of the comparison cohort were individually matched to stress cohort members by sex and age at the matched index date at a ratio of up to 5 to 1. Comparison cohort members were selected at random from the Danish Civil Registration System from among those who met the matching criteria. Data on sample characteristics (date of birth, sex, marital status, and citizenship status) were also obtained from this registry.
Variables and data sources
In Denmark, almost all treatment (hospitalization, outpatient, and emergency) is provided free of charge by a tax-funded universal health care system. As a result, treatment codes are catalogued in various national Danish medical and social longitudinal registries. Each resident of Denmark is assigned a unique 10-digit Civil Registration number, and these numbers were used to retrieve and merge individual data for the creation of the cohorts and the present project.
Predictors
The main predictor variables in our analyses were ICD-10 stress diagnoses: acute stress reaction (ICD-10 code F43.0), PTSD (ICD-10 code F43.1), adjustment disorders (ICD-10 code F43.2), other reactions to severe stress (ICD-10 code F43.8), and reaction to severe stress, unspecified (ICD-10 code F43.9). Diagnostic data (including date of diagnosis) were obtained from the Danish Psychiatric Central Research Registry. This registry includes data on all inpatient and outpatient psychiatric treatments since 1995. It contains treatment dates and up to 20 diagnoses per treatment entry for patients who were admitted to a psychiatric inpatient hospital, received outpatient psychiatric care, or received treatment at a psychiatric emergency unit. Validation studies of diagnoses in the registry (e.g., schizophrenia or affective disorders) have shown high validity compared with computer-generated diagnoses or independent re-interview (21, 22). Our validation study of the stress diagnoses showed that validity was good for the more mild and transient diagnoses (i.e., acute stress reaction; other reactions to severe stress; and reactions to severe stress, unspecified) and high for the more severe, stringently diagnosed or chronic disorders (i.e., PTSD and adjustment disorder) (23).
Outcomes
The primary outcomes in the present study were all-cause mortality and death from suicide. Data on these outcomes were obtained from the Danish Register of Causes of Death. This registry contains information on all deaths in Denmark from 1970 onward. Information in the registry includes time and place of death, events that led to the death, manner of death (e.g., natural, accident, homicide, or suicide), and disease diagnoses that might have contributed to the death. Autopsy findings are included for cases in which an autopsy was conducted. Deaths that were coded with an ICD-10 code in the range of X60–X84 (intentional self-harm) in this registry were classified as suicides. In addition, we included any record in the Danish National Patient Register in which there was a suicide attempt followed by a death recorded in the Civil Registration System in the subsequent 7 days. The secondary method was used because in this registry, the cause of death might be coded as the injury that caused death rather than suicide; for example, the cause of death could be listed as “asphyxiation” for a suicide death by hanging.
We also examined 2 additional sets of secondary outcomes in the present study. The first set was subsequent stressful or traumatic events following a stress diagnosis. Data on these outcomes were obtained from the Danish National Patient Register, which includes discharge records from all somatic Danish hospitalizations and hospital outpatient visits since 1995, coded using ICD-10 (24). We included records with codes for accidents (ICD-10 codes V01–X59), assault (ICD-10 codes X85–Y09), and poisoning by drugs, medicaments, and biological substances (ICD-10 codes T36–T50), as well as maltreatment syndromes (ICD-10 code T74). The second set was incident psychiatric diagnoses following a stress diagnosis. These diagnoses, obtained from both the Danish Psychiatric Central Research Register and the National Patient Register, included depression (ICD-10 codes F32, F33, and F34.1), anxiety disorders (ICD-10 codes F40 and F41), alcohol abuse and dependence (ICD-10 codes F10.1, F10.2, and F10.3), and drug abuse and dependence (ICD-10 codes F11.2, F12.2, F13.1, F13.2, and F14.2).
Covariates
Variables selected for adjustment in the regression analyses included baseline depression and anxiety diagnoses, as well as alcohol and drug abuse and dependence diagnoses (ascertained as described above). We also computed a Charlson Comorbidity Index score as a measure of baseline physical health status for each person based on diagnoses within the National Patient Register. We included this score as a covariate in the analyses of all-cause mortality (25, 26).
Analyses
We conducted descriptive and stratified analyses to examine important demographic variables, baseline psychiatric disorders, and baseline traumatic events across categories of stress diagnoses. We plotted cumulative incidence curves to examine the occurrence of traumatic events and new-onset psychiatric diagnoses in the 15-year study period following the initial stress diagnosis (or the index date among the comparison cohort). Finally, we used Cox proportional hazards regression models to examine the unadjusted and adjusted associations of each stress diagnosis with all-cause mortality (excluding suicide) and suicide. The variables for which we adjusted were chosen based on a literature review, and only those that occurred before stress diagnoses were included to ensure that they were not on the causal pathway from the stress diagnosis to all-cause mortality or suicide. We restricted all analyses to members of the cohorts who were 15 years of age or older and considered to be adults, which was consistent with the maximum age of compulsory education in Denmark. This work was approved by the Institutional Review Board of Boston University, the Danish Health and Medicines Authority, and the Danish Data Protection Agency (record no. 2012-41-0841).
RESULTS
Table 1 displays the baseline characteristics of the stress diagnosis cohort and the comparison cohort. The majority of the cohort members were female, 55 years of age or younger, and never married. Those with stress diagnoses were approximately twice as likely to be divorced or separated as were members of the comparison group. Comorbid psychiatric diagnoses and a Charlson Comorbidity Index score higher than 1 were markedly more common among people with stress diagnoses than among members of the comparison cohort, and this pattern was consistent across the various stress diagnoses. Members of the stress diagnosis cohort experienced more traumatic events before their stress diagnoses than did members of the comparison cohort before the index date (Table 2). The most common experience among both members of the stress diagnosis cohort and members of the comparison group was injury from poisoning, with rates ranging from 1% of the comparison cohort to 16% of those with adjustment disorder. The least frequent event (<1%) among both members of the stress diagnosis cohort and members of the comparison group was abuse, neglect, or other maltreatment.
Table 1.
Baseline Characteristics of the Cohort Members, Denmark, 1995–2011
| Participant Characteristic | Type of Stress Diagnosis |
Comparison Cohort, % (n = 508,315) | ||||
|---|---|---|---|---|---|---|
| Acute Stress Reaction, % (n = 9,182) | PTSD, % (n = 3,786) | Adjustment Disorder, % (n = 66,823) | Other Reactions to Severe Stress, % (n = 1,692) | Reactions to Severe Stress, Unspecified, % (n = 20,180) | ||
| Sex | ||||||
| Female | 55.6 | 60.0 | 60.6 | 65.4 | 59.9 | 60.1 |
| Male | 44.4 | 40.0 | 39.4 | 34.6 | 40.1 | 39.9 |
| Age group, years | ||||||
| 16–30 | 36.2 | 34.7 | 36.4 | 39.5 | 37.4 | 36.1 |
| 31–55 | 50.6 | 54.0 | 47.4 | 45.2 | 47.0 | 47.8 |
| 56–70 | 9.7 | 8.2 | 10.5 | 10.5 | 10.5 | 10.4 |
| ≥71 | 3.5 | 3.0 | 5.7 | 4.8 | 5.0 | 5.3 |
| Marital status | ||||||
| Never married | 49.8 | 48.4 | 48.8 | 51.3 | 50.5 | 46.8 |
| Married | 30.7 | 33.1 | 29.9 | 29.0 | 29.8 | 41.9 |
| Divorced or separated | 15.0 | 14.6 | 15.6 | 15.7 | 14.9 | 7.5 |
| Widowed | 4.5 | 3.8 | 5.8 | 4.1 | 4.8 | 3.8 |
| Depression diagnoses | 16.3 | 23.4 | 18.4 | 21.2 | 18.7 | 1.2 |
| Anxiety disorder diagnoses | 5.2 | 10.3 | 5.7 | 7.5 | 6.0 | 0.6 |
| Alcohol abuse and dependence diagnoses | 10.1 | 8.1 | 11.2 | 10.2 | 9.8 | 0.8 |
| Drug abuse and dependence diagnoses | 2.7 | 2.6 | 3.1 | 2.5 | 2.6 | 0.2 |
| Charlson Comorbidity Index score >1 | 8.5 | 6.7 | 8.9 | 10.1 | 9.1 | 4.8 |
Abbreviation: PTSD, posttraumatic stress disorder.
Table 2.
Traumatic Events Coded Using the International Classification of Diseases, Tenth Revision, That Occurred Before Stress Diagnoses, Denmark, 1995–2011
| Traumatic Event | Type of Stress Diagnosis |
Comparison Cohort, % (n = 508,315) | ||||
|---|---|---|---|---|---|---|
| Acute Stress Reaction, % (n = 9,182) | PTSD, % (n = 3,786) | Adjustment Disorder, % (n = 66,823) | Other Reactions to Severe Stress, % (n = 1,692) | Reactions to Severe Stress, Unspecified, % (n = 20,180) | ||
| Accidents | 6.06 | 4.12 | 6.03 | 4.37 | 5.02 | 0.51 |
| Assaults | 1.47 | 1.61 | 0.53 | 0.65 | 1.20 | 0.17 |
| Injuries from poisoning | 15.18 | 10.14 | 16.19 | 14.66 | 14.19 | 1.02 |
| Abuse, neglect, and other maltreatment | 0.41 | 0.58 | 0.30 | 0.12 | 0.31 | 0.05 |
Abbreviation: PTSD, posttraumatic stress disorder.
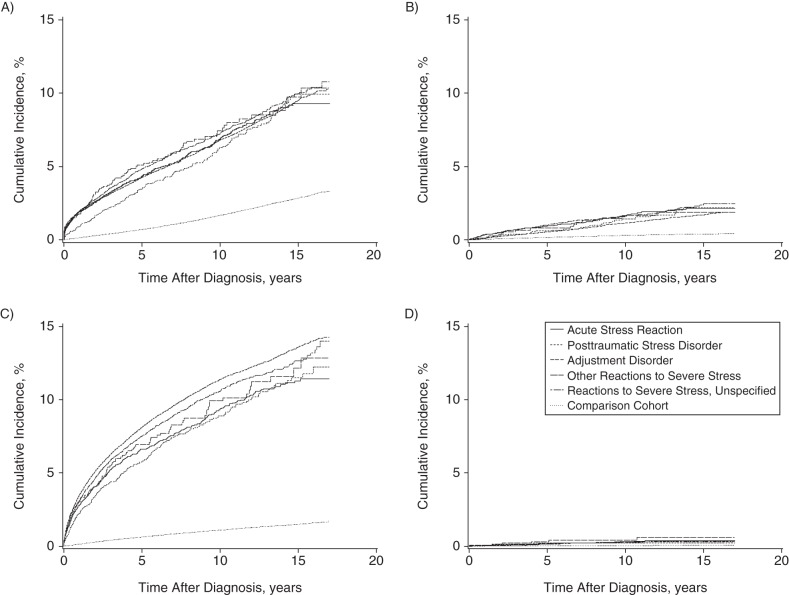
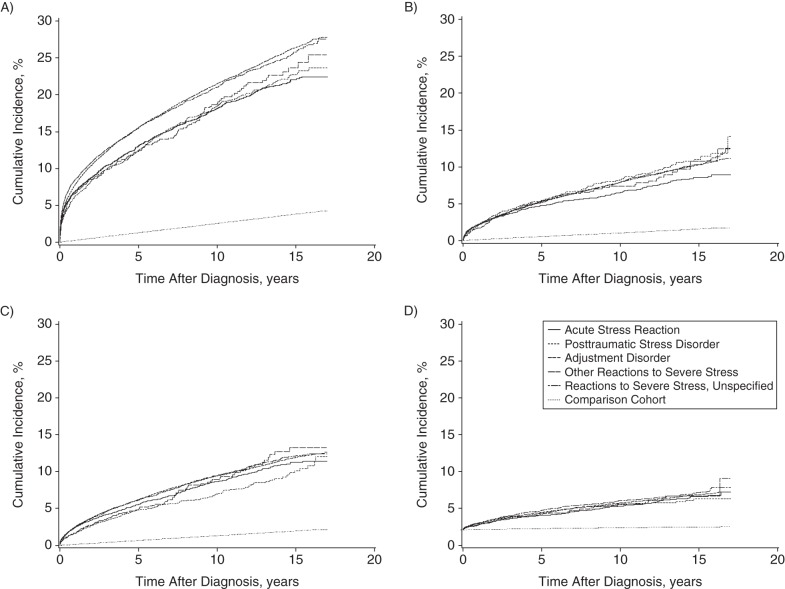
Subsequent trauma and comorbid diagnoses
The cumulative incidence curves displayed in Figure 1 show that members of the stress cohort had a higher incidence of traumatic events following their stress diagnosis than did members of the comparison cohort following their matched index date. These events included accidents, assaults, injuries from external causes, abuse, neglect, and other maltreatment. Similarly, there was a higher incidence of new-onset psychiatric diagnoses in 4 categories—depression, anxiety disorders, alcohol abuse and dependence, and drug abuse and dependence—in the stress diagnosis cohort than in the comparison cohort over the 15-year study period (Figure 2).
Figure 1.
Cumulative incidence curves for traumatic experiences following stress diagnoses (International Classification of Diseases, Tenth Revision), Denmark, 1995–2011. A) Accidents; B) assaults; C) injuries from poisoning or external causes; and D) abuse, neglect, and other maltreatment.
Figure 2.
Cumulative incidence curves for psychiatric diagnoses following stress diagnoses (International Classification of Diseases, Tenth Revision), Denmark, 1995–2011. A) Depression diagnoses; B) anxiety diagnoses; C) alcohol abuse and dependence diagnoses; and D) drug abuse and dependence diagnoses.
All-cause mortality
The incidence of all-cause mortality (excluding suicide) during the study period was 8% among persons with acute stress reaction, 8.1% among those with PTSD, 12% among those with adjustment disorder, 9.9% among those with other reactions to severe stress, 8.6% among those with unspecified reactions to severe stress, and 5.3% among the comparison cohort. Results of the regression analyses that we used to examine associations with all-cause mortality (excluding suicide) revealed that each stress disorder was associated with a mortality rate higher than that seen in the comparison cohort (Table 3), even after adjustment for baseline psychiatric disorders and Charlson Comorbidity Index score. Participants with acute stress reactions and those with other reactions to severe stress each had mortality rates during the study period that were 2.2 times higher than those in the comparison group (for acute stress reaction, 95% confidence interval: 1.9, 2.4; for other reactions to severe stress, 95% confidence interval: 1.7, 2.8). Although these associations were the strongest in magnitude of all those seen for the various stress disorders, the other disorders had a similar pattern of associations.
Table 3.
Associations of Stress Diagnoses With All-Cause Mortality and Suicide, Denmark, 1995–2011
| Cohort | No. | All-Cause Mortalitya |
Suicide |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted Rate Ratio | 95% CI | Adjusted Rate Ratiob | 95% CI | Unadjusted Rate Ratio | 95% CI | Adjusted Rate Ratiob | 95% CI | ||
| Stress diagnosis | |||||||||
| Acute stress reaction | 9,182 | 2.9 | 2.6, 3.2 | 2.2 | 1.9, 2.4 | 26 | 14, 49 | 24 | 10, 53 |
| PTSD | 3,786 | 2.2 | 1.9, 2.6 | 1.8 | 1.5, 2.1 | 19 | 7.6, 46 | 13 | 4.3, 42 |
| Adjustment disorder | 66,823 | 2.6 | 2.7, 2.9 | 1.9 | 1.8, 2.0 | 18 | 15, 21 | 12 | 9.8, 15 |
| Other reactions to severe stress | 1,692 | 2.9 | 2.3, 3.5 | 2.2 | 1.7, 2.8 | 25 | 5.4, 112 | 29 | 3.5, 244 |
| Reactions to severe stress, unspecified | 20,180 | 2.6 | 2.4, 2.8 | 2.0 | 1.9, 2.2 | 26 | 16, 41 | 19 | 12, 31 |
| Comparison cohort | 508,315 | 1.0 | Referent | 1.0 | Referent | 1.0 | Referent | 1.0 | Referent |
Abbreviations: CI, confidence interval; PTSD, posttraumatic stress disorder.
a Suicide deaths were excluded from the all-cause mortality analyses.
b All analyses were adjusted for baseline diagnoses of depression, anxiety, alcohol abuse and dependence, and drug abuse and dependence. All-cause mortality analyses were also adjusted for baseline Charlson Comorbidity Index score.
Death from suicide
The incidence of death from suicide over the study period was 0.63% among those with an acute stress reaction, 0.61% among those with PTSD, 0.78% among those with an adjustment disorder, 0.59% among those with other reactions to severe stress, 0.56% among those with unspecified reactions to severe stress, and 0.04% among members of the comparison cohort. Table 3 also displays both the unadjusted and adjusted associations of each stress disorder with suicide. Strong adjusted associations were found for each stress disorder, with rate ratios ranging from 12 (95% confidence interval: 9.8, 15) in persons with adjustment disorders to 29 (95% confidence interval: 3.5, 244) in those with other reactions to severe stress. Although there is variability in the magnitude of the associations between each stress disorder and death from suicide, all observed associations were large.
DISCUSSION
To our knowledge, this cohort study is the first in which the longitudinal courses of each of the diagnoses of reaction to severe stress and adjustment disorder with regard to subsequent traumatization, psychiatric diagnoses, all-cause mortality, and suicide have been examined. We found that over the 15-year study period, participants with a baseline stress diagnosis had a higher incidence rate of traumatic events than did the comparison group. This result is consistent with those from research examining sexual trauma, intimate-partner violence, and combat-related PTSD, in which an association between PTSD resulting from these events and subsequent traumatization has been found (2–6). The present study adds to this literature by demonstrating an association between stress disorders and a variety of subsequent traumatic experiences over a longer period of time than has been examined in previous studies.
Similarly, we found a higher incidence of new-onset psychiatric diagnoses—including depression, anxiety disorders, alcohol abuse and dependence, and drug abuse and dependence—in participants with baseline stress diagnoses than in a cohort without these diagnoses. This result is consistent with research that showed marked comorbidity between stress diagnoses and other psychiatric disorders, particularly depression, and research that suggested that depression and other psychiatric disorders might be additional sequelae of trauma (7–10). Our results extend this literature by demonstrating a higher incidence of comorbid psychiatric conditions following all stress diagnoses (as indicated by ICD-10 codes) over a longer follow-up period than previously examined.
We found that acute stress reaction, PTSD, adjustment disorder, other reactions to severe stress, and reactions to severe stress (unspecified) were all associated with a higher rate of all-cause mortality (excluding suicide) during the study period, even after adjustment for somatic and psychiatric comorbid conditions. This finding is somewhat consistent with research in US military veterans in which a higher risk of all-cause mortality was found among those diagnosed with PTSD (12–14), but it contradicts a study in which this association was found to be null after adjustment for relevant confounders (14). The difference in findings might be due to the examination of different populations or the ability in the previous research to adjust for variables that we could not account for in the current study because they are not available in coded medical record data (e.g., smoking and exercise). However, these additional confounders are likely associated with Charlson Comorbidity Index score, for which we accounted in our analyses, with increased smoking and decreased exercise resulting in poorer physical health. Therefore, the inclusion of these additional variables would likely not account for our observed associations entirely.
This study also revealed strong associations between stress disorders and suicide even after adjustment for baseline depression, anxiety, and substance abuse diagnoses. This work builds on previous case-control studies of suicide that also revealed strong associations between these disorders and suicide over a shorter follow-up period. Importantly, the associations found within the present study were much stronger in magnitude than those previously reported in case-control studies (15–17). A potential explanation for the differences in findings is the dramatic increase in the incidence of these disorders during the time frame of our study (2007), which postdated the time period of previous research (20).
It is worth noting that the 2 general diagnoses in this ICD-10 category—other reactions to severe stress and reactions to severe stress, unspecified—had associations with all-cause mortality and suicide that were similar in magnitude to those seen with the more stringently diagnosed disorders (e.g., PTSD). This equivalence highlights the importance of examining patients who meet subsyndromal criteria for diagnoses; their outcomes might be just as severe as those of patients who meet full diagnostic criteria. Further, this finding supports recent efforts to direct research toward examination of symptomatology and domains of functioning that span diagnoses rather than strict adherence to diagnostic criteria (e.g., Research Domain Criteria) (27).
Strengths of the current study include data from an unselected population with access to free health care, which is not subject to the selection biases that could affect studies that include only subsets of a population. Further, all data used in the current study were based on clinician assessment and diagnosis. Finally, all data were collected prospectively within the national registries, so they are not subject to the recall bias that limits studies using retrospective self-report.
Our study also has limitations. First, patients who had a stress diagnosis that was treated only by a general practitioner, and not by a psychiatrist or psychologist, were excluded from the analyses. These patients may have had milder cases of these disorders with etiologies and prognoses that differed from those in patients whose conditions were severe enough to cause them to seek psychiatric treatment. In addition, some people with stress and adjustment disorder diagnoses in the general population likely decline to seek medical treatment. Therefore, some persons with stress disorder could be missing from the present study, particularly those with mild or transient disorders (23). Second, it is unclear whether the results of the present study would be generalizable to populations of countries other than Denmark, which have different health care and social support systems for individuals dealing with psychiatric illness and different psychiatric diagnostic guidelines. However, our results are consistent with those in the broader literature to date on retraumatization, comorbid psychiatric conditions, all-cause mortality, and suicide involving US samples, indicating that the longitudinal trajectory of these disorders is likely similar across westernized countries (2–6, 9, 10, 12–14, 19). Last, the information on traumatic events experienced both before and after the stress diagnoses was limited to what would be medically coded and retained in the national Danish registries; it is likely that many traumatic experiences were not captured in our study. Further, we were unable to confirm that these events fully qualify as traumatic experiences according to diagnostic criteria (i.e., that they involved threatened death, actual or threatened serious injury, or actual or threatened sexual violence). Persons with stress disorders might also be more likely to report subsequent traumas to a health care provider or to be more closely monitored within the health care system than those without stress disorders. Additionally, there may be differential reporting of traumatic events based on type of trauma. Although this would not affect our regression results because death data were obtained separately from the health care system, the differences between the stress cohort and comparison cohort with regard to subsequent traumatization and psychiatric diagnoses may be smaller than what we have reported. Previous research has shown that detailed information on a range of traumatic experiences can be obtained from medical records (23); future research should use methodology that incorporates multiple sources of data to obtain a fuller picture of the stressful and traumatic events associated with these disorders.
In conclusion, the present study makes an important contribution to the literature on the longitudinal course of severe stress and adjustment disorder diagnoses, particularly with regard to the diagnoses that have been less commonly examined in the literature. The results support those from the literature to date that have shown the substantial burden of PTSD (11). We found that severe stress and adjustment disorder diagnoses were associated with increases in subsequent traumatic experiences, psychiatric diagnoses, all-cause mortality, and suicide, indicating that these disorders have long-lasting and potentially severe consequences. Future research should explore the mechanisms through which stress disorders and negative sequelae are associated, with the ultimate goal of informing interventions.
ACKNOWLEDGMENTS
Author affiliations: National Center for PTSD, VA Boston Healthcare System and Departments of Psychiatry and Epidemiology, Boston University, Boston, Massachusetts (Jaimie L. Gradus); Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark (Sussie Antonsen); Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark (Elisabeth Svensson); Department of Epidemiology, Emory University, Atlanta, Georgia (Timothy L. Lash); Departments of Psychiatry and Behavioral Sciences, Duke University, Durham, North Carolina (Patricia A. Resick); and Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark (Jens Georg Hansen).
This work was supported by a National Institute of Mental Health (grant 1R21MH094551-01A1) to J.L.G.
We thank Dóra Körmendiné Farkas, MSc, for her contribution to the analyses.
Conflict of interest: none declared.
REFERENCES
- 1.Janca A, Ustun TB, van Drimmelen J, et al. ICD-10 Symptom Checklist for Mental Disorders, Version 1.1. Geneva, Switzerland: Division of Mental Health, World Health Organization; 1994. [Google Scholar]
- 2.Risser HJ, Hetzel-Riggin MD, Thomsen CJ, et al. PTSD as a mediator of sexual revictimization: the role of reexperiencing, avoidance, and arousal symptoms. J Trauma Stress. 2006;195:687–698. [DOI] [PubMed] [Google Scholar]
- 3.Krause ED, Kaltman S, Goodman L, et al. Role of distinct PTSD symptoms in intimate partner reabuse: a prospective study. J Trauma Stress. 2006;194:507–516. [DOI] [PubMed] [Google Scholar]
- 4.Kimerling R, Alvarez J, Pavao J, et al. Epidemiology and consequences of women's revictimization. Womens Health Issues. 2007;172:101–106. [DOI] [PubMed] [Google Scholar]
- 5.Sandberg DA, Matorin AI, Lynn SJ. Dissociation, posttraumatic symptomatology, and sexual revictimization: a prospective examination of mediator and moderator effects. J Trauma Stress. 1999;121:127–138. [DOI] [PubMed] [Google Scholar]
- 6.Orcutt HK, Erickson DJ, Wolfe J. A prospective analysis of trauma exposure: the mediating role of PTSD symptomatology. J Trauma Stress. 2002;153:259–266. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;5212:1048–1060. [DOI] [PubMed] [Google Scholar]
- 8.Debell F, Fear NT, Head M, et al. A systematic review of the comorbidity between PTSD and alcohol misuse. Soc Psychiatry Psychiatr Epidemiol. 2014;499:1401–1425. [DOI] [PubMed] [Google Scholar]
- 9.Brady KT, Killeen TK, Brewerton T, et al. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61(suppl 7):22–32. [PubMed] [Google Scholar]
- 10.Shalev AY, Freedman S, Peri T, et al. Prospective study of posttraumatic stress disorder and depression following trauma. Am J Psychiatry. 1998;1555:630–637. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(suppl 5):4–12. [PubMed] [Google Scholar]
- 12.Boscarino JA. External-cause mortality after psychologic trauma: the effects of stress exposure and predisposition. Compr Psychiatry. 2006;476:503–514. [DOI] [PubMed] [Google Scholar]
- 13.Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army Veterans 30 years after military service. Ann Epidemiol. 2006;164:248–256. [DOI] [PubMed] [Google Scholar]
- 14.Chwastiak LA, Rosenheck RA, Desai R, et al. Association of psychiatric illness and all-cause mortality in the National Department of Veterans Affairs Health Care System. Psychosom Med. 2010;728:817–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gradus JL, Qin P, Lincoln AK, et al. Acute stress reaction and completed suicide. Int J Epidemiol. 2010;396:1478–1484. [DOI] [PubMed] [Google Scholar]
- 16.Gradus JL, Qin P, Lincoln AK, et al. The association between adjustment disorder diagnosed at psychiatric treatment facilities and completed suicide. Clin Epidemiol. 2010;2:23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gradus JL, Qin P, Lincoln AK, et al. Posttraumatic stress disorder and completed suicide. Am J Epidemiol. 2010;1716:721–727. [DOI] [PubMed] [Google Scholar]
- 18.Qin P. The impact of psychiatric illness on suicide: differences by diagnosis of disorders and by sex and age of subjects. J Psychiatr Res. 2011;4511:1445–1452. [DOI] [PubMed] [Google Scholar]
- 19.Ilgen MA, Bohnert ASB, Ignacio RV, et al. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. 2010;6711:1152–1158. [DOI] [PubMed] [Google Scholar]
- 20.Gradus JL, Bozi I, Antonsen S, et al. Severe stress and adjustment disorder diagnoses in the population of Denmark. J Trauma Stress. 2014;273:370–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Munk-Jørgensen P, Mortensen PB. The Danish Psychiatric Central Register. Dan Med Bull. 1997;441:82–84. [PubMed] [Google Scholar]
- 22.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7 Suppl):54–57. [DOI] [PubMed] [Google Scholar]
- 23.Svensson E, Lash TL, Resick PA, et al. Validity of reaction to severe stress and adjustment disorders diagnoses in the Danish Psychiatric Central Research Registry. Clin Epidemiol. 2015;7:235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 suppl):30–33. [DOI] [PubMed] [Google Scholar]
- 25.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;405:373–383. [DOI] [PubMed] [Google Scholar]
- 26.Thygesen SK, Christiansen CF, Christensen S, et al. The predictive value of ICD-10 diagnostic coding used to assess Charlson Comorbidity Index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;1677:748–751. [DOI] [PubMed] [Google Scholar]