Abstract
BACKGROUND
Financial problems caused by cancer and its treatment can substantially affect survivors and their families and create barriers to seeking health care.
METHODS
The authors identified cancer survivors diagnosed as adults (n = 1556) from the nationally representative 2010 National Health Interview Survey. Using multivariable logistic regression analyses, the authors report sociodemographic, clinical, and treatment-related factors associated with perceived cancer-related financial problems and the association between financial problems and forgoing or delaying health care because of cost. Adjusted percentages using the predictive marginals method are presented.
RESULTS
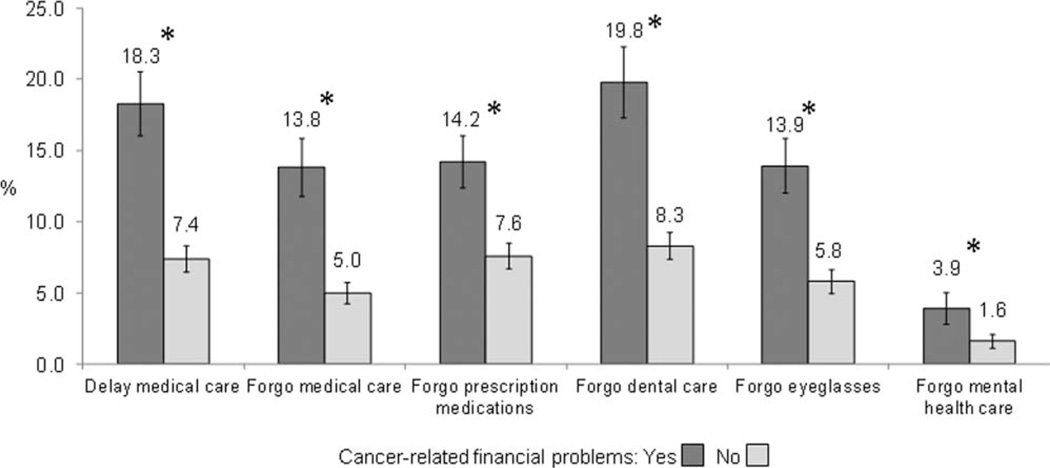
Cancer-related financial problems were reported by 31.8% (95% confidence interval, 29.3%–34.5%) of survivors. Factors found to be significantly associated with cancer-related financial problems in survivors included younger age at diagnosis, minority race/ethnicity, history of chemotherapy or radiation treatment, recurrence or multiple cancers, and shorter time from diagnosis. After adjustment for covariates, respondents who reported financial problems were more likely to report delaying (18.3% vs 7.4%) or forgoing overall medical care (13.8% vs 5.0%), prescription medications (14.2% vs 7.6%), dental care (19.8% vs 8.3%), eyeglasses (13.9% vs 5.8%), and mental health care (3.9% vs 1.6%) than their counterparts without financial problems (all P<.05).
CONCLUSIONS
Cancer-related financial problems are not only disproportionately represented in survivors who are younger, members of a minority group, and have a higher treatment burden, but may also contribute to survivors forgoing or delaying medical care after cancer.
Keywords: cancer, health disparities, survivors, access to care, financial burden
INTRODUCTION
The financial burden that cancer and its treatment poses to families can be substantial, including lost income, increased insurance premiums, deductibles, copayments, transportation costs, and childcare expenses.1 The impact of these costs may be exacerbated in low-income and minority survivors, for whom financial hardship may predate a cancer diagnoses,2 and in survivors who are at younger ages at the time of diagnosis.3 In addition to estimating the actual costs associated with cancer treatment for individual patients, it is also important to understand the financial burden of cancer from the perspectives of survivors themselves.4,5 Financial stress and strain in survivors have been linked to worse health-related quality of life6–9 and greater depression and anxiety.8
Health-related financial problems may be obstacles to preventive care or treatment. High treatment costs, including out-of-pocket medication costs, have been linked to lower adherence to cancer treatment.10,11 Delaying or forgoing care can have drastic consequences for patients undergoing cancer treatment, resulting in less effective treatment and shorter survival.12 Delaying or forgoing care may also affect surveillance for disease recurrence, screening for second cancers, and care for late and long-term effects of cancer treatment.13,14
In the current study, we used national data to characterize individuals with a history of cancer who reported cancer-related financial problems and examined the relationship between these problems and forgoing or delaying health care because of cost. Understanding those most financially affected by cancer is an important first step in identifying intervention strategies to prevent inadequate medical care, an increasingly important task given the growing number of cancer survivors living in the United States.15,16
MATERIALS AND METHODS
We used data from the 2010 National Health Interview Survey (NHIS), an in-person nationally representative survey of health and health behaviors in the United States.17 A sample of the civilian, noninstitutionalized population was derived using a complex, multistage sampling framework. One adult per household was chosen to complete the Sample Adult Questionnaire, which in 2010 included the Cancer Control Supplement and yielded a conditional response rate of 77.3% and a final response rate (accounting for household nonresponse) of 60.8%. Recent articles have used these data to characterize receipt of psychosocial care18 and health-related quality of life19 among cancer survivors. A total of 1822 individuals reported a history of any cancer (excluding nonmelanoma and unknown skin cancer). Survivors who were diagnosed only at an age <22 years (n = 52) were excluded due to differences in treatment settings for childhood and adolescent cancer and to focus on financial problems incurred for adult-onset cancers. Individuals with missing data regarding cancer-related financial problems (n = 214) and other covariates (n = 38) were also excluded, bringing the final analytic sample to 1556.
Measures
Cancer-related financial problems was based on the question “to what degree has cancer caused financial problems for you and your family?” Responses were dichotomized (a lot, some, a little vs none) to account for individual variability in perception of financial burden.
Forgoing or delaying care was based on affirmative responses to the following yes/no questions asked about the past 12 months (items in brackets were asked as separate questions):
“Was there any time when you needed (prescription medicines, mental health care or counseling, eyeglasses, dental care [including check-ups]), but couldn’t afford it?
“Was there any time when you needed medical care, but did not get it because you couldn’t afford it?”
“Has medical care been delayed for you because of worry about the cost?”
Covariates
Our analysis examined the relationship between cancer-related financial problems and the following self-reported factors: age at last cancer diagnosis (because available treatment data refer to the most recent cancer only); sex; marital status; race/ethnicity; education; whether health insurance paid for all or part of cancer treatment; residential region; recurrence or multiple cancers; time since most recent cancer diagnosis; history of surgery, chemotherapy, or radiation; and number of comorbidities. We used an index of non-cancer comorbid health conditions (ever diagnosed) based on previous research linking these conditions to poorer health-related quality of life: hypertension, heart disease, stroke, diabetes, lung disease, and arthritis.19,20 Although we report on household income at the time of survey in the description, we did not include income as a covariate in our analyses for multiple reasons: 1) neither income before cancer diagnosis nor change in income from the time of diagnosis to the survey was available in NHIS, making the association between cancerrelated financial problems and income difficult to interpret; 2) income was missing for approximately 25% of participants; and 3) income was found to be significantly correlated with educational status (r = 0.36; P<.001).
Statistical Analysis
Multivariable logistic regression modeling using the predictive marginals method was used to estimate the association between covariates and cancer-related financial problems.21 Analyses also investigated the possibility of individual interactions between health insurance coverage for treatment, race/ethnicity, history of chemotherapy and treatment, and comorbidities with age at last cancer diagnosis (<65 vs ≥65 years) to determine whether the associations between these variables and cancer-related financial problems differed by age, given documented higher rates of financial hardship among younger cancer survivors.3 Multivariable logistic regression was also conducted to assess whether self-reported cancer-related financial difficulties were associated with delaying or forgoing medical care (overall medical care, mental health care, eyeglasses, prescription medications, and dental care). This analysis only included individuals who reported not having received treatment within the previous 12 months (n = 1276) because the relationship between financial burden and delaying or forgoing care may differ for those still receiving cancer treatment. The analysis was adjusted for variables previously shown to be associated with forgoing or delaying care: age at last cancer diagnosis, sex, race/ethnicity, education, and comorbidities,22 as well as others included in the model of cancerrelated financial problems (marital status; whether insurance paid for cancer treatment; residential region; recurrence or multiple cancer history; years since last cancer diagnosis; and history of surgery, chemotherapy, or radiation). Weighted percentages represent the population percentage of each group reporting cancer-related financial problems after covariate adjustment. An analysis comparing variables for those missing and not missing data regarding cancer-related financial problems was conducted to examine nonresponse bias. Analyses were conducted using the Statistical Analysis Software (SAS) callable version (SAS Institute Inc, Cary, NC) of SUDAAN 10.0 (RTI International, Research Triangle Park, NC) to incorporate sampling weights and account for the complex sampling design. Statistical analyses were deemed significant for a 2-sided test P values of <.05.
RESULTS
Sample Characteristics
Approximately 19.5% of the survivor sample was aged ≤39 years at the time of the most recent cancer diagnosis, 50.5% were aged 40 years to 64 years, and 29.9% were aged ≥65 years (Table 1). Reflective of previous population-based studies of US cancer survivors,16,23 greater than one-half of the participants were female, married/living as married, and reported some college education. Most survivors were non-Hispanic white. Although the majority of participants reported a household income (at time of survey) >200% of the federal poverty level (adjusted for household size), 8.0% reported an income of <100% of the federal poverty level. Approximately 7.0% of participants reported that their cancer treatment was not covered by insurance. Approximately 18.2% of survivors reported having experienced a cancer recurrence or multiple cancers and 14.6% reported having received treatment within the past 12 months. Surgical treatment was reported by 62.6% of participants; 23.0% reported receiving chemotherapy and 24.6% reported receiving radiation. Approximately 48.0% of participants reported 2 or more comorbidities.
TABLE 1.
Characteristics of Survivors of Adult Cancers in the United States (n = 1770)
| Variable | Level | No. | Weighted % | 95% CI |
|---|---|---|---|---|
| Age at last cancer diagnosis, y | <39 | 335 | 19.5 | 17.2–22.0 |
| 40–64 | 883 | 50.5 | 47.6–53.4 | |
| ≥65 | 552 | 29.9 | 27.4–32.6 | |
| Sex | Male | 664 | 42.1 | 39.4–44.9 |
| Female | 1106 | 57.9 | 55.1–60.6 | |
| Race/ethnicity | Non-Hispanic white | 1297 | 83.0 | 81.2–84.6 |
| Non-Hispanic black | 241 | 8.3 | 7.1–9.6 | |
| Hispanic | 164 | 6.0 | 5.0–7.1 | |
| Other | 68 | 2.8 | 2.1–3.8 | |
| Marital status | Married/living as married | 858 | 63.5 | 60.9–65.9 |
| Never married/widowed/divorced/separated | 911 | 36.5 | 34.1–39 | |
| Data missing | 1 | 0 | 0–0.3 | |
| Education | <High school | 296 | 13.5 | 11.8–15.5 |
| High school/GED | 484 | 28.7 | 26.2–31.3 | |
| Some college+ | 980 | 57.3 | 54.5–60.1 | |
| Data missing | 10 | 0.4 | 0.2–0.9 | |
| Current household income (% of federal poverty level)a | 100% | 217 | 8.0 | 6.8–9.5 |
| 100–199% | 326 | 16.3 | 14.4–18.4 | |
| 200–399% | 466 | 28.0 | 25.5–30.8 | |
| ≥400% | 512 | 33.2 | 30.6–35.9 | |
| Data missing | 249 | 14.4 | 12.6–16.5 | |
| Insurance paid for all or part of cancer treatment | Yes | 1365 | 77.8 | 75.4–80.0 |
| No | 145 | 7.0 | 5.8–8.4 | |
| Unknown/data missing | 260 | 15.2 | 13.2–17.4 | |
| Region | Northeast | 299 | 18.4 | 16.0–21.0 |
| Midwest | 436 | 25.4 | 23–27.9 | |
| South | 637 | 35.7 | 32.9–38.6 | |
| West | 398 | 20.5 | 18.2–23.1 | |
| Most recent cancer site | Female breast | 398 | 19.9 | 17.8–22.2 |
| Prostate | 260 | 15.5 | 13.8–17.4 | |
| Melanoma | 147 | 10.1 | 8.6–11.8 | |
| Colorectal | 142 | 7.6 | 6.3–9.2 | |
| Hematologic | 99 | 6.1 | 4.9–7.7 | |
| Short-survival cancersb | 102 | 5.6 | 4.6–7.0 | |
| All other | 539 | 30.5 | 28.2–32.8 | |
| Unknown | 83 | 4.6 | 3.6–5.9 | |
| Recurrence/ multiple cancers | Yes | 309 | 18.2 | 16.4–20.2 |
| No | 1461 | 81.8 | 79.8–83.6 | |
| Recent treatment (past 12 mo) | Yes | 262 | 14.6 | 12.8, 16.7 |
| No | 1362 | 76.8 | 74.3–79.0 | |
| Data missing | 146 | 8.6 | 7.1–10.3 | |
| Y since most recent diagnosis | <2 | 341 | 19.0 | 17.0–21.2 |
| 2–5 | 473 | 28.6 | 26.1–31.2 | |
| 6–9 | 270 | 15.1 | 13.0–17.5 | |
| ≥10 | 686 | 37.3 | 34.7–40 | |
| Surgery | Yes | 1111 | 62.6 | 59.7–65.4 |
| No | 489 | 27.3 | 24.9–29.9 | |
| Data missing | 170 | 10.1 | 8.5–11.9 | |
| Chemotherapy | Yes | 411 | 23.0 | 20.9–25.3 |
| No | 1189 | 66.9 | 64.3–69.5 | |
| Data missing | 170 | 10.1 | 8.5–11.9 | |
| Radiation | Yes | 445 | 24.6 | 22.3–27.1 |
| No | 1155 | 65.3 | 62.7–67.8 | |
| Data missing | 170 | 10.1 | 8.5–11.9 | |
| Noncancer comorbidities | 0 | 394 | 23.9 | 21.8–26.1 |
| 1 | 479 | 27.2 | 24.7–29.7 | |
| ≥2 | 881 | 48.0 | 45.3–50.8 | |
| Data missing | 16 | 0.9 | 0.5–1.7 | |
| Cancer-related financial problems | Yes | 574 | 31.8 | 29.3–34.5 |
| No | 1024 | 57.9 | 55.1–60.7 | |
| Data missing | 172 | 10.2 | 8.7–12.1 |
Abbreviations: 95% CI, 95% confidence interval; GED, General Educational Development test; Y, years.
Current household income (percentage of the federal poverty level) was calculated by comparing reported household income with the 2010 federal poverty level (eg, $22,050 for a family of 4).21
Short-survival cancers included cancers with a relatively short survival time (esophagus, liver, lung, pancreas, and stomach).17
Approximately 31.8% of survivors reported cancer-related financial problems. Participants missing a response to the cancer-related financial problems item were more likely to have undergone cancer treatment that was not covered by health insurance, to not have experienced a recurrence or have multiple cancers, and to have reported a lower household income at the time of the survey (all P < .05).
Cancer-Related Financial Problems
Age, race/ethnicity, time since diagnosis, recurrence or multiple cancers, and history of chemotherapy or radiation were all found to be significantly associated with cancer-related financial problems in multivariable analyses (Table 2). Specifically, 43.4% of survivors aged <40 years at the time of diagnosis and 39.8% of individuals aged 40 years to 64 years reported financial problems, compared with 21.7% of individuals aged ≥65 years (P < .0001). Minority survivors (non-Hispanic black: 46.6%; Hispanic: 42.1%; and other racial/ethnic background: 46.1%) were more likely to report financial problems than non-Hispanic white survivors (33.1%; P = 0.006). Survivors reporting disease recurrence or multiple cancers were also more likely to report cancer-related financial problems (40.9% vs 33.7%; P < .049). Survivors reporting a history of chemotherapy (47.2% vs 30.8%; P < .0001) and radiation (44.7% vs 31.4%; P < .001) were more likely to report financial problems. None of the interaction terms (health insurance coverage for treatment, race/ethnicity, history of chemotherapy or radiation, or comorbidities) with age was found to be significantly associated with cancer-related financial problems (data not shown).
TABLE 2.
Factors Associated With Cancer Survivors Reporting That Cancer Caused Them Financial Problems (n = 1556)a
| Factor | Predictive Marginal (%)b | 95% CI | Wald Pc | |
|---|---|---|---|---|
| Age at last cancer diagnosis, y | ≤39 | 43.4 | 36.9–50.2 | <.0001 |
| 40–64 | 39.8 | 35.8–44.0 | ||
| ≥65 | 21.7 | 17.9–26.0 | ||
| Sex | Male | 36.1 | 31.8–40.7 | .58 |
| Female | 34.5 | 30.9–38.3 | ||
| Marital status | Married or living with partner | 35.8 | 32.0–39.8 | .53 |
| Never married/widowed/divorced/separated | 34.1 | 30.3–38.1 | ||
| Race/ethnicity | Non-Hispanic white | 33.1 | 29.9–36.5 | 0.006 |
| Non-Hispanic black | 46.6 | 38.4–55.0 | ||
| Hispanic | 42.1 | 32.2–52.7 | ||
| Other | 46.1 | 30.8–62.1 | ||
| Education | <High school | 40.2 | 33.3–47.6 | .17 |
| High school or GED | 37.3 | 32.2–42.7 | ||
| Some college+ | 33.0 | 29.2–37.1 | ||
| Insurance paid for all or part of cancer treatment | Yes | 34.8 | 31.7–38.1 | .51 |
| No/unknown | 37.5 | 30.4–45.1 | ||
| Region | Northeast | 29.3 | 24.4–34.8 | .09 |
| Midwest | 36.2 | 30.0–42.8 | ||
| South | 38.7 | 33.5–44.2 | ||
| West | 32.8 | 27.6–38.5 | ||
| Recurrence/multiple cancers | Yes | 40.9 | 34.4–47.7 | .049 |
| No | 33.7 | 30.6–37.0 | ||
| Y since last cancer diagnosis | <2 | 45.2 | 37.4–53.2 | <.0001 |
| 2–5 | 40.0 | 34.9–45.4 | ||
| 6–9 | 34.7 | 28.4–41.5 | ||
| ≥10 | 27.9 | 24.1–31.9 | ||
| Surgery | Yes | 34.5 | 31.2–38.0 | .48 |
| No | 36.6 | 31.7–41.8 | ||
| Chemotherapy | Yes | 47.2 | 41.1–53.5 | <.0001 |
| No | 30.8 | 27.6–34.1 | ||
| Radiation | Yes | 44.7 | 39.0–50.6 | <.001 |
| No | 31.4 | 28.2–34.9 | ||
| No. of comorbidities | 0 | 32.5 | 27.8–37.6 | .51 |
| 1 | 35.5 | 30.1–41.2 | ||
| ≥2 | 36.4 | 32.1–40.8 |
Abbreviations: 95% CI, 95% confidence interval; GED, General Educational Development test; Y, years.
Adjusted r2 = 0.16.
Predictive marginals adjust for all other variables in the model and are weighted to account for the complex sampling design.
Bold type indicates statistical significance.
Delaying or Forgoing Care
After adjustment for covariates, participants who reported financial problems were more likely to report delaying medical care (18.1% vs 7.4%; P < .0001) or forgoing overall medical care (13.5% vs 5.1%; P < .0001), prescription medications (13.8% vs.7.7%; P = .001), dental care (20.0% vs 8.3%; P < .0001), eyeglasses (13.7% vs 5.9%; P < .0001), or mental health care (9.4% vs 7.1%; P = .03) (Fig. 1).
Figure 1.
The percentage of survivors reporting forgoing or delaying care because of cost who also reported that cancer caused them financial problems is shown, adjusted for other covariates (age at last cancer diagnosis; sex; marital status; race/ethnicity; education; whether insurance paid for cancer treatment; residential region; recurrence or multiple cancer history; years since last cancer diagnosis; history of surgery, chemotherapy, or radiation; and number of comorbidities). Only survivors who reported not receiving cancer care within the previous 12 months (n = 1276) were included. *P < .05.
DISCUSSION
In what to our knowledge is one of the first national studies on this topic, we observed that nearly one-third of adult cancer survivors reported cancer-related financial problems. The results of the current study elucidate several factors that are significantly associated with financial burden, including younger age at diagnosis and minority race/ethnicity. In addition, clinical factors that may be indicators of a greater cancer impact (including a history of chemotherapy or radiation treatment, recurrence, and shorter time from diagnosis) also emerged as important correlates to financial burden. Survivors reporting financial problems were more likely to report forgoing or delaying recent medical care, prescription medications, dental care, eyeglasses, or mental health care within the past year, specifically because of concerns about cost. The association between these 2 variables is striking because the majority of survivors in the study were >5 years beyond their most recent cancer diagnosis.
Expenditures attributable to cancer, including out-of-pocket spending, can be substantial, even for long-term survivors.23,24 As shown in the current study and others,25 survivors who are of working age at the time of diagnosis (broadly aged <65 years) may be at particular risk for financial problems, with 40% to 43% reporting cancer-related financial problems. Racial disparities in cancer-related financial problems have been reported in other studies of African American22 and Hispanic/Latino26 survivors. Studies have found higher treatment costs for racial/ethnic minority cancer patients, which suggest that inequitable cost burden may contribute to disparities in cancer-related financial problems.27–29 The lack of difference in financial problems between married and unmarried survivors in the current study is surprising given research documenting the financial protections associated with marriage30,31; this may suggest that marriage-related financial protection is outweighed by other factors, or it may be an artifact due to the finding that marital status was collected at the time of the interview, not diagnosis. Future interventions for survivors experiencing financial difficulties should consider predisposing factors such as race/ethnicity, time since diagnosis, and age.
The association between radiation history and financial problems is a novel finding and may reflect the out-of-pocket costs (travel and lost productivity, as well as possibly accommodations for survivors who live far from treatment centers) associated with sometimes long-lasting and daily treatment. Alternatively, it may reflect the lasting or late-onset health effects that therapeutic radiation can cause in survivors,32 as has been shown for chemotherapy.10,33 Recurrence or multiple cancer diagnoses present major financial challenges to survivors, often requiring additional time away from employment, added out-of-pocket expenditures, and a potential threat to their ability to maintain health insurance (possibly as a result of job loss). Although an observed lower likelihood of financial problems in longer-term survivors was evident in the current study, other studies have documented the persistence of severe financial problems (although not specifically cancer-related) well into posttreatment survivorship.34
Building on a prior analysis that found higher rates of forgoing medical care among individuals with a history of cancer (7.8%) compared with those without cancer (5.2%),22 the results of the current study add that among survivors, patients reporting cancer-related financial problems also are more likely to forgo or delay their current medical care. This suggests that difficulties accessing care appear to be related specifically to cancer-related financial variables. Another population-based study found that survivors of a younger age and lower household income and those who were unemployed were more likely to report treatment nonadherence,10 suggesting that financial challenges may compromise cancer outcomes. Given that higher treatment burden (ie, receiving either more intensive, more frequent, or longer-in-duration treatment) and recurrence are associated with a higher propensity for both serious and lasting late effects and perceived financial burden, the association between forgoing or delaying medical care and previous chemotherapy or radiation treatment is concerning. The importance of these findings is further enhanced given the potential for financial problems to affect the entire family system of cancer patients.35,36
The development of interventions to aid cancer survivors and their families as they confront financial stress is challenging, in part because it entails expansion of existing models of survivorship care as well as multilevel intervention efforts. Key challenges to identifying survivors in financial distress include a lack of standardized methods to assess need and the necessity of accounting for changing needs over time.37 A recently proposed model of cancer rehabilitation that recognizes the need for comprehensive care, including attention to social and vocational needs, suggests that expanding survivorship care to include services that both promote self-management and encourage survivors to remain or return to the workforce has the potential to reduce overall cancer costs as well as costs to individual survivors38 and should be considered as a way to reduce financial burden.
The current study is limited by its cross-sectional data and cannot provide causal inferences regarding the association between financial problems and forgoing medical care. The NHIS is designed to be representative of the general US population but may differ somewhat in terms of its generalizability to members of the US population with a history of cancer. In addition, the NHIS relies on self-reported cancer diagnoses, which may account for different prevalence estimates of cancer observed based on NHIS data compared with registry data.15 Participants may have mistakenly included preclinical lesions; however, it is unlikely that a large percentage of these individuals would also report financial problems. As a result, our estimates may understate the prevalence of financial problems.
Given the cross-sectional nature of the data in the current study, the often large gap in time between cancer diagnosis and income assessment, and the strong connection between income and financial burden, we chose not to examine whether cancer-related financial problems were more common among survivors who report low income; however, other studies have reported higher perceived financial burden among low-income cancer patients.10,39,40 In addition, income and educational attainment were found to be associated in our data set, and we believe that the latter was a more stable predictor of socioeconomic status and was less affected by missing data.
The sample in the current study is widely representative of the general US population of cancer survivors, but it may underrepresent certain groups. For example, the approximately 10% of survivors who did not respond to the question regarding financial problems tended to be uninsured and poorer, and given that individuals in poorer health are less likely to respond to the NHIS,41 the current study may have underestimated financial burden. Finally, financial burden was assessed with a single item that may have been variably interpreted by participants and warrants further exploration. Cognitive testing of this question, however, did not reveal any difficulties in interpretation. Future qualitative research to help elucidate those factors individuals consider as financial difficulties as the result of their cancer experience is needed. Regardless, the results of the current study provide nationally representative population-based estimates of the prevalence of this easily interpretable measure, and subjective financial burden has been significantly associated with objective measures, such as requesting copayment assistance.3 Future studies that incorporate objective measures in addition to patient perceptions, such as changes in income and employment, would help to further classify and quantify the financial effects of cancer.
The current study found that approximately one-third of cancer survivors in the United States report cancer-related financial problems and that these problems are associated with an increased likelihood of forgoing or delaying medical care. Future research should investigate whether certain survivor groups (eg, younger survivors, those of minority racial/ethnic status, and those with a higher treatment burden) are less likely to receive guideline-based follow-up and routine preventive care. When possible, future studies should also use longitudinal study designs, such as those found in the Agency for Healthcare Research and Quality’s Medical Expenditure Panel Survey,42 to examine economic trajectories of survivors and their caregivers and to examine whether cancer survivors who receive inadequate care because of cost experience worse health outcomes.
Acknowledgments
FUNDING SUPPORT
No specific funding was disclosed.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Cancer Institute, the Centers for Disease Control and Prevention, or the Patient-Centered Outcomes Research Institute.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
REFERENCES
- 1.Wagner L, Lacey MD. The hidden costs of cancer care: an overview with implications and referral resources for oncology nurses. Clin J Oncol Nurs. 2004;8:279–287. doi: 10.1188/04.CJON.279-287. [DOI] [PubMed] [Google Scholar]
- 2.Shelton RC, Goldman RE, Emmons KM, Sorensen G, Allen JD. An investigation into the social context of low-income, urban Black and Latina women: implications for adherence to recommended health behaviors. Health Educ Behav. 2011;38:471–481. doi: 10.1177/1090198110382502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18:381–390. doi: 10.1634/theoncologist.2012-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fryback DG, Craig BM. Measuring economic outcomes of cancer. J Natl Cancer Inst Monogr. 2004;33:134–141. doi: 10.1093/jncimonographs/lgh018. [DOI] [PubMed] [Google Scholar]
- 5.Simmons LA. Self-perceived burden in cancer patients: validation of the Self-perceived Burden Scale. Cancer Nurs. 2007;30:405–411. doi: 10.1097/01.NCC.0000290816.37442.af. [DOI] [PubMed] [Google Scholar]
- 6.Gupta D, Lis CG, Grutsch JF. Perceived cancer-related financial difficulty: implications for patient satisfaction with quality of life in advanced cancer. Support Care Cancer. 2007;15:1051–1056. doi: 10.1007/s00520-007-0214-2. [DOI] [PubMed] [Google Scholar]
- 7.Rogers SN, Harvey-Woodworth CN, Hare J, Leong P, Lowe D. Patients’ perception of the financial impact of head and neck cancer and the relationship to health related quality of life. Br J Oral Maxillofac Surg. 2012;50:410–416. doi: 10.1016/j.bjoms.2011.07.026. [DOI] [PubMed] [Google Scholar]
- 8.Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology. 2013;22:745–755. doi: 10.1002/pon.3055. [DOI] [PubMed] [Google Scholar]
- 9.Meneses K, Azuero A, Hassey L, McNees P, Pisu M. Does economic burden influence quality of life in breast cancer survivors? Gynecol Oncol. 2012;124:437–443. doi: 10.1016/j.ygyno.2011.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shankaran V, Jolly S, Blough D, Ramsey SD. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: a population-based exploratory analysis. J Clin Oncol. 2012;30:1608–1614. doi: 10.1200/JCO.2011.37.9511. [DOI] [PubMed] [Google Scholar]
- 11.Sedjo RL, Devine S. Predictors of non-adherence to aromatase inhibitors among commercially insured women with breast cancer. Breast Cancer Res Treat. 2011;125:191–200. doi: 10.1007/s10549-010-0952-6. [DOI] [PubMed] [Google Scholar]
- 12.Byers TE, Wolf HJ, Bauer KR, et al. The impact of socioeconomic status on survival after cancer in the United States: findings from the National Program of Cancer Registries Patterns of Care Study. Cancer. 2008;113:582–591. doi: 10.1002/cncr.23567. [DOI] [PubMed] [Google Scholar]
- 13.Sabatino SA, Thompson TD, Richardson LC, Miller J. Health insurance and other factors associated with mammography surveillance among breast cancer survivors: results from a national survey. Med Care. 2012;50:270–276. doi: 10.1097/MLR.0b013e318244d294. [DOI] [PubMed] [Google Scholar]
- 14.Brewster AM, Hortobagyi GN, Broglio KR, et al. Residual risk of breast cancer recurrence 5 years after adjuvant therapy. J Natl Cancer Inst. 2008;100:1179–1183. doi: 10.1093/jnci/djn233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Cancer Society. Atlanta, GA: American Cancer Society; 2012. Cancer Treatment & Survivorship Facts & Figures 2012–2013. [Google Scholar]
- 16.Parry C, Kent EE, Mariotto AB, Alfano CM, Rowland JH. Cancer survivors: a booming population. Cancer Epidemiol Biomarkers Prev. 2011;20:1996–2005. doi: 10.1158/1055-9965.EPI-11-0729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. National Health Interview Survey (NHIS) Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Accessed January 15, 2013]. www.cdc.gov/nchs/nhis.htm. [Google Scholar]
- 18.Forsythe LP, Kent EE, Weaver KE, et al. Receipt of psychosocial care among cancer survivors in the United States. J Clin Oncol. 2013;31:1961–1969. doi: 10.1200/JCO.2012.46.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weaver KE, Forsythe LP, Reeve BB, et al. Mental and physical health-related quality of life among U.S. cancer survivors: population estimates from the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2012;21:2108–2117. doi: 10.1158/1055-9965.EPI-12-0740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith AW, Reeve BB, Bellizzi KM, et al. Cancer, comorbidities, and health-related quality of life of older adults. Health Care Financing Rev. 2008;29:41–56. [PMC free article] [PubMed] [Google Scholar]
- 21.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55:652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 22.Weaver KE, Rowland JH, Bellizzi KM, Aziz NM. Forgoing medical care because of cost: assessing disparities in healthcare access among cancer survivors living in the United States. Cancer. 2010;116:3493–3504. doi: 10.1002/cncr.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Short PF, Moran JR, Punekar R. Medical expenditures of adult cancer survivors aged <65 years in the United States. Cancer. 2011;117:2791–2800. doi: 10.1002/cncr.25835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pisu M, Azuero A, McNees P, Burkhardt J, Benz R, Meneses K. The out of pocket cost of breast cancer survivors: a review. J Cancer Surviv. 2010;4:202–209. doi: 10.1007/s11764-010-0125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finkelstein EA, Tangka FK, Trogdon JG, Sabatino SA, Richardson LC. The personal financial burden of cancer for the working-aged population. Am J Managed Care. 2009;15:801–806. [PubMed] [Google Scholar]
- 26.Ell K, Xie B, Wells A, Nedjat-Haiem F, Lee PJ, Vourlekis B. Economic stress among low-income women with cancer: effects on quality of life. Cancer. 2008;112:616–625. doi: 10.1002/cncr.23203. [DOI] [PubMed] [Google Scholar]
- 27.Chirikos TN, Roetzheim RG, McCarthy EP, Iezzoni LI. Cost disparities in lung cancer treatment by disability status, sex, and race. Disabil Health J. 2008;1:108–115. doi: 10.1016/j.dhjo.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jayadevappa R, Malkowicz SB, Chhatre S, Gallo J, Schwartz JS. Racial and ethnic variation in health resource use and cost for prostate cancer. BJU Int. 2010;106:801–808. doi: 10.1111/j.1464-410X.2010.09227.x. [DOI] [PubMed] [Google Scholar]
- 29.Pisu M, Azuero A, Meneses K, Burkhardt J, McNees P. Out of pocket cost comparison between Caucasian and minority breast cancer survivors in the Breast Cancer Education Intervention (BCEI) Breast Cancer Res Treat. 2011;127:521–529. doi: 10.1007/s10549-010-1225-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pezzin LE, O’Niel MB, Nattinger AB. The economic consequences of breast cancer adjuvant hormonal treatments. J Gen Intern Med. 2009;24(suppl 2):S446–S450. doi: 10.1007/s11606-009-1079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Waldron I, Hughes ME, Brooks TL. Marriage protection and marriage selection-prospective evidence for reciprocal effects of marital status and health. Soc Sci Med. 1996;43:113–123. doi: 10.1016/0277-9536(95)00347-9. [DOI] [PubMed] [Google Scholar]
- 32.Carver JR, Shapiro CL, Ng A, et al. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol. 2007;25:3991–4008. doi: 10.1200/JCO.2007.10.9777. [DOI] [PubMed] [Google Scholar]
- 33.Brooks J, Wilson K, Amir Z. Additional financial costs borne by cancer patients: a narrative review. Eur J Oncol Nurs. 2011;15:302–310. doi: 10.1016/j.ejon.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 34.Darby K, Davis C, Likes W, Bell J. Exploring the financial impact of breast cancer for African American medically underserved women: a qualitative study. J Health Care Poor Underserved. 2009;20:721–728. doi: 10.1353/hpu.0.0176. [DOI] [PubMed] [Google Scholar]
- 35.Carey M, Paul C, Cameron E, Lynagh M, Hall A, Tzelepis F. Financial and social impact of supporting a haematological cancer survivor. Eur J Cancer Care. 2012;21:169–176. doi: 10.1111/j.1365-2354.2011.01302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mathews M, Park AD. Identifying patients in financial need: cancer care providers’ perceptions of barriers. Clin J Oncol Nurs. 2009;13:501–505. doi: 10.1188/09.CJON.501-505. [DOI] [PubMed] [Google Scholar]
- 38.Alfano CM, Ganz PA, Rowland JH, Hahn EE. Cancer survivorship and cancer rehabilitation: revitalizing the link. J Clin Oncol. 2012;30:904–906. doi: 10.1200/JCO.2011.37.1674. [DOI] [PubMed] [Google Scholar]
- 39.Longo CJ, Fitch M, Deber RB, Williams AP. Financial and family burden associated with cancer treatment in Ontario, Canada. Support Care Cancer. 2006;14:1077–1085. doi: 10.1007/s00520-006-0088-8. [DOI] [PubMed] [Google Scholar]
- 40.Langa KM, Fendrick AM, Chernew ME, Kabeto MU, Paisley KL, Hayman JA. Out-of-pocket health-care expenditures among older Americans with cancer. Value Health. 2004;7:186–194. doi: 10.1111/j.1524-4733.2004.72334.x. [DOI] [PubMed] [Google Scholar]
- 41.Dalhamer JM, Simile CM. Subunit nonresponse in the National Health Interview Survey (NHIS): an exploration using paradata. Joint Statistical Meeting: Section on Government Statistics. Proceedings of the Joint Statistical Meetings; 2009; Washington, DC. pp. 262–276. [Google Scholar]
- 42.Yabroff KR, Dowling E, Rodriguez J, et al. The Medical Expenditure Panel Survey (MEPS) experiences with cancer survivorship supplement. J Cancer Surviv. 2012;6:407–419. doi: 10.1007/s11764-012-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]