Abstract
Background
The Surgical Safety Checklist (SSC) is a tool developed by the World Health Alliance for Patient Safety, to assist health professionals in improving patient safety during surgery. Numerous specialties have incorporated this into their clinical practice. The purpose of this study is to adapt and implement this tool within the field of podiatric surgery and to evaluate its impact upon safety standards and post-surgical complications.
Methods
An analytical, observational, longitudinal study has been performed retrospectively. The implementation of the Surgical Safety Checklist in podiatric surgery took place over a 10-month period. The sample is made up from the medical histories of patients who were operated on (n = 134) in the University of Seville’s podiatric clinic. The sample was divided into three groups: those prior to the implementation process (65 subjects), those after the implementation process: without the SSC (35 subjects) and those with the SSC (34 subjects). The safety standards included in the tool were analysed in conjunction with the results and post-operative complications.
Results
An improvement was seen in compliance with the Prophylaxis Protocol and the correct completion of the Informed Consent (p = 0.00), as well as a statistically significant relationship between the correct use of antibiotic prophylaxis and the use of the Surgical Safety Checklist (p = 0.049). The results demonstrate a reduction in the number of post-operative days (p = 0.012). No cases of surgery being performed in the wrong place were found in this study.
Conclusions
The Surgical Safety Checklist allows us to improve compliance with the safety protocols recommended by the scientific community, and consequently to reduce the incidence of complications related to surgery and to improve patient safety during elective podiatric surgery.
Background
Patient Safety has been discussed since the Aristotelian principle “primum non nocere” but it is still highly relevant today and has gained strength since the creation of the World Alliance for Patient Safety [1].
Finding the cause of adverse events in healthcare and a means of reducing their occurrence is a cause for concern for healthcare professionals and managers. The first publication that highlighted healthcare-related adverse events, and as such, sparked interest in offering safer healthcare and correctly identifying any adverse events in the sector was the Institute of Medicine’s (IOM) 1999 publication ‘To err is human: building a safer health system’ [2]. This estimated that between 44,000 and 98,000 people die every year as a result of medical errors in the United States.
Other studies suggest that the incidence rate is between 2.9 and 16.6 [3–6]. The highest incidence of adverse events is registered in surgical specialities [7].
Given these figures, the World Alliance for Patient Safety outlines specific bi-annual goals. The Surgical Safety Checklist (SSC) has been developed from two projects which they have carried out: “Clean Care is Safer Care” [8] and “Safe Surgery Saves Lives” [1]. It is an easy-to-use, measurable set of safety checks, adaptable to different healthcare settings.
It is well-known that fatigue, stress and the development of complex procedures reduces the precision and speed of the human memory [9, 10]. These studies demonstrate the utility of checklists as a safe and useful tool to help minimise human error.
De Vries [11] introduced a checklist encompassing a patient’s complete medical history. This was later adapted by other authors, including Boscá et al. [12] for use in interventional radiology, and Perea et al. [13] to dental surgery.
There are few studies related to patient safety in the field of podiatry. Jones y Levy (2012) [14] refer to the need to improve the educational model for podiatrists in terms of patient safety and in regards to error disclosure to improve professional development. Other publications in the field of podiatry address some patient safety standards, such as those related to antibiotic prophylaxis [15, 16], the incidence of thrombosis-embolism [17, 18], the surgical preparation of the skin [19–21] and the prevention of surgery in the wrong site [22, 23]. To date, the majority of the bibliography refers to isolated cases or short series on which empirical evaluations have been performed. Coheña et al. [24] are pioneers in this issue in podiatry, having proposed an adapted version of the SSC for podiatric surgery, without results.
The purpose of this study is to evaluate the impact of the SSC proposed by Coheña et al. in regards to safety standard compliance and the reduction of surgical complications in podiatric surgery.
Methods
Setting
Based on the SSC implementation guide in the Safe Surgery Saves Lives [1] programme, in order to implement the SSC in podiatric surgery there are 10 phases, these are identified in the Gantt chart, where each activity is recorded together with the time required for their implementation, (Table 1 Implementation phases). This process took ten months and took place in the Podiatric Clinic at the University of Seville (ACP).
Table 1.
Implementation phases
| Phases | Process |
|---|---|
| 1. Need for implementation and creation of a working group | - Identification of the problem and precision of the verification checklist as a solution |
| - Creation of a team that will develop the implementation. | |
| 2. Definition of purpose of the checklist and the bibliographic review | - Identification of the people to whom the checklist is performed and the type of activity to which this tool is aim to be related to. |
| 3. Analysis of the situation | - Observation of the context where the implementation will be developed. |
| -Evaluation of the strengths and weaknesses. | |
| 4. Elaboration of an activity checklist | - Creation of a sequential list of the actions that are being performed and on which interventions are required. |
| 5. Design of the verification checklist | - Creation of a preliminary format with the help of an activity list. |
| 6. Revision of the checklist | - Periodic review of the checklist with members of the team and participants of the implementation. |
| 7. Proof of the functionality of the verification checklist | - A small-scale evaluation of the checklist. |
| - Training for professionals. | |
| - Analyses of the experience through the direct observation or questionnaires | |
| 8. Approval of the checklist | - Performs of the necessary modifications. |
| 9. Training for professionals | - Training through workshops, talks, live simulations. |
| 10. Regular re-assessment of the checklist | - Analyses of changes on the context of functioning |
| - Performs of readjustments according to the changes in the situation. |
The process of implementation lasts 10 months and it has 10 different phases
Around 150 surgical podiatric procedures are carried out at this centre on an out-patient basis, from nail surgery to osteoarticular surgery with orthopaedic fixation devices under local anaesthetic. As a new tool in the field of podiatry and as recommended by other authors [25–27], an intensive training programme was undertaken during the implementation process before any data was collected. This programme included the development of a handbook, briefings and practical workshops.
Evaluation focused on identifying changes that occurred in patients as a result of using the SSC, comparing the three groups which the sample had been divided into: the pre-implementation group/the group without the SSC and the group with the SSC.
A retrospective quantitative review was made from certain documents from the medical histories as an indicator of the level of compliance to the safety standards established by the WHO. Following the same protocol as this study, the researchers are Doctors in Podiatry and experts in management and quality of care.
Study design
This analytical, observational and longitudinal study was retrospectively evaluated.
Simple random sampling was used and the sample size calculated using a formula where n is the sample size, N is the population size, Z is 0.05 y p is the reference variable.
The sample consisted of 134 patients, divided into the previously described groups. (Fig. 1 Distribution of study groups).
Fig. 1.
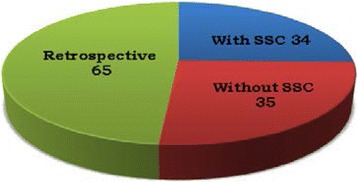
Distribution of study groups. Retrospective group 65 subjects; Without SSC group 35 subjects; With SSC group 34 subjects
The main variable is the degree of patient safety during surgery, in relation to compliance with the SSC-defined safety standards. Independent variables are shown in Table 2. (Table 2 Definition of the independent variables).
Table 2.
Description of the independent variables
| Independent variables | Definition |
|---|---|
| Surgeon | Professional that performs the surgery. |
| Sociodemographic variable | This includes the age and the gender. |
| American Society of Anesthesiologists (ASA) | The surgical risk that a patient can experiment according to the measuring scale of the American Society of Anesthesiologists. The ordinal scale from ASA I to ASA V. |
| Type of surgery | Osteoarticular surgeries with or without implants and nails or skin surgery. |
| Fulfillment of the Informed Consent | It measures the correct fulfillment of the informed consent, codified in complete, incomplete or nonexistent. |
| Identification of the surgical site | It measures the correct identification of the anatomical site where the surgical procedure is going to be performed in the medical history. When the identification is correct, it is codified with a YES, or NO when it is incorrect. The reasons of a NO codification can be an inconsistency of the identification of the surgical site between the documents, or the anatomical site of the operation is not identified, or a surgery has been performed in the wrong site. |
| Fulfillment of the DVT Prophylaxis Protocol (DVTPP) | This is applied to patients undergoing surgery and assesses the risk of a thromboembolism. On the other hand, it measures the level of compliance of the protocol. A “Secure” codification is given to the patient when the assessment page of DVTPP risk is completed, when a DVT prophylaxis is required or when the assessment is completed and the patient does not require it or prophylaxis is not established as a treatment. The rest of the variations are considered insecure practices. |
| Correct use of the antibiotic prophylaxis | Antibiotic prophylaxis is require when the patient presents 3 or more risk factors (≥65 years, Diabetes Mellitus, malnutrition, obesity, ASA ≥ 3, smoking habits, coexistence of the infection in other locations, immunosuppression and radiotherapy treatment) in the cases of surgery with osteosynthesis materials. It is considered a secure practice when the subjects require antibiotic prophylaxis and it is established as a treatment; or when, on the contrary, the antibiotic prophylaxis is not required or established. |
| Infection of the surgical site | This happens when clear signs of infection are described in the medical history (such as pain, swelling, suppuration, erythema, redness) or when a local or oral antibiotic is prescribed during the postsurgical process. |
| Postoperative days | From the days of the operation till the date of discharge. |
Results
The average age of the sample group was 47.49 years old, with a standard deviation of 22.124. In terms of gender, 73.9 % were female and 26.1 % male. In regards to the Surgical Risk Calculation, 51.5 % of patients were classed as ASA I, 47 % were classed as ASA 2 and only 1.5 % as ASA 3.
In terms of the type of surgery carried out, the highest percentage involved nail/skin surgery (66.4 %), followed by osteoarticular surgeries with implants (23.1 %) and osteoarticular surgeries without implants (10.4 %).
Correct compliance with the deep venous thromboembolic prophylaxis protocol (DVTPP)
Through the use of Pearson’s Chi-square Test, p = 0 (>0.05) a significant relationship is observed between the “WITH checklist group” and the correct practice of DVTPP. (Table 3A-B Comparison chart: Correct compliance with the DVTPP risk assessment and Chi-square test). The protocol was proposed by Autar R. [28] and was incorporated into podiatric surgical care at the ACP. The results of this study demonstrate that the SSC helps to improve compliance with the DVTPP. Truran [29], in his pre-post SSC implementation study, compares the compliance rates with the DVTPP, noting that non-compliance fell from 6.9 % to 2.1 %. This study found that the non-compliance rate was 68 % in the period prior to the implementation of the SSC, a figure that decreased to 24 % in the without SSC group and to 8 % in the with SSC group. It could be argued that this difference is due to the increased awareness of patient safety after the implementation period. The high levels of non-compliance found during this study in comparison to that of other studies could be explained by a failure to adhere to the protocol. This is likely because cases of thromboembolic complications in podiatric surgery are much fewer than in general surgery where these types of complications are common and stricter protocols exist.
Table 3.
Comparison chart Correct Fulfillment of the DVTPP risk assessment
| A. | ||||
|---|---|---|---|---|
| DVTPP Assessment | ||||
| Secure | Insecure | |||
| Types of data | With SSC | Recount | 28 | 6 |
| % in the DVTPP security | 47.5 % | 8.0 % | ||
| Revised residues | 5.2 | −5.2 | ||
| Without SSC | Recoaunt | 17 | 18 | |
| % in the DVTPP security | 28.8 % | 24.0 % | ||
| Revised residues | .6 | -.6 | ||
| Retrospective | Recount | 14 | 51 | |
| % in the DVTPP security | 23.7 % | 68.0& | ||
| Revised residues | -5.1 | 5.1 | ||
| B. Chi-square test | ||||
| Value | gl | Sig. Asymptotic (bilateral) | ||
| Pearson chi-square | 33.898 | 2 | .000 | |
| Number of valid cases | 134 | |||
A significant relation has been observed between the group WITH checklist and the secure practice of the DVTPP assessment (>0.05)
Correct antibiotic prophylaxis pratice
Antibiotic prophylaxis is a controversial issue among health professionals, including podiatrists; nonetheless, the correct use of antibiotic prophylaxis reduces the risk of post-surgical complications, offering patients health benefits and an increased quality of care, as well as having financial repercussions [30].
This study makes use of the recommendations made by Córdoba et al. [15] and Mosquera et al. [16] in their reviews as a means of assessing the usefulness of antibiotic prophylaxis. The results of this study demonstrate a significant relationship between the use of the SSC and the correct usage of antibiotic prophylaxis (p = 0.049). (Table 4 Correlation between the use of the SSC and correct use of antibiotic prophylaxis). Similarly, other authors [31] also note a significant improvement in the correct usage of antibiotic prophylaxis (57 % in the period prior to the SSC and 77 % in the period post). Rydenfält [32] observed that the standard associated with antibiotic prophylaxis in the SSC was one of the easiest to comply with.
Table 4.
Correlation between the use of SSC and correct use of the Antibiotic prophylaxis
| A. | ||||||
|---|---|---|---|---|---|---|
| Antibiotic prophylaxis | ||||||
| Required, established treatment | Required, not established treatment | Not required, but established treatment | Not required and not established treatment | |||
| Types of data | With SSC | Recount | 15 | 1 | 3 | 15 |
| % in the antibiotic prophylaxis | 36,6 % | 4,3 % | 37,5 % | 24,2 % | ||
| Revised residues | 2,0 | −2,5 | ,8 | -,3 | ||
| Without SSC | Recount | 6 | 7 | 1 | 21 | |
| % in the antibiotic prophylaxis | 14,6 % | 30,4 % | 12,5 % | 33,9 % | ||
| Revised residues | −2,0 | ,5 | -,9 | 1,9 | ||
| Retrospective | Recount | 20 | 15 | 4 | 26 | |
| % in the antibiotic prophylaxis | 48,8 % | 65,2 % | 50,0 % | 41,9 % | ||
| Revised residues | ,0 | 1,8 | ,1 | −1,4 | ||
| B. Chi-square test | ||||||
| Value | gl | Sig. Asymptotic (bilateral) | ||||
| Pearson chi-square | 12,646 | 6 | .049 | |||
| Number of valid cases | 134 | |||||
Surgical site infection rate
De Vries [33] and Tillman [34] indicate that surgical site infection is the most frequent postsurgical complication and one with the highest impact upon the health/illness process of the patient, satisfaction levels and healthcare spending. According to Butterworth [35] and Zgonis [36] an infection rate of between 0.5 and 6.5 % is accepted as normal in elective foot-ankle surgery amongst podiatric surgeons. This study found a much higher total surgical site infection rate (15.3 %) than that accepted as normal by these authors. This can be explained by the teaching nature of the centre where this study was undertaken and the inherent bias of the medical histories involved. In the Table 5 (Table 5 Comparative analyses of data on surgical site infection) shows the comparative figures between this study and the research of Bliss [37], Tillman [34] and Haynes [38]. A reduction in the surgical site infection rates between the different groups are observed, reflecting lower infection rates in the groups where the SSC was used.
Table 5.
Comparative analyses of data about infection on the surgical site
Furthermore, a significant relationship is observed between the reduction in surgical site infection rate and antibiotic prophylaxis (p = 0.019) (Table 6 A-B Relationship between surgical site infection and the correct usage of antibiotic prophylaxis). This is something which leads us to believe that an indirect correlation exists between the use of the SSC and the reduction in the surgical site infection rate.
Table 6.
Relationship between Surgical site infecion and the secure use of the antibiotic prophylaxis
| A. | |||||
|---|---|---|---|---|---|
| Antibiotic prophylaxis security | |||||
| Secure | Insecure | ||||
| Surgical site Infection | Yes | Recount | 11 | 9 | |
| % in the Antibiotic prophylaxis security | 11,0 % | 29,0 % | |||
| Revised residues | −2,4 | 2,4 | |||
| No | Recount | 89 | 22 | ||
| % in the Antibiotic prophylaxis security | 89,0 % | 71,0 % | |||
| Revised residues | 2,4 | −2,4 | |||
| B. Chi-square Pearson test and Fisher’s exact stadistical test | |||||
| Value | gl | Sig. Asymptotic (bilateral) | Sig. Exact (bilateral) | Sig. Exact (Unilateral) | |
| Pearson chi-square | 5.948 | 1 | .015 | ||
| Fisher’s exact statistical test | .022 | .019 | |||
| Number of valid cases | 134 | ||||
(When it use the antibiotic prophylaxis security correctment, the surgical site infection decrease to stadistical significative way)
Correct completion of informed consent
Numerous authors [39, 40] highlight the importance of patient-surgeon communication and consider the inclusion of the patient in their treatment the fundamental premise of healthcare. The informed consent form is a scientifically endorsed tool available to evaluate this relationship. Yet, in clinical practice is not always employed correctly, impacting upon communication, safety and affording the patient a grounds for claim [41].
The results of this study demonstrate a connection between the use of the SSC and higher levels of compliance and completion of the informed consent in the surgical process. De Vries [42] analysed 294 complaints made to Dutch health professionals, he indicated that 100 % of the 23 complaints registered in relation to the informed consent could have been avoided through the use of the SSC. Indeed, Cavallini [43], through incorporating the SSC into the quality programme at the centre where his study was undertaken, increase the informed consent completion rate to 99.76 %.
Number of post-operative days
The Kruskal-Wallis test for independent samples was used to associate the “post-operative days” independent variable to the study’s different groups, establishing a significance level of 0.05. This study found a significant relationship between the use of the SSC and the reduction of post-operative days, as is shown in Fig. 2 (Fig. 2 Comparative graphic on the number of postsurgical days) and Table 7 (Table 7 Statistical data on number of postoperative days).
Fig. 2.
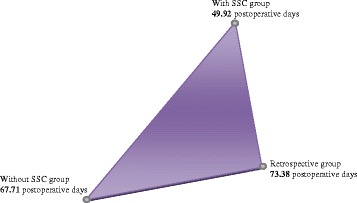
Comparative graphic on the number of postsurgical days. A 49.92 with SSC in comparison with 67.71 without SSC and 73.38 Retrospective
Table 7.
Statistical data to number of postoperative days
| Statistical test | Standard error | Deviation Statistic test | Sign | Adjoining sign | |
|---|---|---|---|---|---|
| With SSC-Retrospective | −23.459 | 8.129 | −2.886 | .004 | .012 |
The use of SSC decrease the postoperative days statistically significant (0,012)
This result confirms that the SSC affords the surgical team a visual and verbal reminder of the recommended safety measures, thereby reducing reliance on memory and improving compliance with basic safety standards [32, 39–43], consequently reducing the post-surgical period.
A retrospective analysis of medical histories was used in this study. The quality of the data collected was dependent upon the quality of the documentation in the medical and legal records. Given that compiled data may not directly reflect clinical practice, and therefore, as Panesar et al. [44] suggests, an infra-supra register might exist, Soria-Aledo [45] acknowledged this as a limitation in their studies. This study was able to minimise the Hawthorne effect by dividing the sample into three groups, as has been described by various authors [29, 46].
Conclusions
Just as the attitude and motivation of professionals can change, so can clinical practice. It is therefore necessary to establish a monitoring process for the SSC, performing audits and re-editing where necessary in order to make it more efficient and effective for professionals. Significant improvements have been seen in the utilization of patient safety protocols such as the DVTPP and antibiotic prophylaxis, as well as a reduction in post-operative days. These changes improve, both directly and indirectly overall patient safety, reducing surgical complications such as surgical site infections. After analysing all of the tests used to evaluate the SSC implementation process in podiatric surgery, we believe the study’s objectives have been fulfilled and confirm that the SSC is a useful and effective tool in the improvement of patient safety. We believe that further studies, over longer timeframes and in other podiatric surgical centres are necessary in order to gather further scientific evidence.
Ethical considerations
This investigation project meets with the approval and acceptance of the Ethical Committee of Experimenting of the University of Seville to investigate with human subjects and it adjusts to the current regulations in Spain and the European Union. To finish, informed consent was obtained of each participant after being completely informed before their participation in this study.
Acknowledgements
Thanks to all the professionals working in the Podiatric clinical area of the University of Seville for their dedication and full readiness.
Abbreviations
- WHO
World Health Organization
- SSC
Surgical Safety Checklist
- ASA
American Society of Anesthesiologists
- IC
Informed Consent
- DVTPP
Deep Venus Tromboembolic Prophylaxis Protocol
Footnotes
Manuel Coheña-Jiménez Pedro Montaño-Jiménez and Antonio Córdoba-Fernández contributed equally to this work.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JGP, MCJ, and PMJ developed the study design. JGP and MCJ were responsible for the data collection. PMJ and ACF conducted the data analysis. JGP wrote the manuscript, with contributions from MCJ and ACF. All authors approved the final manuscript.
Contributor Information
Jaime García-París, Email: jaigarpar@us.es.
Manuel Coheña-Jiménez, Email: mcohena@us.es.
Pedro Montaño-Jiménez, Email: pmj@us.es.
Antonio Córdoba-Fernández, Email: acordoba@us.es.
References
- 1.Guidelines for Safe Surgery . World Health Organization. 1. 2008. [PubMed] [Google Scholar]
- 2.Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 3.Aranaz J, Aibar C, Vitaller J, Mira J, Orozco D. Estudio APEAS: estudio sobre la seguridad de los pacientes en Atención Primaria de Salud. Madrid: Ministerio de Sanidad y Consumo 2008; 2011. [Google Scholar]
- 4.Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. Br Med J. 2001;322:517–519. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38:261–271. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The quality in Australian health care study. Med J Aust. 1995;163:458–471. doi: 10.5694/j.1326-5377.1995.tb124691.x. [DOI] [PubMed] [Google Scholar]
- 7.Ministerio de Sanidad y Consumo . Estudio nacional sobre los efectos adversos ligados a la hospitalización. 2005. [Google Scholar]
- 8.Pittet D, Allegranzi B, Boyce J. The World Health Organization guidelines on hand hygiene in healthcare and their consensus recommendations. Infect Control Hosp Epidemiol. 2009;30:611–622. doi: 10.1086/600379. [DOI] [PubMed] [Google Scholar]
- 9.Lorist MM, Boksem MA, Ridderinkhof KR. Impaired cognitive control and reduced cingulate activity during mental fatigue. Cogn Brain Res. 2005;24:199–205. doi: 10.1016/j.cogbrainres.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 10.Miller G. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychol Rev. 1956;63:81–97. doi: 10.1037/h0043158. [DOI] [PubMed] [Google Scholar]
- 11.De Vries E, Dijkstra L, Smorenburg SM, Meijer RP, Boermeester MA. The Surgical patient Safety System (SURPASS) checklist optimizes timing of antibiotic prophylaxis. Patient Saf Surg. 2010;4. [DOI] [PMC free article] [PubMed]
- 12.Boscá-Mayans MR, Arana E, Sánchez-Aparisi E. Diseño de una lista de verificación para radiología intervencionista. Enferm Clin. 2012;22:299–303. doi: 10.1016/j.enfcli.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Perea B, Santiago A, García F, Labajo E. Proposal for a surgical checklist for ambulatory oral surgery. Int J Oral Maxillofac Surg. 2011;40:949–954. doi: 10.1016/j.ijom.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Jones LJ, Levy LA. An Educational Model for Patient Safety and Disclosure of Medical Error in Podiatric Medicine. J Am Podiatr Med Assoc. 2012;102:505–511. doi: 10.7547/1020505. [DOI] [PubMed] [Google Scholar]
- 15.Córdoba A, Ruiz G, Canca A. Algorithm for the management of antibiotic prophylaxis in onychocryptosis surgery. Foot. 2010;20:140–145. doi: 10.1016/j.foot.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 16.Fernández AM, Rey VS, Carrodeguas MV, Castro RG. Profilaxis antibiótica perioperatoria. Rev Int de Cien Pod. 2013;7:109–114. [Google Scholar]
- 17.Lim W, Wu C. Balancing the risks and benefits of thromboprophylaxis in patients undergoing podiatric surgery. Chest. 2009;135:888–890. doi: 10.1378/chest.08-2799. [DOI] [PubMed] [Google Scholar]
- 18.Felcher AH, Mularski RA, Mosen DM, Kimes TM, De Loughery TG, Laxson SE. Incidence and risk factors for venous thromboembolic disease in podiatric surgery. Chest. 2009;135:917–922. doi: 10.1378/chest.08-1631. [DOI] [PubMed] [Google Scholar]
- 19.Becerro De Bengoa R, Losa ME, Cervera LA, Fernández DS, Prieto JP. Efficacy of intraoperative surgical irrigation with polihexanide and nitrofurazone in reducing bacterial load after nail removal surgery. J Am Acad Dermatol. 2011;64:328–335. doi: 10.1016/j.jaad.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Becerro de Bengoa R, Losa ME, Cervera LA, Fernández DS, Prieto J. Preoperative skin and nail preparation of the foot: Comparison of the efficacy of 4 different methods in reducing bacterial load. J Am Acad Dermatol. 2009;61:986–992. doi: 10.1016/j.jaad.2009.04.045. [DOI] [PubMed] [Google Scholar]
- 21.Ostrander RV, Botte MJ, Brage ME. Efficacy of surgical preparation solutions in foot and ankle surgery. J Bone Joint Surg. 2005;87:980–985. doi: 10.2106/JBJS.D.01977. [DOI] [PubMed] [Google Scholar]
- 22.Beckingsale TB, Greiss ME. Getting off on the wrong foot: Doctor–patient miscommunication: A risk for wrong site surgery. Foot Ankle Surg. 2011;17:201–202. doi: 10.1016/j.fas.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Schweitzer KM, Brimmo O, May R, Parekh SG. Incidence of wrong-site surgery among foot and ankle surgeons. Foot Ankle Spec. 2011;4:10–13. doi: 10.1177/1938640010384992. [DOI] [PubMed] [Google Scholar]
- 24.Coheña M, García J, Córdoba A, Juárez J, Montaño P. Proposal of a Surgical Security Checklist in Podiatric Surgery. Clin Res Foot Ankle. 2014;2.
- 25.Nilsson L, Lindberget O, Gupta A, Vegfors M. Implementing a pre‐operative checklist to increase patient safety: a 1‐year follow‐up of personnel attitudes. Acta Anaesthesiol Scand. 2010;54:176–182. doi: 10.1111/j.1399-6576.2009.02109.x. [DOI] [PubMed] [Google Scholar]
- 26.Martínez O, Gutiérrez S, Liévano SA. Propuesta para implantar una Lista de Verificación de Seguridad en procedimientos invasivos y quirófano. Rev CONAMED. 2011;16:53–58. [Google Scholar]
- 27.Hawkins RB, Levy SM, Zhao JY, Doody KA, Lally KP, Kao LS, et al. Assesment of the implementation of a Surgical preoperative checklist. J Surg Res. 2012;172:207. doi: 10.1016/j.jss.2011.11.482. [DOI] [Google Scholar]
- 28.Autar R. The management of deep vein thrombosis: the Autar DVT risk assessment scale re-visited. J Orth Nurs. 2003;7:114–124. doi: 10.1016/S1361-3111(03)00051-7. [DOI] [Google Scholar]
- 29.Truran P, Critchley RJ, Gilliam A. Does using the WHO surgical checklist improve compliance to venous thromboembolism prophylaxis guidelines? Surgeon. 2011;9:309–311. doi: 10.1016/j.surge.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 30.Sewell M, Adebibe M, Jayakumar P, Jowett C, Kong K, Vemulapalli K, et al. Use of the WHO surgical safety checklist in trauma and orthopaedic patients. Int Orthop. 2011;35:897–901. doi: 10.1007/s00264-010-1112-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vats A, Vincent CA, Nagpal KR, Davies W, Darzi A, Moorthy K. Practical challenges of introducing WHO surgical checklist: UK pilot experience. BMJ. 2010;340. [DOI] [PubMed]
- 32.Rydenfält C, Johansson G, Odenrick P, Åkerman K, Larsson PA. Compliance with the WHO surgical safety checklist: deviations and possible improvements. Int J Qual Health Care. 2013;25:182–187. doi: 10.1093/intqhc/mzt004. [DOI] [PubMed] [Google Scholar]
- 33.Winters BD, Gurses AP, Lehmann H, Sexton JB, Rampersad CJ, Pronovost PJ. Clinical review: checklists-translating evidence into practice. Crit Care. 2009;13:210. doi: 10.1186/cc7792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyons VE, Popejoy LL. Meta-Analysis of Surgical Safety Checklist Effects on Teamwork, Communication, Morbidity, Mortality, and Safety. West J Nurs Res. 2013;36:245–261. doi: 10.1177/0193945913505782. [DOI] [PubMed] [Google Scholar]
- 35.Wachter RM, Shojania KG, Duncan BW. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evid Rep Technol Assess. 2001. [PMC free article] [PubMed]
- 36.De Vries EN, Eikens MP, Hamersma AM, Smorenburg SM, Gouma DJ, Boermeester MA. Prevention of Surgical Malpractice Claims by Use of a Surgical Safety Checklist. Ann Surg. 2011;253:624–628. doi: 10.1097/SLA.0b013e3182068880. [DOI] [PubMed] [Google Scholar]
- 37.Cavallini GM, Campi L, De Maria M, Forlini M. Clinical risk management in eyeout patient surgery: a new surgical safety checklist for cataract surgery and intravitreal anti-VEGF injection. Graefes Arch Clin Exp Ophthalmol. 2013;251:889–894. doi: 10.1007/s00417-012-2206-2. [DOI] [PubMed] [Google Scholar]
- 38.De Vries EN, Prins HA, Crolla RMPH, Den Outer AJ, Van Andel G, Van Helden SH, et al. Effect of a Comprehensive Surgical Safety System on Patient Outcomes. N Engl J Med. 2010;363:1928–1937. doi: 10.1056/NEJMsa0911535. [DOI] [PubMed] [Google Scholar]
- 39.Tillman M, Wehbe-Janek H, Hodges B, Smythe WR, Papaconstantinou HT. Surgical care improvement project and surgical site infections: can integration in the surgical safety checklist improve quality performance and clinical outcomes? J Surg Res. 2013;184:150–156. doi: 10.1016/j.jss.2013.03.048. [DOI] [PubMed] [Google Scholar]
- 40.Butterworth P, Gilheany MFA, Tinley P. Postoperative infection rates in foot and ankle surgery: a clinical audit of Australian podiatric surgeons. Aust Health Rev. 2010;34:180–185. doi: 10.1071/AH08687. [DOI] [PubMed] [Google Scholar]
- 41.Zgonis T, Jolly GP, Garbalosa JC. The efficacy of prophylactic intravenous antibiotics in elective foot and ankle surgery. J Foot Ankle Surg. 2004;43:97–103. doi: 10.1053/j.jfas.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 42.Bliss LA, Ross-Richardson CB, Sanzari LJ, Shapiro DS, Lukianoff AE, Bernstein BA, et al. Thirty-Day Outcomes Support Implementation of a Surgical Safety Checklist. J Am Coll Surg. 2012;215:766–776. doi: 10.1016/j.jamcollsurg.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 43.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AS, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 44.Panesar SS, Noble DJ, Mirza SB, Patel B, Mann B, Emerton M, et al. Can the surgical checklist reduce the risk of wrong site surgery in orthopaedics?-can the checklist help? Supporting evidence from analysis of a national patient incident reporting system. J Orthop Surg Res. 2011;6:18. doi: 10.1186/1749-799X-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Soria-Aledo V, Andre Da Silva Z, Saturno PJ, Grau-Polan M, Carrillo-Alcaraz A. Dificultades en la implantación del checklist en los quirófanos de cirugía. Cir Esp. 2012;90:180–185. doi: 10.1016/j.ciresp.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 46.Van Klei W, Hoff R, Van Aarnhem E, Simmermacher R, Regli L, Kappen T, et al. Effects of the introduction of the WHO “Surgical Safety Checklist” on in-hospital mortality: a cohort study. Ann Surg. 2012;255:44–49. doi: 10.1097/SLA.0b013e31823779ae. [DOI] [PubMed] [Google Scholar]


