Abstract
Background
Cardiopulmonary resuscitation (CPR) was first introduced in 1960 for people who unexpectedly experience sudden cardiac arrest. Over the years, it became routine practice in all institutions to perform CPR for all patients even though, for some patients with fatal conditions, application of CPR only prolongs the dying process through temporarily restoring cardiac function.
Objectives
This analysis aims to systematically review the literature to provide an accurate estimate of survival following CPR in patients with terminal health conditions.
Data Sources
A literature search was performed for studies published from January 1, 2004, until January 10, 2014. The search was updated monthly to March 1, 2014.
Review Methods
Abstracts and full text of studies that met eligibility criteria were reviewed. Reference lists were also examined for any additional relevant studies not identified through the search.
Results
Cancer patients have lower survival rates following CPR than patients with conditions other than cancer, and cancer patients who receive CPR in intensive care units have one-fifth the rate of survival to discharge of cancer patients who receive CPR in general wards. While the meta-analysis of studies published between 1967 and 2005 reported a lower survival to discharge for cancer patients (6.2%), more recent studies reported higher survival to discharge or to 30-day survival for these patients. Higher survival rates in more recent studies could originate with more “do not attempt resuscitation” orders for patients with end-stage cancer in recent years.
Older age does not significantly decrease the rate of survival following CPR while the degree, the type, and the number of chronic health conditions; functional dependence; and multiple CPRs (particularly in advanced age) do reduce survival rates. Emergency Medical Services response time have a significant impact on survival following out-of-hospital CPR.
Conclusions
Survival after CPR depends on the severity of illness, type and number of health conditions, functional dependence, and multiple CPRs.
Plain Language Summary
Patients whose hearts stop and who are revived through cardiopulmonary resuscitation (CPR) are unlikely to live for a long period of time if they are in very poor health prior to receiving CPR. For instance, studies show that patients with advanced illnesses (such as disseminated cancer or multiple organ failure) who receive CPR are very unlikely to recover. Although CPR might be initially successful, survival is short for these patients, with most dying during the same hospital stay.
Overall, about 1 in 10 cancer patients who survive CPR will leave hospital alive, meaning that 9 of 10 who initially survived CPR will die soon after. The survival rate for seriously ill cancer patients who receive CPR in intensive care units is very low (reported as 2%).
Background
In July 2013, the Evidence Development and Standards (EDS) branch of Health Quality Ontario (HQO) began work on developing an evidentiary framework for end of life care. The focus was on adults with advanced disease who are not expected to recover from their condition. This project emerged from a request by the Ministry of Health and Long-Term Care that HQO provide them with an evidentiary platform on strategies to optimize the care for patients with advanced disease, their caregivers (including family members), and providers.
After an initial review of research on end-of-life care, consultation with experts, and presentation to the Ontario Health Technology Advisory Committee (OHTAC), the evidentiary framework was produced to focus on quality of care in both the inpatient and the outpatient (community) settings to reflect the reality that the best end-of-life care setting will differ with the circumstances and preferences of each client. HQO identified the following topics for analysis: determinants of place of death, patient care planning discussions, cardiopulmonary resuscitation, patient, informal caregiver and healthcare provider education, and team-based models of care. Evidence-based analyses were prepared for each of these topics.
HQO partnered with the Toronto Health Economics and Technology Assessment (THETA) Collaborative to evaluate the cost-effectiveness of the selected interventions in Ontario populations. The economic models used administrative data to identify an end-of-life population and estimate costs and savings for interventions with significant estimates of effect. For more information on the economic analysis, please contact Murray Krahn at murray.krahn@theta.utoronto.ca.
The End-of-Life mega-analysis series is made up of the following reports, which can be publicly accessed at http://www.hqontario.ca/evidence/publications-and-ohtac-recommendations/ohtas-reports-and-ohtac-recommendations.
-
▸
End-of-Life Health Care in Ontario: OHTAC Recommendation
-
▸
Health Care for People Approaching the End of Life: An Evidentiary Framework
-
▸
Effect of Supportive Interventions on Informal Caregivers of People at the End of Life: A Rapid Review
-
▸
Cardiopulmonary Resuscitation in Patients with Terminal Illness: An Evidence-Based Analysis
-
▸
The Determinants of Place of Death: An Evidence-Based Analysis
-
▸
Educational Intervention in End-of-Life Care: An Evidence-Based Analysis
-
▸
End-of-Life Care Interventions: An Economic Analysis
-
▸
Patient Care Planning Discussions for Patients at the End of Life: An Evidence-Based Analysis
-
▸
Team-Based Models for End-of-Life Care: An Evidence-Based Analysis
Objective of Analysis
This analysis aims to systematically review the literature to provide an accurate estimate of chance of survival following cardiopulmonary resuscitation (CPR) in patients with terminal health conditions.
Clinical Need and Target Population
Cardiopulmonary resuscitation has become the default response to cardiac arrests that occur in or out of hospital. Not all patients will survive after CPR, and the underlying cause of cardiac arrest, the type and severity of illness, or the initial heart rhythm can contribute to the chance of survival after CPR. As with other medical interventions, clinicians should provide patients with information about likelihood of survival following CPR and risks associated with this intervention.
There is an increasing focus on improving the quality of end-of-life care including appropriateness of some aggressive interventions to avoid nonbeneficial interventions or doing harm to the patient.
Improving communication with patients and families through patient-centred discussion and supporting and respecting patients’ autonomy and dignity is critical in making resuscitation decisions.
Although survival rates following CPR for patients with advanced chronic health conditions do not appear to be zero, rates are low enough that patients may choose not to undergo this intervention if they receive meaningful and accurate information on their likelihood of survival following CPR. Accurate prediction of survival following CPR in terminally ill patients allows patients and their families to understand the patient's condition and to prepare for the eventuality of death. Patients with terminal health conditions need information on the expected course of their disease and accurate prognostic information regarding both survival and quality of life after CPR, if it becomes necessary, in order to make informed end-of-life decisions.
Patients’ Perception of Their Chance of Survival
Patients’ sometimes unrealistic estimates of their chance of survival following CPR can differ from the estimates given by health care providers. Beliefs of elderly patients regarding the likelihood of surviving CPR, if it becomes necessary during the course of their hospitalization, was the subject of a few studies. A Canadian study (1) that administered a face-to-face questionnaire to older patients with end-stage cancer and advanced diseases in 5 Canadian hospitals reported that only 2.7% of patients thought that the success rate of CPR was < 10%. This study showed that seriously ill hospitalized patients have poor knowledge about CPR. Only 11.3% of patients could describe more than 2 components of CPR.
Adams and Snedden (2) administered a standardized survey to 100 patients 70 years or older who were randomly selected from emergency department, internal medicine clinic, and general medical wards at one urban medical centre. They reported that 81% of respondents believed that their chance of surviving CPR and leaving the hospital was 50% or more, and 23% believed that their chance was 90% or better. The source of information for most patients was television or their physician.
“Do Not Attempt to Resuscitate” Order
The “do not attempt to resuscitate” (DNAR) order is a component of advance directives and prohibits the use of resuscitation measures in the event of cardiac arrest. It allows patients to express their own wishes for resuscitation options in the event they become incapacitated and could no longer communicate their wishes.
The process of DNAR completion involves patients, family members, and the health care team, in the context of an emotional and stressful environment characterized by many uncertainties. The likelihood of completing the DNAR order is influenced by many factors, and considerable research has examined the determinants of DNAR orders for various health conditions and settings.
Prevalence and Incidence
Temporal trends in the incidence of CPR and the rate of survival after CPR were examined in a study that used Medicare data from 1992 through 2005 for beneficiaries 65 years of age or older who underwent CPR in US hospitals. (3) The cumulative incidence of in-hospital CPR was 2.73 events per 1,000 admissions; this incidence did not change substantially during the study period. An examination of hospital deaths showed that the proportion of deaths preceded by in-hospital CPR increased from 3.8% in 1992 to 5.2% in 2005 (P < 0.001).
The proportion of patients who survived CPR and were discharged home decreased significantly during the study period, whereas the proportion of patients discharged to a hospice increased significantly after 1997.
Technology/Technique
Cardiopulmonary resuscitation includes administration of chest compressions in combination with artificial respiration, cardiac defibrillation, and intravenous medications. The CPR technique was developed in the early 1960s as a simple and effective way to resuscitate patients suffering from cardiac arrest. Performing CPR regardless of underlying cause of cardiac arrest can transiently restore circulation, but this survival is not guaranteed to the point of leaving hospital alive.
A meta-analysis (4) of studies that investigated the rate of immediate survival and survival to discharge for all adult patients who underwent in-hospital CPR showed that the rate of immediate survival was 4 in 10 and that the likelihood of survival to discharge was 1 in 3 for those patients who were revived (1 in 8 among all patients who underwent CPR in the hospital).
Evidence-Based Analysis
Research Question
What is the post–cardiopulmonary resuscitation (CPR) survival rate for patients with terminal illness?
Research Methods
Literature Search Strategy
A literature search was performed on January 10, 2013, using Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid Embase, EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL), and EBM Reviews, for studies published from January 1, 2004, to January 10, 2014. (Appendix 1 provides details of the search strategies.) Abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also examined for any additional relevant studies not identified through the search. The search was automatically updated until March 1, 2014, through the AutoAlert function of the search, and all identified studies were included in this review.
Inclusion Criteria
English-language full-text publications
published between January 1, 2004, and January 1, 2014
randomized controlled trials (RCTs), systematic reviews, meta-analyses, and observational studies
studies reporting survival of population of interest after receiving CPR
Exclusion Criteria
studies on pediatric population (patients under age 18)
studies on patients with acute health conditions (e.g., trauma, surgical, burn)
studies on patients in settings other than those commonly used for end-of-life patients (e.g., inmates)
Outcomes of Interest
rate of immediate survival following CPR
rate of survival to discharge following in-hospital CPR
rate of 1-year survival
Statistical Analysis
Patient and study characteristics were presented in tables. Rate of immediate survival and longer-term survival was graphically displayed for different patient populations, conditions, or location of cardiac arrest using STATA 11 software.
Quality of Evidence
The quality of the body of evidence for each outcome was examined according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group criteria. (5) The overall quality was determined to be high, moderate, low, or very low using a step-wise, structural methodology.
Study design was the first consideration; the starting assumption was that randomized controlled trials (RCTs) are high quality, whereas observational studies are low quality. Five additional factors—risk of bias, inconsistency, indirectness, imprecision, and publication bias—were then taken into account. Limitations in these areas resulted in downgrading the quality of evidence. Finally, 3 main factors that may raise the quality of evidence were considered: the large magnitude of effect, the dose-response gradient, and any residual confounding factors. (5) For more detailed information, please refer to the latest series of GRADE articles. (5)
As stated by the GRADE Working Group, the final quality score can be interpreted using the following definitions:
| High | High confidence in the effect estimate—the true effect lies close to the estimate of the effect |
| Moderate | Moderate confidence in the effect estimate—the true effect is likely to be close to the estimate of the effect, but may be substantially different |
| Low | Low confidence in the effect estimate—the true effect may be substantially different from the estimate of the effect |
| Very Low | Very low confidence in the effect estimate—the true effect is likely to be substantially different from the estimate of the effect |
Results of Evidence-Based Analysis
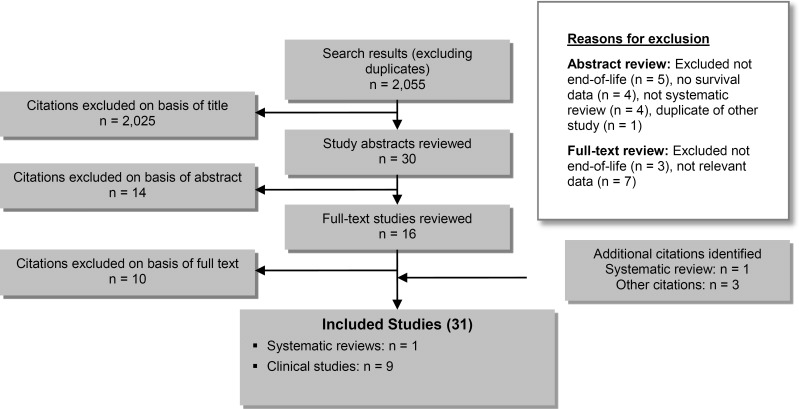
The database search yielded 2,055 citations published between January 1, 2004, and March 1, 2014 (with duplicates removed). Articles were excluded on the basis of information in the title and abstract (Figure 1). The full texts of potentially relevant articles were obtained for further assessment. Figure 2 shows the breakdown of when and for what reason citations were excluded from the analysis.
Figure 1: Citation Flow Chart.
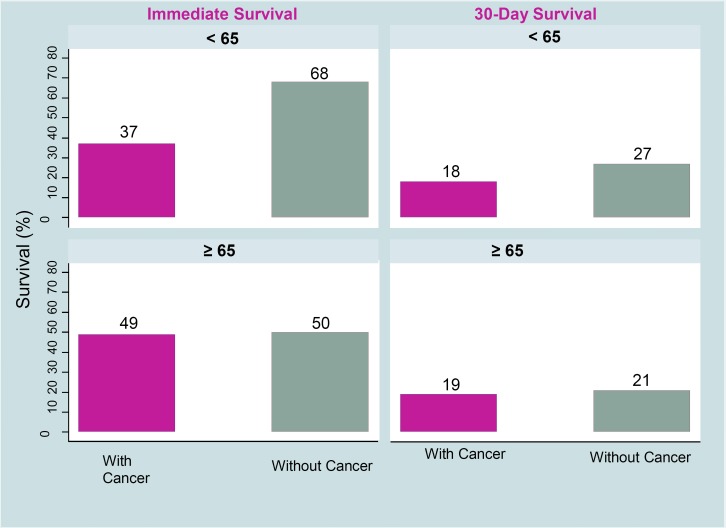
Figure 2: Survival Following In-Hospital Cardiopulmonary Resuscitation: Patients With Cancer Versus Without Cancer According to Age Categories.
Six studies met the inclusion criteria. The reference lists of the included studies were hand-searched to identify other relevant studies. One systematic review and 3 additional citations were included in this review, for a total of 10.
For each included study, the study design was identified and is summarized below in Table 1, a modified version of a hierarchy of study design by Goodman, 1996. (6)
Table 1:
Body of Evidence Examined According to Study Design
| Study Design | Number of Eligible Studies |
|---|---|
| RCTs | |
| Systematic review of RCTs | |
| Large RCT | |
| Small RCT | |
| Observational Studies | |
| Systematic review of non-RCTs with contemporaneous controls | |
| Non-RCT with non-contemporaneous controls | |
| Systematic review of non-RCTs with historical controls | 1 |
| Non-RCT with historical controls | |
| Database, registry, or cross-sectional study | 5 |
| Case series | 4 |
| Retrospective review, modelling | |
| Studies presented at an international conference | |
| Expert opinion | |
| Total | 10 |
Source: Goodman 1996. (6)
Abbreviation: RCT, randomized controlled trial.
The 10 included studies consisted of 1 meta-analysis (7) and 9 clinical studies. (8–16)
Four clinical studies (8–11) and 1 systematic review (7) reported CPR in cancer patients. Three clinical studies reported on CPR in patients with chronic health conditions (10;12;13) and 4 (10;14–16) reported on CPR in older patients.
Outcomes of Cardiopulmonary Resuscitation in Patients With Cancer
Table 2 shows characteristics of studies that reported outcomes of CPR in cancer patients.
Table 2:
Survival Rate for Patients With and Without Cancer who Received Cardiopulmonary Resuscitation
| Author, Year | Country | Study Design | Study Period | Patients | Age | Location of Cardiac Arrest |
|---|---|---|---|---|---|---|
| Lin et al 2012 (8) | Taiwan | Population-based database | Jan 1997–Dec 2004 | 11,710 | All ages | Hospital |
| Taran et al 2012 (9) | United States | Retrospective electronic medical record review | Oct 1999–Oct 2011 | 154 | Cancer:
|
Hospital |
Patients without cancer:
|
||||||
| Larkin et al 2010 (10) | United States | National CPR registry | Jan 2000–Sept 2004 | 49,130 5,494 metastatic/hematologic cancer | Mean (SD): 66.7 (15.7) ≥ 18 | Hospital |
| Hwang et al 2010 (11) | United States | Retrospective medical record review | 2000–2002 | 41 | Mean (range) 60 (19–84) | Out of hospital |
| Reisfield et al 2006 (7) | United States | Meta-analysis (42 studies) | Jan 1966–Aug 2004 | 1,707 | N/A |
Abbreviations: CPR, cardiopulmonary resuscitation; N/A, not applicable; SD, standard deviation.
Survival After In-Hospital Cardiac Arrest
Two clinical studies (7;9) and 1 meta-analysis (8) compared survival after in-hospital CPR of patients with cancer with survival of patients without cancer. A large study (n = 11,710) based on a population health database including patients of all ages (8) compared survival to discharge after in-hospital CPR of cancer patients with survival to discharge of patients without cancer. Results showed that patients with cancer diagnoses had lower chance of survival to discharge after CPR than patients without cancer (11.6% versus 15.3%, P < 0.001).
The second study, which had a smaller sample (n = 154), (9) compared the rate of immediate survival and survival at 30 days among adult patients who underwent in-hospital CPR. As the first study did, this study reported lower survival rates in cancer patients than in patients without cancer, but the difference between the 2 groups of patients was not statistically significant. When cancer patients were stratified into 2 age groups (< 65 and ≥ 65 years), younger cancer patients had a lower rate of immediate and 30-day survival than younger patients without cancer, but no significant difference is reported (Figure 2).
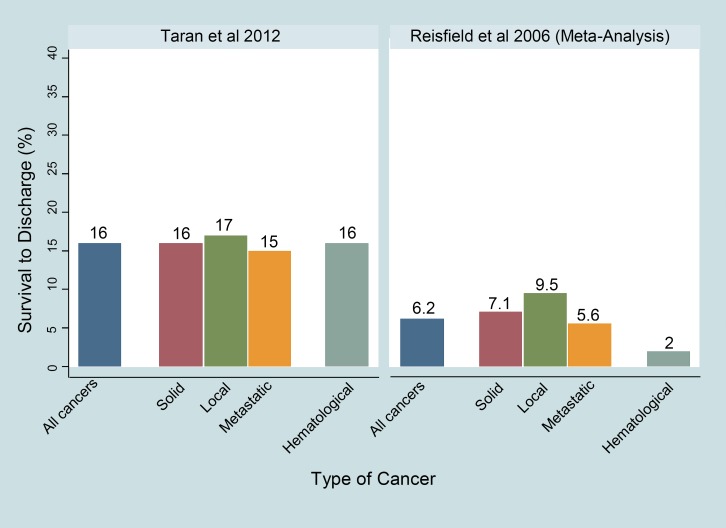
This study also stratified cancer patients into those with solid tumors and those with hematologic malignancies. The solid tumor group was further divided into localized and metastatic disease groups. The 30-day survival for both solid and hematologic tumors was 16% (Figure 3).
Figure 3: Survival to Discharge Following In-Hospital Cardiopulmonary Resuscitation for Patients with Cancer According to Type of Cancer.
A meta-analysis by Reisfield et al (7) that included 42 studies published between 1966 and 2005 (n = 1,707) reported that 6.2% of cancer patients who underwent in-hospital CPR survived to hospital discharge. Survival to discharge was significantly higher for patients with solid tumors than for those with hematologic cancers (7.1% and 2% [odds ratio (OR), 3.75; 95% confidence interval (CI), 1.76–7.98; P = 0.001]). With respect to the extent of solid tumors, patients with localized tumors had better survival than patients with metastases (9.5% versus 5.6% [OR, 1.77; 95% CI, 1.0–3.14; P = 0.05]).
Survival rates according to the type of cancer are shown in Figure 3.
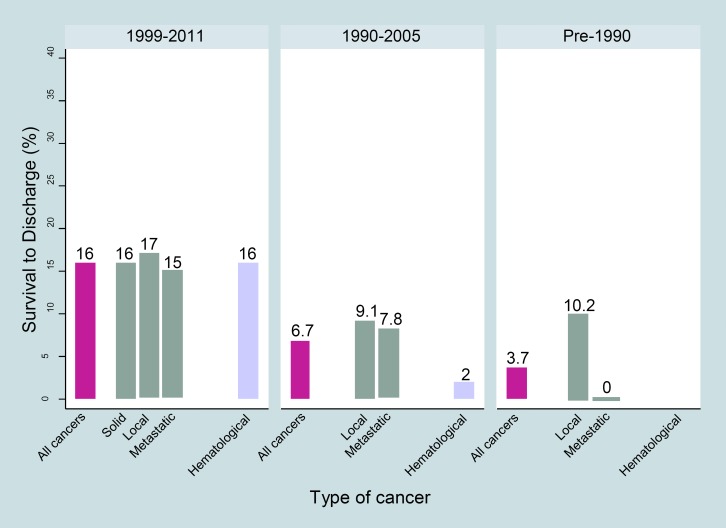
Studies published before 1990 (the year in which the first patient with metastatic cancer who underwent CPR survived) were compared with studies published since 1990. The meta-analysis reported a difference between the studies before and after 1990. While before 1990 no patient with metastatic disease who underwent CPR survived, studies published between 1990 and 2005 showed a pooled survival to hospital discharge of 7.8% (P < 0.001) (Figure 4).
Figure 4: Survival Following In-Hospital Cardiopulmonary Resuscitation for Patients with Cancer According to Type of Cancer and Period.
Another large study (10) was based on a cohort of 49,130 adults who experienced cardiopulmonary arrest (from January 2000 to September 2004) documented in the US National Registry of Cardiopulmonary Resuscitation. As in the meta-analysis, a 7.8% survival to discharge of patients with metastatic or hematologic malignancy was reported. On the other hand Taran et al, (9) who studied patients from 1999 to 2011, reported a considerably higher survival 30 days after CPR (15%) for patients with metastatic disease (Figure 4).
It could be assumed that advances in CPR have improved survival rates in patients with metastatic cancer. However, because the “do not attempt resuscitation” orders that became more common in recent years could have influenced the frequency of administering CPR in patients with more advanced disease, the discrepancy in reported survival rates between prior studies and more recent studies could be due to selection bias in more recent studies. An example is the study by Lin et al, (8) which reported that, between 1997 and 2004, there was a 58.3% decrease in the number of patients with cancer who received CPR, mainly because the Hospice Palliative Care Act was implemented around the year 2000 in the country where the study took place. The Act clearly regulated the right to specify “do not attempt resuscitation.” During the same period the rate of performing CPR in patients without cancer decreased by only 16.4%, less than the rate for cancer patients (P < 0.001).
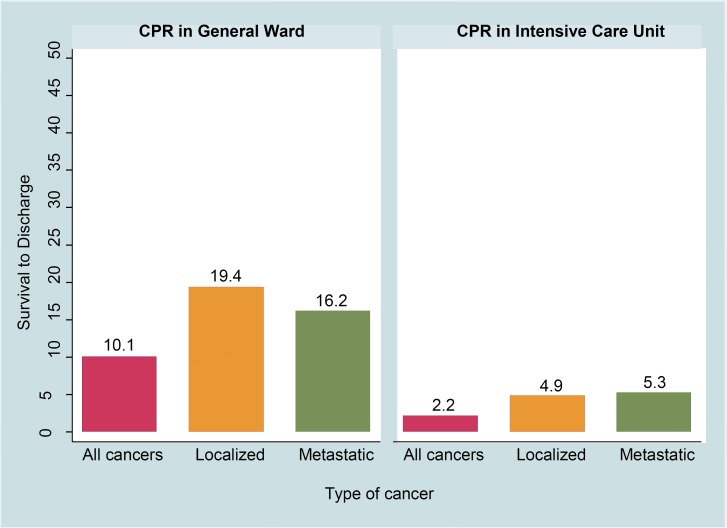
In their meta-analysis, Reisfield et al (7) also stratified patients according to the place of cardiac arrest and reported that patients who had CPR in intensive care units had one-fifth the chance of survival to discharge than patients who received CPR in general wards (2.2% [95% CI, 0.0–4.6] versus 10.1% [95% CI, 3.5–16.6]; OR, 4.97 [95% CI, 2.3–10.74; P < 0.001]) (Figure 5).
Figure 5: Survival to Discharge Following In-Hospital Cardiopulmonary Resuscitation for Patients with Cancer According to Location of Cardiac Arrest.
Abbreviation: CPR, cardiopulmonary resuscitation.
Survival After Out-of-Hospital Cardiopulmonary Resuscitation
Survival of cancer patients after out-of-hospital cardiac arrest was investigated by one small study (n = 41). (11) Cardiopulmonary resuscitation for patients included in this study had been initiated either out of hospital or in emergency departments. In these patients rate of immediate survival was 43% and rate of survival to discharge was 17%. Only 2 patients (4.9%) in this series were discharged home.
Outcomes of Cardiopulmonary Resuscitation in Patients with Chronic Health Conditions
Three studies (10;12;13) reported on the outcomes of CPR in patients with chronic health conditions (Table 3). One of these studies investigated survival of patients who experienced out-of-hospital cardiac arrest due to ventricular fibrillation (VF) and who received CPR from emergency medical services (EMS). (12)
Table 3:
Survival Rate for Patients with Chronic Health Conditions who Received Cardiopulmonary Resuscitation
| Study Characteristics | Larkin et al, 2010 (9) | Carew et al, 2007 (11)a | Lafrance et al, 2006 (12) |
|---|---|---|---|
| Country | United States | United States | Canada |
| Design | National registry for CPR | Retrospective cohort | Retrospective cohort |
| Study period | Jan 2000–Sept 2004 | Jan 1999–Dec 2003 | Aug 1997–Dec 2004 |
| Patienta |
|
|
24 |
| Agea Mean (SD) | NR |
|
64.5 (14.2) |
| Location of cardiac arrest | Hospital |
|
Hospital hemodialysis unit |
| Health condition | Variety | Heart disease 50.7% | Renal insufficiency |
| Survival of the event, % |
|
NR | ∼83.0 |
| Survival to discharge,a % |
|
|
|
Abbreviations: CI, confidence interval; CPR, cardiopulmonary resuscitation EMS, emergency medical services; MI, myocardial infarction; NR, not recorded; OR, odds ratio; SD, standard deviation; VF, ventricular fibrillation.
According to the number of chronic health conditions in the study by Carew et al.
Survival After In-Hospital Cardiopulmonary Resuscitation
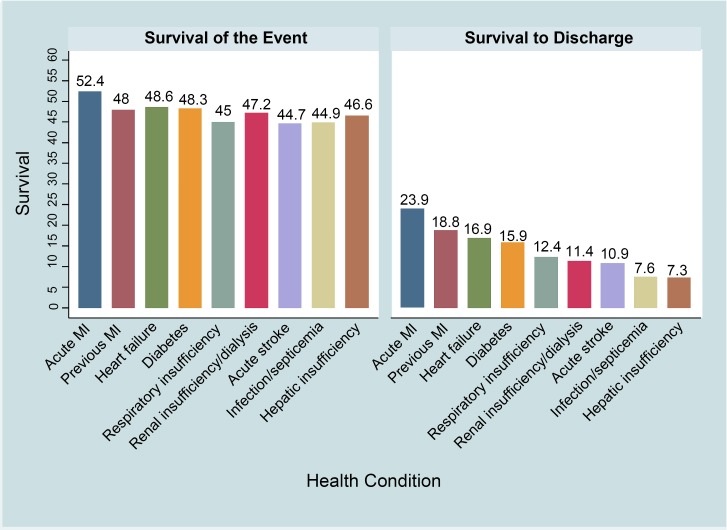
Larkin et al (10) reported rate of immediate survival and survival to discharge for several chronic health conditions. Although about half of these patients were immediately revived, many did not survive to hospital discharge. In addition, the type of health condition influenced survival. Patients who had myocardial infarction (MI) had better survival to discharge than patients who had other health conditions. The lowest reported survival to discharge was in patients with hepatic insufficiency (Figure 6).
Figure 6: Survival to Discharge Following In-Hospital Cardiopulmonary Resuscitation for Patients with Chronic Health Conditions According to Type of Chronic Health Condition.
Abbreviation: MI, myocardial infarction.
Another study investigated outcomes of CPR after cardiac arrest in a hospital hemodialysis unit. (13) Most CPR events (78%) occurred during the hemodialysis treatment. Of the 38 events, 24 were true cardiac arrest. Among these patients, 48-hour, 30-day, and 58-day survival was 83%, 75%, and 58.3%, respectively.
Survival After Out-of-Hospital Cardiopulmonary Resuscitation
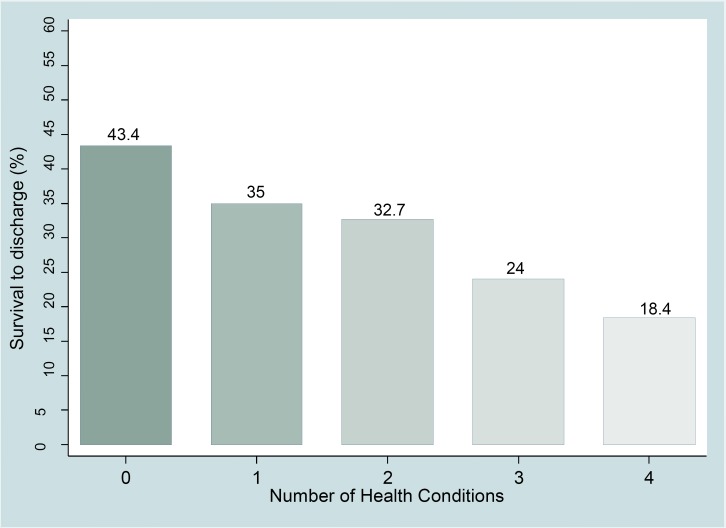
A study of patients who had cardiac arrest out of hospital because of VF and who received CPR by EMSs examined the association between the number of chronic health conditions and survival after CPR. (12) This study showed that survival to discharge decreased as the number of chronic health conditions increased (Figure 7). Increasing count of chronic health conditions was associated with older age, female sex, unwitnessed arrest, and nonpublic location.
Figure 7: Survival to Discharge Following Out-of-Hospital Cardiopulmonary Resuscitation for Patients with Chronic Health Conditions According to the Number of Chronic Health Conditions.
Increasing numbers of chronic health conditions were inversely associated with the chance of survival to hospital discharge, and each successive increase in numbers of chronic health condition resulted in 16% lower chance of survival (adjusted OR [95% CI], 0.84 [0.74–0.95]). This relationship was also associated with EMS response time. When EMS response time was 8 minutes, the OR decreased to 0.72, and each successive increase in the number of chronic health conditions resulted in 28% lower chance of survival. When EMS response time was 3 minutes, OR increased to 0.95 and each successive increase in the number of chronic health conditions resulted in only 5% lower chance of survival (Table 4).
Table 4:
Survival to Discharge According to Emergency Medical Services Response Time
| EMS Response Time | OR (95% CI) |
|---|---|
| 3 minutes | 0.95 (0.79–1.14) |
| 8 minutes | 0.72 (0.59–0.88) |
Abbreviations: CI, confidence interval; EMS, emergency medical service; OR, odds ratio.
Outcomes of Cardiopulmonary Resuscitation in Older Patients
Characteristics of studies that investigated the outcomes of CPR among older patients are shown in Table 5.
Table 5:
Survival Rate of Patients who Received Cardiopulmonary Resuscitation According to Patient Age
| Author, Year | Country | Study Design | Study period | Patients | Age Mean (SD) or Median (IQR) | Location of Cardiac Arrest | Discharge Destination % |
|---|---|---|---|---|---|---|---|
| Menon et al, 2014 (14) | United States | Review of Medicare data | 1992–2005 | Received CPR once: 413,403 Received CPR more than once: 7,991 | NR | Hospital | One episode:
|
More than one episode:
|
|||||||
| P < 0.001 for one vs. more than one episode for home discharge | |||||||
| Xue et al, 2013 (15) | China | CPR registry | Jan 2005–Dec 2011 | 725 | 46.94 (19.05) | In-hospital ED/out of hospital | NR |
| Abbo et al, 2013 (16) | United States | National CPR registry | Jan 2000–Feb 2008 | Community, independent: 20,532 | Community, independent: 76 (71–82) | Hospital | NR |
| Community, dependent: 2,952 | Community, dependent: 78 (72–84) | ||||||
| Nursing home, independent: 1,546 | Nursing home, independent: 79 (73–85) | ||||||
| Nursing home, dependent: 1,299 | Nursing home, dependent: 80 (74–86) | ||||||
| Larkin et al, 2010 (10) | United States | National CPR registry | Jan 2000–Sept 2004 | 5,494 | 66.7 (15.7) Included ≥ 18 | Hospital |
Abbreviations: CPR, cardiopulmonary resuscitation; ED, emergency department; IQR, interquartile range; NR, not reported; SD, standard deviation.
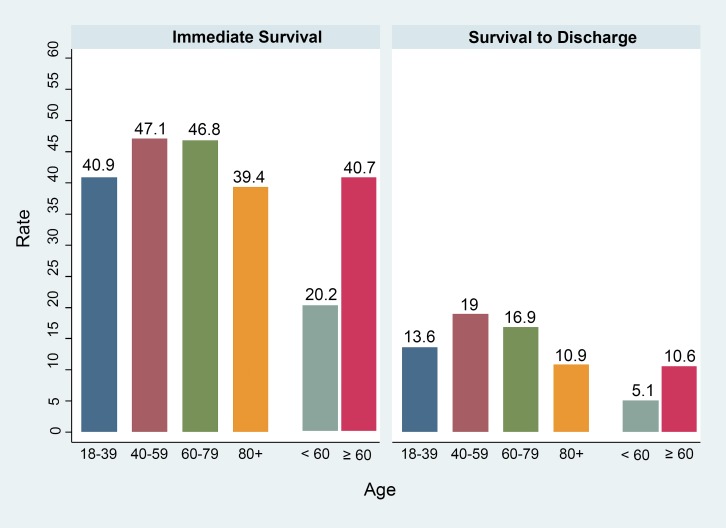
The study that used the US National Registry of Cardiopulmonary Resuscitation (10) found an inverse but linear relationship with age and survival. However, the data suggested that biological age is less important than functional status and other risk factors when estimating survival (Figure 8).
Figure 8: Survival Following In-Hospital Cardiopulmonary Resuscitation According to Age Categories: Reports From 2 Studies.
Another registry of CPR (15) also showed that age was not associated with outcomes of CPR. In this study, patients younger than age 60 years had lower chance of survival after CPR than patients age 60 years or older. This difference was due to the higher prevalence of multiorgan failure, terminal illnesses, and traumatic injuries among younger patients (Figure 8).
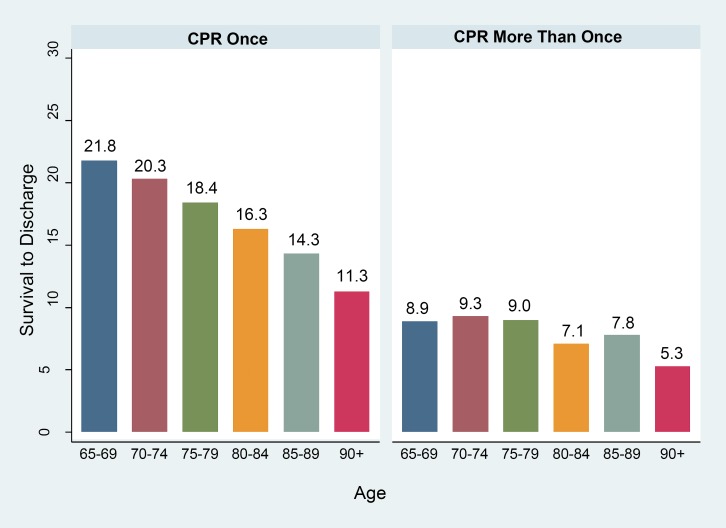
Menon et al (14) analyzed data from 421,394 patients who underwent CPR and showed association between age and survival. They also showed that undergoing multiple CPRs during hospitalization is associated with a substantially lower rate of survival to discharge than undergoing a single CPR (Figure 9).
Figure 9: Survival to Discharge Following In-Hospital Cardiopulmonary Resuscitation: Patients 65 Years and Older According to Age and Frequency of Cardiopulmonary Resuscitation.
Abbreviation: CPR, cardiopulmonary resuscitation.
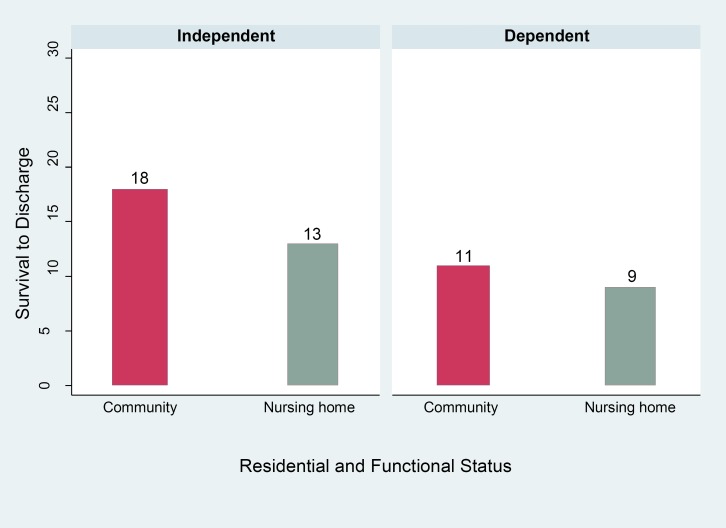
The study by Abbo et al (16) examined the association of functional status with the outcomes of CPR using the United States National Registry of Cardiopulmonary Resuscitation. This study stratified patients into 4 groups according to their dependency in performing activities of daily living (ADL) and residential status (community dwelling or nursing home). In this study survival with good neurologic function was considered as a secondary outcome.
The results showed that community-dwelling patients independent in performing ADL had the highest rate of survival to discharge (18%) and that nursing home residents dependent in ADL had the lowest rate of survival (9%) (Figure 10).
Figure 10: Survival to Discharge Following In-Hospital Cardiopulmonary Resuscitation for Patients 65 Years and Older According to Residential and Functional Status.
Adjusted analysis showed that patients dependent in ADL had lower rate of survival to discharge regardless of residence status. Odds ratios and 95% CI for community-dwelling dependent and nursing home dependent versus community-dwelling independent were 0.76 (0.63–0.92) and 0.79 (0.64–0.96), respectively.
Survival to discharge with good neurologic outcome was also higher in community-dwelling patients independent in ADL than in the other 3 groups (15% for community dwelling, independent; 11% for nursing home, independent; 10% for community dwelling, dependent; 8% for nursing home, dependent; P < 0.001).
Conclusions
Recent studies report higher chance of survival in cancer patients. This could reflect the impact of “do not resuscitate” orders in recent years for patients with end-stage cancer.
Overall, patients with cancer have lower chances of survival following cardiopulmonary resuscitation (CPR) than patients without cancer.
Severity of illness in cancer patients can affect survival following CPR. A meta-analysis showed survival to discharge of patients with cancer who receive CPR in intensive care units is 2.2%, one-fifth the rate of survival of patients with cancer who receive CPR in general wards (10.1%), despite constant monitoring in intensive care units.
Patients with cancer who have cardiac arrest out of hospital and receive CPR either out of hospital or in emergency departments have survival to discharge rates similar to those of hospitalized patients who receive CPR in hospital.
The type and the number of chronic health conditions can affect survival following CPR. Studies show that patients who have myocardial infarction have better survival to discharge following CPR than patients with other health conditions and that patients undergoing hemodialysis have a high chance of survival following CPR.
Older age is not necessarily a factor in lowering the odds of survival, but functional dependence and undergoing multiple CPRs, particularly in advanced age, can reduce the chance of survival following CPR.
Response time of emergency medical services contributes to the chance of survival following out-of-hospital CPR in patients with chronic health conditions.
Acknowledgements
Editorial Staff
Elizabeth Jean Betsch, ELS
Medical Information Services
Corinne Holubowich, BEd, MLIS
Health Quality Ontario's Expert Advisory Panel on End-of-Life Care
| Panel Member | Affiliation(s) | Appointment(s) |
|---|---|---|
| Panel Co-Chairs | ||
| Dr Robert Fowler | Sunnybrook Research Institute University of Toronto | Senior Scientist Associate Professor |
| Shirlee Sharkey | St. Elizabeth Health Care Centre | President and CEO |
| Professional Organizations Representation | ||
| Dr Scott Wooder | Ontario Medical Association | President |
| Health Care System Representation | ||
| Dr Douglas Manuel | Ottawa Hospital Research Institute University of Ottawa | Senior Scientist Associate Professor |
| Primary/ Palliative Care | ||
| Dr Russell Goldman | Mount Sinai Hospital, Tammy Latner Centre for Palliative Care | Director |
| Dr Sandy Buchman | Mount Sinai Hospital, Tammy Latner Centre for Palliative Care Cancer Care Ontario University of Toronto | Educational Lead Clinical Lead QI Assistant Professor |
| Dr Mary Anne Huggins | Mississauga Halton Palliative Care Network; Dorothy Ley Hospice | Medical Director |
| Dr Cathy Faulds | London Family Health Team | Lead Physician |
| Dr José Pereira | The Ottawa Hospital University of Ottawa | Professor, and Chief of the Palliative Care program at The Ottawa Hospital |
| Dean Walters | Central East Community Care Access Centre | Nurse Practitioner |
| Critical Care | ||
| Dr Daren Heyland | Clinical Evaluation Research Unit Kingston General Hospital | Scientific Director |
| Oncology | ||
| Dr Craig Earle | Ontario Institute for Cancer Research Cancer Care Ontario | Director of Health Services Research Program |
| Internal Medicine | ||
| Dr John You | McMaster University | Associate Professor |
| Geriatrics | ||
| Dr Daphna Grossman | Baycrest Health Sciences | Deputy Head Palliative Care |
| Social Work | ||
| Mary-Lou Kelley | School of Social Work and Northern Ontario School of Medicine | |
| Lakehead University | Professor | |
| Emergency Medicine | ||
| Dr Barry McLellan | Sunnybrook Health Sciences Centre | President and Chief Executive Officer |
| Bioethics | ||
| Robert Sibbald | London Health Sciences Centre University of Western Ontario | Professor |
| Nursing | ||
| Vicki Lejambe | Saint Elizabeth Health Care | Advanced Practice Consultant |
| Tracey DasGupta | Sunnybrook Health Sciences Centre | Director, Interprofessional Practice |
| Mary Jane Esplen | De Souza Institute University of Toronto | Director Clinician Scientist |
Appendices
Appendix 1: Literature Search Strategies
Search date: January 10, 2014
Database: EBM Reviews - Cochrane Database of Systematic Reviews <2005 to November 2013>, EBM Reviews - ACP Journal Club <1991 to December 2013>, EBM Reviews - Database of Abstracts of Reviews of Effects <4th Quarter 2013>, EBM Reviews - Cochrane Central Register of Controlled Trials <December 2013>, EBM Reviews - Cochrane Methodology Register <3rd Quarter 2012>, EBM Reviews - Health Technology Assessment <4th Quarter 2013>, EBM Reviews - NHS Economic Evaluation Database <4th Quarter 2013>, Embase <1980 to 2014 Week 01>, Ovid MEDLINE(R) <1946 to November Week 3 2013>, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations <January 09, 2014>
-
1
exp Terminal Care/
-
2
exp Palliative Care/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed or exp Terminally Ill/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed
-
3
exp palliative therapy/ use emez or exp terminally ill patient/ use emez or exp terminal disease/ use emez or exp dying/ use emez
-
4
((End adj2 life adj2 care) or EOL care or (terminal* adj2 (care or caring or ill* or disease*)) or palliat* or dying or (Advanced adj3 (disease* or illness*)) or end stage*).ti,ab.
-
5
or/1–4
-
6
exp Cardiopulmonary Resuscitation/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed
-
7
exp resuscitation/ use emez
-
8
exp Resuscitation Orders/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed
-
9
((resuscitation* adj2 (cardiopulmonary or cardio pulmonary)) or code blue* or (mouth adj2 mouth adj2 resuscitation*) or basic cardiac life support* or BCLS or advanced cardiac life support* or ACLS or CPR or “do not resuscitate” or DNR).ti,ab.
-
10
or/6–9
-
11
5 and 10
-
12
limit 11 to english language [Limit not valid in CDSR,ACP Journal Club,DARE,CCTR,CLCMR; records were retained]
-
13
limit 12 to yr=“2004 -current” [Limit not valid in DARE; records were retained]
-
14
Case Reports/ or Comment.pt. or Editorial.pt. or Letter.pt. or Congresses.pt.
-
15
Case Report/ or Comment/ or Editorial/ or Letter/ or conference abstract.pt.
-
16
or/14–15
-
17
13 not 16
-
18
remove duplicates from 17
EBSCO Cumulative Index to Nursing & Allied Health Literature
| # | Query |
|---|---|
| S1 | (MH “Terminal Care+”) |
| S2 | (MH “Palliative Care”) |
| S3 | (MH “Terminally Ill Patients+”) |
| S4 | ((End N2 life N2 care) or EOL care or (terminal* N2 (care or caring or ill* or disease*)) or palliat* or dying or (advanced N3 (disease* or illness*)) or end stage*) |
| S5 | S1 OR S2 OR S3 OR S4 |
| S6 | (MH “Resuscitation, Cardiopulmonary+”) |
| S7 | (MH “Resuscitation Orders”) |
| S8 | ((resuscitation* N2 (cardiopulmonary or cardio pulmonary)) or code blue* or (mouth N2 mouth N2 resuscitation*) or basic cardiac life support* or BCLS or advanced cardiac life support* or ACLS or CPR or “do not resuscitate” or DNR) |
| S9 | S6 OR S7 OR S8 |
| S10 | S5 AND S9 |
| S11 | S5 AND S9 Limiters – Publication Type: Case Study, Commentary, Conference, Editorial, Letter |
| S12 | S10 NOT S11 |
| S13 | S10 NOT S11 Limiters - Published Date: 20040101-current; English Language |
Appendix 2: Evidence Quality Assessment
Table A1:
GRADE Evidence Profile
| Number of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Immediate Survival | |||||||
| 8 observational | Serious limitations (−1)a | No serious limitations | No serious limitations | No serious limitations | Undetected | N/A | ⊕⊕ Low |
| 1 meta-analysis | Serious limitations (−1)a | No serious limitations | No serious limitations | No serious limitations | Undetected | N/A | ⊕⊕ Low |
| Survival to Discharge/30 Day-Survival | |||||||
| 9 observational | Serious limitations (−1)a | No serious limitations | No serious limitations | No serious limitations | Undetected | N/A | ⊕⊕ Low |
| 1 meta-analysis | Serious limitations (−1)a | No serious limitations | No serious limitations | No serious limitations | Undetected | N/A | ⊕⊕ Low |
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; N/A, not applicable.
Studies were retrospective.
References
- (1).Heyland DK, Frank C, Groll D, Pichora D, Dodek P, Rocker G, et al. Understanding cardiopulmonary resuscitation decision making: perspectives of seriously ill hospitalized patients and family members. Chest. 2006 Aug; 130(2): 419–28. [DOI] [PubMed] [Google Scholar]
- (2).Adams DH, Snedden DP. How misconceptions among elderly patients regarding survival outcomes of inpatient cardiopulmonary resuscitation affect do-not-resuscitate orders. J Am Osteopath Assoc. 2006 Jul; 106(7): 402–4. [PubMed] [Google Scholar]
- (3).Ehlenbach WJ, Barnato AE, Curtis JR, Kreuter W, Koepsell TD, Deyo RA, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009 Jul 2; 361(1): 22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Ebell MH, Becker LA, Barry HC, Hagen M. Survival after in-hospital cardiopulmonary resuscitation. A meta-analysis. J Gen Intern Med. 1998 Dec; 13(12): 805–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011 Apr; 64(4): 380–2. [DOI] [PubMed] [Google Scholar]
- (6).Goodman C. Literature searching and evidence interpretation for assessing health care practices. SBU Report No. 119E. Stockholm, Sweden: Swedish Council on Technology Assessment in Health Care; 1996. 1–81 p. [DOI] [PubMed] [Google Scholar]
- (7).Reisfield GM, Wallace SK, Munsell MF, Webb FJ, Alvarez ER, Wilson GR. Survival in cancer patients undergoing in-hospital cardiopulmonary resuscitation: a meta-analysis. Resuscitation. 2006 Nov; 71(2): 152–60. [DOI] [PubMed] [Google Scholar]
- (8).Lin M-H, Peng L-N, Chen L-K, Chen T-J, Hwang S-J. Cardiopulmonary resuscitation for hospital inpatients in Taiwan: an 8-year nationwide survey. Resuscitation. 2012; 83(3): 343–6. [DOI] [PubMed] [Google Scholar]
- (9).Taran A, Guarino M, Kolm P, Petrelli N. Cardiopulmonary resuscitation inpatient outcomes in cancer patients in a large community hospital. Del Med J. 2012; 84(4): 117–21. [PubMed] [Google Scholar]
- (10).Larkin GL, Copes WS, Nathanson BH, Kaye W. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: a report from the National Registry for Cardiopulmonary Resuscitation. Resuscitation. 2010 Mar; 81(3): 302–11. [DOI] [PubMed] [Google Scholar]
- (11).Hwang JP, Patlan J, de Achaval S. Escalante CP. Survival in cancer patients after out-of-hospital cardiac arrest. Support Care Cancer. 2010; 18(1): 51–5. [DOI] [PubMed] [Google Scholar]
- (12).Carew HT, Zhang W, Rea TD. Chronic health conditions and survival after out-of-hospital ventricular fibrillation cardiac arrest. Heart. 2007 Jun; 93(6): 728–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Lafrance JP, Nolin L, Senecal L, Leblanc M. Predictors and outcome of cardiopulmonary resuscitation (CPR) calls in a large haemodialysis unit over a seven-year period. Nephrol Dial Transplant. 2006 Apr; 21(4): 1006–12. [DOI] [PubMed] [Google Scholar]
- (14).Menon PR, Ehlenbach WJ, Ford DW, Stapleton RD. Multiple in-hospital resuscitation efforts in the elderly. Crit Care Med. 2014; 42(1): 108–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Xue J-K, Leng Q-Y, Gao Y-Z, Chen S-Q, Li Z-P, Li H-P, et al. Factors influencing outcomes after cardiopulmonary resuscitation in emergency department. World J Emerg Med. 2013; 4(3): 183–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Abbo ED, Yuen TC, Buhrmester L, Geocadin R, Volandes AE, Siddique J, et al. Cardiopulmonary resuscitation outcomes in hospitalized community-dwelling individuals and nursing home residents based on activities of daily living. J Am Geriatr Soc. 2013 Jan; 61(1): 34–9. [DOI] [PubMed] [Google Scholar]