Abstract
Objectives
Failure to adapt to limitations in control may place older adults at risk for suicidal behavior. The present study examined the relation between control strategies, depressive symptoms, and suicidal ideation in older adults with health-related limitations.
Methods
Cross-sectional study of 50 older adult (aged 65–94) primary care patients with health-related limitations.
Results
Compensatory primary control strategies, characterized, e.g., by seeking help from others, were associated with lower levels of suicidal ideation, independent of depressive symptoms. Selective primary control strategies (e.g., persistence) were also associated with reduced suicidal ideation independent of depressive symptoms, but only when a low level of compensatory primary control strategies was endorsed. Selective secondary control strategies were associated with higher suicidal ideation, whereas compensatory secondary control strategies (e.g., goal disengagement) were unrelated in this sample after controlling for covariates.
Conclusions
Findings demonstrate that primary care patients with functional limitations who are not striving to meet their goals, either through persistence or by seeking help from others, are at elevated risk of suicidal thinking.
Keywords: geriatric, suicide, depression, control strategies, functional limitations, primary care
Suicide is an important public health problem that disproportionately affects older adults. In 2010, adults age 65 or older comprised 13.0% of the U.S. population but represented 15.6% of the suicides [1]. Risk of suicide is especially elevated in men aged 75 and older, whose rate is nearly triple the overall suicide rate in the United States [2]. Depression, the predominant risk factor for suicide among older adults, is implicated in the majority of suicides in this age group [3]. Nevertheless, it is a non-specific risk factor, as the vast majority of older adults with a depressive disorder do not die by suicide. Thus, there is a pressing need to identify factors independently associated with suicide risk in older adults.
Physical illness and disability are associated with increased risk of suicide in late life, and effects appear to be partially independent of depression [4]. Although there may be multiple explanations for the link between physical health problems and suicide, evidence suggests that difficulties adapting to physical limitations may play a role. Among health problems associated with suicide in late life, many are chronic and potentially disabling conditions, including some types of cancer, neurological disorders, congestive heart failure, chronic pulmonary disorder, renal failure and impairments in vision and hearing [4]. Functional impairment has been linked to suicide risk in older adults [5, 6; cf. 7], although the possibility that functional impairment explains the relation between physical illness and suicide remains to be evaluated. Additional evidence comes from studies showing that among individuals with cancer, the risk of suicide is especially elevated early in the course of the disease [8], consistent with the possibility that suicide risk is related to problems adapting to the disease. Furthermore, qualitative reports suggest that older adults who died by suicide had pronounced problems adapting to loss of control, including limitations in physical functioning [9]. Taken together, these findings are consistent with the proposition that suicidal ideation in late life may be related, in part, to problems of adaptation.
The Motivational Theory of Life Span Development [10] provides a framework for understanding mental health outcomes in the context of age-associated limitations in physical functioning. According to this theory, individuals of all ages prefer to attain their goals by exerting control directly on their environment, but opportunities to exert control tend to decline with age. Individuals who exhibit flexibility in coping with their changed circumstances should have the most positive outcomes. Successful adaptation theoretically requires changing strategies for attaining goals as well as managing motivation through cycles of disengaging from unobtainable goals and reengaging with more feasible ones.
Heckhausen and colleagues [10] define control strategies along two dimensions: selective versus compensatory and primary versus secondary. Selective strategies reflect investment of one’s own effort to attain a goal. In contrast, compensatory strategies involve recruitment of external resources, such as asking for help from others. Primary control strategies are those aimed at changing the environment, whereas secondary control strategies are focused on changing the self. The theory specifies that selective primary control strategies are preferred across the lifespan, but as individuals age and encounter limitations in the ability to exert primary control, use of other strategies becomes adaptive.
Research supports the theory, showing that control strategies change in predicted ways with normal aging [e.g., 11], as well as following onset of health problems among older adults [12]. Furthermore, control strategies reflecting an active engagement in personal goals are associated with lower levels of depressive symptoms [13], and buffer the effects of health problems on both depressed mood and the stress response [14]. In addition, a growing literature has shown that disengagement from unobtainable goals (compensatory secondary control) is associated with better mental health outcomes relative to continued striving [e.g., 15, 16, 17]. Research also supports theoretical predictions that specific type of control strategy employed should be related to outcomes, as successful aging involves a match between opportunity for control and strategy used to exert control [10]. Similarly, Clark’s model of late life suicidal behavior suggests that individuals who have limited flexibility will have the greatest difficulty adapting to the losses associated with aging and will consequently be at risk of suicide [18]. Consistent with these theoretical frameworks, evidence shows that individuals who continue striving (selective primary control) without employing a more diverse repertoire of control strategies are at risk of poor outcomes when they encounter age-related limitations in their ability to exercise control [e.g., 15, 16, 19].
Compensatory primary control strategies, which involve the recruitment of external resources, may be particularly relevant for older adults facing health-related limitations. Among both older [20] and middle-aged adults [21] with vision impairment, compensatory primary control strategies were the most frequently endorsed strategies. Strategies related to seeking or accepting help from others were more often used by participants with more severe impairments, whereas use of technical aids was more frequently used by participants with the least severe impairments. These strategies may also be particularly adaptive. In a prospective study, older men with “health-induced task-related restrictions” who endorsed primary control striving (“persistence”) but did not endorse help seeking or task modification were at increased risk of subsequent hospitalization for medical or other reasons [19]. The Motivational Theory of LifeSpan Development also provides a basis for predicting suicidal outcomes in late life. For individuals who are not able to attain goals through direct effort (selective primary control), are not willing or able to seek help (compensatory primary control) and do not disengage from the goal (compensatory secondary control), hopelessness and suicidal thinking may ensue. Given this conceptual rationale, as well as previous research demonstrating that older adults who die by suicide are characterized by an inability to adapt to age-related losses in functioning [9], endorsement of a diverse set of control strategies in the face of independence-limiting conditions should be associated with less suicidal ideation than continued striving alone.
In summary, specific profiles of control strategies have been shown to predict mental and physical health outcomes in older adults with health problems, but the relation between control strategies and suicidal ideation has not yet been tested. The purpose of the present study was to examine this relation in older primary care patients with functional limitations. Our first hypothesis, based on existing research, was that greater endorsement of compensatory primary control strategies would be associated with lower levels of both depressive symptoms and suicidal ideation, controlling for other types of control strategies. Given our conceptualization that failure to adapt to limitations may lead specifically to a hopeless state, we also anticipated that the relation between compensatory primary control strategy endorsement and suicidal ideation would be partially independent of the effects of depressive symptoms. Our second hypothesis, also based in prior empirical literature, was that greater endorsement of secondary control strategies (both selective and compensatory) would be associated with lower levels of depressive symptoms and suicidal ideation.
Methods
Participants
Older adult participants were recruited from the waiting room of a university-affiliated primary care clinic in the mid-Atlantic region of the United States. Individuals aged 65 and older were invited to participate in a questionnaire-based study of sleep, functioning and mood. Eighty-one older adults completed the questionnaire. For the current study, the sample consisted of individuals who endorsed experiencing a health-related functional impairment (n = 50, age range: 65–94). Participants were included if they either: 1) endorsed one or more specific limitations in their ability to carry out activities of daily living (see below); or 2) answered YES to the question, “Does your health keep you from doing things you would like to do?” Eighteen percent (n=9) of participants also endorsed needing assistance with basic activities of daily living (see below).
Characteristics of the sample are displayed in Table 1. Consistent with the population of the region, a high proportion of participants were White. In addition, the sample consisted of a highly educated group, likely due to being a university-affiliated clinic. For example, 45.7% of the sample reported having at least a bachelor’s degree, compared to 27% of men and 16% of women in a 2008 national survey of adults age 65 and older [22]. As would be expected in this sample of primary care patients with functional impairment, participants endorsed physical illnesses on a self-report list of common diseases and disorders at rates similar to or higher than rates reported in national surveys of older adults. For example, arthritis was reported by 63% (n=30) of the present sample compared to 50% in a national survey [22].
Table 1.
Sample Characteristics
| Characteristic | n (%) | M (SD) |
|---|---|---|
| Age | 74.5 (7.3) | |
| Gender: female | 29 (60.4) | |
| Ethnicity (%) | ||
| White | 46 (95.8) | |
| African American | 1 (2.1) | |
| Native American | 1 (2.1) | |
| Marital Status | ||
| Single | 2 (4.3) | |
| Married | 29 (61.7) | |
| Divorced | 5 (10.6) | |
| Widowed | 11 (23.4) | |
| Highest level of education | ||
| Some high school | 2 (4.3) | |
| High school/GED | 12 (26.1) | |
| Some college | 7 (15.2) | |
| College degree | 21 (45.7) | |
| Other (not specified) | 1 (2.2) | |
| Current occupational status | ||
| Full-time | 3 (6.5) | |
| Part-time | 2 (4.4) | |
| Homemaker | 4 (8.7) | |
| Retired | 28 (60.9) | |
| Disabled | 9 (19.6) | |
| Physical illness | ||
| Cancer | 10 (21.3) | |
| Heart Attack | 5 (10.4) | |
| Stroke | 7 (14.9) | |
| Congestive Heart Failure | 5 (10.6) | |
| Asthma | 6 (12.8) | |
| Kidney Failure | 5 (10.6) | |
| Arthritis | 30 (62.5) | |
| Diabetes | 11 (22.9) | |
| Chronic Pain | 7 (14.9) | |
Note. N = 46–48, with variation due to missing data.
Measures
Optimization of Primary and Secondary Control Scale
The Optimization of Primary and Secondary Control scale (OPS) [23] is a 32-item measure of control strategies based on the Motivational Theory of Life-Span Development [10]. The measure includes four, 8-item subscales, including Selective Primary Control (SPC; e.g., “When obstacles get in my way I put in more effort.”), Compensatory Primary Control (CPC; e.g., ”When I get stuck on a task, I don’t hesitate asking others for advice”), Selective Secondary Control (SSC; e.g., “When I have decided on something, I avoid anything that could distract me”), and Compensatory Secondary Control (CSC; e.g., “When I have not accomplished something important, I console myself by thinking about other area where I had more success”). Participants indicated how true each statement was for them (from never true to almost always true). SPC, CPC, and SSC have demonstrated adequate internal consistency in previous research with older adults with disability (α = .68–.80; [12]). Internal consistency for CSC was found to be low (α = .59 [12]). In the current sample, reliability for three of the subscales was acceptable (SPC α = .85; CPC α = .84; SSC α = .75), whereas reliability of the CSC scale was somewhat low (α = .50).
Considering the relatively low alpha for the CSC scale, we conducted a principal components analysis (PCA) with Varimax rotation for each of the subscales. Results suggested that that the SPC and SSC subscales each formed a single factor, but the CPC and CSC subscales were better represented by multiple factors (see Table 2). The PCA of the CPC subscale yielded two factors: seeking help from others (CPC Help; 4 items, including the example above, α = .87) and seeking new or modified ways to solve problems (CPC Modify; 4 items, including “When I cannot get to a goal directly, I sometimes choose a roundabout way to achieve it,” α = .75). The PCA of the CSC subscale yielded three factors: social and intra-individual comparisons (CSC Compare; 4 items, including the example above, α = .68), goal disengagement (CSC Disengage; 2 items, e.g., “When it turns out that I cannot attain a goal in any way I let go of it,” α = .66), and self-protective attributions (CSC Self-Protect; 2 items, e.g., “When I do not reach a goal, I often tell myself that it wasn’t my fault,” α = .72). Analyses were performed using the full subscales and repeated using each of the two CPC factors and the three CSC factors. Except where findings differ, only the results from the latter, more detailed analyses are reported here.
Table 2.
Factor Structure of Compensatory Primary and Secondary Control Subscales
| Strategy | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|
| Compensatory Primary Control | |||
| Help | |||
| when difficulties too great, ask others for advice | .90 | .08 | |
| when can’t solve problem alone, ask others for help | .88 | .14 | |
| when obstacles, get help from others | .79 | .16 | |
| when stuck, ask others for advice | .76 | .12 | |
| Modify | |||
| when obstacles, find another way | .13 | .83 | |
| when obstacles, find even unusual way | −.15 | .82 | |
| when not making progress, find new way | .37 | .70 | |
| if cannot achieve goal directly, use roundabout way | .27 | .65 | |
| Compensatory Secondary Control | |||
| Compare | |||
| when in difficulty, remind self I’m better off than others | .82 | −.11 | −.18 |
| when bad things happen, others are worse off | .77 | −.16 | .10 |
| when doubt self, remind of past accomplishments | .65 | .28 | .11 |
| when goal not accomplished, think of other successes | .60 | .29 | .02 |
| Self-Protect | |||
| if goal not reached, not my fault | .02 | .89 | .04 |
| if does not work out, was bad luck | .08 | .79 | −.12 |
| Disengage | |||
| if cannot attain goal, let go of it | .03 | −.17 | .86 |
| when goal too difficult, put out of my thoughts | .01 | .20 | .81 |
Note. N = 76.
Center for Epidemiological Studies Depression Scale – Revised
The Center for Epidemiological Studies Depression Scale – Revised (CESD-R) [24] is a revision of the original CES-D measure [25]. Changes include improved coverage of symptoms required for a diagnosis of major depressive disorder and elimination of reverse-scored items. The CESD-R is a 20-item measure of depressive symptoms with scores ranging from 0–60. Scores of 16 or greater are indicative of clinically significant depressive symptoms. Participants indicated how often they experienced each symptom over the past week (not at all or less than one day [0 points]; 1–2 days [1 point], 3–4 days [2 points], 5–7 days [3 points], or nearly every day for the past two weeks [3 points]). Past research using the CESD-R with older adults has demonstrated excellent internal consistency (α = .93; [26]) and good convergent validity with the original CES-D [24]. In the current sample, reliability was excellent (α = .93). Sixteen percent of the sample scored in the clinical range (16 or greater).
Geriatric Suicide Ideation Scale
The Geriatric Suicide Ideation Scale (GSIS) [27] is a 31-item measure of suicidal ideation designed specifically for older adults. The measure contains distinct subscales measuring suicide ideation, death ideation, meaning in life, and loss of personal and social worth. For the current study, the 10-item suicide ideation subscale was used because it measures suicidal ideation specifically, whereas the other subscales measure related constructs. The suicide ideation subscale of the GSIS has been validated as a measure of suicide ideation [27]. Analyses were repeated using the full GSIS instrument as an outcome measure; because results were substantially similar to those obtained with the suicidal ideation subscale, they are not reported here. Items are scored on a Likert-type scale from 1 (strongly disagree) to 5 (strongly agree). High scores reflect greater suicidal ideation (min = 10, max = 50). The GSIS suicide ideation subscale has demonstrated adequate internal constancy in previous studies with older adults (α = .82; [27]) as well as convergent validity with respect to other measures of suicide ideation and moderate to strong correlations with related constructs (e.g., depressive symptoms [27]). Suicidal ideation was present in the current sample, as 6.7% of participants (n=3) scored above the mean of 19 reported in a psychiatric sample [27]. Reliability for the subscale in the current sample was good (α = .80).
Activities of Daily Living and Instrumental Activities of Daily Living
Both the Activities of Daily Living (ADL) [28] and Instrumental Activities of Daily Living (IADL) [29] scales assess functional ability in older adults. Whereas the ADL scale measures basic activities, such as bathing and dressing, the IADL scale assesses more complex activities, such as housework and finances. The current study combined items from both scales to generate a 21-item assessment of functional ability, with higher scores indicating a higher level of functioning. Research findings support the unidimensional structure of the disability construct derived from combined ADL and IADL items [30]. Past research has demonstrated good internal consistency of the combined total score (α = .88; [30]) Participants were asked to rate their ability to perform a certain task (e.g., “Can you take your medicine correctly?”) by checking “I cannot perform this activity,” “I can perform this activity with some help,” or “I can perform this activity without any help.” These statements were scored from 0–2, with a maximum functional ability score of 42. In the current sample, reliability was excellent (α = .90).
Procedure
Data collection occurred between April and August 2010. Participants were recruited from the waiting room of a university-affiliated primary care clinic. Individuals 65 years or older were invited to take part in the research study. After a complete description of the study was provided to participants, written informed consent was obtained. Participants completed self-report questionnaires in the waiting-room or upon departure from the clinic. Upon completion of the study, participants received a list of referrals to mental health providers in the community and a $5 stipend for their participation. The study was conducted in accordance with an approved IRB protocol. All analyses were conducted using SAS (v. 9.2).
Results
Means, standard deviations, and bivariate correlations for all study variables are included in Table 3. SPC was not significantly related to depressive symptoms but, as expected, it was negatively associated with suicidal ideation, indicating that participants who endorsed greater engagement in strategies aimed at accomplishing goals through direct investment of effort reported lower suicidal ideation. A similar pattern of correlations emerged for CPC, indicating that participants who endorsed greater recruitment of external resources to achieve their goals reported lower suicidal ideation. Both of the CPC factors, help-seeking and modifying the task, were associated with lower levels of suicidal ideation. Participants who endorsed greater use of strategies aimed at disengaging from an unattainable goal reported lower levels of depressive symptoms, but none of the CSC factors was significantly related to suicidal ideation. The correlations of both social and intra-individual comparison and self-protective attribution factors with depressive symptoms were positive, but in both cases the correlations were small and non-significant.
Table 3.
Means, Standard Deviations, and Pearson’s Correlation Coefficients for Study Variables
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 74.5 | 7.3 | - | ||||||||||||
| 2. Sex | - | - | −.39 | - | |||||||||||
| 3. ADL | 37.0 | 7.2 | −.12 | .31 | - | ||||||||||
| 4. SPC | 23.3 | 5.2 | −.24 | .41 | .36 | - | |||||||||
| 5. CPC | 22.6 | 5.2 | −.12 | .20 | .30 | .68 | - | ||||||||
| 6. CPC Help | 11.5 | 3.3 | −.07 | .01 | .30 | .41 | .88 | - | |||||||
| 7. CPC Modify | 11.1 | 2.8 | −.18 | .32 | .19 | .76 | .83 | .46 | - | ||||||
| 8. SSC | 20.7 | 4.7 | −.21 | .11 | .17 | .71 | .47 | .30 | .52 | - | |||||
| 9. CSC | 18.8 | 3.8 | −.06 | −.39 | −.01 | .23 | .15 | .08 | .19 | .44 | - | ||||
| 10. CSC Compare | 10.9 | 2.8 | −.19 | −.25 | .26 | .38 | .37 | .36 | .25 | .48 | .78 | - | |||
| 11. CSC Disengage | 4.7 | 1.7 | .09 | −.03 | .04 | .11 | .01 | −.09 | .10 | .09 | .39 | −.04 | - | ||
| 12. CSC Self-Protect | 3.0 | 1.9 | .12 | −.21 | −.28 | −.20 | −.30 | −.31 | −.16 | .21 | .50 | .07 | .05 | - | |
| 13. CESD-R | 8.1 | 10.5 | −.01 | −.15 | −.16 | −.16 | −.22 | −.26 | −.11 | .00 | .30 | .25 | −.29 | .23 | - |
| 14. GSIS-SI | 12.0 | 3.1 | .08 | −.12 | −.16 | −.40 | −.45 | −.44 | −.31 | −.16 | −.05 | −.14 | −.23 | .12 | .64 |
Note. ADL = Activities of Daily Living (higher score reflects better functioning); SPC = Selective Primary Control; CPC = Compensatory Primary Control; SSC = Selective Secondary Control; CSC = Compensatory Selective Control; CESD-R = Center for Epidemiological Studies Depression Scale – Revised; GSIS-SI = Geriatric Suicide Ideation Scale-Suicide Ideation subscale; biserial correlations are reported for sex (0 = female, 1 = male); significant correlations, p < .05, shown in boldface type.
Regression analysis showed, in line with the first hypothesis, that the CPC Help factor was associated with lower levels of depressive symptoms when controlling for age, sex, ADLs and all other control strategies (Table 4, first column). As anticipated, the CPC subscale was associated with lower levels of suicidal ideation after controlling for covariates, including depressive symptoms (B = −.23, SE = .10, p < .05). This finding indicates that participants who endorsed compensatory primary control strategies to a greater extent reported lower suicidal ideation. When analyzing CPC subfactors, only Help approached significance (Table 4, second column). In the same model, SPC was found to be negatively associated with suicidal ideation, such that participants with greater direct investment of effort to accomplish goals reported lower suicidal ideation.
Table 4.
Multivariate Regression Models Predicting Depressive Symptoms and Suicidal ideation With Control Strategies
| Predictor | Depressive Symptoms | Suicidal Ideation | ||
|---|---|---|---|---|
|
| ||||
| R2 | B (SE) | R2 | B (SE) | |
| Step 1 | .002 | .36 | ||
| Age | .01 (.23) | .05 (.07) | ||
| Sex | −.99 (3.53) | .54 (.89) | ||
| ADL | .02 (.23) | −.05 (.06) | ||
| CESDR | .19*** (.04) | |||
| Step 2 | .51a | .57b | ||
| SPC | −.72 (.48) | −.36* (.15) | ||
| CPC Help | −1.31** (.47) | −.26 (.14) | ||
| CPC Modify | .15 (.70) | −.17 (.19) | ||
| SSC | .63 (.44) | .38** (.13) | ||
| CSC Compare | 1.32* (.57) | −.13 (.18) | ||
| CSC Disengage | −.66 (.77) | .29 (.23) | ||
| CSC Self-Protect | 1.63 (.88) | −.14 (.26) | ||
Note. ADL = Activities of Daily Living; CESDR = Center for Epidemiologic Studies Depression Scale Revised; SPC = Selective Primary Control; CPC = Compensatory Primary Control; SSC = Selective Secondary Control; CSC = Compensatory Selective Control; Compare = Social and Intra-Individual Comparisons; Disengage = Goal Disengagement; Self-Protect = Self-Protective Attributions.
F[10, 32] = 3.29, p < .01.
F[11, 27] = 4.71, p < .001.
p < .05,
p < .01,
p < .001.
The second hypothesis, that secondary control strategies would be associated with lower levels of depressive symptoms and suicidal ideation, was not supported. SSC and the CSC Compare factor were related to greater depressive symptoms in the multivariate model (Table 4, first column), indicating that those participants who focused, to a greater extent, on enhancing their motivation to accomplish their goals or on social comparisons reported greater depressive symptoms after controlling for age, sex, ADLs, and all other control strategies. Furthermore, SSC was associated with greater suicidal ideation and none of the CSC factors was significantly related to suicidal ideation (Table 4, second column).
To clarify our results, we conducted additional analyses testing for interactions between SPC and CPC-Help in predicting depressive symptoms and suicidal ideation, controlling for the same covariates as in the multivariate models above. Prior to testing the interaction term, variables were mean-centered. The interaction of SPC and CPC-Help was not significant in the model predicting depressive symptoms, but was significant in the model predicting suicidal ideation, F(1,38) = 6.87, p = .01, ΔR2 = .07. The main effect for CPC Help remained significant after the interaction term was introduced into the model, F(1,38) = 5.08, p = .03, but the main effect for SPC did not, F(1,38) = 2.44, p = .13. Figure 1 displays the interaction between SPC and CPC Help variables at values one standard deviation above and below the mean. As the figure illustrates, high endorsement of selective primary control strategies is associated with lower levels of suicidal ideation only in the context of low endorsement of the compensatory primary control strategy of getting help from others.
Figure 1.
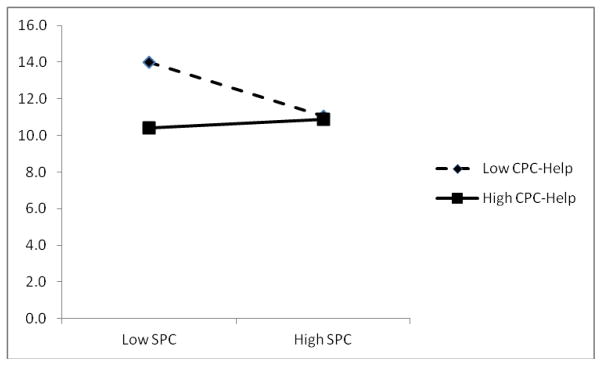
Interaction between Selective Primary Control (SPC) and Help-seeking (CPC-Help) strategies predicts scores on the suicidal ideation subscale of the Geriatric Suicide Ideation Scale (GSIS-SI).
Discussion
The present study is the first, to our knowledge, to demonstrate a relation between control strategy endorsement and suicidal ideation. The central finding is that among older adults with health-related limitations, strategies for attaining goals either through persistent striving (selective primary control) or by seeking help or advice from others (that is, compensatory primary control) were associated with lower levels of suicidal ideation independent of depressive symptoms. Additional analyses suggested that seeking help from others was directly related to lower suicidal ideation, whereas the relation between persistence and suicidal ideation was dependent upon the level of help-seeking. These results are consistent with the Motivational Theory of Life-Span Development [10], which proposes that striving for control is universal and adaptive throughout the lifespan, but that the most positive outcomes derive from an optimal match between opportunities for control and types of control strategies employed. The results of the present study are also in line with previous research that has linked control strategy endorsement to lower levels of depressive symptoms among older adults with health problems [13, 14]. The present study extends this work by showing that control strategies are also associated with suicidal ideation. In addition, our results add to the literature that suggests the importance of compensation in the process of adapting to age-related challenges [15, 19–21]. Our results support our conceptualization that suicidal thinking may arise among older adults who are no longer able to attain goals directly due to health limitations but are unable or unwilling to make use of external sources of support.
Seeking help is an inherently social activity. Thus, the finding that compensatory primary control is associated with reduced levels of suicide risk is consistent with the well-established relation between social connectedness and suicidal behaviors among older adults [reviewed by 3]. Older adults who live alone or do not have a confidante are at greater risk of suicide [3]. On the other hand, older adults who perceive themselves to be a burden on others in their social network are also at elevated risk for suicidal ideation [31]. Future research on suicide risk in late life should examine the use of compensatory primary control strategies in the context of social factors.
An unanticipated finding of the present study was that selective secondary control strategies—that is, efforts to adjust one’s own thinking to enhance motivation to attain a goal—were associated with higher levels of suicidal ideation after accounting for the effects of covariates, including depressive symptoms and other types of control strategies. It should be remembered when interpreting these findings that the study design was cross-sectional and, as such, could not determine direction of effect. It is possible that individuals who were suicidal engaged in more intense efforts to change their thinking. It is also possible that individuals who engaged in more secondary control strategies may have comprised a group with greater severity of functional impairment that was not detected (and controlled) by our measure of functioning. Additional research will be needed to further clarify this surprising finding.
It is also surprising that goal disengagement was not associated with lower levels of depressive symptoms or suicidal ideation. It is possible that the lack of a significant effect was due to lack of power. In addition, although disengagement from unattainable goals has generally been associated with positive mental health outcomes [e.g., 15, 16, 17], there are also conditions under which it can be harmful to give up on one’s aspirations, such as when a person does not reengage with a new goal [32]. Furthermore, it is possible that most participants in the present sample have not yet reached a stage of disablement that would render goal disengagement an adaptive strategy [12]. Future studies in more severely impaired samples would be helpful.
Results of this study should be considered in light of several limitations. The cross-sectional study design limited our ability to disentangle cause and effect, as noted above. Although we have conceptualized affective states as outcomes of control strategies, it is also possible that choice of control strategy is influenced by affective state. Prospective research will be needed to establish temporal precedence. Nonetheless, the current results are valuable in that they appear to be the first to establish a relation between control strategies and suicidal ideation.
It should also be noted that the sample was relatively small. Given this fact, it is notable that our first hypothesis was nonetheless supported. Lack of a significant relation between goal disengagement and suicidal ideation, however, should be considered in light of limited power.
The level of suicidal ideation in the current sample (GSIS-SI mean = 12.0, SD = 3.1) was relatively low in comparison with the mean of 19 reported in a psychiatric sample [27]. Seven percent of the participants in the present study scored at or above the psychiatric mean. Results of the present study may be understated due to this restricted range.
The relatively low rate of suicidal ideation in the current study reflects the use of an outpatient medical sample rather than a psychiatric clinical sample. Participants in the current study appear to differ from clinical samples of suicidal older adults on several key demographic variables, including greater likelihood of being married compared to older adult samples of suicide attempters [e.g., 33], In addition, the present sample reported a high level of educational attainment compared to national samples [22], and lower education has been associated with suicide in late life [5]. In one important dimension, however, the current sample was similar to samples of older adults at risk of suicidal behavior. Participants in the present study reported relatively high rates of physical illnesses and all participants were included only if they endorsed some form of functional impairment. Furthermore, it can be argued that it is critically important to study late life suicidal behavior in a primary care setting. Older adults are more likely to seek help in general medical settings than in specialized mental health care settings [34]. Moreover, most older adults who die by suicide visit a primary care provider within the month prior to the death [35].
Finally, although the sample included a wide range of ages within older adulthood, there was little ethnic diversity in the sample, consistent with the population in the surrounding region. This limitation should be considered when generalizing the results.
Several directions for future research are suggested by the results of the present study. Research evaluating possible moderators of the relation between control strategy use and suicidal outcomes would be valuable. Because control strategy use may be particularly relevant for older men [e.g., 19], who are also at elevated risk of suicide [1], future studies should evaluate whether gender modifies the relation between control strategy use and suicidality. In addition, research in a sample of older adults with a particular type of functional limitation would provide the opportunity to investigate relations between control strategies and affective outcomes with greater specificity. Prospective research would be important in order to determine temporal precedence of control strategies and depressive or suicidal symptoms. Finally, research involving interventions to alter specific types of control strategies, e.g., problem-solving therapy aimed at increasing the use of external resources, would provide the opportunity for a direct test of the effects of control strategy use on outcomes.
There are also several clinical implications of the present study. Previous research has shown that screening for depression in primary care settings increases detection rates and treatment [36]. The current study’s finding suggest that health care providers should be especially alert to the possibility of suicidal thinking in patients who are not actively striving to meet goals. Health care providers working with older adults with functional limitations are encouraged to ask whether the patient continues to engage in daily activities and assist the patient in identifying activities the patient is still capable of doing, or replacement activities in place of lost activities, in order to maintain continued striving and sense of control. Brief problem-solving exercises, such as those derived from Problem-Solving Therapy (PST; [37]), may also enhance control striving by helping the older adult to solve problems associated with their functional limitations. PST may also reduce suicide risk by reducing proximal risk factors, such as hopelessness and depressive symptoms [36].
Findings that compensatory primary control strategies are associated with lower levels of suicidal ideation in older adults with health limitations imply that the ability to utilize external resources, especially asking others for help, may be protective against suicidal thinking. Health care providers can briefly assess the availability of individuals in the patient’s life whom they can ask for help, as well as the patient’s degree of comfort asking others for help. Patients with a sparse social network or those who are reluctant to ask for help should be monitored closely for suicidal ideation. Moreover, referral to a mental health specialist may be warranted for patients who present with depressive symptoms and either lack social support or are unwilling to ask for help, as they are at greatest risk of developing suicidal thinking. Research suggests that compared to treatment-as-usual, close monitoring of depressive symptoms and suicide ideation by a depression care manager, along with either antidepressant or psychosocial intervention, reduced suicide ideation over two years among older adult primary care patients with major depressive disorder [38].
Importantly, because the results of the present study demonstrate that control strategies are associated with suicidal ideation independent of depressive symptoms, assessment for suicidality would be warranted in these circumstances whether or not depressive symptoms are endorsed.
In conclusion, the current study found that among older adults with health-related limitations, greater use of compensatory primary control strategies characterized by help-seeking, and greater persistence among those who do not engage in help-seeking, was associated with lower levels of suicidal thinking, independent of depressive symptoms.
Acknowledgments
This work was supported by the National Institute of Mental Health at the National Institutes of Health (grant number R15 MH080399) to AF.
The authors wish to thank Kathrin Boerner, Marnin J. Heisel, Richard Schulz for reviewing an early draft of this manuscript and providing helpful suggestions.
Contributor Information
Amy Fiske, Department of Psychology and Injury Control Research Center, West Virginia University
Patricia M. Bamonti, Department of Psychology, West Virginia University
Michael R. Nadorff, Department of Psychology, West Virginia University.
Rachel A. Petts, Department of Psychology, West Virginia University.
Jeannie A. Sperry, West Virginia University Department of Family Medicine
References
- 1.McIntosh JL, Drapeau CW for the American Association of Suicidology. USA suicide: 2010 official final data. Washington, DC: American Association of Suicidology; Sep 20, 2012. downloaded October 6, 2012, from http://www.suicidology.org. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) 2013 Retrieved June 12, 2013, from http://www.cdc.gov/injury/wisqars/index.html.
- 3.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatric Clinics of North America. 2011;34:451–468. doi: 10.1016/j.psc.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fiske A, O’Riley AA, Widoe RK. Physical health and suicide in late life. Clinical Gerontologist. 2008;31:31–50. doi: 10.1080/07317110801947151. [DOI] [Google Scholar]
- 5.Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, et al. Completed suicide among older patients in primary care practice: A controlled study. Journal of the American Geriatrics Society. 2000;48:23–29. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan MS, McFarland BH, Huguet N, Newsom JT. Physical illness, functional limitations, and suicide risk: A population-based study. American Journal of Orthopsychiatry. 2007;77:56–60. doi: 10.1037/0002-9432.77.1.56. [DOI] [PubMed] [Google Scholar]
- 7.Préville M, Hébert R, Boyer R, Bravo G, Séquin M. Physical health and mental disorder in elderly suicide: A case-control study. Aging and Mental Health. 2005;9:576–584. doi: 10.1080/13607860500192973. [DOI] [PubMed] [Google Scholar]
- 8.Llorente MD, Burke M, Gregory GR, Bosworth HB, Grambow SC, Horner RD, et al. Prostate cancer: A significant risk factor for late-life suicide. American Journal of Geriatric Psychiatry. 2005;13:195–201. doi: 10.1176/appi.ajgp.13.3.195. [DOI] [PubMed] [Google Scholar]
- 9.Kjølseth I, Ekeberg O, Stihaug S. “Why do they become vulnerable when faced with the challenges of old age?” Elderly people who committed suicide, described by those who knew them. International Psychogeriatrics. 2009;21:903–912. doi: 10.1017/S1041610209990342. [DOI] [PubMed] [Google Scholar]
- 10.Heckhausen J, Wrosch C, Schulz R. A motivational theory of life-span development. Psychological Review. 2010;117:32–60. doi: 10.1037/a0017668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heckhausen J. Developmental regulation across adulthood: Primary and secondary control of age-related challenges. Developmental Psychology. 1997;33:176–187. doi: 10.1037//0012-1649.33.1.176. [DOI] [PubMed] [Google Scholar]
- 12.Wahl H-W, Schilling O, Becker S. Age-related macular degeneration and change in psychological control: Role of time since diagnosis and functional ability. Journals of Gerontology: Psychological Sciences. 2007;62B:90–97. doi: 10.1093/geronb/62.2.p90. [DOI] [PubMed] [Google Scholar]
- 13.Wrosch C, Schulz R, Heckhausen J. Health stresses and depressive symptomatology in the elderly: The importance of health engagement control strategies. Health Psychology. 2002;21:340–348. doi: 10.1037//0278-6133.21.4.340. [DOI] [PubMed] [Google Scholar]
- 14.Wrosch C, Schulz R, Miller GE, Lupien S, Dunne E. Physical health problems, depressive mood, and cortisol secretion in old age: Buffer effects of health engagement control strategies. Health Psychology. 2007;26:341–349. doi: 10.1037/0278-6133.26.3.341. [DOI] [PubMed] [Google Scholar]
- 15.Dunne E, Wrosch C, Miller GE. Goal disengagement, functional disability, and depressive symptoms in old age. Health Psychology. 2011;30:763–770. doi: 10.1037/a0024019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wrosch C, Heckhausen J, Lachman ME. Primary and secondary control strategies for managing health and financial stress across adulthood. Psychology and Aging. 2000;15:387–399. doi: 10.1037//0882-7974.15.3.387. [DOI] [PubMed] [Google Scholar]
- 17.Wallace ML, Dombrovski AY, Morse JQ, Houck PR, Frank E, Alexopoulos GS, et al. Coping with health stresses and remission from late-life depression in primary care: A two-year prospective study. International Journal of Geriatric Psychiatry. 2012;27:178–186. doi: 10.1002/gps.2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark DC. Narcissistic crises of aging and suicidal despair. Suicide and Life-Threatening Behavior. 1993;23:21–26. [PubMed] [Google Scholar]
- 19.Chipperfield JG, Perry RP. Primary- and secondary-control strategies in later life: Predicting hospital outcomes in men and women. Health Psychology. 2006;25:226–236. doi: 10.1037/0278-6133.25.2.226. [DOI] [PubMed] [Google Scholar]
- 20.Boerner K, Brennan M, Horowitz A, Reinhardt JP. Tackling vision-related disability in old age: An application of the life-span theory of control to narrative data. Journal of Gerontology: Psychological Sciences. 2010;65B:22–31. doi: 10.1093/geronb/gbp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boerner K, Wang S. Goals with limited vision: A qualitative study of coping with vision-related goal interference in midlife. Clinical Rehabilitation. 2012;26:81–93. doi: 10.1177/0269215511407219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Older Americans 2010: Key Indicators of Well-Being. Washington, DC: U.S. Government Printing Office; Jul, 2010. Federal Interagency Forum on Aging-Related Statistics. [Google Scholar]
- 23.Heckhausen J, Schulz R, Wrosch C. Developmental regulation in adulthood: Optimization in primary and secondary control—A multiscale questionnaire (OPS-Scales) Berlin, Germany: Max Planck Institute for Human Development; 1998. [Google Scholar]
- 24.Eaton WW, Muntaner C, Smith C, Tien A, Ybarra M . Center for Epidemiologic Studies Depression Scale. Review and revision (CESD and CESDR) In: Maruish ME, editor. The use of psychological testing for treatment planning and outcome assessments: Volume 3: Instruments for adults. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 363–377. [Google Scholar]
- 25.Radloff LS. A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 26.Friedlander A, Nazem S, Fiske A, Nadorff MR, Smith MD. Self-Concealment and Suicidal Behaviors. Suicide and Life-Threatening Behavior. 2012;42:332–340. doi: 10.1111/j.1943-278X.2012.00094.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heisel MJ, Flett GL. The development and initial validation of the Geriatric Suicide Ideation Scale. American Journal of Geriatric Psychiatry. 2006;14:742–751. doi: 10.1097/01.JGP.0000218699.27899.f9. [DOI] [PubMed] [Google Scholar]
- 28.Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. The Journal of the American Medical Association. 1963;185:94–99. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 29.Lawton M, Brody E. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 30.Spector WD, Fleishman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology: Psychological Sciences and Social Sciences. 1998;53B:S46–S57. doi: 10.1093/geronb/53b.1.s46. [DOI] [PubMed] [Google Scholar]
- 31.Cukrowicz KC, Cheavens JS, Van Orden KA, Ragain RM, Cook RL. Perceived burdensomeness and suicidal ideation in older adults. Psychology and Aging. 2011;26:331–338. doi: 10.1037/a0021836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Connor RC, Fraser L, Whyte MC, MacHale S, Masterton G. Self-regulation of unattainable goals in suicide attempters: The relationship between goal disengagement, goal reengagement and suicidal ideation. Behavior Research & Therapy. 2009;47:164–169. doi: 10.1016/j.brat.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Szanto K, Dombrovski AY, Sahakian BJ, Mulsant BH, Houck PR, Reynolds CF, III, et al. Social emotion recognition, social functioning, and attempted suicide in late-life depression. American Journal of Geriatric Psychiatry. 2012;20:257–265. doi: 10.1097/JGP.0b013e31820eea0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harman JS, Veazie PJ, Lyness JM. Primary Care Physician Office Visits for Depression by Older Americans. Journal of General Internal Medicine. 2006;21:926–930. doi: 10.1007/bf02743139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: A review of the evidence. American Journal of Psychiatry. 2002;159:909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 37.D’Zurilla TJ, Nezu AM. Problem-Solving Therapy. In: Dobson KS, editor. Handbook of cognitive-behavioral therapies. New York, NY: The Guilford Press; 2010. pp. 197–225. [Google Scholar]
- 38.Alexopoulos GS, Reynolds CF, Bruce ML, Katz IR, Raue PJ, Mulsant BH, et al. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. The American Journal of Psychiatry. 2009;166:882. doi: 10.1176/appi.ajp.2009.08121779. [DOI] [PMC free article] [PubMed] [Google Scholar]


