Abstract
Tendon surgery is unique because it should ensure tendon gliding after surgery. Tendon surgery now can be performed under local anesthesia without tourniquet, by injecting epinephrine mixed with lidocaine, to achieve vasoconstriction in the area of surgery. This method allows the tendon to move actively during surgery to test tendon function intraoperatively and to ensure the tendon is properly repaired before leaving the operating table. I applied this method to primary flexor tendon repair in zone 1 or 2, tenolysis, and tendon transfer, and found this approach makes tendon surgery easier and more reliable. This article describes the method that I have used for tendon surgery.
Keywords: Tendon, Surgical repair, Anesthesia, Rehabilitation
It has been a standard practice to obtain local or general anesthesia and apply a tourniquet to perform tendon surgery. However, this practice has been changed in recent years. Tendon surgery is unique because it should ensure tendon gliding after surgery. Tendon surgery now can be performed under local anesthesia without tourniquet, by injecting epinephrine mixed with lidocaine, to achieve vasoconstriction in the area of surgery.1,2,3,4,5,6) Therefore, such wide-awake no tourniquet surgery, which allows tendon to actively move during surgery, has huge benefits for helping surgeons to test tendon function during the process of surgery and to ensure the tendon is properly repaired before leaving the operating table.
I have used this approach in patients who prefer tendon surgery when he or she is awake after I started to adopt it about two years ago. About half of the patients actually prefer to use this method, cost of treatment comes down (because of no anesthesia cost in this kind of surgery), and some of the surgery can be done in a simpler operating setting, such as in a minor procedure room. I typically applied this method to primary flexor tendon repair in zone 1 or 2, tenolysis, and tendon transfer.
PRIMARY FLEXOR TENDON REPAIR IN ZONE 1 OR 2
Anesthetic Solution
The local anesthetic (1% lidocaine with epinephrine, 1:100,000 for tendon surgery in 1 or 2 digits or in the palm) is injected to the digits of the patient in the waiting area starting 30 minutes before surgery for anesthesia. Injection of such mixture to the hand was found to be safe.1,2,3,4,5,6) Waiting after injection allows the epinephrine to take effect and provide an adequately dry working field. The patient should be lying down for the injection. Injection can be done in a surgical preparation room or a waiting room.
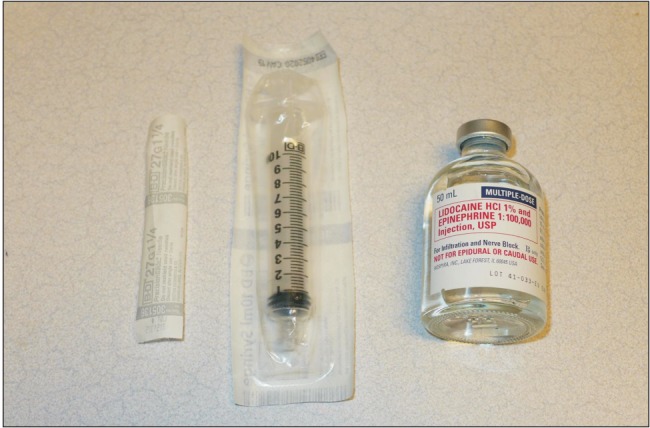
Lidocaine with epinephrine buffered with 10:1 8.4% bicarbonate is used for all injections. All the local anesthetic solution is warmed to body temperature. If premixed anesthetics are available, this can be injected directly (Fig. 1).
Fig. 1. The pre-mixed anesthetic solution used for injection and the injection needle (25 or 27 gauge).
We keep the total dose of infiltration less than 7 mg/kg. Usually, less than 50 mL is required for tendon surgery in the hand (including digits and palm areas), and we use premixed 1% lidocaine with 1:100,000 epinephrine. Occasionally, 50 to 100 mL is required when surgery is involved in 3 or 4 digits or in the forearm; in these cases, we dilute with saline to a concentration of 0.5% lidocaine with 1:200,000 epinephrine.
Methods of Injection
The injection starts proximally with a fine needle (25 or 27 gauge) (Fig. 1). Between 10 mL and 15 mL infiltration is injected in the most proximal part of the likely dissection area to block the nerves distally. This site is located in the distal part of the palm for a zone 2 tendon repair. In this way, the large volume of the first injection will bathe all of the nerves leading to the area of the next injections. For a zone 1 tendon repair, we usually inject the solution similarly as for a zone 2 tendon repair.
In making the first injection, we insert the needle perpendicular to the skin into the subcutaneous fat to reduce pain of injection.6) Then the syringe is stabilized with fingers propped on the skin to avoid needle wobble. We inject the first 0.5 mL slowly (5 seconds) and then pause. Wait 15 to 45 seconds until the patient tells us that the sting is gone. Then, we proceed to inject the rest of infiltration very slowly (more than 5 minutes) without moving the needle (Fig. 2A). Sometimes, I make this first injection in a quicker fashion than I described above and inject continuously in the way that we all use for local anesthesia, if the patient tolerates well.
Fig. 2. Wide-awake local anesthesia for a case with a complete zone 2 flexor tendon cut in the middle finger. (A) The first injection (10-15 mL) was performed in the most proximal part of the likely dissection to block the nerves distally. (B) Fifteen minutes after the first injection, the second injection (2 mL) was performed subcutaneously at the palmar digital crease between both digital nerves. (C) The third injection (2 mL) was performed immediately after the second injection under the skin at the digital crease of the proximal interphalangeal joint between both digital nerves. (D) The final injection (1 mL) was performed immediately after the third injection under the skin at the digital crease of the distal interphalangeal joint between both digital nerves.
About 10 to 15 minutes after the first injection, the whole distal area of dissection is almost or totally numb. The next injections will be pain free. The next three injections are used mainly for the epinephrine vasoconstriction effect. Between both digital nerves, 2 mL of infiltration is injected subcutaneously at the palmar digital crease, so the bevel of the needle does not lacerate the nerve fascicles (Fig. 2B). Another 2 mL of infiltration is also injected subcutaneously at the digital crease of the proximal interphalangeal (PIP) joint between both digital nerves (Fig. 2C). The final 1 mL of infiltration is then injected subcutaneously at the digital crease of the distal interphalangeal (DIP) joint between both digital nerves (Fig. 2D). We then wait 15 minutes to proceed to field sterilization and the surgery.
Surgical Procedures
The surgery starts 30 minutes after the first injection or 15 minutes after completion of all injections. The patient is prepared and draped in the operating room. A Bruner incision of about 2 cm is used to expose the tendon sheath. The flexor sheath is exposed. The sheath is opened through a small incision along the midline, about 1 to 1.5 cm usually. The sheath opening should be limited within 1.5 to 2 cm.
Retraction of the tendon ends, especially the proximal tendon end, is very common. Flexion of the distal finger joints helps bring the distal end into the operating field. If the tendon is cut in zone 2, flexion of the metacarpophalangeal (MP) joint sometimes helps the proximal stump advance to the sheath opening area, but very often a separate incision at the distal palm is needed to find the proximal stump and it is advanced distally through the preserved sheath to approximate the distal tendon. If the tendon is cut in zone 1, flexion of the PIP joint usually brings the proximal end back to the operative field.
During the surgery, some mild bleeding may be seen when the skin incision is made, but after wiping the sites with gauzes, the bleeding usually stops. We no longer use cautery but occasionally use a hemostat on bigger vessels for a few minutes to achieve hemostasis.
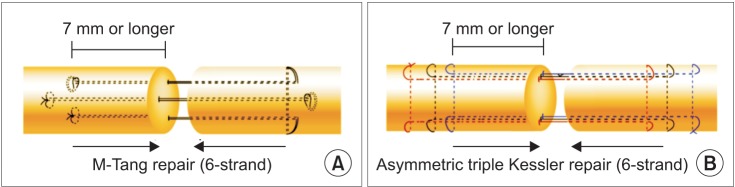
The flexor digitorum profundus (FDP) tendon is repaired with a 6-strand core suture repair (4-0 suture, M-Tang method using looped suture (Fig. 3),7) such as Supramid (S Jackson, Inc., Alexandria, VA, USA), or a triple Kessler method with asymmetric core suture purchases at two tendon stumps8)) plus a simple running peripheral suture (6-0 suture) (Fig. 4). Core suture purchases should be at least 7 mm, ideally around 10 cm (Fig. 5). This is a very important requirement for the core suture.9,10) The core suture is performed with some extent of tension to make the two tendon ends approximate tightly to increase gapping resistance, but not too tight to avoid marked tendon bulkiness. It is important to make the repair a bit tensed, rather than being loose or tension-free. My method is to tension the core suture lines to the degree that makes the tendon segments within the core sutures shortened slightly, by approximately 10% (Fig. 5).11,12) The lacerated flexor digitorum superficialis (FDS) tendon is repaired when the wound is clean and the repair is easy and the cut is not in the area of zone under the A2 pulley. In many cases, I do not repair the FDS tendon, especially when at delayed primary repair, and when in the A2 pulley area, or when FDS tendon retracted proximally. I have not found that has affected finger function.
Fig. 3. Thirty minutes after the local anesthesia injection, the epinephrine takes effect. The skin of the operative field has turned pale. The wound was exposed through a Bruner incision, and the distal half of the A2 pulley was incised through the volar midline. The proximal end of ruptured tendon was found in a small incision in the distal palm and advanced under the preserved A1 and the proximal part of the A2 pulleys. This flexor digitorum profundus tendon shown was repaired with a 6-strand M-Tang technique.

Fig. 4. Either a M-shaped 6-strand repair with 4-0 looped suture (A) or a 6-strand asymmetric Kessler repair using 4-0 suture (B) is used. A simple running peripheral suture is added later.
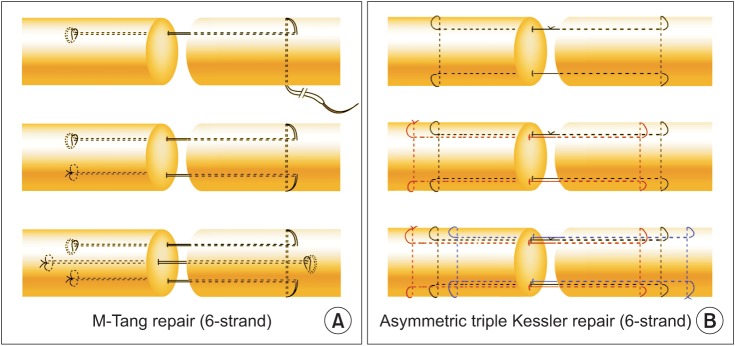
Fig. 5. Sufficient core suture purchase (> 7 mm) and slight tension over the repaired segment are two important elements in surgical repair, making the sutured tendon segment slightly tensioned by creating about 10% shortening in the sutured segment. (A, B) The length of core suture purchase and the direction of slight tension (arrows) in the two repair methods.
Repair of damaged synovial sheath is usually not necessary and whether the sheath is closed does not affect outcomes. However, it is necessary to take care to preserve most or most parts of the annular pulleys if possible. When other annular pulleys are intact, we can vent the A4 pulley entirely if the tendon ends can pass under this narrow pulley or the pulley restricts tendon gliding (which is often the case).7) If the injury site is at or around the A2 pulley, a part (1/2 to 2/3) of the A2 pulley can be vented.6) My method of venting is a direct cut along the volar midline using scissors. Pulley venting may be done together with cutting of a part of adjacent synovial sheath. The total length of sheath-pulley release in the site of repair surgery is 1.5 cm or 2 cm depending on the finger length.6) Our studies show that this length of release allows ample tendon gliding but will not cause tendon bowstringing when other sheath parts are intact. I have performed such venting for over 10 years and have not seen functional damage to the finger after properly doing the venting.
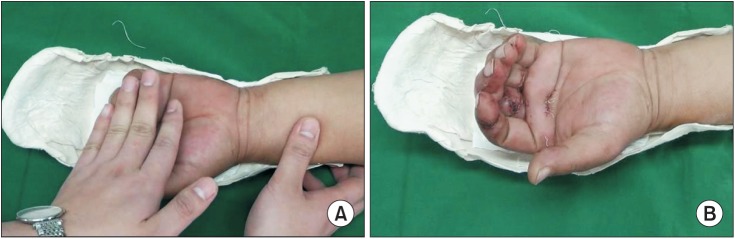
Extension-Flexion Test
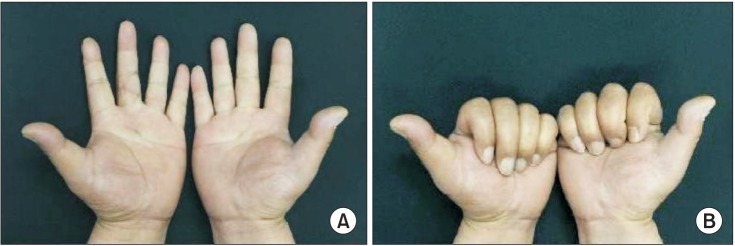
This is a test that should be done immediately after the repair. We ask the patient to actively extend and flex the surgically repaired digits. This test verifies that the repair is strong and is able to tolerate early active digital motion during rehabilitation.13,14) This test is called "digital extension-flexion test."14)
There are thee needed parts of this test: (1) full active extension to verify no gapping between the tendon ends (Fig. 6); (2) smooth active flexion to verify smooth gliding of the tendon and its repair site; and (3) active flexion to almost totally flex the digit to verify that the no pulley prevents tendon gliding. If the examination creates a visible gap between the two tendon ends during finger extension, the suture is usually not tight enough and needs to be replaced with a tighter suture with proper tension to avoid rupture. Active flexion indicates the annular pulley prevents ample gliding of the tendon. Pulleys may need to be vented further.
Fig. 6. After flexor digitorum profundus tendon repair, the patient actively extended and flexed the finger to perform the extension-flexion test. The photo shows active extension of the repaired digit without gapping at the repair site.

Here, I strongly stress that the repeated total active movement examination may be needed to verify that the repair is strong and pulley release is sufficient. The allowable length of the pulley release for the A2 is 2/3, and the entire A4 pulley can be vented with a part of the synovial sheath when all other annular pulleys are well preserved. Usually this venting allows ample tendon gliding but will not cause tendon bowstringing when other sheath parts are intact.
Repair of flexor tendon in proximal zone 1 can use similar approaches because only FDP tendon is repaired. To find or pass the retracted proximal end, the A4 pulley may need entire venting if the repair is very close to that pulley. A separate incision in the proximal part of the digit or distal palm may be necessary to find the retracted FDP tendon and A4 may need total venting to pass the proximal stump distally. The repair method is the same as in zone 2 repair.
Postoperative Care
The patient is protected with a very short forearm based splint, from about 6-8 cm above the wrist to the tip of the finger, with the wrist at 20° to 30° flexion, MP joint at slight flexion, and the interphalangeal joints in extension. 15) I sometimes put the patient's wrist in neutral position.7,15) I think, with a strong repair method and validation of good repair using the intraoperative extension-flexion test, we have a greater room to place the wrist at a position between a wrist neutral position and slight flexion, and may even slight extension.
The early active motion that I use is a combined passive-active motion, starting from 3 to 5 days after the surgery.15) I do not move the operated digits in the first 3 days after surgery because edema is prominent, pain is severe, and adhesions do not form in this period. Motion starts from day 4 or 5. In the initial 1 to 2 weeks after surgery, we keep the active finger flexion within only one-third of the total range of finger motion (Fig. 7). The partial range of active motion is progressively increased to two-thirds in week 3 or 4 after surgery. The patient should avoid full range of active flexion in the first 2 to 3 weeks after surgery because the final extreme digital flexion produces the greatest bending force to the tendon and tendon is prone to disruption. Full range of active motion starts at week 4. I sometimes start full active motion even a little later in the patient who had tendon repairs in multiple fingers, or when the tendon is repaired 3 to 5 weeks after trauma or after repair of ruptured primary repair.
Fig. 7. Postoperative motion: full passive digital flexion (A) is done first, followed by partial active motion (B) in the first 3 weeks.
In performing these motion exercises, the full range of passive digital motion (10 to 30 repetitions) is carried out before the initiation of active digital movement in each session. The number of exercise sessions can range from 5 to 6 times per day and hourly in daytime, depending on the need of motion to prevent or correct digital joint stiffness and patient's desire or availability for the exercise. Four to 5 sessions are minimal each day and 10 to 30 repetitions of passive motion and 20 to 30 repetitions of active motion are minimal for each session in our practice. I do not order patients to move hourly, but some patients prefer to do exercise whenever he or she has free time. I encourage full active extension of the interphalangeal joints in all the postsurgical weeks and encourage differential PIP and DIP joint motions.
The exercise should persist for about 10 to 12 weeks after surgery. Many patients need further extension exercises because of some extension or flexion lags, which can be corrected in subsequent exercises. We inform the patient that improvement is possible even months after repair (Fig. 8), and persistent exercises of up to 5 or 6 month may still show improvement of function.
Fig. 8. Follow-up at six months after surgery. (A) Full range of active extension of the left middle finger was achieved without extension deficits of the finger joints. (B) Full range of active flexion.
TENOLYSIS
Tenolysis in the hand and forearm can be done with similar anesthesia without tourniquet. Therefore, the patient can actively move the digits or the hand to ensure that tenolysis is adequate and the tendon is strong enough to move the tendon. The method of anesthesia is the same as we described earlier for primary repair, and surgical incisions for tenolysis are the same with those used traditionally. The only difference is that the surgeons can ask the patient to actively flex or extend the digit or the hand to see active gliding of the tendon. If the tenolysis is sufficient, the surgery is complete. If the tenolysis is insufficient, as indicated by insufficient digit or hand motion, further release of scar around the tendon is necessary. Tendons sometimes are found frayed during surgery. Such active motions help the surgeon to test the strength of these tendons. If the tendon is remarkably elongated or is broken when the digits or the hand actively moved, tendon reconstruction using a tendon grafting should be considered. During active motion, strength of the pulley can be tested as well and whether the pulleys restrict tendon gliding can be assessed. If the pulleys are broken during active tendon motion, important annular pulleys may need reconstruction. Restriction of the tendon gliding from the pulleys may need further release of adhesions or a pulley plasty or pulley shortening procedure.
TENDON TRANSFER
Tendon transfer is actually best indicated for such wide-awake surgery, because adjusting tension of the transfer has always been difficult. With the patient being awake, the digits or the hand can move actively to determine correct tension of the transfer. The patient should be asked to perform the desired action after transferring the tendon before the surgeon places the suture to fix the transferred tendon to the damaged tendon. This practice has been a routine for some hand surgeons now, and has been used in most commonly performed tendon transfers such as extensor indicis proprius transfer to the extensor pollicis longus, flexor carpi radialis transfer to the extensor digitorum communis. The anesthesia method is the same as described for the flexor tendon repair in the palm. If a lengthy incision or dissection over an extensive area is necessary in the forearm, 0.5% lidocaine with 1:200,000 epinephrine is used to decrease the total amount of injected epinephrine. Strength and gliding of the tendon suture site (usually Pulvertaft weave suture) are also possible with the patient actively moving the digits or the hand.
Besides tendon surgery, similar wide-awake surgery has been used in carpal tunnel release, cubital tunnel release, wrist arthroscopy, and some benign tumor resection.16,17,18,19) These uses have greatly reduced the cost of the surgery and diminished the use of supplies during surgery.16,17,18,19) Many patients now can be operated in a minor procedure room. In our department, we established a wide-awake surgical room right in the ward. Many patients do not need to go to the main operating theatre to have surgery. Such a wide-wake surgical room reduces surgical waiting time and save the time of patient transfer and recovery, representing a huge increase in efficiency of surgical treatment as compared to previous surgical settings.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Thomson CJ, Lalonde DH, Denkler KA, Feicht AJ. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg. 2007;119(1):260–266. doi: 10.1097/01.prs.0000237039.71227.11. [DOI] [PubMed] [Google Scholar]
- 2.Nodwell T, Lalonde D. How long does it take phentolamine to reverse adrenaline-induced vasoconstriction in the finger and hand? A prospective, randomized, blinded study: the Dalhousie project experimental phase. Can J Plast Surg. 2003;11(4):187–190. doi: 10.1177/229255030301100408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, Chang P. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical phase. J Hand Surg Am. 2005;30(5):1061–1067. doi: 10.1016/j.jhsa.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Fitzcharles-Bowe C, Denkler K, Lalonde D. Finger injection with high-dose (1:1,000) epinephrine: does it cause finger necrosis and should it be treated? Hand (N Y) 2007;2(1):5–11. doi: 10.1007/s11552-006-9012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mustoe TA, Buck DW, 2nd, Lalonde DH. The safe management of anesthesia, sedation, and pain in plastic surgery. Plast Reconstr Surg. 2010;126(4):165e–176e. doi: 10.1097/PRS.0b013e3181ebe5e9. [DOI] [PubMed] [Google Scholar]
- 6.Lalonde DH. "Hole-in-one" local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg. 2010;126(5):1642–1644. doi: 10.1097/PRS.0b013e3181f1c0ef. [DOI] [PubMed] [Google Scholar]
- 7.Tang JB. Clinical outcomes associated with flexor tendon repair. Hand Clin. 2005;21(2):199–210. doi: 10.1016/j.hcl.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Tang JB. Release of the A4 pulley to facilitate zone II flexor tendon repair. J Hand Surg Am. 2014;39(11):2300–2307. doi: 10.1016/j.jhsa.2014.08.025. [DOI] [PubMed] [Google Scholar]
- 9.Tang JB, Zhang Y, Cao Y, Xie RG. Core suture purchase affects strength of tendon repairs. J Hand Surg Am. 2005;30(6):1262–1266. doi: 10.1016/j.jhsa.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Cao Y, Zhu B, Xie RG, Tang JB. Influence of core suture purchase length on strength of four-strand tendon repairs. J Hand Surg Am. 2006;31(1):107–112. doi: 10.1016/j.jhsa.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Wu YF, Tang JB. Effects of tension across the tendon repair site on tendon gap and ultimate strength. J Hand Surg Am. 2012;37(5):906–912. doi: 10.1016/j.jhsa.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Wu YF, Tang JB. Recent developments in flexor tendon repair techniques and factors influencing strength of the tendon repair. J Hand Surg Eur Vol. 2014;39(1):6–19. doi: 10.1177/1753193413492914. [DOI] [PubMed] [Google Scholar]
- 13.Higgins A, Lalonde DH, Bell M, McKee D, Lalonde JF. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg. 2010;126(3):941–945. doi: 10.1097/PRS.0b013e3181e60489. [DOI] [PubMed] [Google Scholar]
- 14.Tang JB. Outcomes and evaluation of flexor tendon repair. Hand Clin. 2013;29(2):251–259. doi: 10.1016/j.hcl.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Tang JB. Indications, methods, postoperative motion and outcome evaluation of primary flexor tendon repairs in Zone 2. J Hand Surg Eur Vol. 2007;32(2):118–129. doi: 10.1016/J.JHSB.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Lalonde DH. Wide-awake flexor tendon repair. Plast Reconstr Surg. 2009;123(2):623–625. doi: 10.1097/PRS.0b013e318195664c. [DOI] [PubMed] [Google Scholar]
- 17.Lalonde D. Minimally invasive anesthesia in wide awake hand surgery. Hand Clin. 2014;30(1):1–6. doi: 10.1016/j.hcl.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 18.Lalonde DH, Martin AL. Wide-awake flexor tendon repair and early tendon mobilization in zones 1 and 2. Hand Clin. 2013;29(2):207–213. doi: 10.1016/j.hcl.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Tang JB, Avanessian B. New tendon, nerve, and bone surgical methods impacting the practice of hand surgery. Clin Plast Surg. 2014;41(3):xix–xxx. doi: 10.1016/j.cps.2014.06.003. [DOI] [PubMed] [Google Scholar]



