Abstract
Background
Suspension ligamentoplasty using abductor pollicis longus (APL) tendon without bone tunneling, was introduced as one of the techniques for treatment of advanced first carpometacarpal (CMC) arthritis. The purpose of this study was to evaluate the radiologic and clinical results of APL suspension ligamentoplasty.
Methods
The medical records of 19 patients who underwent APL suspension ligamentoplasty for advanced first CMC arthritis between January 2008 and May 2012 were reviewed retrospectively. The study included 13 female and 6 male patients, whose mean age was 62 years (range, 43 to 82 years). For clinical evaluation, we assessed the grip and pinch power, radial and volar abduction angle, thumb adduction (modified Kapandji index), including visual analogue scale (VAS) and Disabilities of the Arm, Shoulder and Hand (DASH) scores. Radiologic evaluation was performed using simple radiographs.
Results
The mean follow-up was 36 months (range, 19 to 73.7 months). Mean power improved from 18.3 to 27 kg for grip power, from 2.8 to 3.5 kg for tip pinch, and from 4.3 to 5.4 kg for power pinch. All patients showed decreased VAS from 7.2 to 1.7. Radial abduction improved from 71° preoperatively to 82° postoperatively. The modified Kapandji index showed improvement from 6 to 7.3, and mean DASH was improved from 41 to 17.8. The height of the space decreased from 10.8 to 7.1 mm. Only one case had a complication involving temporary sensory loss of the first dorsal web space, which resolved spontaneously.
Conclusions
The APL suspension ligamentoplasty for treatment of advanced first CMC arthritis yielded satisfactory functional results.
Keywords: Thumb, Carpometacarpal joint, Osteoarthritis, Tendon, Suspension ligamentoplasty
Due to the inherently unstable saddle joint and extrinsic tendon forces,1) the first carpometacarpal (CMC) joint is the most commonly affected site for osteoarthritis in hands. Although it is controversial to treat early stage CMC joint arthritis with surgery, advanced CMC arthritis necessitates surgical treatment if the symptoms are not relieved by non-surgical treatment. The management for advanced arthritis of this joint varies from simple trapeziectomy to numerous technical reconstruction surgeries, according to the stage of the disease and the surgeon's preference.1,2) Most of the treatments include total trapeziectomy, which can generate theoretical pinch weakness due to shortening of the first thumb ray.3) Recent studies have found no difference in functional results between simple trapeziectomy and ligament stabilization procedures. 3,4,5,6,7,8) However, Davis et al.5) show only a 1-year follow-up, while Field and Buchanan6) compared the results of simple trapeziectomy with ligament reconstruction and tendon interposition. Myriad techniques of suspension ligamentoplasty have been used widely to treat CMC arthritis of the thumb, while preserving the length of the first ray. Mathoulin et al.9) reported favorable results of simple suspension ligamentoplasty after trapeziectomy without bone procedure, using abductor pollicis longus (APL). The purpose of this study was to evaluate the clinical and radiologic results of this simple technique.
METHODS
Between January 2008 and May 2012, the records of 19 consecutive patients (19 unilateral cases) who were treated using the APL suspension ligamentoplasty, were retrospectively reviewed, after obtaining the approval of our Institutional Review Board. Indications for surgical treatment were advanced arthritis (Eaton stage III and IV)10) of the first CMC joint, which did not respond to conservative treatment (splinting and pain control). The patients with follow-up less than 1 year were excluded. There were 13 female and 6 male patients, having a mean age of 62 years (range, 43 to 82 years). The arthritis in 11 patients was in the dominant hand, and the remaining was in the non-dominant hand. The major cause was primary arthritis, with the exception of four posttraumatic arthritis cases.
Surgical Technique
The surgical technique mainly follows the method as described by Mathoulin et al.9) with minor modification in which the remaining APL tendon, after suture to the joint capsule, stuffed the trapezial space. Surgery was performed under general anesthesia or brachial plexus block with a pneumatic tourniquet. A zigzag skin incision of about 5 cm length was made over the CMC joint and over the anatomical stuff box starting at the base of the dorsum of the thumb. The superficial branch of the radial nerve and the radial artery were identified and protected. Between the extensor pollicis brevis tendon and the APL tendon, the capsule over the trapezium was opened in T- or H-shape. The trapezium was exposed with subperiosteal dissection. Trapeziectomy was performed in toto or piecemeal, while being careful not to damage the flexor carpi radialis (FCR) tendon which is located just volar to the trapezium. At the base of the trapezial space, the FCR tendon was identified. Usually the APL consists of several slips. One of the slips, which is located at the radial side and not attached to the thenar muscle, was harvested with the distal end attached to the base of the first metacarpal bone. The tendon of APL had to be divided as far proximally as possible to harvest at least a 6-cm length slip.
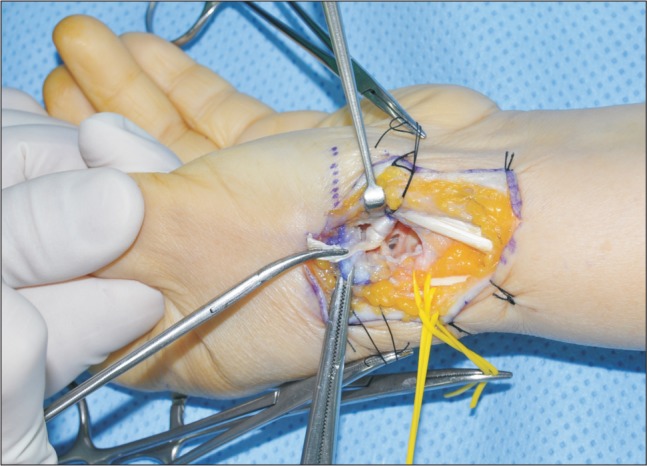
The APL slip was wrapped two or three times around the FCR tendon to make a hammock, which suspends the base of the first metacarpal bone; this prevents the proximal migration of the first metacarpal bone (Fig. 1). While the end of the APL slip was pulled tightly, two sutures of 3-0 prolene were passed through the crossed APL and FCR tendon bundle. Maintaining the tension of the APL, the end of the APL was stitched to the base of the first metacarpal bone with 3-0 absorbable vicryl suture material so that the first metacarpal base was suspended as far distally as possible. The remaining end of the APL slip was packed into the trapezial space. The dorsal capsule over the trapezial space was then closed.
Fig. 1. The abductor pollicis longus (APL) slip was wrapped two or three times around the flexor carpi radialis tendon to make a hammock, which suspended the base of the first metacarpal bone. The most distal end of the APL was put into the trapezial space after being fixed to the dorsal capsule.
Postoperative Immobilization and Rehabilitation
For 4 weeks, the thumb was immobilized in an abducted position in a thumb spica cast. Post immobilization, the activity of the thumb was encouraged.
Patient Evaluation and Follow-up
For clinical evaluation, we checked the visual analogue scale (VAS), patient satisfaction for the postoperative appearance of the hand, and time for returning to work. We also evaluated the range of motion (ROM) of the thumb, metacarpophalangeal joint ROM, interphalangeal joint ROM, palmar abduction, and radial abduction. Thumb opposition was assessed using the Kapandji11) scoring system. Grip strength, key pinch strength, and tip pinch strength were examined. The Disabilities of the Arm, Shoulder and Hand (DASH) score was used as another clinical assessment. The clinical assessments were made both preoperatively and at the latest follow-up visit.
Radiologic evaluation was performed by simple radiographs of the thumb, in which the height of the trapezial space was measured in anteroposterior view, both preoperatively and postoperatively. The measurement was performed by three independent orthopaedic hand surgeons, and averaged. Four routine radiographic views (anteroposterior, lateral, and both oblique views) were examined for both hands.
Statistical Analysis
Mann-Whitney U-test was used to analyze the difference between the preoperative and postoperative measurements. We considered p < 0.05 as significant.
RESULTS
The mean follow-up was 36 months (range, 19 to 73.7 months). There were 13 cases of stage III and 6 cases of stage IV arthritis.
Clinical Results
Clinical results including scores, ROM, and power are shown in Table 1. All patients expressed their satisfaction for improved postoperative appearance of the hand.
Table 1. Clinical and Radiological Results.
| Clinical result | Preoperative | Postoperative | p-value | ||
|---|---|---|---|---|---|
| Mean | Range | Mean | Range | ||
| Visual analogue scale | 7.2 | 3-10 | 1.7 | 0-3 | < 0.05 |
| DASH score | 41.0 | 19.6-66.0 | 17.8 | 8.5-36.2 | < 0.05 |
| Kapandji score | 6 | 5-7 | 7.3 | 5-9 | < 0.05 |
| Range of motion (°) | |||||
| Radial abduction | 71 | 60-90 | 82 | 70-90 | < 0.05 |
| Volar abduction | 71 | 50-90 | 79 | 60-90 | < 0.05 |
| Grip power (kg) | 18.3 | 5-26 | 27 | 10-44 | > 0.05 |
| Pinch power (kg) | |||||
| Tip pinch | 2.8 | 1-4 | 3.5 | 2-6 | > 0.05 |
| Power pinch | 4.3 | 1-6 | 5.4 | 3-8 | < 0.05 |
DASH: Disabilities of the Arm, Shoulder and Hand.
Radiologic Results
The height of the trapezial space was significantly reduced to 7.1 mm (range, 3.1 to 10.2 mm) postoperatively, from 10.8 mm (range, 8.7 to 12.6 mm) preoperatively (p < 0.05) (Figs. 2 and 3).
Fig. 2. The immediate postoperative radiograph showed a trapezial space of 10 mm.
Fig. 3. The trapezial space decreased to 7.7 mm at 17 months after surgery.
Complications
A solitary case of temporary sensory loss of the first dorsal web space was observed, which recovered spontaneously. No other surgery-related complications, such as infection or wound problems, were reported. No complex regional pain syndrome was reported. Among the 13 patients who were working preoperatively, three patients returned to their work without any difficulty or occupation modification (two light manual workers, and a taxi driver). Modifications were required in three patients to enable them to return to their original occupations (two were manual workers). The remaining seven were housewives, who returned to their daily activities.
DISCUSSION
In most cases, nonoperative treatment should take priority for CMC joint arthritis. The surgical indications for CMC joint arthritis are patients having consistent symptoms, although nonoperative modalities have been applied. The surgical interventions include volar ligament reconstruction which is indicated for early stage arthritis,12) and trapeziectomy and its variations for late stage arthritis. Although some reports revealed no functional difference between simple trapeziectomy and trapeziectomy with reconstruction,4,5) a myriad of techniques to avoid telescoping of the thumb ray have been used. For this reason, local tendons were utilized, including FCR. Suspension ligamentoplasty using the APL tendon was one of the techniques advocated by several authors.9,13,14,15,16) Mathoulin et al.9) described a modified APL suspension ligamentoplasty with successful pain relief in the patients. The technique avoids bone procedure, such as making a bone tunnel,13,14) and does not consist of complex tendon fabrication.15,16,17) We focused our study on the simplicity of this technique.
Employing this technique, we obtained excellent pain control and functional results without severe complications. All patients had pain relief with a mean VAS score of 1.7, and returned to their respective occupational activities. Although we cannot simply compare our results to the previous study or other ligamentoplasties, the decreased VAS may be indicative of the efficacy of this procedure. However, the radiographs suggested that the proximal migration of the base of the metacarpal bone progressed somewhat in this short-term follow-up study. We postulated that the 'hammock' effect of the tendon bundle prohibits proximal migration of the metacarpal bone. Hence, the conclusion on this postulation should be postponed until a long-term follow-up is acquired.
In addition to favorable results, there are two major advantages of using this technique. First, this technique is simple. Without a risk of bone fracture by bone tunneling and nuisance from other additional procedure, we could make the 'hammock' which suspended the base of the first proximal phalanx. Second, using the APL slip has the advantage of reducing thumb deformation, i.e., dorsal subluxation of the base of the first metacarpal bone. The APL tendon attaches to the base of the first metacarpal bone, hence giving force against dorsal subluxation. Because we used the partial slip of the APL tendon, the deforming force decreased and the subluxation may also decrease. The technical point to be noted is that only a radial slip of the APL is used, and not an ulnar one which attaches to the thenar muscle. Using more slips than one, especially ones which attach to the thenar muscle, might abate abduction power of the thumb.
This study has its limitations, which are as follows: (1) retrospective design, (2) small number of patients, and (3) short-term follow-up. Despite the theoretical advantages of this procedure and the success achieved in this study, comparative studies regarding pain control, functional score, and migration of the thumb ray may be needed which involves larger number of cases in a randomized fashion. Until then, definite conclusions from the results of this study should be delayed. In addition, we need a more objective measurement tool to evaluate the improvement of dorsal angulation of the first CMC joints.
This being a relatively simple procedure having minimal complications, we obtained good pain relief and functional outcomes. We can cautiously conclude that APL suspension ligamentoplasty might be an alternative for advanced arthritis of the first CMC joint, with minimal complications.
ACKNOWLEDGEMENTS
This research was supported by the convergence technology development program for bionic arm through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Plannig (No. 2014M3C1B2048422).
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Cooney WP, 3rd, Chao EY. Biomechanical analysis of static forces in the thumb during hand function. J Bone Joint Surg Am. 1977;59(1):27–36. [PubMed] [Google Scholar]
- 2.Gervis WH, Wells T. A review of excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint after twenty-five years. J Bone Joint Surg Br. 1973;55(1):56–57. [PubMed] [Google Scholar]
- 3.Murdoch G. Errors of diagnosis revealed at meniscectomy. J Bone Joint Surg Br. 1957;39(3):502–507. doi: 10.1302/0301-620X.39B3.502. [DOI] [PubMed] [Google Scholar]
- 4.Belcher HJ, Nicholl JE. A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg Br. 2000;25(4):350–356. doi: 10.1054/jhsb.2000.0431. [DOI] [PubMed] [Google Scholar]
- 5.Davis TR, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29(6):1069–1077. doi: 10.1016/j.jhsa.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Field J, Buchanan D. To suspend or not to suspend: a randomised single blind trial of simple trapeziectomy versus trapeziectomy and flexor carpi radialis suspension. J Hand Surg Eur Vol. 2007;32(4):462–466. doi: 10.1016/J.JHSB.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Downing ND, Davis TR. Trapezial space height after trapeziectomy: mechanism of formation and benefits. J Hand Surg Am. 2001;26(5):862–868. doi: 10.1053/jhsu.2001.27761. [DOI] [PubMed] [Google Scholar]
- 8.Tomaino MM. Basal metacarpal osteotomy for osteoarthritis of the thumb. J Hand Surg Am. 2011;36(6):1076–1079. doi: 10.1016/j.jhsa.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 9.Mathoulin C, Moreel P, Costa R, Wilson SM. Abductor pollicis longus "hammock" ligamentoplasty for treatment of first carpometacarpal arthritis. J Hand Surg Eur Vol. 2008;33(3):292–297. doi: 10.1177/1753193408087073. [DOI] [PubMed] [Google Scholar]
- 10.Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55(8):1655–1666. [PubMed] [Google Scholar]
- 11.Kapandji A. Clinical test of apposition and counter-apposition of the thumb. Ann Chir Main. 1986;5(1):67–73. doi: 10.1016/s0753-9053(86)80053-9. [DOI] [PubMed] [Google Scholar]
- 12.Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984;9(5):692–699. doi: 10.1016/s0363-5023(84)80015-5. [DOI] [PubMed] [Google Scholar]
- 13.Brunelli G, Monini L, Brunelli F. Stabilisation of the trapezio-metacarpal joint. J Hand Surg Br. 1989;14(2):209–212. doi: 10.1016/0266-7681_89_90128-9. [DOI] [PubMed] [Google Scholar]
- 14.Kaarela O, Raatikainen T. Abductor pollicis longus tendon interposition arthroplasty for carpometacarpal osteoarthritis of the thumb. J Hand Surg Am. 1999;24(3):469–475. doi: 10.1053/jhsu.1999.0469. [DOI] [PubMed] [Google Scholar]
- 15.Sigfusson R, Lundborg G. Abductor pollicis longus tendon arthroplasty for treatment of arthrosis in the first carpometacarpal joint. Scand J Plast Reconstr Surg Hand Surg. 1991;25(1):73–77. doi: 10.3109/02844319109034926. [DOI] [PubMed] [Google Scholar]
- 16.Sirotakova M, Figus A, Elliot D. A new abductor pollicis longus suspension arthroplasty. J Hand Surg Am. 2007;32(1):12–22. doi: 10.1016/j.jhsa.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 17.Rutegard JN, Eriksson C, Olsson K. Tendon arthroplasty for treatment of trapeziometacarpal arthrosis. Scand J Plast Reconstr Surg Hand Surg. 1994;28(4):295–298. doi: 10.3109/02844319409022015. [DOI] [PubMed] [Google Scholar]




