Abstract
The aim of this brief analytical review is to highlight and disentangle research dilemmas in the field of exercise addiction. Research examining exercise addiction is primarily based on self-reports, obtained by questionnaires (incorporating psychometrically validated instruments), and interviews, which provide a range of risk scores rather than diagnosis. Survey methodology indicates that the prevalence of risk for exercise addiction is approximately 3 percent among the exercising population. Several studies have reported a substantially greater prevalence of risk for exercise addiction in elite athletes compared to those who exercise for leisure. However, elite athletes may assign a different interpretation to the assessment tools than leisure exercisers. The present paper examines the: 1) discrepancies in the classification of exercise addiction; 2) inconsistent reporting of exercise addiction prevalence; and 3) varied interpretation of exercise addiction diagnostic tools. It is concluded that there is the need for consistent terminology, to follow-up results derived from exercise addiction instruments with interviews, and to follow a theory-driven rationale in this area of research.
Keywords: athlete, behavioral addiction, commitment to exercise, exerciser, methodology
Introduction
While studying the effects of exercise on sleep, Baekeland [1] noted that regular exercisers experienced withdrawal symptoms when deprived of exercise. This observation pointed to the addictive nature of exercise and provided an important starting point and impetus for research into exercise addiction. Exercise addiction falls within the field of behavioral addictions, similar to gambling disorder, but due to the lack of sustained and methodologically rigorous evidence for exercise addiction as a morbidity, the disorder is not listed as a mental dysfunction in the latest (fifth) edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [2]. In fact, to the authors’ knowledge, only three case studies have been reported in the literature to date [3,4,5].
Exercise addiction has been described as a morbid pattern of behavior in which the habitually exercising individual loses control over his or her exercise habits and acts compulsively, exhibits dependence, and experiences negative consequences to health as well as in his or her social and professional life. It is different from exaggerated exercise present in various eating disorders (also known as secondary exercise addiction [5]), in which the behavior represents a means of weight loss rather than addiction. The negative consequences experienced are the key factors that separate healthy from unhealthy patterns of exercise. In addition to bodily injuries and re-injuries due to exaggerated amounts of exercise without proper rest and recuperation, social and psychological hardship is also evident in exercise addiction [3]. The inability to sleep and concentrate, a sense of restlessness, and painful withdrawal symptoms (akin to substance abuse) are also daily manifestations in exercise addiction [3]. These negative consequences are so severe that they interfere with the normal daily functioning of the individual. Therefore, exercise addiction is a serious psychological morbidity that should be understood and recognized by clinicians and prevented whenever possible.
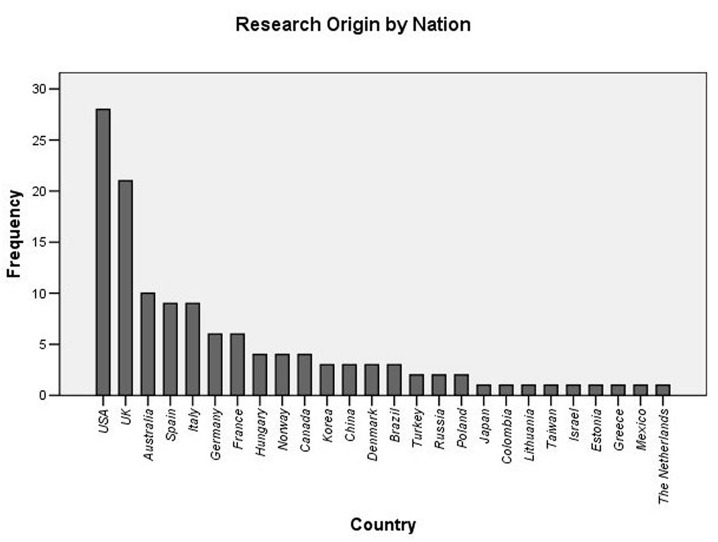
The present authors carried out an analysis of published outputs in PubMed and Google Scholar over a 3-year period (January 2011 to January 2014), and 128 publications were found that examine exercise addiction. This shows that there are approximately 40 publications per year on exercise addiction in recent years. The 128 publications appeared in 89 different journals, showing that exercise addiction is studied in a multidisciplinary field. The majority of the research comes primarily from just three developed nations (Figure 1), where exercise may represent a higher-order need in contrast to the less-developed nations [6]. In spite of the growing keen interest in exercise addiction research, there are several methodological and also conceptual limitations that obscure the focus of the research and obstruct the advancement of knowledge in the area. These limiting factors delay the hope for the inclusion of the disorder in a future edition of the DSM.
Figure 1.
Country origin of research on exercise addiction over a 3-year period (2011-2014) based on publications identified by PubMed and Google Scholar. The frequency denotes the number of papers published by scholars in the given nation over 3 years.
The present paper is organized into three main sections: 1) the discrepancies in the classification of exercise addiction; 2) the inconsistent reporting of exercise addiction prevalence; and 3) the varied interpretation of exercise addiction diagnostic tools. Through the analysis of these sections, it will be demonstrated that there is an urgent need for consistent terminology, a good reason for following up on questionnaire results with interviews, and a need to conduct theory-based research in the area.
Discrepancies in Classification of Exercise Addiction
Terminology
To date, research investigating exercise addiction has been unfocused. For example, several terminologies are used for describing exercise addiction, including: exercise dependence [7], compulsive exercise [8], obligatory exercise [9], and exercise abuse [10]. Cook and Hausenblas [11] specifically noted that using the same scientific term to denote different situations or adopting different terms for the same situation leads to ambiguity, misconception, irreproducible results, and errors in interpretation. In spite of the fact that exercise dependence is the most often-used term (Table 1), some scholars [12,13] have emphasized that the term addiction may be the most appropriate, because it includes both dependence and compulsion [14].
Table 1. Research using different terminologies for the pathological exercise.
| Terms used in the title of published papers listed on two scholastic databases | Number of studies found on PubMed and Google Scholar in May 2015 |
| Exercise addiction | PubMed 18, Scholar 158 |
| Exercise dependence | PubMed 56, Scholar 256 |
| Compulsive exercise | PubMed 17, Scholar 70 |
| Obligatory exercise | PubMed 7, Scholar 47 |
| Exercise abuse | PubMed 2, Scholar 9 |
Amount of Exercise
Exercising excessively does not necessarily indicate a disorder. A further dilemma concerns the evaluation of exercise addiction, which considers the maladaptive behavior as being reflected by very high (often termed as “exaggerated”) volume of exercise. However, excessive exercise itself is not necessarily maladaptive. Athletes who become national or international competitors spend the largest proportion of their day in training or activities related to their training without having psychological problems related to their volume of exercise and/or the general stresses of their day-to-day job (something that would be experienced by most workers in whatever job they do and therefore not necessarily related to exercise addiction). They do not experience harm (apart from injuries) in their personal and social lives as a consequence of their excessive exercise behavior, because the latter is part of their expected daily routine, so they can also fulfill their other life obligations. In contrast, morbid patterns of exercise can result in personal and social harm to the individual.
Inconsistent Reporting of Exercise Addiction Prevalence
Questionnaire-based studies establish the risk for exercise addiction rather than clinical cases (diagnosis). The latter can be made using the criteria for addictive disorders listed in the DSM-5. To date, and as noted earlier, only three such cases have been reported [3,4,5]. A prominent inconsistency in the field concerns the reporting of prevalence rates for exercise addiction. For instance, Mónok et al. [15] found that the incidence of high risk for exercise addiction is 0.3 percent to 0.5 percent in the general population, while among regular exercisers it is 1.9 percent to 3.2 percent. A figure of around 3.0 percent is consistent with several empirical studies in the literature [13,16,17,18,19,20]. However, there are numerous reports with prevalence rates that exceed five to 10 times this figure. For example, Lejoyeux et al. [21] reported that 42 percent of a sample were diagnosed with exercise addiction (“All clients of the fitness room 18 years and older were invited to participate in the study. Three hundred subjects were included; 125 (42 percent) presented diagnostic criteria of exercise dependence.”). Apart from the issue that questionnaires do not serve diagnostic purposes (discussed below), the wide range of prevalence rates reported for the disorder raise questions about why the findings are so inconsistent.
There are probably several explanations for the wide diversity of prevalence rates for exercise addiction. First, the various assessment scales used may yield different results. Even the two most popular and well-validated instruments in the field, the Exercise Addiction Inventory (EAI) [22] and the Exercises Dependence Scale (EDS) [23] generate somewhat different, although arguably comparable, results [15]. The difference between the two instruments is that the latter is based on DSM and its revised version has 21 items, while the former is based on six common symptoms of addiction [13] and has only six items. Second, the populations sampled in various studies may not only be different (e.g., students, runners, body builders, gym users, etc.), but also, as a consequence of this diversity, may attribute different interpretation to the items in the survey instrument used [24]. Third, recent evidence shows that there are differences in the subjective interpretation of the items on the EAI between men and women, as well as across different cultures [24]. Therefore, the gender ratio in a sample and cultural component of any given investigation also may contribute to the large difference in prevalence rates. Furthermore, intense involvement with sports and exercise may influence either the interpretation and/or the actual scoring of the instruments utilized. Indeed, Szabo and Griffiths [19] showed that Sport Science undergraduates reported being at twice the risk for exercise addiction than general, habitual exercisers.
It appears that the risk for exercise addiction is influenced by several subjective and objective factors. Consideration of all known factors such as gender, athletic involvement, and all others shown to have an effect on the results may — at least in part — help bring about greater agreement in the reports of risk-prevalence of exercise addiction. Results of prior empirical research may only have been relevant to a homogeneous subgroup of exercisers. This appears to be a fact that needs to be recognized by the scholastic community before attempting to generalize the findings across the field.
Varied Interpretation of Exercise Addiction Diagnostic Tools
Need for Interviews
Instruments that assess exercise addiction do not serve as diagnostic tools for exercise addiction. The problem with sole reliance on self-report instruments in studying exercise addiction is that they yield a range of scores with values in the higher end that are interpreted as indices of risk for addiction. A score (on such instruments) may not indicate damage or detriment to individuals or those around them. If there is no harm, there is no addiction. By definition, excessive exercise is only problematic if it results in some sort of harm (injury, negligence of work, family, or other obligations that trigger negative consequences or harm in the individual's life). Therefore, data obtained using validated instruments need to be followed up with interviews and/or corroborative evidence to elaborate and confirm individual negative consequences. However, only a very small proportion of the empirical studies examining exercise addiction has complemented survey data with interviews.
Müller at al. [25] examined the level of agreement between the questionnaire-based classification of “at-risk for exercise addiction” and the results of the evaluations conducted via interviews. These authors studied 134 participants using the EDS and a structured clinical interview. The congruence between the questionnaire-based categorizations of “at-risk for exercise addiction” and the diagnosis of the disorder was examined using k-coefficients (Cohen’s kappa coefficient [26]). The findings demonstrated that the agreement between questionnaire-based and interview-based assessment was only fair to moderate, with more false positive classifications emerging from self-report instruments. The authors concluded that if the structured clinical interview is accepted to be a reliable method for the detection of the disorder, then the instruments — in this case, the EDS, which is one of the most reliable assessment tools for exercise addiction — overestimates the risk for the prevalence of exercise addiction.
The clear message of Müller et al.’s study is that without an associated interview, researchers cannot be certain of a problem in the exercise behavior of their study participants. Between the “at-risk” classification and disorder, there is an obscure gray area because it is relatively unpredictable (at the present time) as to who will develop an exercise addiction disorder from among those who were classified — via questionnaires — as being “at-risk” for the disorder. A clear borderline between “at-risk” and pathology is the evidence of harm suffered as a consequence of the (exercise) behavior. This “at-risk/disorder” borderline can only be rigorously assessed via interviews on a case-by-case basis. This is because via interviews “approaching” harm and lack of control over exercise may surface in a clearer way than via assessment scales. The mistake of not using interviews in diagnosis is a major shortcoming of the exercise addiction literature and hinders the advancement of the knowledge in the field. The present authors recommend that future studies should examine the disorder by (at the very least) interviewing those who score above a given cutoff point on a given paper-and-pencil instrument. These interviews should look not only to presence but also to the severity of the symptoms of addiction and the risk of harm to the physical and mental health of the individual. Any detrimental health effects and the endorsement of DSM-5 criteria for addictive disorders should be interpreted as markers of a morbid exercise pattern.
Issues with Using Elite Athletes as Test Subjects
Unlike athletic training, the satisfying of addictive urges cannot be scheduled. If elite athletes were addicted, they would have to exercise beyond their already demanding training schedule, which would be physically impossible. Therefore, studying exercise addiction among elite athletes could be viewed as futile. Nevertheless, researchers have begun to examine exercise addiction among elite or competitive athletes. Despite the fact that exercise addiction — if present — could represent the end of the sporting career for elite athletes, most studies that have scrutinized them have reported a significantly higher prevalence of high risk for exercise addiction than in leisure or student exercisers. Blaydon and Lindner [27] studied 203 triathletes competing at amateur (n = 133) and professional (n = 70) levels. They found that the incidence of exercise addiction ranged from 21.6 percent to 30.4 percent in the whole sample, while among the sub-sample of professional athletes, 41.4 percent were at risk for exercise addiction. Studying participants competing at different triathlon distances, Youngman [28] reported that almost 20 percent of the 1,285 triathletes studied were at risk for exercise addiction. According to the results of a study by McNamara and McCabe [29], approximately one-third of Australian elite athletes (34 percent) may be at high risk for exercise addiction. In a more recent investigation, a significant proportion of Spanish ultra-marathoners (17 percent) were classified as at high risk for exercise addiction [30]. Results with Italian athletes have shown a similar rate, with 18.3 percent of 262 competitive athletes from nine different sports (basketball, futsal, football, handball, hockey, rugby, softball, volleyball, and water polo) found to be at risk for exercise addiction [31]. A lower incidence of 7.1 percent was found in non-professional second and third division Danish soccer players [32]. However, even this “lower” figure is high, considering the much lower percentages found in the general and recreational exercising population [13,15,20].
A major conceptual concern regarding these high prevalence figures (ranging between 7 percent and 42 percent) is that if elite athletes are indeed at such a high risk for exercise addiction, then coaches, health professionals, and research scholars are dealing with a psychopathology-prone athletic population. However, this is very unlikely. To date, there is no empirical data that has recognized differences in the interpretation of the scale items by leisure exercisers and elite athletes. This issue needs systematic investigation in the future, because, conceptually, the investigation of the disorder among elite athletes does not make any rational sense.
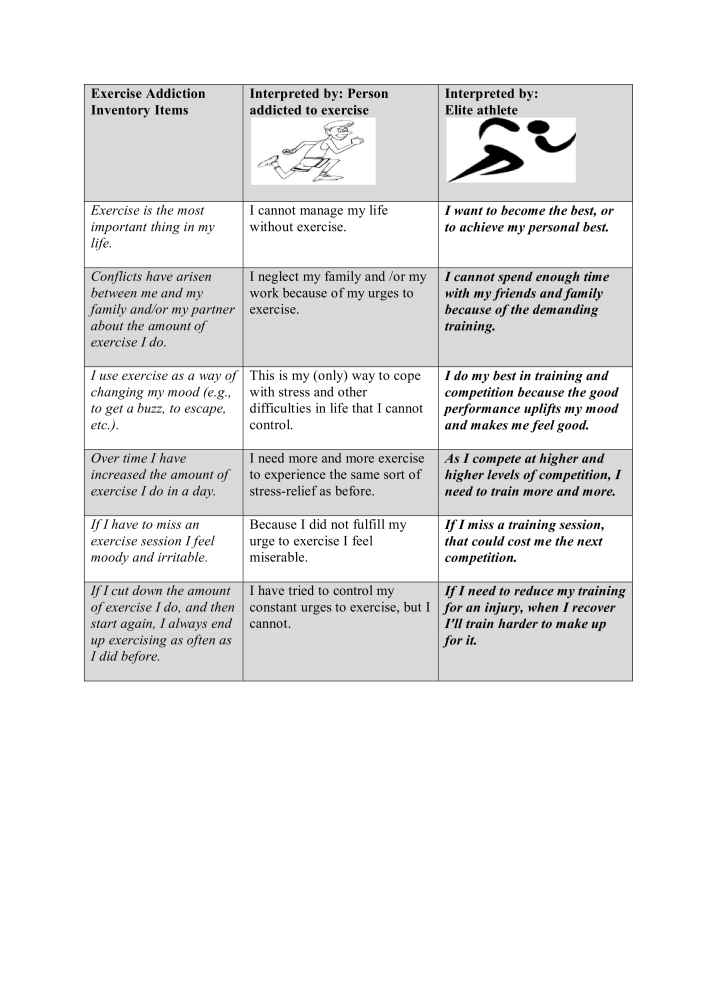
First, by definition in exercise addiction, there is a loss of control over the behavior. Therefore, the gratification must occur when the urge compels the individual to exercise. In sports, training and competition sessions are scheduled. They do not match one’s inner urges and compulsions. Hence, the exercise-addicted athlete would need to exercise before and after training, too, which would be physically impossible. There is no scheduled addiction. The high “addiction” scores of athletes must therefore be due to a different interpretation of the instrument’s items. For example, “Exercise is the most important thing in my life” (Item 1 of the EAI) can also be interpreted as the main goal is to succeed in sporting career; thus, an endorsement of “strongly agree” (maximum score) on the questionnaire may be a sincere response from an elite athlete. Furthermore, athletes also may experience conflicts in their lives because of their training. The frequent and demanding workouts could interfere with their personal and social lives. However, like work interfering with other life activities for other people, this type of conflict is not the intra- and interpersonal conflict that is experienced by people addicted to exercise. Nevertheless, a high or maximum high score may be given for Item 2 on the EAI: “Conflicts have arisen between me and my family and/or my partner about the amount of exercise I do” at the time of assessment. Another item on the EAI is: “If I have to miss an exercise session I feel moody and irritable.” Professional athletes naturally will get irritated when they have to miss an important training session, because that may cost them participation at an upcoming competition. Further possible differences in interpretation of instrument items are illustrated in Figure 2.
Figure 2.
Illustration of the possible different interpretations of the statements on the EAI by maladaptive exercisers and elite athletes. Note: The key point of Figure 2 is to illustrate that different interpretations may yield equally high scores leading to erroneous conclusions.
Consequently, elite athletes demonstrate high ratings on the instruments assessing exercise addiction, not because of morbidity but because of a different interpretation associated with their high commitment to their sporting profession. Their responses may involve aspirations and visions within their strong motivation to become the best they can be in their sport. Without follow-up interviews, the athletes’ high scores on exercise addiction instruments may be a conceptual mistake. Müller et al. [25] have demonstrated that self-report instruments overestimate the prevalence of exercise addiction. In the case of elite athletes, this observation may be even more pertinent.
Conclusions and Outlook
Research examining exercise addiction is steadily growing, yet methodological and conceptual limitations hinder advancement of knowledge in the field. As yet, there is no consistency in describing addictive exercise behavior. Self-report instruments only provide a risk score, and due to inconsistent interpretations related to the nature of the studied sample (e.g., participants’ gender, athletic involvement, and cultural differences), the meaning of the self-report data is difficult to explain and/or interpret. The presumption that athletes are addicted to exercise may be wrong. Their higher scores compared to leisure exercisers may reflect different attitudes toward exercise and sport behavior that are mirrored in a different interpretation of the instrument items.
Future research should therefore use in-depth interviews with those suspected to be addicted to exercise as based on their high scores obtained on relevant instruments. Research into exercise addiction should be theoretically driven. For example, the description of behavioral disorders in the “Addictive Disorders” section of the DSM-5 is potentially useful as a model for studying exercise addiction, while also taking into consideration the common symptoms found in addictions [13]. Like all other addictions, exercise addiction may reflect an escape from a hardship along with an accessible way to overcome negative criticism, because exercise itself is a positive and socially valued behavior. The diagnosis of exercise addiction should establish harm and damage — and its cause — suffered by the individual as a consequence of the maladaptive exercise behavior.
Abbreviations
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders, 5th edition
- EAI
Exercise Addiction Inventory
- EDS
Exercise Dependence Scale
Author contributions
AS and ZD conceived the framework of the paper and wrote the majority; MDG had conceptual and theoretical input and also wrote parts of the paper; RVM synthesized the literature, provided writing ideas and critically evaluated the final version of the manuscript; BM reviewed PubMed and Google Scholar for research trends in exercise addiction.
References
- Baekeland F. Exercise deprivation: sleep and psychological reactions. Arch Gen Psychiatry. 1970;22(4):365–369. doi: 10.1001/archpsyc.1970.01740280077014. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Griffiths M. Exercise addiction: a case study. Addiction Research. 1997;5(2):161–168. [Google Scholar]
- Kotbagi G, Muller I, Romo L, Kern L. Pratique problématique d’exercice physique: un cas clinique. Annales Médico-Psychologuiques Revue Psychiatrique. 2014;172(10):883–887. [Google Scholar]
- Veale CD. In: Exercise addiction: motivation for participation in sport and exercise. Anett J, Cripps B, Steinberg H, editors. Leicester, UK: The British Psychological Society; 1995. Does primary exercise dependence really exist; pp. 1–5. [Google Scholar]
- Maslow AH. Toward a psychology of being. New York: Start Publishing; 2002. [Google Scholar]
- Adams J. Understanding exercise dependence. J Contemp Psychother. 2009;39(4):231–240. [Google Scholar]
- Murray SB, Maguire S, Russell J, Touyz SW. The emotional regulatory features of bulimic episodes and compulsive exercise in muscle dysmorphia: a case report. Eur Eat Disord Rev. 2012;20(1):68–73. doi: 10.1002/erv.1088. [DOI] [PubMed] [Google Scholar]
- Thome JL, Espelage DL. Obligatory exercise and eating pathology in college females: replication and development of a structural model. Eat Behav. 2007;8(3):334–349. doi: 10.1016/j.eatbeh.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Calogero RM, Pedrotty KN. The practice and process of healthy exercise: an investigation of the treatment of exercise abuse in women with eating disorders. Eat Disord. 2004;12(4):273–291. doi: 10.1080/10640260490521352. [DOI] [PubMed] [Google Scholar]
- Cook BJ, Hausenblas HA. The role of exercise dependence for the relationship between exercise behavior and eating pathology mediator or moderator? J Health Psychol. 2008;13(4):495–502. doi: 10.1177/1359105308088520. [DOI] [PubMed] [Google Scholar]
- Berczik K, Szabo A, Griffiths MD, Kurimay T, Kun B, Urbán R. et al. Exercise addiction: symptoms, diagnosis, epidemiology, and etiology. Subst Use Misuse. 2012;47(4):403–417. doi: 10.3109/10826084.2011.639120. [DOI] [PubMed] [Google Scholar]
- Szabo A. Addiction to exercise: a symptom or a disorder? New York: Nova Science Publishers; 2010. [Google Scholar]
- Goodman A. Addiction: definition and implications. Brit J Addict. 1990;85(11):1403–1408. doi: 10.1111/j.1360-0443.1990.tb01620.x. [DOI] [PubMed] [Google Scholar]
- Mónok K, Berczik K, Urbán R, Szabo A, Griffiths MD, Farkas J. et al. Psychometric properties and concurrent validity of two exercise addiction measures: a population wide study. Psychology of Sport and Exercise. 2012;13(6):739–746. [Google Scholar]
- Allegre B, Therme P, Griffiths M. Individual factors and the context of physical activity in exercise dependence: a prospective study of ‘ultra-marathoners’. Int J Ment Health Addiction. 2007;5(3):233–243. [Google Scholar]
- Edmunds J, Ntoumanis N, Duda JL. Examining exercise dependence symptomatology from a self-determination perspective. J Health Psychol. 2006;11(6):887–903. doi: 10.1177/1359105306069091. [DOI] [PubMed] [Google Scholar]
- Griffiths MD, Szabo A, Terry A. The exercise addiction inventory: a quick and easy screening tool for health practitioners. Brit J Sport Med. 2005;39(6):e30. doi: 10.1136/bjsm.2004.017020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo A, Griffiths MD. Exercise addiction in British sport science students. Int J Ment Health Addiction. 2007;5(1):25–28. [Google Scholar]
- Szabo A. In: Physical activity and psychological well-being. Biddle SJH, Fox KR, Boutcher SH, editors. London: Routledge; 2000. Physical activity a s a source of psychological dysfunction; pp. 130–153. [Google Scholar]
- Lejoyeux M, Avril M, Richoux C, Embouazza H, Nivoli F. Prevalence of exercise dependence and other behavioral addictions among clients of a Parisian fitness room. Compr Psychiatry. 2008;49(4):353–358. doi: 10.1016/j.comppsych.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Terry A, Szabo A, Griffiths MD. The exercise addiction inventory: a new brief screening tool. Addiction Research & Theory. 2004;12(5):489–499. [Google Scholar]
- Hausenblas HA, Symons Downs D. How much is too much? The development and validation of the exercise dependence scale. Psychology and Health. 2002;17(4):387–404. [Google Scholar]
- Griffiths MD, Urbán R, Demetrovics Z, Lichtenstein MB, de la Vega R, Kun B. et al. A cross-cultural re-evaluation of the Exercise Addiction Inventory (EAI) in five countries. Sports Medicine – Open. 2015;1(1):1–5. doi: 10.1186/s40798-014-0005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller A, Cook B, Zander H, Herberg A, Müller V, de Zwaan M. Does the German version of the Exercise Dependence Scale measure exercise dependence? Psychology of Sport and Exercise. 2014;15(3):288–292. [Google Scholar]
- Carletta J. Assessing agreement on classification tasks: the kappa statistic. Computational Linguistics. 1996;22(2):249–254. [Google Scholar]
- Blaydon MJ, Lindner KJ. Eating disorders and exercise dependence in triathletes. Eat Disord. 2002;10(1):49–60. doi: 10.1080/106402602753573559. [DOI] [PubMed] [Google Scholar]
- Youngman JD. Risk for exercise addiction: a comparison of triathletes training for sprint-, olympic-, half-Ironman-, and Ironman-distance triathlons [dissertation] [Miami FL]: University of Miami; 2007. Available from: http://scholarlyrepository.miami.edu/oa_dissertations/12/ [Google Scholar]
- McNamara J, McCabe MP. Striving for success or addiction? Exercise dependence among elite Australian athletes. J Sports Sci. 2012;30(8):755–766. doi: 10.1080/02640414.2012.667879. [DOI] [PubMed] [Google Scholar]
- Szabo A, Vega R, Ruiz-Barquín R, Rivera O. Exercise addiction in Spanish athletes: investigation of the roles of gender, social context and level of involvement. J Behav Addict. 2013;2(4):249–252. doi: 10.1556/JBA.2.2013.4.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa S, Hausenblas HA, Oliva P, Cuzzocrea F, Larcan R. Perceived parental psychological control and exercise dependence symptoms in competitive athletes. Int J Ment Health Addiction. 2015;13(1):59–72. [Google Scholar]
- Lichtenstein MB, Larsen KS, Christiansen E, Støving RK, Bredahl TVG. Exercise addiction in team sport and individual sport: prevalences and validation of the exercise addiction inventory. Addiction Research & Theory. 2014;22(5):431–437. [Google Scholar]