Abstract
Background:
Although sinus restoration for transverse-sigmoid sinus (TSS) dural arteriovenous fistula (DAVF) has rarely been reported over the past decade, its advantage and indication still remain unclear. Herein, we discuss the indications and technical aspects of this therapy with a review of the literature.
Case Description:
A 79-year-old female was referred to our department with generalized convulsion. An angiogram revealed a DAVF at the junction of the right TSS. The right sigmoid and left transverse sinuses were occluded, which resulted in remarkable leptomeningeal venous reflux and cerebral venous congestion. A preoperative computed tomography (CT) venogram precisely revealed the occluded segment of the right sigmoid sinus, which facilitated the sinus restoration with balloon percutaneous transluminal angioplasty and stenting.
Conclusion:
Sinus restoration is preferable in patients with severe cerebral venous congestion due to multiple sinus occlusions and/or a restricted collateral venous outlet. CT venography is useful for precise evaluation of the length and configuration of the occluded segment, which thus make it possible to evaluate the feasibility of stenting.
Keywords: Computed tomography venography, dural arteriovenous fistula, sinus restoration, stent, transverse-sigmoid sinus
INTRODUCTION
Treatment of dural arteriovenous fistulas (DAVFs) at the junction of the right transverse-sigmoid sinus (TSS) can include transvenous coil embolization (TVE) of the affected sinus or transarterial embolization (TAE) using onyx, particularly in patients with advanced lesions such as Cognard Type III and IV and Borden Type III.[5,7] However, DAVFs are often difficult to treat when they have multiple sinus occlusions or diffuse fistulae with multiple feeders. Restricted venous outlets are the obstacle that make the treatment strategy demanding. In such cases, using a remodeling technique can be preferable compared with TAE or TVE.[11] Although several authors have reported and encouraged the use of venous remodeling technique as an alternative to TAE or TVE, its advantage and indication still remains unclear.[2,4,6,9,10,11] Herein, we report a case of TSS DAVF successfully treated by sinus restoration, which was complicated due to multiple venous sinus restrictions. In addition, we discuss the indications and technical aspects of this therapy with a review of the literature.
CASE REPORT
A 79-year-old female presented with progressive deterioration of her cognitive function over a period of 10 months. She became bedridden and was referred to our department due to convulsive seizure. She scored only three points with a mini-mental state examination (MMSE) at the time of admission. Magnetic resonance imaging diagnosed prominent DAVF in the right transverse sinus. Numerous flow voids corresponding to varicose veins were observed over the superficial and deep surfaces of the brain. A subsequent diagnostic angiogram showed DAVF at the junction of the right TSS fed by several branches originating from the right external carotid artery, involving the middle meningeal artery, occipital artery, posterior auricular artery, and accessory meningeal artery. The tentorial artery arose from the right internal carotid artery also fed the fistulae [Figure 1a and c]. The right sigmoid sinus and left transverse sinus were occluded. The patency of the right jugular bulb and an internal jugular vein was obscured by the angiogram. Retrograde venous drainage was directed toward the straight and superior sagittal sinuses. Markedly dilated cortical veins were noted. A reverse flow was primarily observed in the dilated left superficial middle cerebral vein toward the cavernous sinus and vein of Labbe toward the left sigmoid sinus [Figure 1b and d]. The DAVF was diagnosed as Cognard Type IIa + Type IIb and Borden Type II.[1,3]
Figure 1.
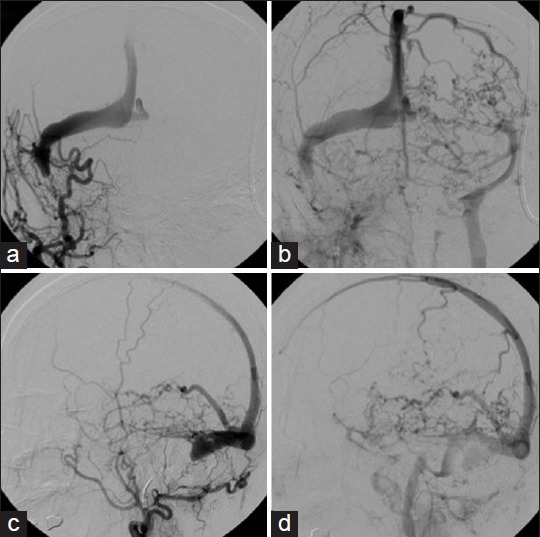
Preoperative angiogram. Right external carotid artery angiogram (a and c: Early phase, b and d: Late phase) showing a transverse-sigmoid sinus dural arteriovenous fistula with occlusive changes in both the right sigmoid sinus and the left transverse sinus. Marked retrograde venous drainage was directed toward the deep venous system through the straight sinus and toward the cerebral hemisphere via the superior sagittal sinus
The cerebral circulatory disturbance was due to venous congestion, which was caused by TSS DAVF and bilateral venous sinus occlusion [Figure 4a]. The clinical symptoms of the patient were considered to be due to this cerebral circulatory insufficiency, and therefore sinus restoration may be a more preferable treatment than TAE or TVE to improve the cerebral venous return. Considering the sinus restoration strategy, we performed computed tomography (CT) venography preoperatively, which precisely revealed an occluded segment [Figure 2] and the right jugular bulb and internal jugular vein were both patent. The patient and her family were thoroughly informed of the nature of the intended procedure; they understood its potential risks and benefits and agreed to the treatment. The patient was given 100 mg of aspirin and 75 mg of clopidogrel daily, started 7 days before the intervention.
Figure 4.
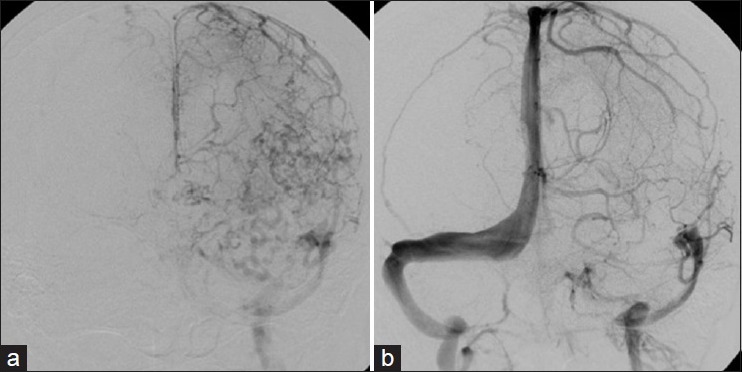
(a) Preoperative left internal carotid angiogram showing severe venous flow impairment. Markedly dilated cortical veins were observed, the cerebral blood flow narrowly returned through either the superficial middle cerebral vein or the vein of Labbe and retrograde venous drainage due to dural arteriovenous fistula was noted. (b) Angiogram obtained 12 months after sinus reconstruction showing a remarkable improvement in the cerebral venous return. The treated right sigmoid sinus was patent
Figure 2.
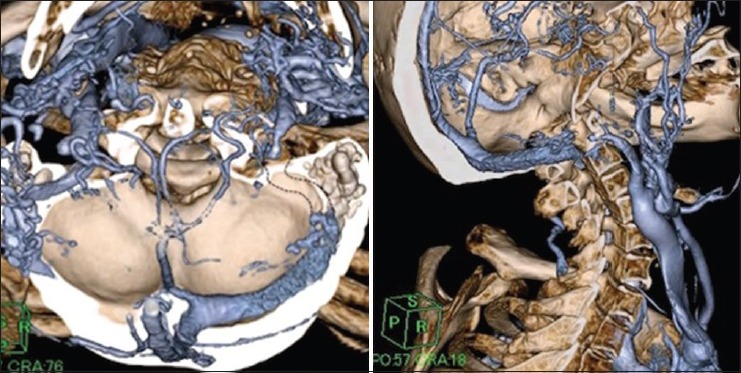
Preoperative computed tomography venography precisely showing occlusive part of the right sigmoid sinus. The dotted lines indicate the presumed occluded sinus. The white asterisk indicates the partially thrombosed right jugular bulb
The endovascular procedure was performed under general anesthesia. Bilateral groin access was used. A 4-French diagnostic catheter was advanced into the right external carotid artery to obtain the diagnostic angiograms and roadmaps. An 8-French guiding catheter (Launcher; Medotronic Inc., Minneapolis, MN) was advanced into the right internal jugular vein, and a 0.035” guidewire (Radifocus; Terumo, Tokyo, Japan) over a 4-Fr diagnostic catheter was successfully penetrated through the occluded portion and advanced to the right transverse sinus. Subsequently, the Radifocus wire was replaced with a 0.014” micro guidewire (Chikai; Asahi intecc, Aichi, Japan), which was advanced to the superior sagittal sinus. Balloon angioplasties (Gateway 3 mm × 12 mm; Stryker Neurovascular, Fremont, CA) were repeatedly performed from the distal (closer to the torcula) to the proximal (further from the torcula) portion. A subsequent angiogram showed that antegrade venous flow was restored [Figure 3a], and an additional balloon angioplasty (Bandicoot RX 6 mm × 40 mm; Kaneka, Osaka, Japan) was performed at the lower part of the sigmoid sinus [Figure 3b]. Next, a self-expanding stent (Precise 8 mm × 40 mm; Codman, Raynham, MA) was deployed between the sigmoid sinus and jugular bulb, which resulted in complete restoration of the venous flow in the occluded right sigmoid sinus [Figure 3c]; the Cognard Type II DAVF was converted to a Type I. After stenting, cortical venous reflux had disappeared and only antegrade flow into right jugular bulb remained. Bilateral internal carotid angiograms showed a remarkable improvement in cerebral perfusion [Figure 4b]. After the treatment, the patient showed no complication or convulsion. She was discharged our hospital with independent gait 6 months after the treatment. Her cognitive function gradually improved with MMSE score improved 26 points at 12 months after the treatment. She received the aforesaid double antiplatelet therapy until 3 months after the stenting, but was continued on a single 75 mg dose of clopidogrel for 1-year.
Figure 3.
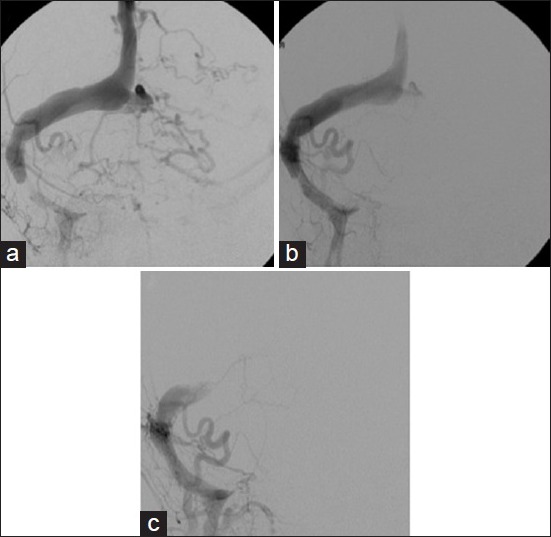
(a) Following preliminary balloon angioplasty, restoration of the antegrade venous flow was observed on a left external carotid angiogram. (b) Subsequent balloon angioplasty with a peripheral balloon catheter achieved a further improvement in the antegrade venous flow; however, the retrograde sinus flow persisted. (c) Next, a self-expanding stent was successfully deployed, and the retrograde venous flow completely disappeared; the Cognard Type IV dural arteriovenous fistula was converted to a Type I
DISCUSSION
Indications for reconstructive therapy
The TVE for TSS DAVFs is a widespread treatment option with high rates of safety and success.[5] However, this technique may not be suitable for a small proportion of patients who present with remarkable impairment in cerebral venous return due to multiple sinus occlusions and/or a restricted collateral venous outlet. The use of sinus packing in such patients can result in unexpected venous infarction or hemorrhage due to an inadequate collateral venous pathway, compensating for the sacrificed sinus.[8] Although transarterial onyx embolization has recently been suggested as a safe and effective treatment option to preserve patency of the affected sinus,[7] diffuse fistulae with multiple feeders, especially including dangerous anastomosis, causes considerable difficulty in the treatment. Sinus restoration for TSS DAVFs was first reported by Murphy et al.[13] Their case was similar to the present case in which the transverse sinus complicated by an ipsilateral sigmoid sinus occlusion, and the contralateral transverse sinus was either aplastic or occluded. Therefore, bilateral venous sinus occlusion induced remarkable venous reflux toward the straight and the superior sagittal sinuses. The above authors mechanically recanalized the affected sinus by balloon angioplasty, followed by stenting later due to acute occlusion of the treated sinus. After successful balloon angioplasty, the Type IV fistula was converted to a Type I fistula. Subsequently, several authors have reported and advocated the use of this novel technique, which is employed to treat not only advanced but also benign lesions (i.e. the affected sinus participates in the regulation of a normal venous return) [Table 1].[2,6,10,11]
Table 1.
Summary of reported TSS DAVF cases treated with venous stenting
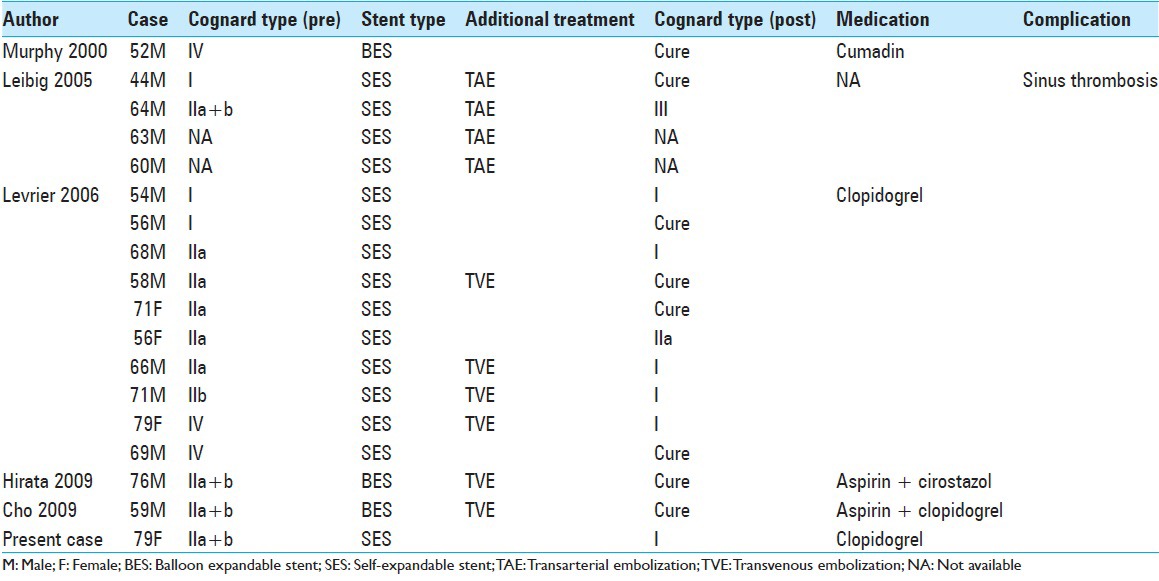
In these reports, almost all cases achieved either a complete cure or transition to a benign status. Liebig et al. reported the adverse events of subsequent occlusion of the stent, which resulted in clinical deterioration.[11] As demonstrated above, the use of sinus restoration for DAVFs is an effective alternative in cases with severe cerebral venous congestion due to multiple sinus occlusions; however, it has a potential risk for acute venous flow exacerbation due to acute stent occlusion.
Technical aspects of reconstructive therapy
Penetrating a chronically occluded sinus is challenging, even when the occluded segment is short. CT venography is more useful for precisely evaluating the length and configuration of the occluded region and predicting the feasibility of stenting than conventional angiography. In the present case, the angiogram showed opacity in the proximal portion of the occluded sinus. CT venography provided a definitive clue to perform the stenting. After penetrating the occluded sinus, using preliminary balloon angioplasty is recommended. Further navigation of the stent delivery system into stenotic venous sinuses is occasionally difficult because of the stiffness of these divided areas and the acute angle between the internal jugular vein and sigmoid sinus. Therefore, providing adequate support for the guiding system (e.g. using an 8- to 9-Fr guiding catheter) is preferable. To obtain adequate wall apposition and optimal position, the oversized self-expandable stent should be selected and deployed under the roadmap. With respect to the postoperative use of antithrombotic therapy to prevent stent thrombosis, the anticoagulant agent is preferred for peripheral venous stenting.[12] However, in the sinus restoration for TSS DAVFs, almost all authors selected antiplatelet agent (administered clopidogrel at the usual dose).[2,6,10] This medication was thereafter terminated between 3 months and 1-year after the initiation of treatment. In addition, Levrier et al. recommended the early postoperative use of the anticoagulation drug to avoid cortical vein thrombosis.[10]
CONCLUSION
Although the optimal treatment goal for DAVFs is the complete eradication of fistulae, occluded sinus restoration is preferable in patients with severe cerebral venous congestion due to multiple sinus occlusions and/or a restricted collateral venous outlet. CT venography is useful for precise evaluation of the length and configuration of the occluded segment, which thus make it possible to evaluate the feasibility of stenting.
Footnotes
Contributor Information
Koichiro Takemoto, Email: take9016@gmail.com.
Toshio Higashi, Email: toshi-higashi@pop13.odn.ne.jp.
Seisaburo Sakamoto, Email: ns.sanchan@hakujyujikai.or.jp.
Tooru Inoue, Email: toinoue@fukuoka-u.ac.jp.
REFERENCES
- 1.Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995;82:166–79. doi: 10.3171/jns.1995.82.2.0166. [DOI] [PubMed] [Google Scholar]
- 2.Choi BJ, Lee TH, Kim CW, Choi CH. Reconstructive treatment using a stent graft for a dural arteriovenous fistula of the transverse sinus in the case of hypoplasia of the contralateral venous sinuses: Technical case report. Neurosurgery. 2009;65:E994–6. doi: 10.1227/01.NEU.0000351772.45417.92. [DOI] [PubMed] [Google Scholar]
- 3.Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671–80. doi: 10.1148/radiology.194.3.7862961. [DOI] [PubMed] [Google Scholar]
- 4.Gutierrez A, Do HM, Marks MP. Alteration in the venous drainage of a dural arteriovenous fistula following angioplasty. AJNR Am J Neuroradiol. 2004;25:1086–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Halbach VV, Higashida RT, Hieshima GB, Mehringer CM, Hardin CW. Transvenous embolization of dural fistulas involving the transverse and sigmoid sinuses. AJNR Am J Neuroradiol. 1989;10:385–92. [PMC free article] [PubMed] [Google Scholar]
- 6.Hirata E, Higashi T, Iwamuro Y, Watanabe Y, Ando M, Arakawa Y, et al. Angioplasty and stent deployment in acute sinus thrombosis following endovascular treatment of dural arteriovenous fistulae. J Clin Neurosci. 2009;16:725–7. doi: 10.1016/j.jocn.2008.07.071. [DOI] [PubMed] [Google Scholar]
- 7.Ihn YK, Kim MJ, Shin YS, Kim BS. Dural arteriovenous fistula involving an isolated sinus treated using transarterial onyx embolization. J Korean Neurosurg Soc. 2012;52:480–3. doi: 10.3340/jkns.2012.52.5.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kallmes DF, Jensen ME, Cloft HJ, Kassell NF, Dion JE. Percutaneous transvenous coil embolization of a Djindjian type 4 tentorial dural arteriovenous malformation. AJNR Am J Neuroradiol. 1997;18:673–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Kirsch M, Liebig T, Kühne D, Henkes H. Endovascular management of dural arteriovenous fistulas of the transverse and sigmoid sinus in 150 patients. Neuroradiology. 2009;51:477–83. doi: 10.1007/s00234-009-0524-9. [DOI] [PubMed] [Google Scholar]
- 10.Levrier O, Métellus P, Fuentes S, Manera L, Dufour H, Donnet A, et al. Use of a self-expanding stent with balloon angioplasty in the treatment of dural arteriovenous fistulas involving the transverse and/or sigmoid sinus: Functional and neuroimaging-based outcome in 10 patients. J Neurosurg. 2006;104:254–63. doi: 10.3171/jns.2006.104.2.254. [DOI] [PubMed] [Google Scholar]
- 11.Liebig T, Henkes H, Brew S, Miloslavski E, Kirsch M, Kühne D. Reconstructive treatment of dural arteriovenous fistulas of the transverse and sigmoid sinus: Transvenous angioplasty and stent deployment. Neuroradiology. 2005;47:543–51. doi: 10.1007/s00234-005-1377-5. [DOI] [PubMed] [Google Scholar]
- 12.McBane RD, 2nd, Leadley RJ, Jr, Baxi SM, Karnicki K, Wysokinski W. Iliac venous stenting: Antithrombotic efficacy of PD0348292, an oral direct Factor Xa inhibitor, compared with antiplatelet agents in pigs. Arterioscler Thromb Vasc Biol. 2008;28:413–8. doi: 10.1161/ATVBAHA.107.158691. [DOI] [PubMed] [Google Scholar]
- 13.Murphy KJ, Gailloud P, Venbrux A, Deramond H, Hanley D, Rigamonti D. Endovascular treatment of a grade IV transverse sinus dural arteriovenous fistula by sinus recanalization, angioplasty, and stent placement: Technical case report. Neurosurgery. 2000;46:497–500. doi: 10.1097/00006123-200002000-00048. [DOI] [PubMed] [Google Scholar]


