Abstract
Participation in a screening program by itself may not improve clinical outcomes. Treatment gaps in the program may limit its full benefit. We evaluated statin prescription rates for subjects with sustained hypercholesterolemia to assess the treatment gaps in the National Health Screening Program (NHSP) in Korea. A retrospective, random cohort was established among National Health Insurance Corporation (NHIC) members. Finally, we examined 465,499 individuals who attended the NHSP from 2003 to 2010 without any history of dyslipidemia, statin prescription, or hospitalization for cardiovascular events until the end of 2002. The subsequent statin prescription rates were identified from the NHIC medical service claim database from 2003 to 2011. Descriptive data and odds ratio from multivariate logistic analyses on statin prescription rates and the corresponding correlations were evaluated. The NHSP detected 114,085 (24.5%) cases of newly diagnosed hypercholesterolemia. However, only 8.6% of these received statin prescription within 6 months of diagnosis. For cases of sustained hypercholesterolemia determined in the next screening visit by the NHSP, the statin prescription rate increased, but only to 12.2%. Statin prescriptions were more common among females, older individuals, and hypertension or diabetes patients. Furthermore, the statin prescription rates had increased over the study period. The NHSP exhibited low statin prescription rate which has been improving. For the NHSP to be effective, it would be worthwhile to decrease the gap between the diagnosis of hypercholesterolemia and the following treatment.
Graphical Abstract
Keywords: Hypercholesterolemia, Cholesterol, Cardiovascular Diseases, Prevention, Statins
INTRODUCTION
Hypercholesterolemia is a well-established risk factor for cardiovascular disease (CVD), and accounts for 4.5% of all-cause mortality worldwide (1). Furthermore, it is a risk factor that can be modified by therapeutic lifestyle changes (TLC) and lipid-lowering agents (2,3). Among the available lipid-lowering therapies, statins represent a cost-effective tool for the primary prevention of coronary heart disease (4,5), and can reduce the relative risk of major vascular events by 20% for each 1 mM/L reduction in low density lipoprotein (LDL) (6).
The National Cholesterol Expert Panel (NCEP) recommends screening for dyslipidemia in individuals from the age of 20 yr and initiating lipid-lowering medication in cases where the therapeutic goal is not reached within 12 weeks of TLC. The United States Preventive Services Task Force (USPSTF) and European Society of Cardiology (ESC) similarly support screening and therapeutic intervention for dyslipidemia. Based on these recommendations, many countries are conducting national screening programs for dyslipidemia, including Japan, Korea, United Kingdom, and the United States. In Korea, the National Health Insurance Corporation (NHIC) introduced an examination for hypercholesterolemia in the biennial National Health Screening Program (NHSP) in 1995.
However, previous studies have shown that the invitation of patients for health checks failed to improve total mortality or cardiovascular mortality (7), and that for a screening program to be effective in clinical settings, appropriate therapeutic interventions should be employed (8). In usual medical practice, compliance of patients following the prescription of lipid-lowering therapy is known to be poor (9). However, only few empirical studies have investigated the follow-up practices after population screening regarding appropriate prescription of lipid lowering agents when patients are detected with hypercholesterolemia.
The number of statin prescriptions written can be a strong surrogate marker of effective clinical intervention for hypercholesterolemia, because statins are the most frequently prescribed (87%) lipid-lowering agents (10). Therefore, we analyzed the statin prescription rate for newly diagnosed hypercholesterolemia and sustained hypercholesterolemia patients identified by the national screening program as the primary outcome. We also analyzed factors associated with statin prescription rates, to examine the patients at risk of not receiving effective treatment in spite of having sustained hypercholesterolemia.
MATERIALS AND METHODS
NHSP in Korea
Screening for hypercholesterolemia is a part of the NHSP. The NHSP is a population-based health-screening program provided biennially by the Korean NHIC, a universal healthcare payer covering nearly the whole Korean population (96.9%). The participation rate in the NHSP was 48% in 2003 and increased to 73% in 2011. The NHIC directly invites the subjects to participate in the program and afterwards informs them about the test results. During the process, subjects are to choose for themselves which medical center or clinic they wish to get their screening tests done and receive the necessitated management from.
Data sources
This study is based on the insurance registry database of NHIC members, their NHSP data, and the Korean National Health Insurance (NHI) medical service claims data. The NHSP data provided information about serum cholesterol levels and health behaviors. The NHI medical service claims data provided information on medical history, including comorbid diseases and statin prescriptions.
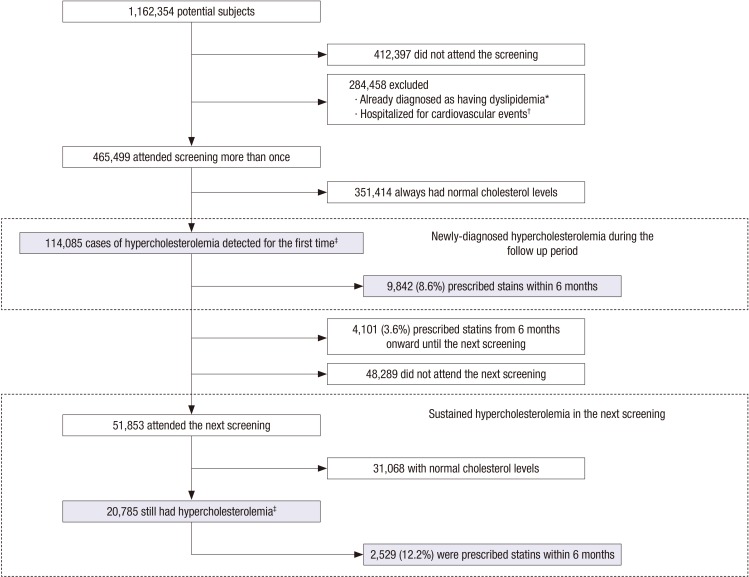
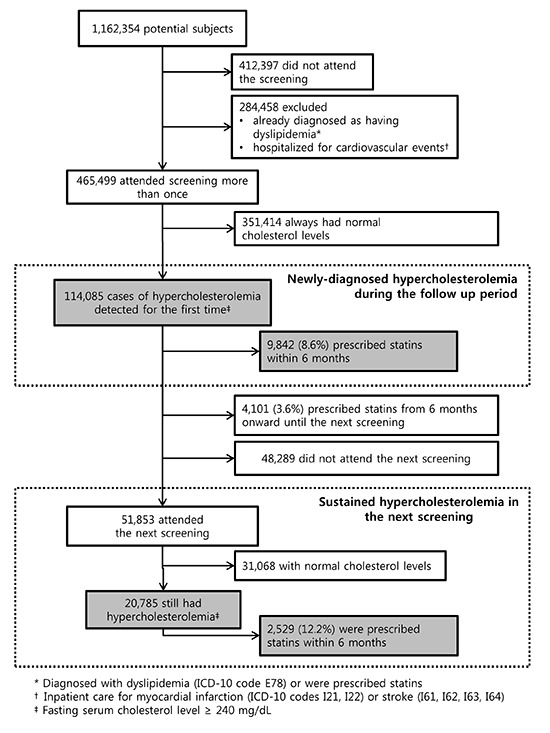
Study subjects
The potentially eligible subjects included 3% of the adults (>20 yr) who were selected randomly from the NHIC registry, as of December 31, 2002. They included 3% random sample of householders stratified by age and gender using the social security number and their household members. The follow-up period was up to 8 yr, through December 31, 2010. Among 1,162,354 eligible subjects, we excluded 412,397 subjects who did not participate in the screening program during the study period. We also excluded 284,458 subjects who were diagnosed with hypercholesterolemia, prescribed statins, or hospitalized for myocardial infarction (ICD-10 codes I21, I22) or stroke (I61, I62, I63, I64) before they first attended the NHSP. The number of subjects in the study population was 465,499 (Fig. 1).
Fig. 1. Flow chart of subjects. *Diagnosed with dyslipidemia (ICD-10 code E78) or were prescribed statins; †Inpatient care for myocardial infarction (ICD-10 codes I21, I22) or stroke (I61, I62, I63, I64); ‡Fasting serum cholesterol level ≥ 240 mg/dL.
Definitions and study outcome
Newly diagnosed hypercholesterolemia was considered when cases of hypercholesterolemia were diagnosed for the first time during the study period. Sustained hypercholesterolemia was defined as those with hypercholesterolemia in >2 consecutive screenings, each in 2 yr interval. To evaluate the clinical intervention rate in the NHSP strictly, we operationally defined the target population for statin treatment as cases with sustained hypercholesterolemia on the consecutive screening after the first diagnosis (newly diagnosed hypercholesterolemia) (Table 1). Hypercholesterolemia was defined as a total serum cholesterol concentration of ≥6.2 mM/L (≥240 mg/dL) (4). Serum cholesterol was tested in fasting conditions, and the level was measured using an enzymatic method. Quality control in each hospital was assured by the Korean Association of Laboratory Quality Control (11).
Table 1. Examples of cases of newly diagnosed hypercholesterolemia and sustained hypercholesterolemia.
| Cases | Year of examination | Interpretation | |||
|---|---|---|---|---|---|
| 2003-2004 | 2005-2006 | 2007-2008 | 2009-2010 | ||
| Case 1 | X | O | X | X | Newly diagnosed hypercholesterolemia in 2005-2006 but it was not sustained |
| Case 2 | X | X | X | O | Newly diagnosed hypercholesterolemia in 2009-2010 but it was not sustained |
| Case 3 | X | O | O | X | Newly diagnosed hypercholesterolemia in 2005-2006 and it was sustained in2007-2008 |
| Case 4 | X | O | X | O | Newly diagnosed hypercholesterolemia in 2005-2006 but it was not sustained |
| Case 5 | O | X | O | O | Newly diagnosed hypercholesterolemia in 2003-2004 but it was not sustained |
O: Serum cholesterol level ≥240 mg/dL. X: Serum cholesterol level <240 mg/dL or did not attend the National Health Screening Program.
Statin prescription was defined as the prescription of statins within 6 months after detection through the NHSP. The time limit of 6 months was set to measure the direct effect of NHSP, while considering the 12 weeks of TLS in the NCEP recommendation (4) as well as a cushion period. The prescription code included any form of statin listed in the claims data: atorvastatin, fluvastatin, pitavastatin, pravastatin, rosuvastatin, and simvastatin. Based on these definitions, we analyzed the statin prescription rate for newly diagnosed hypercholesterolemia and sustained hypercholesterolemia patients as the primary outcome measure.
Statistical analyses
Descriptive statistics were used to present data on the attendance for health-screening check-ups as well as statin prescription information. Among clinical characteristics of study subjects, Charlson comorbidity index (12) was calculated using the diagnosis for inpatient care from the KNHI medical service claims data. To evaluate the correlation between subject characteristics and statin prescription, a multivariate logistic model was constructed based on the univariate analyses of risk factors of coronary heart disease (CHD) (4) using the stepwise selection technique. In the final model, we calculated the odds ratio and 95% confidence intervals, adjusted for gender, age, comorbidities (hypertension and diabetes), smoking, and year of examination. We used STATA version 12.0 (StatCorp. Houston, TX, USA) to analyze the data, and the statistical significance was defined as P<0.05.
Ethics statement
This study was approved by the institutional review board of Seoul National University Hospital (IRB No. C-1206-055-414). Informed consent was exempted by the board.
RESULTS
Diagnosis of hypercholesterolemia and statin prescriptions
Among 465,499 subjects who attended the first screening visit of the NHSP and were not previously diagnosed with hypercholesterolemia, 114,085 subjects (24.5%) were newly diagnosed with hypercholesterolemia. Of these, 8.6% (n=9,842) were prescribed with statin within 6 months of the NHSP, and an additional 3.6% (n=4,101) were prescribed statins in the subsequent 6 months until the next NHSP screening.
Among the 100,142 subjects who had not been prescribed for a statin after their initial diagnosis of hypercholesterolemia, 51,853 (51.8%) attended the next NHSP screening and 20,785 of these subjects (40.1%) had sustained hypercholesterolemia. However, only 12.2% (n=2,529) of them were prescribed statin treatment within 6 months following the examination (Fig. 1).
Statin prescription after hypercholesterolemia by age, sex, and comorbidities
The statin prescription rate was higher among women than men for those aged ≥40 yr; this trend was not observed for those aged <40 yr. Considering CVD risk factors, people were prescribed statins more frequently if they were diagnosed as hypertension and aged from 20 to 59 yr old. Notably, male patients of all ages and female patients aged >40 yr, who had been diagnosed with diabetes, were most frequently prescribed with statins. The prescription rate was high in subjects with sustained hypercholesterolemia compared to subjects with newly diagnosed hypercholesterolemia regardless of gender or age (Table 2).
Table 2. Statin prescriptions in hypercholesterolemic subjects within the first 6 months after the NHSP.
| All ages | Age 20-39 yr | Age 40-59 yr | Age ≥60 yr | |||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | |
| After newly diagnosed hypercholesterolemia | ||||||||
| Total | n=60,093 | n=53,992 | n=20,328 | n=5,490 | n=30,492 | n=30,285 | n=9,273 | n=18,217 |
| No (%) treated | 3,739 (6.2) | 6,103 (11.30) | 486 (2.4) | 90 (1.6) | 2,230 (7.3) | 3,735 (12.3) | 1,023 (11.0) | 2,278 (12.5) |
| With hypertension* | n=18,535 | n=14,598 | n=4,843 | n=342 | n=9,663 | n=6,759 | n=4,029 | n=7,497 |
| No (%) treated | 1,352 (7.3) | 1,880 (12.9) | 156 (3.2) | 13 (3.8) | 789 (8.2) | 947 (14.0) | 407 (10.1) | 920 (12.3) |
| With diabetes* | n=6,151 | n=4,541 | n=1,063 | n=165 | n=3,593 | n=2,044 | n=1,495 | n=2,332 |
| No (%) treated | 628 (10.2) | 711 (15.7) | 52 (4.9) | 8 (4.9) | 381 (10.6) | 375 (18.4) | 195 (13.0) | 328 (14.1) |
| After sustained hypercholesterolemia in the next screening by NHSP | ||||||||
| Total | n=11,950 | n=8,835 | n=4,192 | n=592 | n=6,144 | n=4,860 | n=1,614 | n=3,383 |
| No (%) treated | 1,016 (8.5) | 1,513 (17.1) | 180 (4.3) | 36 (6.1) | 580 (9.4) | 883 (18.2) | 256 (15.9) | 594 (17.6) |
| With hypertension* | n=3,196 | n=2,121 | n=923 | n=34 | n=1,637 | n=934 | n=636 | n=1,153 |
| No (%) treated | 327 (10.2) | 421 (19.9) | 53 (5.7) | 4 (11.8) | 177 (10.8) | 205 (22.0) | 97 (15.3) | 212 (18.4) |
| With diabetes* | n=1,216 | n=759 | n=272 | n=20 | n=680 | n=342 | n=264 | n=397 |
| No (%) treated | 145 (11.9) | 171 (22.5) | 24 (8.8) | 2 (10.0) | 80 (11.8) | 88 (25.7) | 41 (15.5) | 81 (20.4) |
*Diagnosed with hypertension (ICD-10 codes I10-I15) or diabetes (ICD-10 codes E10-E14) in the National Health Insurance medical service claims data. NHSP, National Health Screening Program.
Factors associated with statin prescriptions in subjects with sustained hypercholesterolemia
Among 20,785 cases of sustained hypercholesterolemia, statin prescriptions correlated with female gender (adjusted odds ratio [aOR], 1.73; 95% CI, 1.40-2.15) and older age (aOR for age 40-59 yr, 2.13; 95% CI, 1.73-2.63; aOR for ages 60-79 yr, 2.55; 95% CI, 1.94-3.34). Past diagnoses of comorbidities were also important correlates, including hypertension (aOR, 1.41; 95% CI, 1.19-1.67) and diabetes (aOR, 1.26; 95% CI, 1.00-1.34). Above all, statin prescription rates were found to have increased in recent years (aOR for 2007-2008, 1.27; 95% CI, 1.13-1.43; aOR for 2009-2010, 1.70; 95% CI, 1.53-1.89) (Table 3).
Table 3. Factors associated with statin prescriptions for sustained hypercholesterolemia in the National Health Screening Program.
| Characteristics | Prescription for statins within 6 months | |||
|---|---|---|---|---|
| (n =20,785) | OR (95% CI) | aOR* (95% CI) | ||
| No (n=18,256) No (%) |
Yes (n=2,529) No (%) |
|||
| Sex | ||||
| Male | 10,934 (91.5) | 1,016 (8.5) | 1 (reference) | 1 (reference) |
| Female | 7,322 (82.9) | 1,513 (17.1) | 2.22 (2.04-2.42) | 1.58 (1.40-1.79) |
| Age (yr)† | ||||
| (mean±SD) | 49.76±12.62 | 54.96±10.40 | ||
| 20-39 | 4,568 (95.5) | 216 (4.5) | 1 (reference) | 1 (reference) |
| 40-59 | 9,541 (86.7) | 1,463 (13.3) | 3.24 (2.80-3.76) | 2.35 (2.00-2.75) |
| 60-79 | 4,147 (83.0) | 850 (17.0) | 4.33 (3.71-5.06) | 2.39 (2.00-2.85) |
| BMI (kg/m2) | ||||
| (mean±SD) | 24.87±3.09 | 24.82±2.96 | ||
| <17 | 40 (90.9) | 4 (9.1) | 0.70 (0.25-1.97) | N/A |
| 17-24 | 9,841 (87.6) | 1,397 (12.4) | 1 (reference) | N/A |
| ≥25 | 8,372 (88.1) | 1,126 (11.9) | 0.95 (0.87-1.03) | N/A |
| Missing data | 3 (60.0) | 2 (40.0) | N/A | N/A |
| CCI‡ | ||||
| (mean±SD) | 0.34±0.72 | 0.65±0.91 | ||
| 0 | 13,731 (90.5) | 1,436 (9.5) | 1 (reference) | 1 (reference) |
| 1 | 3,298 (82.3) | 709 (17.7) | 2.06 (1.86-2.27) | 1.70 (1.52-1.89) |
| 2 | 881 (76.5) | 271 (23.5) | 2.94 (2.54-3.41) | 2.34 (1.99-2.76) |
| ≥3 | 346 (75.4) | 113 (24.6) | 3.12 (2.51-3.89) | 2.20 (1.72-2.81) |
| Hypertension§ | ||||
| No | 13,687 (88.5) | 1,781 (11.5) | 1 (reference) | 1 (reference) |
| Yes | 4,569 (85.9) | 748 (14.1) | 1.26 (1.15-1.38) | 1.28 (1.26-1.42) |
| Diabetes§ | ||||
| No | 6,209 (89.3) | 744 (10.7) | 1 (reference) | 1 (reference) |
| Yes | 12,047 (87.1) | 1,785 (12.9) | 1.43 (1.26-1.62) | 1.26 (1.00-1.34) |
| Smoking | ||||
| None | 9,935 (86.0) | 1,622 (14.0) | 1 (reference) | 1 (reference) |
| Ex-smoker∥ | 1,983 (90.1) | 217 (9.9) | 0.67 (0.58-0.78) | 1.02 (0.86-1.21) |
| Smoker | 4,751 (92.5) | 387 (7.5) | 0.50 (0.44-0.56) | 0.89 (0.77-1.03) |
| Missing | 1,587 (84.0) | 303 (16.5) | N/A | N/A |
| Drinking problems¶ | ||||
| No | 5,789 (89.8) | 656 (10.2) | 1 (reference) | N/A |
| Yes | 3,233 (91.0) | 321 (9.0) | 0.88 (0.76-1.01) | N/A |
| Missing data | 9,234 (85.6) | 1,552 (14.4) | N/A | N/A |
| Year of examination | ||||
| 2003-2004 | N/A | N/A | N/A | N/A |
| 2005-2006 | 8,600 (90.0) | 953 (10.0) | 1 (reference) | 1 (reference) |
| 2007-2008 | 5,091 (87.4) | 736 (12.6) | 1.30 (1.18-1.45) | 1.27 (1.13-1.43) |
| 2009-2010 | 4,565 (84.5) | 840 (15.5) | 1.66 (1.50-1.83) | 1.70 (1.53-1.89) |
*Adjusted for gender, age, number of comorbidity, hypertension, diabetes, smoking, year of examination; †Age at the second hypercholesterolemia; ‡ICD-10 version of Charlson comorbidity index (12); §Diagnosed with hypertension (ICD-10 codes I10-I15) or diabetes (ICD-10 codes E10-E14) in the National Health Insurance medical service claims data; ∥Person who have quitted smoking at the time of screening test but ever smoked more than 100 tobacco cigarette; ¶Drinking problem: more than 14 units of alcohol per week for men; 10 units of alcohol per week for women. TC, serum total cholesterol; OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval; SD, standard deviation; BMI, body mass index; N/A, not available; CCI, Charlson comorbidity index.
DISCUSSION
To our knowledge, this is the first longitudinal report about the treatment gap observed in a population-based dyslipidemia screening program. It is an important issue because it could limit the full benefit of a prevention program for cardiovascular diseases (13). The strengths of our study include the use of a large database from a nationally representative sample, and the nearly complete follow-up for the primary outcome variable. The use of claim data for comorbidities and statin prescription details, rather than self-reported information, is another strength compared to other previous studies reporting prescription rates for dyslipidemia (14,15,16).
Although we designed a conservative study, only 12.2% of patients with sustained hypercholesterolemia were prescribed with statins within 6 months of the screening. This suggests that many patients with hypercholesterolemia do not receive appropriate clinical intervention despite their active participation in a consecutive health-screening program, indicating that the test results may not be suitably utilized for preventing CVD. Participants were more likely to be prescribed statins if they had established risk factors (4). This was the case if they were older, hypertensive, diabetic or middle-aged and older women. However, the prescription rates were <20% even for higher risk groups, such as older people, smokers, and those with diabetes or hypertension, although recent guidelines have recommended intensive statin treatment in such high risk groups (4).
Although the data may not be directly comparable, our results are in marked contrast to the statin prescription rates seen in the National Health Service (NHS) Health Check in the UK. In the first 2 yr of the NHS Health Check, statin prescription rates increased from 14.0% to 60.6% between the pre- and post-screening periods in groups at high risk of CVD (17). The discrepancy in the efficacy of NHS Health Check and NHSP could be due to the different degree of integration and the continuity of healthcare services. In the NHS Health Checks, the test is ordered and followed up by medical professionals who care for each patient at high risk (18). The cardiovascular disease screening by Medicare in the US adopts a similar process where the test is initiated by doctors or healthcare providers for their own patients (19). However, the NHSP is operated independently from the primary care physicians of individual patients. Physicians cannot browse nor follow up on the NHSP reports for their patients. In the NHSP, patients have to apply for the screening, receive the test report, and then seek medical advice by themselves.
Compliance with lipid-lowering therapy is usually poor (9). It has been reported that many patients were not concerned regarding their cholesterol level reports (20), were not aware of the desirable cholesterol levels (21,22), or did not understand its importance as a risk factor for CVD (22,23). In addition, patients often believe that TLC would be equally as effective at lowering cholesterol as statins (20) and often have concerns about the adverse effects of statins (20,24,25). Therefore, it is difficult to achieve appropriate treatment if the clinical follow up is left entirely to the patient. A promising finding was that the prescription rate increased from 10.0% to 15.5% during the study period of 8 yr. This finding agrees with the increasing trend of lipid-lowering drug use worldwide (5,14,15,26), although the prescription rate is still low in Korea, as reported in 2011 (27).
This study has several limitations. First, our study evaluated only the treatment gap in the NHSP. During the study period (median follow-up, 3.86 yr), we could not assess for a significant decrease in myocardial infarction and all-cause mortality using information on statin prescription within the first 6 months (data not shown). The effect of pharmacologic intervention rates on long-term clinical outcomes in every stage, such as the treatment rate, control rate, cardiovascular event, and cardiovascular mortality remains to be investigated. Second, in the present study, the criteria for statin prescriptions were based on serum total cholesterol level only, and not on the LDL or High Density Lipoprotein (HDL) levels that are used in clinical practice. In Korea, serum total cholesterol levels have been used as the conventional standard for prescribing statins for a long time (27), and during the study period, the National Health Insurance allowed insurance coverage for statin prescription based on the serum total cholesterol level. In a similar vein, the National Health-Screening Program tested only for serum total cholesterol levels until 2008. Although recent guidelines are focusing more on the LDL or HDL levels, we adopted the conventional standard during the study period for the fair evaluation of the follow-up practice during the same period. Meanwhile, the total cholesterol levels are good for predicting the risk of cardiovascular disease, compared to the new biomarkers (2,28). Moreover, statin prescription rates were still very low in high risk groups, suggesting that the conclusion of our study would be robust even with different criteria for statin treatment. Third, a comprehensive evaluation of interventions for dyslipidemia was not considered, as we had no information on the TLC. However, we overcame this limitation by using the criterion of statin prescription only in patients with sustained hypercholesterolemia. Fourth, the statin prescription rate may have been overestimated due to a selection bias, as participants in a health-screening program are more likely to be interested in their health and adhere to clinical follow-up.
In spite of these limitations, this study showed that a wide treatment gap is present in the NHSP in Korea, although it is improving. There has been remarkable development in lipid-lowering therapies, which can help in cases of sustained dyslipidemia (6). Considering the contrasting findings between NHSP and NHS Health Check, the real-world benefit and efficacy of screening programs can vary widely. Therefore, to reduce the cardiovascular disease burden, it would be worthwhile to decrease the treatment gap and to re-evaluate the clinical benefits of a health-screening program.
Footnotes
Funding: This research was supported by a fund from the Research of Korea Centers for Disease Control and Prevention (No. 2012E3302800).
DISCLOSURE: The authors declare no conflict of interest.
AUTHOR CONTRIBUTION: Conception of the study: Shin DW, Cho BL, Son KY. Acquisition of data: Cho BL, Yang HK. Statistical analysis: Ahn E, Yang HK. Manuscript preparation: Ahn E, Shin DW, Chun SH, Suh B. Manuscript approval: all authors.
References
- 1.World Health Organization. Global status report on noncommunicable diseases 2010. Geneva: World Health Organization; 2011. [Google Scholar]
- 2.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 3.Lee KH, Jeong MH, Ahn Y, Cho MC, Kim CJ, Kim YJ. New horizons of acute myocardial infarction: from the Korea Acute Myocardial Infarction Registry. J Korean Med Sci. 2013;28:173–180. doi: 10.3346/jkms.2013.28.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 5.Ebrahim S, Casas JP. Statins for all by the age of 50 years? Lancet. 2012;380:545–547. doi: 10.1016/S0140-6736(12)60694-1. [DOI] [PubMed] [Google Scholar]
- 6.Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590. doi: 10.1016/S0140-6736(12)60367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krogsbøll LT, Jørgensen KJ, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease. JAMA. 2013;309:2489–2490. doi: 10.1001/jama.2013.5039. [DOI] [PubMed] [Google Scholar]
- 8.Donabedian A. The quality of medical care. Science. 1978;200:856–864. doi: 10.1126/science.417400. [DOI] [PubMed] [Google Scholar]
- 9.Liberopoulos EN, Florentin M, Mikhailidis DP, Elisaf MS. Compliance with lipid-lowering therapy and its impact on cardiovascular morbidity and mortality. Expert Opin Drug Saf. 2008;7:717–725. doi: 10.1517/14740330802396984. [DOI] [PubMed] [Google Scholar]
- 10.Böhler S, Scharnagl H, Freisinger F, Stojakovic T, Glaesmer H, Klotsche J, Pieper L, Pittrow D, Kirch W, Schneider H, et al. DETECT-Study Group. Unmet needs in the diagnosis and treatment of dyslipidemia in the primary care setting in Germany. Atherosclerosis. 2007;190:397–407. doi: 10.1016/j.atherosclerosis.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 11.Cho HI. Twenty-years of experiences in external quality assurance in Korea. Southeast Asian J Trop Med Public Health. 1999;30:32–38. [PubMed] [Google Scholar]
- 12.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57:1288–1294. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Pearson T, Kopin L. Bridging the treatment gap: improving compliance with lipid-modifying agents and therapeutic lifestyle changes. Prev Cardiol. 2003;6:204–211. doi: 10.1111/j.1520-037x.2003.02633.x. [DOI] [PubMed] [Google Scholar]
- 14.Primatesta P, Poulter NR. Lipid concentrations and the use of lipid lowering drugs: evidence from a national cross sectional survey. BMJ. 2000;321:1322–1325. doi: 10.1136/bmj.321.7272.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation. 2003;107:2185–2189. doi: 10.1161/01.CIR.0000066320.27195.B4. [DOI] [PubMed] [Google Scholar]
- 16.Goff DC, Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, Psaty BM. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006;113:647–656. doi: 10.1161/CIRCULATIONAHA.105.552737. [DOI] [PubMed] [Google Scholar]
- 17.Artac M, Dalton AR, Majeed A, Car J, Millett C. Effectiveness of a national cardiovascular disease risk assessment program (NHS Health Check): results after one year. Prev Med. 2013;57:129–134. doi: 10.1016/j.ypmed.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 18.National Health Service (UK) What is NHS Health Check. [accessed on 30 January 2015]. Available at http://www.nhs.uk/Planners/NHSHealthCheck/Pages/NHSHealthCheckwhat.aspx.
- 19.Centers for Medicare and Medicaid Services (US) Your guide to Medicare's preventive services. 4th ed. Baltimore, MD: Centers for Medicare & Medicaid Services, US Department of Health and Human Services; 2011. [Google Scholar]
- 20.Aung TH, Go YY, Low LP, Chua T. Public perceptions, knowledge and awareness of cholesterol management in Singapore: a prospective pilot study. Singapore Med J. 2013;54:32–35. doi: 10.11622/smedj.2013008. [DOI] [PubMed] [Google Scholar]
- 21.Choi EJ, Jekal Y, Kim S, Yoo JS, Kim HS, Oh EG, Jeon JY, Jang Y, Chu SH, Kim MJ. Middle-aged women's awareness of cholesterol as a risk factor: results from a national survey of Korean Middle-aged Women's Health Awareness (KomWHA) study. Int J Nurs Stud. 2010;47:452–460. doi: 10.1016/j.ijnurstu.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Nash IS, Mosca L, Blumenthal RS, Davidson MH, Smith SC, Jr, Pasternak RC. Contemporary awareness and understanding of cholesterol as a risk factor: results of an American Heart Association national survey. Arch Intern Med. 2003;163:1597–1600. doi: 10.1001/archinte.163.13.1597. [DOI] [PubMed] [Google Scholar]
- 23.Kandula NR, Tirodkar MA, Lauderdale DS, Khurana NR, Makoul G, Baker DW. Knowledge gaps and misconceptions about coronary heart disease among U.S. South Asians. Am J Prev Med. 2010;38:439–442. doi: 10.1016/j.amepre.2009.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kon RH, Russo MW, Ory B, Mendys P, Simpson RJ., Jr Misperception among physicians and patients regarding the risks and benefits of statin treatment: the potential role of direct-to-consumer advertising. J Clin Lipidol. 2008;2:51–57. doi: 10.1016/j.jacl.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Tolmie EP, Lindsay GM, Kerr SM, Brown MR, Ford I, Gaw A. Patients' perspectives on statin therapy for treatment of hypercholesterolaemia: a qualitative study. Eur J Cardiovasc Nurs. 2003;2:141–149. doi: 10.1016/S1474-5151(03)00028-8. [DOI] [PubMed] [Google Scholar]
- 26.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140:226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 27.Ministry of Health and Welfare (KR); Korea Centers for Disease Control and Prevention. 2011 National Health Statistics: the fifth Korea National Health and Nutrition Examination Survey, 2010-2012. Seoul: Ministry of Health and Welfare; 2012. p. 432. [Google Scholar]
- 28.Ingelsson E, Schaefer EJ, Contois JH, McNamara JR, Sullivan L, Keyes MJ, Pencina MJ, Schoonmaker C, Wilson PW, D'Agostino RB, et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. 2007;298:776–785. doi: 10.1001/jama.298.7.776. [DOI] [PubMed] [Google Scholar]