Abstract
Cardiac arrest (CA) in children is associated with high mortality rates. In Korea, cohort studies regarding the outcomes of pediatric CAs are lacking, especially in emergency departments (EDs) or in-hospital settings. This study was conducted to examine the trends in epidemiology and survival outcomes in children with resuscitation-attempted CAs using data from a cross-sectional, national, ED-based clinical registry. We extracted cases in which cardiopulmonary resuscitation and/or manual defibrillation were performed according to treatment codes using the National Emergency Department Information System (NEDIS) from 2008 to 2012. The total number of ED visits registered in the NEDIS during the 5-yr evaluation period was 20,424,530; among these, there were 2,970 resuscitation-attempted CAs in children. The annual rates of pediatric CAs per 1,000 ED visits showed an upward trend from 2.81 in 2009 to 3.62 in 2012 (P for trend = 0.045). The median number of estimated pediatric CAs at each ED was 7.8 (25th to 75th percentile, 4 to 13) per year. The overall rates for admission survival and discharge survival were 35.2% and 12.8%, respectively. The survival outcome of adults increased substantially over the past 5 yr (11.8% in 2008, 11.7% in 2010, and 13.6% in 2012; P for trend = 0.001); however, the results for children did not improve (13.6% in 2008, 11.4% in 2010, and 13.7% in 2012; P for trend = 0.870). Conclusively, we found that the overall incidence of pediatric CAs in EDs increased substantially over the past 5 yr, but without significantly higher survival outcomes.
Graphical Abstract
Keywords: Pediatrics; Heart Arrest; Resuscitation; Outcome; Emergency Service, Hospital
INTRODUCTION
Cardiac arrest (CA) in children is a relatively infrequent event; however, it is often associated with death or a poor neurological outcome (1,2,3). Previous researchers have reported survival rates in children ranging from 9% to 47% after in-hospital cardiac arrest (IHCA) and from 0% to 29% after out-of-hospital cardiac arrest (OHCA) (4). Despite ongoing efforts to improve the quality of pediatric resuscitation, improvements in the survival rates of children with resuscitated CAs remains unknown. In the United States and Japan, studies with a large sample size and a high evidence level have been reported using nationwide hospital registries for out-of-hospital, in-hospital, and emergency department settings. In Korea, the annual incidence of pediatric CA and resuscitated intervention has increased over time. However, cohort studies of pediatric CA outcomes are rare, especially for in-hospital or emergency department (ED) settings (5). These studies were small, retrospective case series conducted in single hospitals, operating rooms, or intensive care units (ICU); therefore, future studies for understanding the pattern in a large sample of pediatric CAs are required (6,7).
The CA outcomes have been divided into OHCA and IHCA in previous epidemiologic and prognostic studies. The ED is an important entry to hospital-based emergent care for acutely- and critically-ill children. Furthermore, advanced life support (ALS) is initiated at the EDs in Korea and acts as a window between OHCA and IHCA; therefore, some characteristics of CAs in EDs tend to compound OHCA and IHCA. Nadkarni et al. reported that pediatric CAs in EDs accounted for 14% of IHCA (8). Due to the special situation of CAs in EDs, some researchers have recently studied CAs using the Nationwide Emergency Department Sample data in the United States (9).
Despite important concerns, little is known about CAs in Korean EDs (10). The objective of this study was to determine the characteristics of pediatric CAs in a nationwide ED setting. We extracted cases in which cardiopulmonary resuscitation (CPR) and/or manual defibrillation were performed according to treatment codes of the National Emergency Department Information System (NEDIS) from 2008 to 2012. To address the existing status of pediatric CAs, we examined the trends in epidemiologic characteristics and survival outcomes in children with resuscitated CAs in EDs using data from a cross-sectional, national ED-based registry.
MATERIALS AND METHODS
NEDIS database
Data were obtained from the NEDIS database, which is updated in real time by the National Emergency Medical Center (NEMC). The database was developed in 2004. Its quality control, feedback, and evaluation systems regarding emergency patients' registration information were established in 2006 and 2007. We obtained official permission to use the extracted the NEDIS data set from the NEMC. This information included patients' demographic characteristics, clinical parameters, ED diagnosis codes, core treatment parameters, patient disposition, and primary basic information regarding quality monitoring (11). As of 2012, all 23 level I regional centers and all 113 level II local centers had participated in the NEDIS project, accounting for more than 48.5% of the national overall ED census (Table 1). All patient-related information was automatically transferred from each hospital to a central government server within 2 or 14 days of the patient's discharge from an ED or hospital ward, respectively. Inaccurate data were filtered by a data processing system. The health authority maintains an accuracy assessment system and annually reports the results to the Ministry of Health and Welfare.
Table 1. Characteristics of the National Emergency Department Information System participants and the national emergency census in Korea.
| Year | Total | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|
| Pediatric subgroup in NEDIS | ||||||
| Pediatric, subtotal, No. | 6,692,840 | 990,686 | 1,330,117 | 1,374,105 | 1,418,582 | 1,579,350 |
| Infants ( < 1 yr) | 879,794 | 149,068 | 155,318 | 178,566 | 191,489 | 205,353 |
| Children (1-11 yr) | 4,067,845 | 600,458 | 785,026 | 855,750 | 856,553 | 970,058 |
| Adolescents (12-19 yr) | 1,745,201 | 241,160 | 389,773 | 339,789 | 370,540 | 403,939 |
| Pediatric CAs in EDs, No. | 2,970 | 510 | 436 | 600 | 680 | 744 |
| Infants ( < 1 yr) | 933 | 175 | 118 | 193 | 209 | 238 |
| Children (1-11 yr) | 944 | 172 | 122 | 183 | 207 | 260 |
| Adolescents (12-19 yr) | 1093 | 163 | 196 | 224 | 264 | 246 |
| CAs in EDs per 1,000 pediatric visits | 3.38 | 3.42 | 2.81 | 3.36 | 3.55 | 3.62 |
| Overall NEDIS database* (all ages) | ||||||
| ER visits in the NEDIS database, No. | 20,424,530 | 3,107,527 | 3,818,466 | 4,098,110 | 4,429,535 | 4,970,892 |
| National hospital-based census* | ||||||
| Total ER visits in Korea, No. | 50,522,478 | 8,905,766 | 10,814,628 | 10,232,016 | 10,327,028 | 10,243,040 |
| NEDIS: national ER census ratio | 40.4% | 34.9% | 35.3% | 40.1% | 42.9% | 48.5% |
*Data source: 2008-2012 Yearbook of Emergency Medical Statistics (reference: http://www.nemc.or.kr/). CA, cardiac arrest; ED, emergency department; ER, emergency room; NEDIS, National Emergency Department Information System.
Study population and variables
Our target was to record all cases of attempted CPR that began or continued in EDs upon arrival with OHCA (9,12). Data for CPR-attempted CAs in EDs were extracted by the NEDIS. We used the following data from 2008 to 2012: 1) cardiac compression and/or manual defibrillation as treatment codes in the ED,2) the ICD-10 code for CAs (I490-I469, I490, R02) in any disease field, and 3) the main symptom or diagnosis of CA, respiratory arrest, ventricular fibrillation (VF), or pulseless ventricular tachycardia (pVT) (9,13). Cases involving death on arrival, do-not-attempt resuscitation, or pre-hospital return of spontaneous circulation were excluded.
The following variables were analyzed: patient and peri-event characteristics (i.e., sex and age [infants < 1 yr, children 1-11 yr, and adolescents 12-19 yr]), etiology (i.e., disease or injury), whether the ED diagnosis was shockable arrhythmia (i.e., VF or pVT) or if the event occurred during night duty (i.e., 11:00 PM to 07:59 AM), the admission day (i.e., weekday or weekend, and the day of the week), and the month of year (14,15,16).
Primary and secondary outcomes
The primary outcomes were estimated incidence and survival outcomes at admission and discharge. To understand which circadian, weekly, and monthly variations were associated with a temporal improvement in survival, we examined trend analysis as the secondary outcome (17,18).
Statistical analysis
The overall resuscitated pediatric CAs in EDs from January 1, 2008 to December 31, 2012 were analyzed using IBM SPSS Statistics version 21.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were presented as medians and interquartile ranges (IQR; 25th and 75th percentiles). Categorical variables were presented as numbers and percentages. Chi-square or Mann-Whitney tests were performed during the univariate analysis of the survival outcomes. The annual changes from 2008 to 2012 were tested using a linear-by-linear association and expressed as a P value for the trend (19). All statistical tests were two-tailed, and P values <0.05 were considered statistically significant.
Ethics statement
The study was reviewed and approved by the institutional review board of Kyungpook National University Hospital (KNUH 201408006). Informed consent was waived by the board.
RESULTS
Demographic characteristics
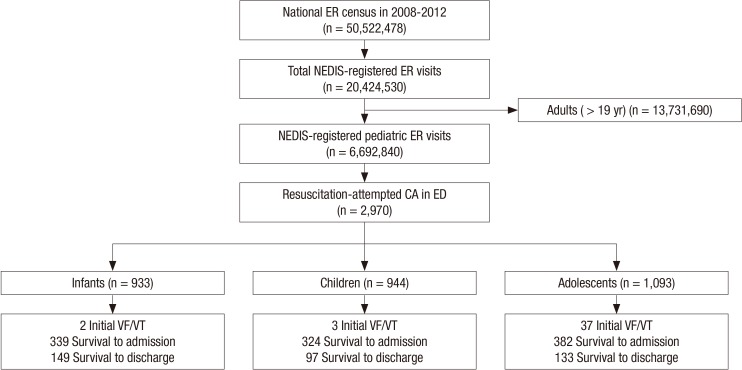
The total number of emergency visits, registered in the NEDIS from 2008 to 2012, was 20,424,530. Among these, the total number of pediatric cases was 6,692,840, of which 2,970 cases received CPR in an ED, an average of 594 visits per year (Fig. 1). These visits represented 0.34% of all pediatric ED visits over the period (rate 3.38 per 1,000 ED visits, 95% confidence interval [CI]: 3.37-3.39). The annual rates of pediatric CAs per 1,000 ED visits showed an upward trend from 2.81 in 2009 to 3.62 in 2012 (P for trend=0.045; Table 1).
Fig. 1. Patient flow according to the National Emergency Department Information System database determined based on resuscitated pediatric cardiac arrests in the emergency department. ER, emergency room; NEDIS, National Emergency Department Information System; CA, cardiac arrest; VT, ventricular tachycardia; VF, ventricular fibrillation.
The median number of pediatric CAs in the ED at each hospital was 39 (25th to 75th percentile, IQR, 20 to 64). For estimated annual incidence, the median number of case at each hospital per year was 7.8 (IQR, 4 to 13). The maximal and minimal numbers of registered cases were 130 and 1, respectively.
Regarding age groups, 31.4% of the cases were infants and 36.8% were adolescents. Furthermore, 63.3% of the cases were male. The frequency of cases in which the ED diagnosis was pVT or VF was 2.8%; the frequency of cases in which the cause of CA was trauma, poisoning, or other injuries was 37.4%; and the frequency of cases during night duty (11:00 PM to 07:59 AM) was 33.3%. Public ambulance services were used in 59.7% of the ED cases. The characteristics of the overall and annual resuscitated pediatric CAs in EDs are shown in Table 2.
Table 2. Trend of pediatric-resuscitated cardiac arrests in emergency departments.
| Variables | Overall (n=2,970) | 2008 (n=510) | 2009 (n=436) | 2010 (n=600) | 2011 (n=680) | 2012 (n=744) | P for trend |
|---|---|---|---|---|---|---|---|
| Prevalence (per 1,000 ED visits) | 3.38 | 3.42 | 2.81 | 3.36 | 3.55 | 3.62 | 0.045 |
| Demographics, No. (%) | |||||||
| Age, median (IQR) | 5 (0-15) | 4 (0-14) | 8 (0-16) | 6 (0-15) | 7 (0-16) | 4 (0-14) | |
| Infants (<1 yr) | 933 (31.4) | 175 (34.3) | 118 (27.1) | 193 (32.2) | 209 (30.7) | 238 (32.0) | 0.737 |
| Children (1-11 yr) | 944 (31.8) | 172 (33.7) | 122 (28.0) | 183 (30.5) | 207 (30.4) | 260 (34.9) | |
| Adolescents (12-19 yr) | 1,093 (36.8) | 163 (32.0) | 196 (45.0) | 224 (37.3) | 264 (38.8) | 246 (33.1) | |
| Sex, male | 1,879 (63.3) | 321 (62.9) | 277 (63.5) | 383 (63.8) | 428 (62.9) | 471 (63.2) | 0.969 |
| Event time, No. (%) | |||||||
| Night, 11 PM-8 AM | 981 (33.0) | 150 (29.4) | 124 (28.4) | 213 (35.5) | 217 (31.9) | 277 (37.2) | 0.002 |
| Weekend | 875 (29.5) | 147 (28.8) | 115 (26.4) | 182 (30.3) | 215 (31.6) | 216 (29.0) | 0.423 |
| Etiology of cardiac arrest, No. (%) | |||||||
| Shockable rhythm (VF/pVT) | 84 (2.8) | 6 (1.2) | 10 (2.2) | 20 (3.4) | 20 (3.0) | 28 (3.8) | 0.063 |
| Medical disease progression | 1,857 (62.6) | 315 (62.0) | 237 (54.5) | 374 (62.4) | 452 (66.5) | 479 (64.4) | 0.012 |
| Trauma, poisoning, other injuries | 1,109 (37.4) | 193 (38.0) | 198 (45.5) | 225 (37.6) | 228 (33.5) | 265 (35.6) | 0.012 |
| Transport by public ambulance | 1,774 (59.7) | 269 (52.7) | 262 (60.1) | 337 (56.2) | 423 (62.2) | 483 (64.9) | <0.001 |
| Survival outcomes, No. (%)* | |||||||
| Survival at admission | 1,045 (35.2) | 192 (37.8) | 155 (35.6) | 185 (30.9) | 243 (35.7) | 270 (36.3) | 0.823 |
| Survival at discharge | 379 (12.8) | 69 (13.6) | 55 (12.6) | 68 (11.4) | 85 (12.5) | 102 (13.7) | 0.870 |
Data are shown as the number of events (column percentage). *Unknown or undetermined data: survival admission analysis (Year 2008 [n=2], Year 2010 [n=2]) and survival discharge analysis (Year 2008 [n=3], Year 2010 [n=2]). ED, emergency department; IQR, interquartile range; pVT, pulseless ventricular tachycardia; VF, ventricular fibrillation.
Survival outcomes
The overall rates for admission survival and discharge survival were 35.2% and 12.8%, respectively (Table 2). Among admitted patients, 149/339 (44.0%) infants, 97/324 (29.9%) children, and 133/382 (34.8%) adolescents survived at discharge (Fig. 1).
Of hospital factors, a greater survival at discharge was observed in hospitals located in the metropolitan area (odds ratio [OR], 1.41; 95% CI, 1.11-1.79, P=0.005) and hospitals with higher annual CPR volume (OR, 1.38; 95% CI, 1.06-1.87, P=0.034), but not high EMC levels (OR, 1.19; 95% CI, 0.92-1.53, P=0.179).
Circadian, weekly, and monthly variations
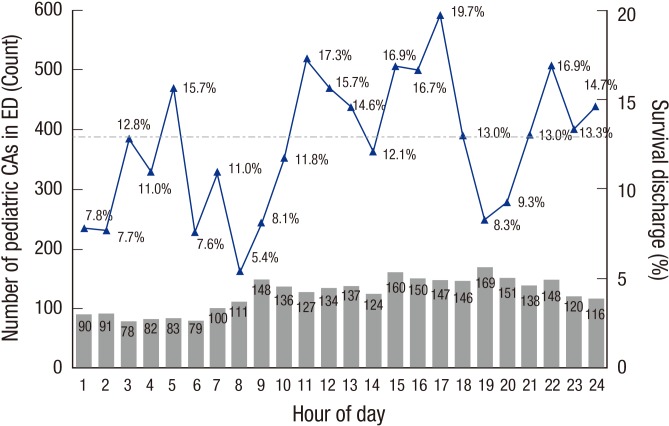
The circadian variation among all children with a CA in the ED is shown in Fig. 2. Bimodal incidence peaks (one in the late morning and one in the afternoon) was observed; however, there was a trough at 2 to 3 AM (n=78, 2.6%). The highest survival discharge rate was observed at 4 to 5 PM (29/147, 19.7%). Three lower troughs were detected at 7 to 8 AM (6/111, 5.4%), midnight to 2 AM (14/181, 7.7%), and 6 to 7 PM (14/169, 8.3%). The survival discharge rate was statistically different according to the hour of day (P=0.028).
Fig. 2. Circadian survival rhythm of pediatric cardiac arrests (CAs) in the emergency department (ED).
There was uniformity in the occurrence of CA by day of the week. The highest and lowest incidence rates were observed on Mondays (473 victims) and Tuesday (383 victims), respectively; however, the survival discharge rate was not significantly different (11.1% to 14.1%, P=0.863). The months with the highest and lowest survival outcome were June (41/228, 18.0%) and December (27/277, 9.7%), respectively; however, there was no significant difference in the monthly variations of pediatric resuscitation-attempted CAs in EDs (P=0.207).
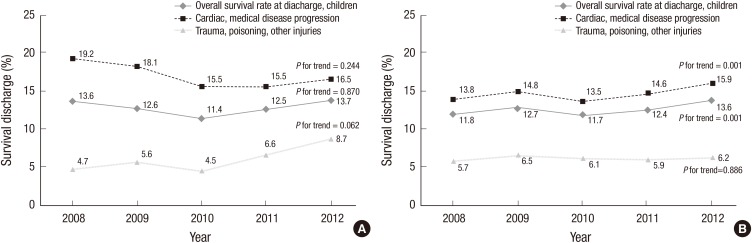
Comparison of survival outcome trends between children and adults
In children, the trend for the discharge survival rate was similar in the two etiology groups of sudden cardiac death (Fig. 3A). In adults, survival rates of medical caused-CAs increased over time (13.8% in 2008, 13.5% in 2010, and 15.9% in 2012; P for trend= 0.001; Fig. 3B). Survival outcomes did not improve in injury-induced CAs in both children and adults (P for trend=0.062 and 0.886). In adults, overall annual survival rates at discharge gradually improved significantly (11.8% in 2008, 11.7% in 2010, and 13.6% in 2012; P for trend=0.001; Fig. 3B); however, rates for children did not improve (13.6% in 2008, 11.4% in 2010, and 13.7% in 2012; P for trend=0.870; Fig. 3A).
Fig. 3. Trend plots of survival discharge in children (A) and adults (B) by calendar year. During the past 5 yr, the proportion of children survivors (overall, cardiac, and trauma group) did not improve (all P for trend > 0.05). However, the proportion of adult survivors (overall and non-traumatic group) increased over time (P for trend < 0.05).
DISCUSSION
Earlier studies of pediatric CAs were mostly focused on out-of-hospital settings. According to the Korea Center for Disease Control and Prevention surveys (the CAVAS project), the incidence rate of pediatric non-traumatic OHCA in Korea was 4.2 per 100,000 person-years, with a survival rate of 4.9% from 2006 to 2007 (5). However, studies relating to pediatric IHCA were retrospective and conducted at a single center with only a few years of data collection, thus precluding a trend analysis. Previous studies regarding pediatric CA were limited in location (OHCA vs. IHCA) or etiology (trauma vs. cardiac); moreover, most of those studies were conducted in the United States, Canada, Japan, and Europe (6,20). Therefore, there is need for multicenter studies involving a large sample of pediatric CAs in both in-hospital and ED settings in Korea. The present report represented a national ED-based observational study of pediatric resuscitations in Korea. We analyzed the epidemiology and survival trends of resuscitated pediatric outcomes in a nationwide ED setting.
The prevalence of IHCA in children ranges from 0.08% to 2.0% (21,22). The ED, which is among the first locations where advanced resuscitated managements are provided, acts as window between OHCA and IHCA in Korea. The ED was the second most common location of pediatric IHCAs (21). Among inpatients suffering from CAs, approximately 11%-15% patients had their original event in the ED (8,14). Using NEDIS dataset, we extracted nationwide data for CAs treated with ALS in EDs and analyzed the survival outcomes. From 2008 to 2012, 64,143 ALS interventions were attempted in EDs for patients of all ages. During the same period, 3.13 CAs per 1,000 visits were reported for ED patients of all ages (0.31%). Of these, 2,970 were performed on pediatric patients; therefore, the predicted proportion of resuscitation-attempted CAs was 3.38 cases per 1,000 pediatric ED visits (0.34%). According to our results, the annual incidence of pediatric CAs and resuscitated efforts have increased over time (P for trend=0.045). However, some annual data were underestimated (3.42 events per 1,000 pediatric ED visits in 2008 vs. 2.81 in 2009) because of an unusual surge of pediatric ED visits in 2009, mainly due to the pandemic influenza A.
Previous researchers have reported survival rates in children ranging 9% to 47% after IHCA and 0% to 29% after OHCA (4,22). In the present study of pediatric resuscitation-attempted CAs in EDs, the proportions of patients who were alive at hospitalization and survived at discharge were 35.2% and 12.8%, respectively. These rates were twice as high as those reported in a previous study using pediatric OHCA data in Korea (17.6% and 4.7%) (5). Considering the terms of CA in the ED, Kayser et al. reported a survival discharge of 22.8% for IHCAs in EDs in the United States, but a direct comparison with our study is difficult because it excluded resuscitation-attempted OHCAs in EDs (23). Out-of-hospital and in-hospital patients suffering CAs in EDs show a mixture of characteristics. Patients who visit the ED are usually presented with an acute or critical problem, and therefore, one might assume that their level of instability might predict a poorer outcome than other in-patients (11,23).
This was the first reported study with survival outcomes of pediatric CAs in EDs based on a nationwide database system in Korea. Various pre-arrest conditions and hospital factors potentially influencing the survival outcomes or physiological mechanism were not considered in this study because of the limited parameters of the NEDIS reports and the coding process of the Personal Information Protection Act. Therefore, we focused on the epidemiology and trend analysis rather than comparisons with other study outcomes. Understanding the epidemiology and trends is important because the presence of substantial variability would suggest an opportunity to improve pediatric outcomes after CAs (21). As reported in many previous OHCA studies, we demonstrated circadian variation in the incidence and survival rates of pediatric CAs in EDs (15,16). Similar to the Japanese OHCA data findings (17), there were bimodal peaks of incidence, with one in the late morning (8-9 AM) and one in the afternoon (6-8 PM). Pediatric CAs at midnight had a higher mortality than any other period. This is in agreement with recently published results (13,14,15,16), but not the results of the study by Nakanishi et al. (17). Conspicuously, children with CAs in EDs were vulnerable to survival at 7-8 AM and 6-7 PM, which are relevant to day-night work shifting times in most emergency rooms. Therefore, the present results suggest that endogenous (e.g., age, patient's disease, or etiology of CA) and exogenous (e.g., number of physicians and nurses, and level of emergency resources) factors may affect the outcomes. These factors should be addressed in future studies, which should include multivariate analysis of factor affecting survival outcomes. In-depth research studies considering all factors (hospital- and patient-related) and another qualified dataset (e.g. population-based analysis using the Health Insurance Review and Assessment Service data) should be conducted in the future.
One of the most influential patient-related factors is the initial shockable rhythm (8,24,25,26). In contrast, other studies report that certain shockable arrest rhythms are not associated with improved survival in children (21). The rate of VT/VF rhythm in children has been reported as 8.1% in a meta-analysis and 7%-9% in some population-based studies (5,8,26). A lower percentage of VF or pVT, ranging from 2% to 3% (5), has been reported in other pediatric OHCA studies. Among all subjects in our study, the VF/pVT subgroup was relatively small (2.8%). The discrepancies among these data may be due to the different definitions and study designs. The coding rhythm in the present study was different from the actual monitored electrocardiogram because shockable rhythms were estimated from the ICD-10 codes (VF and VT) or attempted manual defibrillation.
Despite increased survival rates after CA in other countries, trends for survival outcomes of pediatric CAs did not improve in Korea during the 5 yr (24). The overall rate of survival at discharge of resuscitated pediatric CAs in EDs was 12.8% compared with 12.5% for adults. According to the trend analysis, a survival rate of resuscitated adult CAs in EDs improved from 2008 to 2012; however, that of resuscitated pediatric CAs remained unchanged. Although development of medical facility and an extended CPR training program have been continued, these resources only affected adult survival outcomes of ALS-attempted CAs in EDs and not children. Pediatric CA patients constitute a relatively small patient population in the ED. On average, the rate of pediatric CAs in the United States was 15 in-hospital and 6 out-of-hospital arrests per hospital per year. Similarly in this study, the median number of pediatric CAs in the ED at each hospital was 7.8 cases per year in Korea, which can consequently lead to unfamiliarity regarding proper pediatric CA procedures among hospital staff (1).
Regionalization of healthcare means providing high-quality and cost-effective care for patients in critical conditions. Therefore, CA centers have been suggested as a strategy to improve survival outcomes (9). Regarding inter-hospital variability of post-CA mortality, several researchers have previously reported that CA patients treated at higher volume centers admitted to the ICU or ED per year were significantly less likely to die in the hospital (21,27). This provides support for regionalized CA care systems that include a designated high volume cardiac resuscitation center (16). Related hospital factors in the present study corresponded with the aforementioned studies in which a greater survival was reported in an urban location, a teaching hospital, a hospital with >20,000 ED visits, a hospital with emergent intervention capability, and hospitals with high OHCA volume EDs (9,16,27). Similar to previous studies, a greater survival at discharge was observed in hospitals located in the metropolitan area and hospitals that had higher annual CPR volume, but not EMC levels.
This study has several limitations. Firstly, although a nation-wide database was used, not all EDs in Korea were included. Pediatric resuscitation was not likely to be performed in locations with EDs below level III; therefore, we were able to identify a general trend for pediatric CAs using the NEDIS data, which included all level I and II EDs. Secondly, given the limited details of the NEDIS reports, data regarding long-term survival or neurologic status were not included in the analysis. Therefore, the final outcomes were determined at hospital discharge without 6-month survival and neurocognitive follow-up. However, previous researchers have indicated that survival outcome at discharge was not substantially different from status at 6 months and 1 yr post-arrest (28). Thirdly, we did not conduct subgroup analysis for OHCA and CAs that occurred in EDs. We were unable to separate the NEDIS dataset into OHCAs resuscitated in EDs and IHCA in EDs. Finally, it was difficult to compare CA characteristics over time with that of previous studies (CAVAS in Korea, Pediatric Emergency Care Applied Research Network, and Get With the Guidelines-Resuscitation Investigators group in the United States) because of differences in the inclusion criteria (e.g., including trauma victims) and definitions of CA (e.g., resuscitated with manual compression, adrenalines, and/or defibrillation) and the age of the pediatric group (e.g., less than 20 yr or 18 yr).
In conclusion, we found that the NEDIS-based nationwide incidence rate of resuscitated pediatric CAs in EDs was 3.38 per 1,000 ED visit per year. The overall rate of survival at discharge was 12.8%. In the trend analysis, the survival rate of resuscitated adult CAs in EDs improved from 2008 to 2012, but the survival rate of pediatric CA patients remained unchanged. Future studies are needed to determine the multidisciplinary hospital and patient factors responsible for improving CA survival in children.
Footnotes
DISCLOSURE: The authors have no conflicts of interest to declare.
AUTHOR CONTRIBUTION: Conception & design of the study: Lee MJ. Acquisition of data and statistical analysis: Ahn JY, Kim H, Lee MJ. Data review: Yoon HD, Jang HY. Manuscript preparation: Ahn JY, Lee MJ. Revised manuscript: Kim H, Lee MJ. Manuscript approval: all authors.
References
- 1.Woods WA. Pediatric resuscitation and cardiac arrest. Emerg Med Clin North Am. 2012;30:153–168. doi: 10.1016/j.emc.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 2.Young KD, Gausche-Hill M, McClung CD, Lewis RJ. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics. 2004;114:157–164. doi: 10.1542/peds.114.1.157. [DOI] [PubMed] [Google Scholar]
- 3.Herlitz J, Svensson L, Engdahl J, Gelberg J, Silfverstolpe J, Wisten A, Angquist KA, Holmberg S. Characteristics of cardiac arrest and resuscitation by age group: an analysis from the Swedish Cardiac Arrest Registry. Am J Emerg Med. 2007;25:1025–1031. doi: 10.1016/j.ajem.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Meert KL, Donaldson A, Nadkarni V, Tieves KS, Schleien CL, Brilli RJ, Clark RS, Shaffner DH, Levy F, Statler K, et al. Pediatric Emergency Care Applied Research Network. Multicenter cohort study of in-hospital pediatric cardiac arrest. Pediatr Crit Care Med. 2009;10:544–553. doi: 10.1097/PCC.0b013e3181a7045c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park CB, Shin SD, Suh GJ, Ahn KO, Cha WC, Song KJ, Kim SJ, Lee EJ, Ong ME. Pediatric out-of-hospital cardiac arrest in Korea: A nationwide population-based study. Resuscitation. 2010;81:512–517. doi: 10.1016/j.resuscitation.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Lee MJ. Incidence and outcome of cardiac arrest in Korea. J Korean Soc Emerg Med. 2012;23:168–180. [Google Scholar]
- 7.Kim WJ, Kim JJ, Jang JH, Hyun SY, Yang HJ, Lee G. Implementation of therapeutic hypothermia after pediatric out-of hospital cardiac arrest in one tertiary emergency center. Korean J Crit Care Med. 2013;28:25–32. [Google Scholar]
- 8.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, et al. National Registry of Cardiopulmonary Resuscitation Investigators. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 9.Johnson NJ, Salhi RA, Abella BS, Neumar RW, Gaieski DF, Carr BG. Emergency department factors associated with survival after sudden cardiac arrest. Resuscitation. 2013;84:292–297. doi: 10.1016/j.resuscitation.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 10.Cho H, Moon S, Park SJ, Han G, Park JH, Lee H, Choi J, Hwang S, Bobrow BJ. Out-of-hospital cardiac arrest: incidence, process of care, and outcomes in an urban city, Korea. Clin Exp Emerg Med. 2014;1:94–100. doi: 10.15441/ceem.14.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwak YH, Kim DK, Jang HY. Utilization of emergency department by children in Korea. J Korean Med Sci. 2012;27:1222–1228. doi: 10.3346/jkms.2012.27.10.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tunstall-Pedoe H, Bailey L, Chamberlain DA, Marsden AK, Ward ME, Zideman DA. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): methods and overall results. BMJ. 1992;304:1347–1351. doi: 10.1136/bmj.304.6838.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Valderrama AL, Fang J, Merritt RK, Hong Y. Cardiac arrest patients in the emergency department-National Hospital Ambulatory Medical Care Survey, 2001-2007. Resuscitation. 2011;82:1298–1301. doi: 10.1016/j.resuscitation.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, Meaney PA, Cen L, Nadkarni VM, Praestgaard AH, et al. National Registry of Cardiopulmonary Resuscitation Investigators. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 15.Ro YS, Shin SD, Song KJ, Lee EJ, Kim JY, Ahn KO, Chung SP, Kim YT, Hong SO, Choi JA, et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: a nationwide observational study from 2006 to 2010 in South Korea. Resuscitation. 2013;84:547–557. doi: 10.1016/j.resuscitation.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 16.Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80:30–34. doi: 10.1016/j.resuscitation.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Nakanishi N, Nishizawa S, Kitamura Y, Nakamura T, Matsumuro A, Sawada T, Matsubara H. Circadian, weekly, and seasonal mortality variations in out-of-hospital cardiac arrest in Japan: analysis from AMI-Kyoto Multicenter Risk Study database. Am J Emerg Med. 2011;29:1037–1043. doi: 10.1016/j.ajem.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim HJ, Kim KI, Cho YS, Kang J, Park JJ, Oh IY, Yoon CH, Suh JW, Youn TJ, Chae IH, et al. The effect of admission at weekends on clinical outcomes in patients with non-ST-segment elevation acute coronary syndrome and its contributing factors. J Korean Med Sci. 2015;30:414–425. doi: 10.3346/jkms.2015.30.4.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang HJ, Kim GW, Kim H, Cho JS, Rho TH, Yoon HD, Lee MJ NEDIS-CA Consortium. Epidemiology and outcomes in out-of-hospital cardiac arrest: a report from the NEDIS-based cardiac arrest registry in Korea. J Korean Med Sci. 2015;30:95–103. doi: 10.3346/jkms.2015.30.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jayaram N, Spertus JA, Nadkarni V, Berg RA, Tang F, Raymond T, Guerguerian AM, Chan PS American Heart Association's Get with the Guidelines-Resuscitation Investigators. Hospital variation in survival after pediatric in-hospital cardiac arrest. Circ Cardiovasc Qual Outcomes. 2014;7:517–523. doi: 10.1161/CIRCOUTCOMES.113.000691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zeng J, Qian S, Zheng M, Wang Y, Zhou G, Wang H. The epidemiology and resuscitation effects of cardiopulmonary arrest among hospitalized children and adolescents in Beijing: an observational study. Resuscitation. 2013;84:1685–1690. doi: 10.1016/j.resuscitation.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 23.Kayser RG, Ornato JP, Peberdy MA American Heart Association National Registry of Cardiopulmonary Resuscitation. Cardiac arrest in the Emergency Department: a report from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2008;78:151–160. doi: 10.1016/j.resuscitation.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS American Heart Association Get With the Guidelines-Resuscitation Investigators. Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6:42–49. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nagata T, Abe T, Noda E, Hasegawa M, Hashizume M, Hagihara A. Factors associated with the clinical outcomes of paediatric out-of-hospital cardiac arrest in Japan. BMJ Open. 2014;4:e003481. doi: 10.1136/bmjopen-2013-003481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RA Resuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ro YS, Shin SD, Song KJ, Park CB, Lee EJ, Ahn KO, Cho SI. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low- and high-resuscitation case volume. Resuscitation. 2012;83:855–861. doi: 10.1016/j.resuscitation.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 28.López-Herce J, García C, Rodríguez-Núñez A, Domínguez P, Carrillo A, Calvo C, Delgado MA Spanish Study Group of Cardiopulmonary Arrest in Children. Long-term outcome of paediatric cardiorespiratory arrest in Spain. Resuscitation. 2005;64:79–85. doi: 10.1016/j.resuscitation.2004.07.010. [DOI] [PubMed] [Google Scholar]