Abstract
An aneurysmal bone cyst (ABC) is a benign, locally proliferative vascular disorder of non-neoplastic osseous lesions in children and young adults. Seventy-five percent of ABCs occur before the age of 20 years. They comprise 1.4% of all primary bone tumors, and commonly occur in the long bones. Spinal ABCs are much rarer. We present to you one such rare case of ABC involving the lumbar spine which was successfully treated with surgery. The clinical pathological and radiological features are described. The treatment options available are discussed.
Keywords: Aneurysmal bone cyst, spinal stabilization, transpedicular approach, vertebral body tumors, winking owl sign
Introduction
An aneurysmal bone cyst (ABC) is a benign, locally proliferative vascular disorder of non-neoplastic osseous lesions in children and young adults. Seventy-five percent of ABCs occur before the age of 20 years. They comprise 1.4% of all primary bone tumors, and commonly occur in the long bones. Spinal ABCs are much rarer. We present to you one such rare case of ABC involving the lumbar spine which was successfully treated with surgery.
Case Report
A 17-year-old girl presented with one week history of severe localized lower back pain at fourth lumbar vertebral level which increases on lying supine. On examination, she had left dorsiflexion and EHL weakness of grade 4/5 with sensory impairment in left L5 dermatome. Local tenderness on palpation was present. Her bladder and bowel habits were normal. There was no previous history of trauma. X-rays showed osteolytic lesion involving the L4 vertebral body with winking owl sign on AP views [Figure 1a]. Computed tomography (CT) scan of lumbar spine with reconstruction showed lytic expansile lesion involving the L4 vertebral body and left pedicle [Figure 1b–e]. Magnetic resonance imaging (MRI) showed characteristic findings of aneurysmal bone cyst with multiple fluid-fluid levels [Figure 2a–d]. There was extension of the lesion into the spinal canal and pressure on the left sided nerve roots. She underwent left transpedicular approach and complete excision of the lesion followed by pedicle screw fixation. The lesion had a dark red fleshy appearance with moderate vascularity. The lesion was encasing the nerve root on the left side, which was carefully dissected and excised. Multiple blood filled cysts involving the L4 vertebral body were encountered. The tumor was totally extradural and was completely excised. Histopathology of the lesion showed uniformly distributed osteoclast type giant cells having multiple nuclei [Figure 3]. There were few cysts containing hemorrhage and were lined by histiocytes and osteoclast giant cells. These features were suggestive of secondary aneurysmal bone cyst.
Figure 1.

(a) X-ray AP view showing lytic lesion involving the L4 vertebral body with winking owl sign; (b) Lateral; (c and d) Axial section of lumbar spine CT scan with reconstruction; (e) Lytic expansile lesion involving the L4 vertebral body and left pedicle
Figure 2.
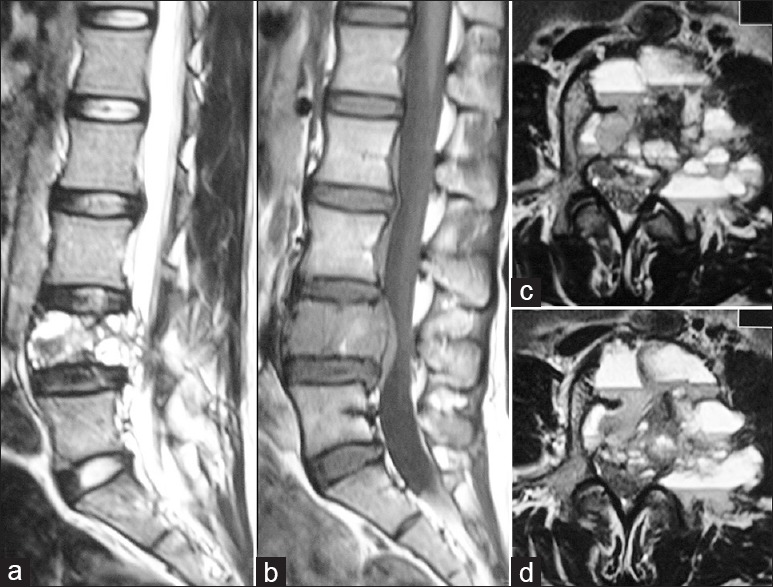
MRI scan of the lumbar spine sagittal T1 (a) and T2 (b) Weighted images and axial sections; (c and d) of T2 weighted images showing characteristic findings of aneurysmal bone cyst with multiple fluid-fluid levels
Figure 3.
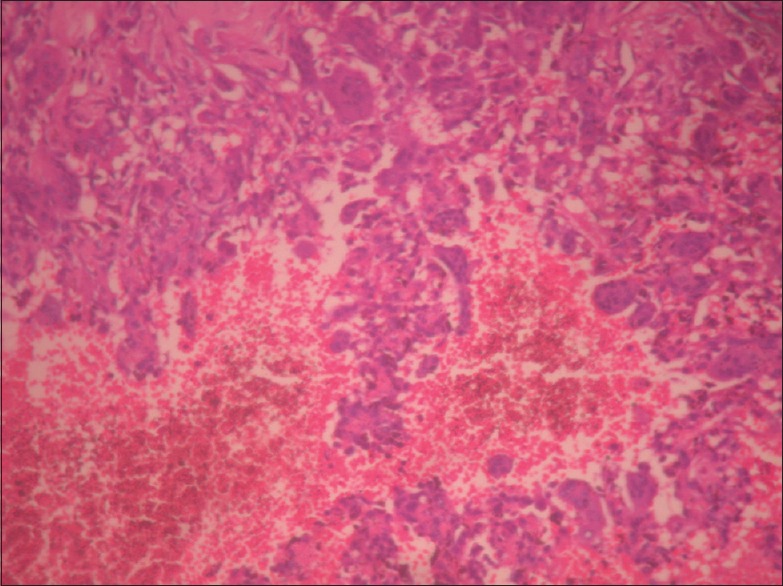
H and E stains showing osteoclast type giant cells having multiple nuclei. Cysts containing haemorrhage and lined by histiocytes and osteoclast giant cells can be noted. There features are suggestive of secondary aneurysmal bone cyst
Post operatively, she had complete relief of pain and improvement in weakness. Post operative X-rays showed implant in position [Figure 4a and b].
Figure 4.
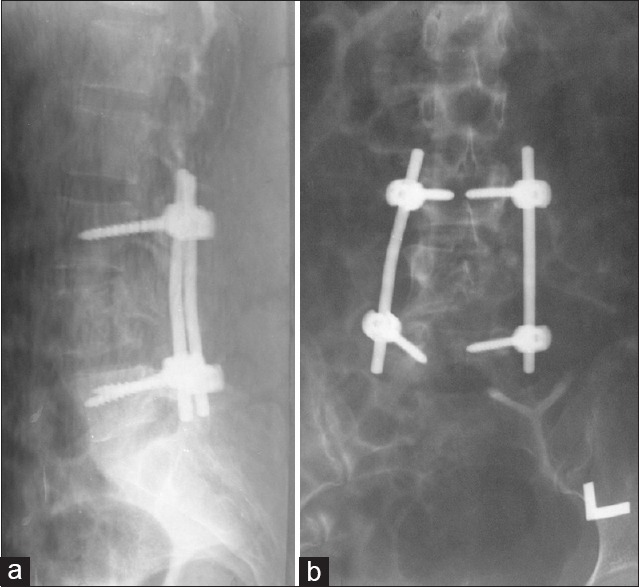
(a) X-ray of the lumbar spine AP; (b) Lateral view showing pedical screw fixation done from L3 to L5 levels
Discussion
Jaffe and Lichtenstein were the first to describe ABC as a distinct entity in 1942, when they noted “a peculiar blood-containing cyst of large size.”[1] World Health Organization has defined ABC as a benign tumor like lesion, “an expanding osteolytic lesion consisting of blood-filled spaces of variable size separated by connective tissue septa containing trabeculae or osteoid tissue and osteoclast giant cells.”[2] ABC comprises approximately 1.4% of all bone tumors and a spinal location is even rarer. It commonly involves the metaphyses of long bones like humerus, femur, tibia, and the flat bones of the pelvis. Spinal involvement is seen in about 10% of cases, most commonly in the thoracic and lumbar regions. ABC is commonly seen in 10-20 years with slight female preponderance. The pedicles are usually affected first then the lesion extends into the vertebral body.[3,4] Some authors are of the opinion that the lesion begins in the posterior elements and then involve the pedicle before extending into the vertebral body.[5,6] ABC is thought to arise from a pre-existing lesion due to a superimposed secondary vascular phenomenon which initiates a periosteal or intraosseous arteriovenous malformation resulting in the erosion of the osseous trabeculae into a cystic cavity.[3,4] A primary ABC is defined histologically as anatomizing fibrous-walled channels that have a complete or incomplete lining of endothelial cells, but in contrast to true blood vessels, they contain no elastic lamina or muscular layers. A secondary ABC has the same microscopic characteristics, but with the additional findings of a coexisting lesion either benign or malignant.[7,8]
Pain is the most common symptom. The patient may present with sensory disturbance, motor weakness, paravertebral mass, or kyphoscoliosis. They can also present with acute symptoms of root/cord compression.[1,3,4] X-rays show a ballooning of the vertebra. In the lumbar region, a winking owl sign is seen. CT scan demonstrates the exact extent and the fluid filled bony cavities. The presence of multiloculated fluid-fluid filled cysts on MRI is characteristic of ABC. This appearance is due to the presence of blood in different stages of evolution within the cyst. On contrast, administration the internal septations show enhancement. MRI also helps to evaluate the cord compression and paravertebral extension.[4] Differential diagnosis includes giant cell tumor, hemangioma, fibrous dysplasia, osteosarcoma, osteoblastoma, and metastatic lesions. Aneurysmal bone cysts have a sponge-like appearance with multi-loculated blood-filled cavities separated by thin, fibrous septa. Fibrous septa of aneurysmal bone cysts are made of fibroblasts, myofibroblasts, multinucleated osteoclast-like giant cells, hemosiderin deposits, blood vessels, and fields of osteoid and woven bone.[4]
In patients without neurological involvement and with pain as the only symptom can be treated with selective arterial embolization alone or by intralesional calcitonin and methylprednisolone injection or vertebroplasty. The results of embolization can be seen in the form of involution of the soft-tissue component, sclerosis, and ossification. The intralesional injection of calcitonin can induce the formation of cancellous bone and inhibit the osteoclastic activity. Methylprednisolone can reduce the fibroblastic action and the angiogenesis.[9,10] This kind of treatment can take years to cure. In patients with neurological involvement surgical management is warranted. Pre-operative selective arterial embolization will reduce the operative blood loss. Simple curettage with or without bone grafting is not ideal in spine and a recurrence rate of approximately 19% within two years is reported.[11] Complete resection of the lesion is the treatment of choice with excellent outcome. Total excision must include the entire cyst wall, all abnormal tissues that feel spongy and bone surfaces that are lined with fragile and hypervascular membranes.[3,4] Bleeding during surgery is from the sinusoid lining of the thin walled vascular space and may be difficult to control until all the lining has been removed.[8] For extensive lesions and those with unstable spine require stabilization. Radiation alone may have no benefit other than an addition risk of malignant transformation. Adjuvant radiation may be given to patients with inoperable lesions, hypervascular lesions, aggressive recurrent disease, or high risk surgical candidates.
Conclusion
Aneurysmal bone cyst is a rare bony tumor of the spine, seen especially in the second decade of the life. ABC has characteristic radiological features. Presence of root/cord compression will require surgical decompression. Stabilization may be required in the presence of instability. Total excision has to be done to achieve total cure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004–25. [Google Scholar]
- 2.Schajowicz F. Berlin, Germany: Springer-Verlag; 1992. Aneurysmal bone cyst. Histologic Typing of Bone Tumors; p. 37. [Google Scholar]
- 3.Ameli NO, Abbassioun K, Saleh H, Eslamdoost A. Aneurysmal bone cyst of the spine. Report of 17 cases. J Neurosurg. 1985;63:685–90. doi: 10.3171/jns.1985.63.5.0685. [DOI] [PubMed] [Google Scholar]
- 4.Liu JK, Brockmeyer DL, Dailey AT, Schmidt MH. Surgical management of aneurysmal bone cysts of the spine. Neurosurg Focus. 2003;15:4. [PubMed] [Google Scholar]
- 5.Koci TM, Mehringer CM, Yamagata N, Chiang F. Aneurysmal Bone Cyst of the Thoracic Spine: Evolution after Particulate Embolization. AJNR Am J Neuroradiol. 1995;16(4 Suppl):857–60. [PMC free article] [PubMed] [Google Scholar]
- 6.Hay MC, Paterson D, Taylor TF. Aneurysmal bone cysts of the spine. J Bone Joint Surg Br. 1978;60:406–11. doi: 10.1302/0301-620X.60B3.681419. [DOI] [PubMed] [Google Scholar]
- 7.Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: Concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. 1995;164:573–80. doi: 10.2214/ajr.164.3.7863874. [DOI] [PubMed] [Google Scholar]
- 8.Chen SH, Huang TJ, Hsueh S, Lee YY, Hsu RW. Unusual bleeding of aneurysmal bone cyst in the upper thoracic spine. Chang Gung Med J. 2002;25:183–9. [PubMed] [Google Scholar]
- 9.Gladden ML, Jr, Gillingham BL, Hennrikus W, Vaughan LM. Aneurysmal bone cyst of the first vertebrae in a child treated with percutaneous intralesional Injection of calcitonin and methylprednisolone: A case report. Spine. 2000;25:527–30. doi: 10.1097/00007632-200002150-00023. [DOI] [PubMed] [Google Scholar]
- 10.Ohashi M, Ito T, Hirano T, Endo N. Percutaneous intralesional injection of calcitonin and methylprednisolone for treatment of an aneurysmal bone cyst at C-2. J Neurosurg Pediatr. 2008;2:365–9. doi: 10.3171/PED.2008.2.11.365. [DOI] [PubMed] [Google Scholar]
- 11.Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK. Aneurysmal bone cyst: a clinicopathologic study of 238 cases. Cancer. 1992;69:2921–31. doi: 10.1002/1097-0142(19920615)69:12<2921::aid-cncr2820691210>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]


