Abstract
This article aims to review our 13-year experience in the treatment of patients with cervical cancer by comparing total laparoscopic radical hysterectomy and lymphadenectomy with laparotomy.
We reviewed all patients undergoing total laparoscopic or laparotomic radical hysterectomy and lymphadenectomy because of cervical cancer between 2001 and 2014 in our hospital.
In total, 154 eligible patients with International Federation of Gynecology and Obstetrics Ia–IIb were enrolled, including 106 patients undergoing total laparoscopic procedure and 48 patients undergoing laparotomic procedure. In the present study, patients in total laparoscopy group were associated with superior surgical outcomes, such as significantly lower blood transfusion compared to those in laparotomy group. Furthermore, patients had significantly lower postoperative complication rate in total laparoscopy group compared with that in laparotomy group (24.5% vs 52.1%) (P = 0.001). Three patients (2.8%) in total laparoscopy group had unplanned conversion to laparotomy. Disease-free survival rates were 89.7% and 88.9% in total laparoscopy and laparotomy groups (P = 0.39), respectively, and overall survival rates were 90.2% in total laparoscopy group and 91.3% in laparotomy group (P = 0.40).
Total laparoscopic procedure is a surgically and oncologically safe and reliable alternative to laparotomic procedure in the treatment for cervical cancer.
INTRODUCTION
Cervical cancer is the third most common cancer and the fourth leading cause of cancer death among women worldwide.1 Moreover, there is a disproportionately high burden of cervical cancer in developing countries, as for various factors.1 Although abdominal radical hysterectomy (ARH) and pelvic lymphadenectomy is the current gold standard for the treatment of early-stage cervical cancer, laparoscopy has become increasingly popular among gynecologic oncologists.2 As total laparoscopic surgery for cervical cancer treatment was first described by Nezhat et al3 and Querleu4 in the early 1900s, there has been increasing evidence in the literature5–9 showing that laparoscopic surgery is safer and more feasible over conventional abdominal surgery, including less blood loss, shorter postoperative hospitalization, and less postoperative complications. Similarly, it is also feasible and safe for elderly and obese cervical cancer patients.10,11 In addition, survival outcomes are comparable for cervical cancer patients based on surgical approaches.5,6,8,10,11 Although a number of other groups have published their experiences showing the safety and feasibility of laparoscopic procedure, few studies have compared total laparoscopic with ARH and pelvic hysterectomy in the treatment of cervical cancer, and most previous studies have enrolled a small series of patients or have a short follow-up; particularly, data related to survival outcomes are limited. In the present study, we will review our 13-year experience and compare the feasibility, morbidity, and survival outcomes of total laparoscopic procedure with abdominal procedure in the treatment of cervical cancer.
MATERIALS AND METHODS
We retrospected the demographic characteristics and surgical outcomes of patients who were diagnosed with histopathology confirmed cervical cancer and have received surgery in our hospital between January 2001 and March 2014. The inclusion criteria were as follows: underwent total laparoscopic or abdominal Piver–Rutledge type III12 radial hysterectomy and lymphadenectomy; with complete medical recordings; not pregnant at diagnosis; and regularly followed up. The study protocol was approved by the Institutional Review Board of our hospital and the patients’ information and statistics were anonymous and unidentified when analyzed.
All patients have received gynecologic examination, vaginal ultrasound, magnetic resonance imaging (MRI), chest x-ray, blood sampling, colposcopy, and biopsy before surgery. The clinical stages were confirmed by 2 experienced gynecologists, and the histopathological results were confirmed by experienced pathologists. Patients who were International Federation of Gynecology and Obstetrics (FIGO) Ib2 with tumor diameter ≥4 cm on MRI or gross appearance and stage II with normal liver and renal functions were scheduled to receive neoadjuvant chemotherapy (NACT), which consisted of 3 agents, including bleomycin (20 mg/m2), cisplatin (80 mg/m2), and mitomycin (10 mg/m2), for 2 to 3 courses before surgery as reported in our previous study13; tumor responses were evaluated according to the criteria reported.14 Patients deemed operable would receive surgery via laparoscopy or laparotomy within 4 weeks from the last course.
Radical hysterectomy and pelvic lymphadenectomy were performed for all patients in the 2 groups. Paraaortic lymph nodes sampling was performed for patients with FIGO Ib–IIb; paraaortic lymphadenectomy was not routinely performed unless suspicious pelvic lymph nodes were confirmed to have metastases on frozen section. No uterus manipulator devices were used in our study, but the cervix was grasped with a cervical clamp and a self-made balloon-like solid occluder was emplaced in vagina in order to improve exposure and preserve an adequate pneumoperitoneum during colpotomy. According to the stages and patient's desire, the ovaries were either dissected or transposed laterally to the paracolic gutters and fixed securely to the abdominal wall. All lymph nodes and other dissected tissues were placed into a pipe and retrieved through the vagina. The vaginal cut was also laparoscopically sutured in the total laparoscopy group. At the end of surgery, injecting sterile water with 16 mg mitomycin was used to irrigate the pelvic cavity in order to reduce the recurrence of pelvic effectively.
All patients were given intravenously prophylactic antibiotics (cefoxitin sodium 2 g) half an hour before the surgery. Since 2010, all patients in our department have been provided with prophylactic devices or medicine for prevention of thrombosis as reported in the previous studies.15 A Foley catheter remained in place for at least 2 weeks after surgery and then patients received a bladder voiding trial. The catheter would be removed if the amount of residual urine was <100 mL; otherwise patients should keep a replaced catheter till bladder function recovered normally. After surgery, patients with intermediate or high risk factors were recommended to receive adjuvant therapies as indicated in another study.5
All patients in the present study were scheduled to surgery via total laparoscopy or laparotomy, and the final decisions were decided by patients themselves after a thorough counseling and comprehension of benefits, potential risks, and possibility of conversion to laparotomy for patients undergoing laparoscopic procedure.
Following completion of treatment, all patients were scheduled to follow-up regularly, as 1 month after surgery, then every 3 months for the first 2 years, every 4 months for the next 2 years, and every 6 months thereafter. Follow-up information, including postoperative complications, recurrence, date and cause of death, and latest status, were all recorded in detail.
The Student t test and the Mann–Whitney U test were used for comparison of continuous parametric and nonparametric variables, respectively. Pearson χ2 test or Fisher exact test was used to analyze proportions. Disease-free survival (DFS) time was calculated as the number of months from the date of surgery to the date of recurrence or censoring. DFS and overall survival (OS) rates and curves were estimated by Kaplan–Meier method and log rank test. Statistical significance was set at a 2-sided P value <0.05. All data were analyzed with SPSS 13.0 (SPSS Inc., Chicago, IL).
RESULTS
We have retrospected a series of 280 patients with histopathologically confirmed cervical cancer; a total of 154 patients fulfilled our inclusion criteria and were enrolled in the present study, including 106 patients in total laparoscopy group and 48 in laparotomy group. We excluded 126 patients from the study: 60 patients underwent other types of radical hysterectomy (Piver–Rutledge type II or IV)12; 30 patients had radical trachelectomy for future pregnancy; 15 patients underwent vaginal-assisted laparoscopic or laparoscopic-assisted vaginal radical hysterectomy; 7 patients refused surgery and chose radiotherapy; 4 patients had incomplete medical recordings; 5 patients were pregnant; 3 patients combined with other gynecological malignant tumors; and 1 patient had histopathology confirmed cervical melanoma.
Patients’ information and tumor characteristics are specified in Table 1. Mean ages were 43.7 (range, 22–68) years and 45.7 (range, 28–78) years in total laparoscopy group and laparotomy group, respectively. Patients had a mean body mass index (BMI) of 23.8 (range, 17.5–42.5) kg/m2 and 24.7 (range, 17.2–36.0) kg/m2 in total laparoscopy and laparotomy groups, respectively. No significant differences were found in age, BMI, and tumor characteristics, such as FIGO stage. More lymph nodes were dissected in laparotomy group than that in the total laparoscopy group (mean, 24.3 vs 20.5, P = 0.008), whereas no significant differences were observed regarding number of metastatic lymph nodes and the dissected lymph nodes for patients with metastatic lymph nodes between the 2 groups, showed in Figure 1.
TABLE 1.
Demographic Characteristics and Histopathological Outcomes of Patients Based on Surgical Approach
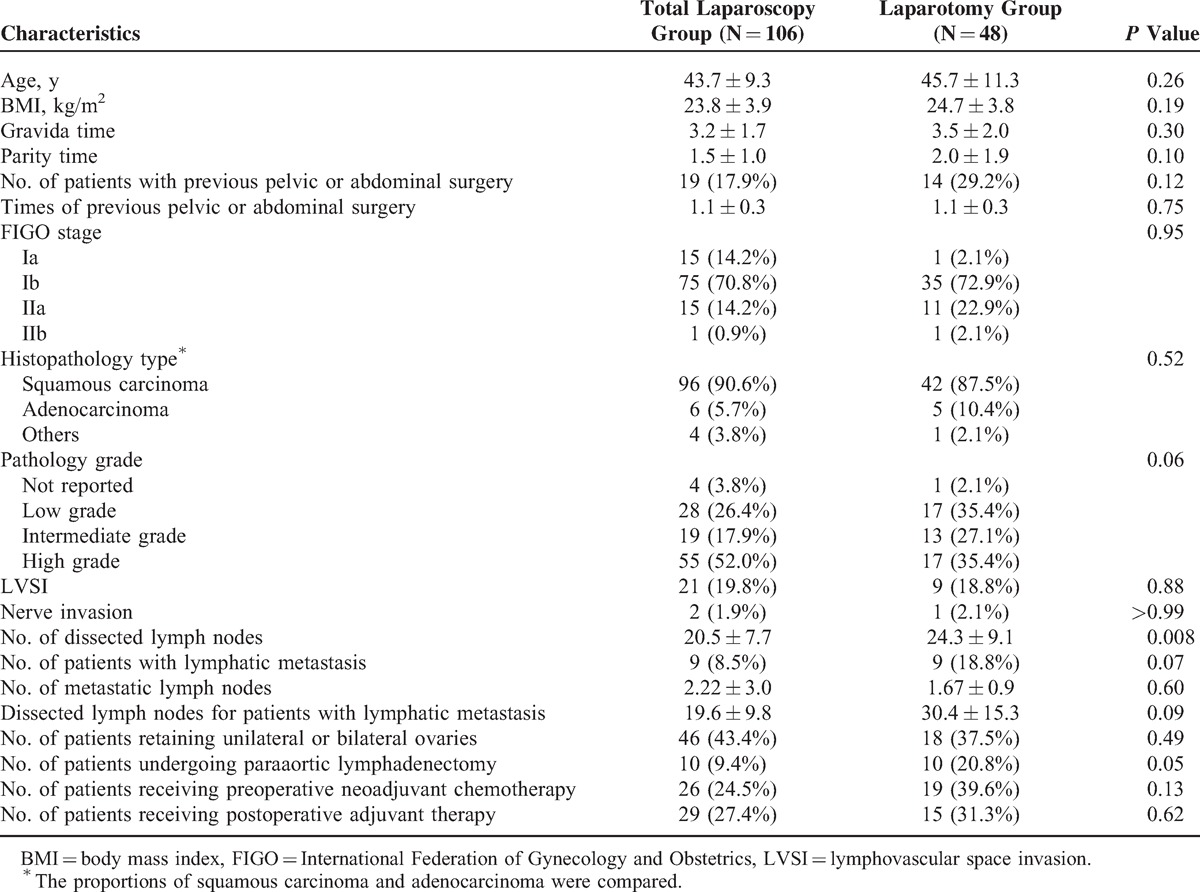
FIGURE 1.
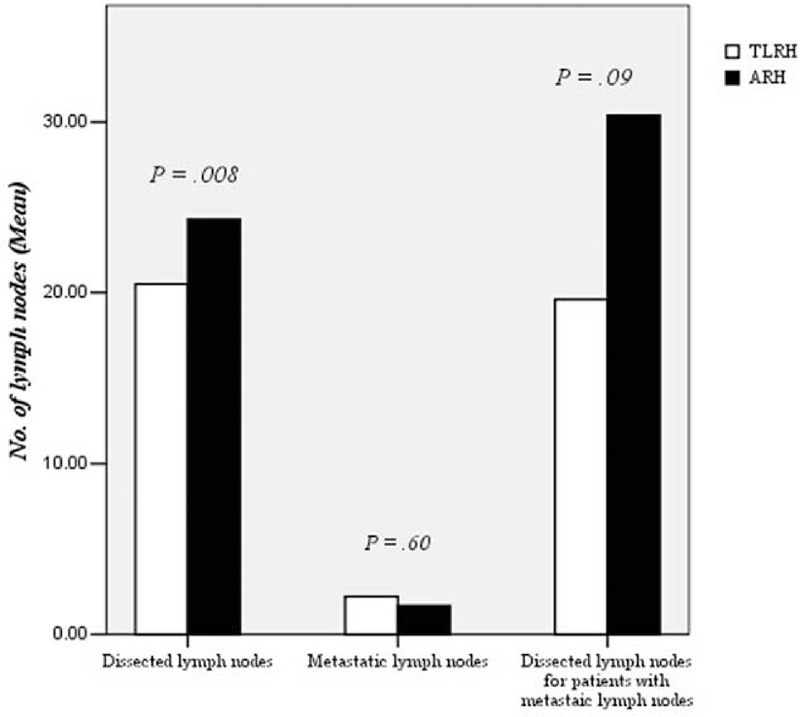
Comparison of dissected lymph nodes for patients undergoing total laparoscopic radical hysterectomy (TLRH) or abdominal radical hysterectomy (ARH).
Surgical details and complications of patients based on surgical approach were summarized in Table 2. Significantly shorter operative time (mean, 270.8 vs 310.2 min), earlier to flatus (mean, 2.3 vs 2.7 days), shorter postoperative hospitalization (mean, 16.8 vs 20.7 days), less estimated blood loss (mean, 232.6 vs 797.9 mL), and lower blood transfusion rate (13.2% vs 54.2%) were for patients in total laparoscopy group compared with those in the laparotomy group. Some patients had concurrent kinds of complications and no between-group significant difference was found regarding intraoperative complications. Three patients (2.8%) in total laparoscopy group had unplanned conversion to laparotomic procedure, all because of severe adhesion after previous pelvic infection and/or surgeries. All organ injuries happened in laparotomy group, including 2 cases with ureteral injury and 1 with obturator nerve injury. What is worse—patients with ureteral injury all had ureterovaginal fistula a month after operation and all received another operation.
TABLE 2.
Surgical Details and Intra/Postoperative Complications of Patients Based on Surgical Approach
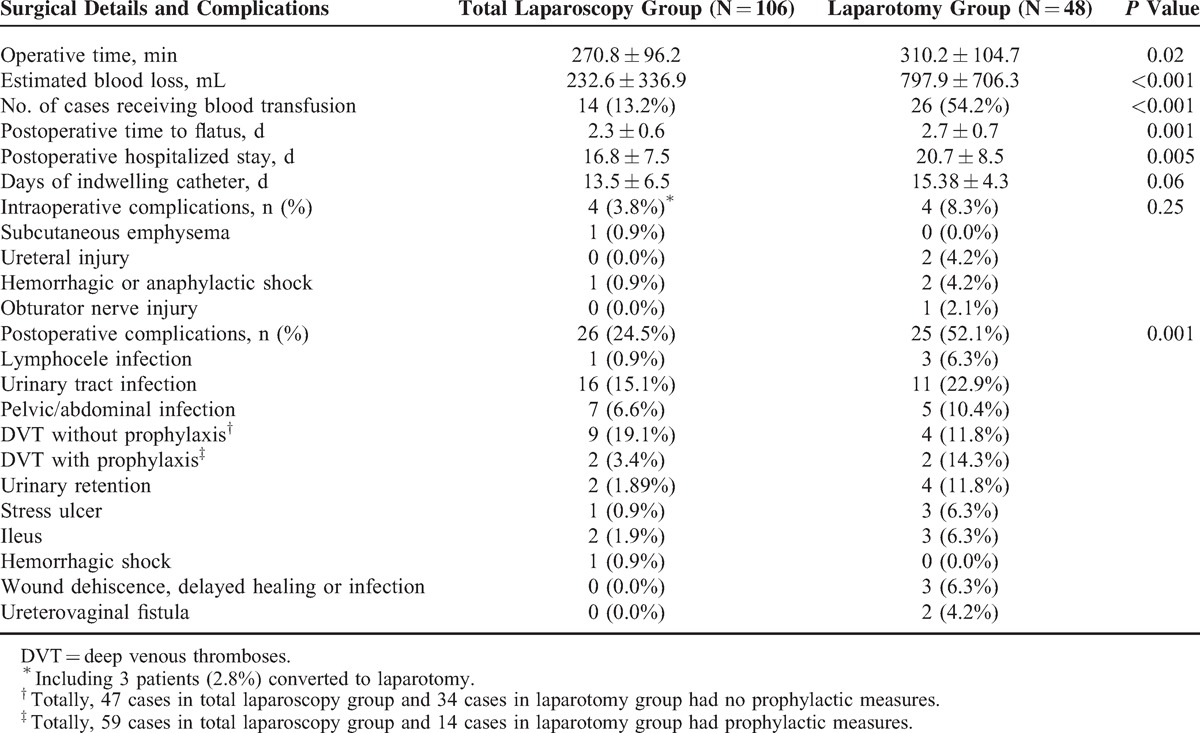
In total laparoscopy group, 24.5% of patients had postoperative complications within 60 days after the surgery, which was significantly lower than that of 52.1% in the laparotomy group (P = 0.001). The most common postoperative complication was urinary tract infection, with no significant differences between total laparoscopy and laparotomy groups (15.1% vs 22.9%). Without prophylactic devices and medicine, 19.1% (9/47) and 11.8% (4/34) of patients in the total laparoscopy group and the laparotomy group, respectively, had deep venous thromboses (DVT) after surgery, including 4.3% (2/47) and 2.9% (1/34), respectively, with concurrent pulmonary embolism. Since 2010, with prophylactic measures, only 3.4% (2/59) and 14.3% (2/14) of patients had DVT in total laparoscopy and laparotomy groups, respectively, and no cases had pulmonary embolism. No significant differences were found between the 2 groups. Nevertheless, 16.0% (13/81) of patients without prophylactic measures had DVT, which was significantly higher than that of 5.5% (4/73) of patients with prophylactic measures (P = 0.04). Urinary retention, stress ulcer, and ileus also similarly happened to patients in the 2 groups. However, complications associated with surgical incision, such as infection, were only found in the laparotomy group.
By December 31, 2014, the final follow-up day, we have successfully followed up all patients in outpatient clinic or by telephone; 6 patients (5.7%) in total laparoscopy group and 5 patients (10.4%) in laparotomy group had documented histopathologically confirmed recurrence, and 10 patients have died, with 4 patients assigned to total laparoscopy group and 6 to laparotomy group. One patient died from intercurrent disease and 1 from fatal cerebral hemorrhage in laparotomy group and others from cervical cancer. Although the follow-up time was a little longer in laparotomy group than that in the total laparoscopy group (mean, 64.6 vs 48.2 months, P = 0.02), no between-group differences were observed in the survival outcomes (Table 3); the DFS and OS for cervical cancer patients undergoing total laparoscopic or laparotomic procedure were separately shown in Figure 2.
TABLE 3.
Survival Outcomes of Patients Based on Surgical Approach
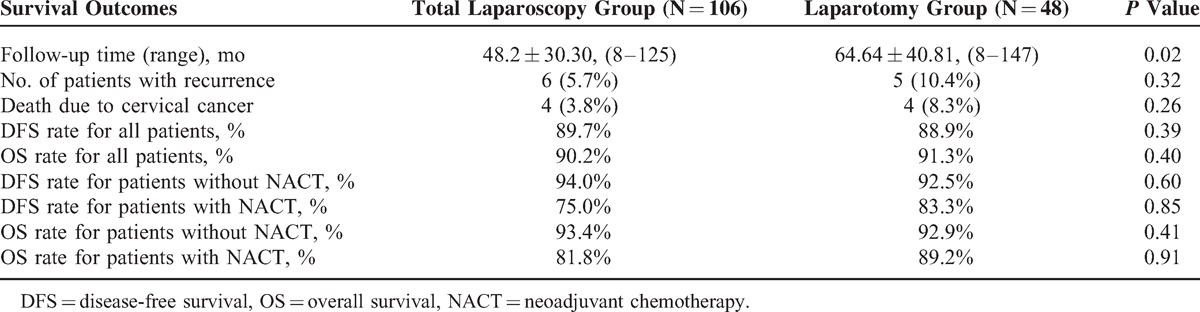
FIGURE 2.
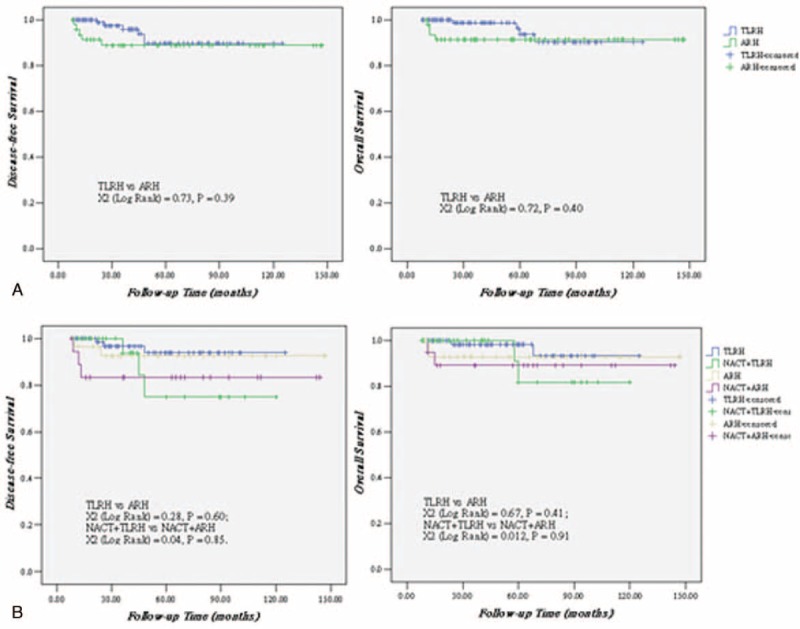
(A) Disease-free survival and overall survival for patients undergoing total laparoscopic radical hysterectomy (TLRH) or abdominal radical hysterectomy (ARH); (B) Disease-free survival and overall survival for patients with early-stage cervical cancer undergoing TLRH or ARH, and with locally advanced disease receiving neoadjuvant chemotherapy (NACT) along with TLRH or NACT along with ARH.
DISCUSSION
Our data indicated that both laparoscopic and laparotomic approaches were feasible for patients with cervical cancer. Moreover, laparoscopy had superior surgical outcomes, with significantly less operative time, earlier anal exhaust, shorter postoperative hospitalization, less estimated blood loss, and less postoperative complications, compared with that of laparotomy, consistent with that in other studies.10 In the present study, duration of postoperative hospitalization were 16.7 and 20.7 days in total laparoscopy and laparotomy groups, respectively, which were in agreement with that in other Chinese hospitals,16 but obviously longer than that in western hospitals, with mean duration of 2 to 4 versus 5 to 8 days in Laparoscopic Radical Hysterectomy group and laparotomy group, respectively.7,8 This may be due to the insurance policies for cancer patients in our country and most patients preferred to stay in hospital as long as they wanted or until the removal of catheter.
Moreover, with 13.2% versus 54.2% in total laparoscopy group and laparotomy group, respectively, blood transfusion rates here seemed quite high, compared with that reported by others with 0.0% versus 8.3%,9 0.0% versus 16.7%,7 and 0.0% versus 35.7%.17 However, Hou et al18 reported 27.3% and 83.3% of patients with FIGO Ia–IIb receiving blood transfusion in laparoscopy and laparotomy groups, respectively. That great distinction may be attributed to the trend to overestimate the amount of blood loss in case of radical hysterectomy for cervical cancer; the transfusion indication for cervical cancer patients undergoing radical hysterectomy is more flexible than others. In addition, the number of patients with locally invasive cervical cancer differed greatly in these studies and paraaortic lymphadenectomy may bring high incidence of blood transfusion.
Significantly less lymph nodes were dissected in total laparoscopy group than that in the laparotomy group (mean, 20.5 vs 24.3), whereas no significant differences were observed in the number of metastatic lymph nodes, which was in accord with other studies.19 Others7 found significantly more lymph nodes dissected for cervical cancer patients in laparoscopy than that in laparotomy (31.0 vs 21.8). Berta et al20 suggested that the removal of at least 20 pelvic or paraaortic lymph nodes might be regarded as an adequate lymphadenectomy. Differences between the number of lymph nodes retrieved may not be because of a kind of technique.21 Particularly, others22 indicated that lymph node metastasis was the only independent factor for poor prognosis for cervical cancer patients. Therefore, a difference of 3.8 for dissected lymph nodes seemed to have no clinically significant influence on the oncological outcomes in patients with cervical cancer.
Data5,8,10,11,16 suggested that cervical cancer patients in laparoscopy had similar intraoperative complication rates and significantly lower postoperative complication rates compared with those in laparotomy, consistent with the results in our study. Nevertheless, the postoperative complication rates (total laparoscopy vs laparotomy, 24.5% vs 52.1%) seemed to be much higher than that in others.5,8,10,11,16 In a propensity-matched study with 130 cervical cancer patients, Giorgio et al8 reported postoperative complication for ≥grade 323 rate was 6.0% versus 18.0% (laparoscopy vs laparotomy). Michael et al19 reported incidences of 17.1% and 18.5% for cervical cancer patients with FIGO Ia1–Ib2 in laparoscopy and laparotomy groups, respectively, whereas rates were 18.0% and 53.0% when infectious morbidity included. Therefore, higher incidences of postoperative complications in the present study may be due to detailed records of all the mild or severe complications, especially infectious morbidity. As the more radical the surgery, the greater will be the extent of surgery and the more likely postoperative complications will result; a few patients with locally invasive cervical cancer enrolled in our study may be another factor.
Li et al16 reported that 32.2% and 28.6% of patients in laparoscopy and laparotomy groups, respectively, had urinary retention. Yan et al24 found that 32.5% of patients had urinary retention (as defined by a postvoid residual <100 mL of urine <10 days) and exhibited complete resolution within 6 months, although the incidences of bladder retention in the present study were obviously low (total laparoscopy vs laparotomy, 1.9% vs 11.8%). Though the incidences of bladder retention and the return of normal bladder function are difficult to compare between studies as various definitions and criteria are used, we still believe that keeping the catheter for no <14 days could make bladder full rest and reduce the incidence of bladder retention.
All laparoscopic procedures were completed successfully except 3 cases that were converted to laparotomy and the conversion rate was 2.8%, which was similar to the previous studies, ranking from 1.7% to 5.7%.16,19,24
The survival outcome is the gold standard to evaluate a new surgical technique, and the present data are corroborated by the results in others.5,6,8 Nam et al,5 in a large matched-cohort study comparing 263 pairs of patients with early-stage cervical cancer undergoing laparoscopic or laparotomic procedure, found that the type of surgical approach does not influence survival outcomes, with 5-year DFS of 93% and 94% in laparoscopy and laparotomy groups, respectively. In another retrospective study with 88 cervical cancer patients of FIGO stage Ib2–IIa, Tae et al6 reported that DFS was 97.5% and 97.9% for patients in laparoscopy and laparotomy groups, respectively. In particular, another propensity-matched study8 with 65 cervical cancer patient pairs reported that the 5-year DFS (83% for laparoscopy vs 80% for laparotomy) and OS (89% for laparoscopy vs 83% for laparotomy) did not differ significantly in the two groups; moreover, for patients with locally advanced cervical cancer undergoing NACT along with surgery, no significant differences were found in 5-year OS between laparoscopy and laparotomy groups (77% vs 67%). In addition, a multicenter Italian study25 with 341 locally advanced cervical cancer patients of FIGO stage Ib2–IIb undergoing NACT along with radical hysterectomy indicated that laparoscopic surgery does not negatively influence survival outcomes.
However, there is one main limitation that it is a retrospective study and enrolled some patients having received NACT before undergoing total laparoscopic or laparotomic radical hysterectomy and lymphadenectomy. Although prospective randomized controlled trials have been ongoing,2 we reviewed our 13-year experience in the surgery treatment of cervical cancer patients in a developing country and paid more attention to the surgical and survival outcomes; moreover, we separately calculated and analyzed the survival outcomes for patients with or without preoperative NACT. Particularly, we have successfully followed up all the enrolled patients. Therefore, the data in our study could provide more evidence, especially survival outcomes, for cervical cancer patients undergoing surgery treatment with different surgical approach.
In conclusion, the findings in the present study suggested that total laparoscopic procedure is a surgically and oncologically safe and reliable alternative to abdominal procedure in the treatment for cervical cancer patients. Certainly, more multicenter prospective randomized controlled trials are required to further evaluate the overall oncological outcomes of this approach.
Footnotes
Abbreviations: ARH = abdominal radical hysterectomy, BMI = body mass index, DFS = disease-free survival, DVT = deep venous thromboses, FIGO = International Federation of Gynecology and Obstetrics, LVSI = lymphovascular space invasion, MRI = magnetic resonance imaging, NACT = neoadjuvant chemotherapy, OS = overall survival, TLRH = total laparoscopic radical hysterectomy.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Ahmedin J, Freddie B, Melissa MC, et al. Global Cancer Statistics. CA Cancer J Clin 2011; 61:69–90. [DOI] [PubMed] [Google Scholar]
- 2.Andreas O, Val G, Michael F, et al. A phase III randomized clinical trial comparing laparoscopic or robotic radical hysterectomy with abdominal radical hysterectomy in patients with early stage cervical cancer. J Minim Invasive Gynecol 2008; 15:584–588. [DOI] [PubMed] [Google Scholar]
- 3.Nezhat CR, Burrell MO, Nezhat FR, et al. Laparoscopic radical hysterectomy with para-aortic and pelvic node dissection. Am J Obstet Gynecol 1992; 166:864–865. [DOI] [PubMed] [Google Scholar]
- 4.Querleu D. Laparoscopic radical hysterectomy. Am J Obstet Gynecol 1993; 168:1643–1645. [DOI] [PubMed] [Google Scholar]
- 5.Nam J-H, Park J-Y, Kim D-Y, et al. Laparoscopic vs open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol 2012; 23:903–911. [DOI] [PubMed] [Google Scholar]
- 6.Tae WK, Suk-Joon C, Jisun L, et al. Comparison of laparoscopic vs abdominal radical hysterectomy for FIGO stage IB and IIA cervical cancer with tumor diameter of 3 cm or greater. Int J Gynecol Cancer 2014; 24:280–288. [DOI] [PubMed] [Google Scholar]
- 7.Zakashansky K, Chuang L, Gretz H, et al. A case-controlled study of total laparoscopic radical hysterectomy with pelvic lymphadenectomy vs radical abdominal hysterectomy in a fellowship training program. Int J Gynecol Cancer 2007; 17:1075–1082. [DOI] [PubMed] [Google Scholar]
- 8.Giorgio B, Antonella C, Stefano U, et al. Laparoscopic vs open abdominal management of cervical cancer: long-term results from a propensity-matched analysis. J Minim Invasive Gynecol 2014; 21:857–862. [DOI] [PubMed] [Google Scholar]
- 9.Fabio G, Antonella C, Giuseppe C, et al. Surgicopathologic outcome of laparoscopic vs open radical hysterectomy. Gynecol Oncol 2007; 106:502–506. [DOI] [PubMed] [Google Scholar]
- 10.Park J-Y, Kim D-Y, Kim J-H, et al. Laparoscopic vs open radical hysterectomy for elderly patients with early-stage cervical cancer. Am J Obstet Gynecol 2012; 207:195.e1–195.e8. [DOI] [PubMed] [Google Scholar]
- 11.Park J-Y, Kim D-Y, Kim J-H, et al. Laparoscopic compared with open radical hysterectomy in obese women with early-stage cervical cancer. Obstet Gynecol 2012; 119:1201–1209. [DOI] [PubMed] [Google Scholar]
- 12.Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol 1974; 44:265–272. [PubMed] [Google Scholar]
- 13.Qi Lu, Yunhe Zhang, Shuzhen Wang, et al. Neoadjuvant intra-arterial chemotherapy followed by total laparoscopic radical trachelectomy in stage IB1 cervical cancer. Fertil Steril 2014; 101:0015–0282. [DOI] [PubMed] [Google Scholar]
- 14.Patrick T, Susan GA, Elizabeth AE, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 2000; 92:205–216. [DOI] [PubMed] [Google Scholar]
- 15.Lu Q, Zhang Y, Liu C, et al. Total laparoscopic radical trachelectomy in the treatment of early squamous cell cervical cancer: a retrospective study with 8-year follow-up. Gynecol Oncol 2013; 130:275–279. [DOI] [PubMed] [Google Scholar]
- 16.Li G, Yan X, Shang H, et al. A comparison of laparoscopic radical hysterectomy and pelvic lymphadenectomy and laparotomy in the treatment of Ib-IIa cervical cancer. Gynecol Oncol 2007; 105:176–180. [DOI] [PubMed] [Google Scholar]
- 17.Ricardo E, Nicholas L, Robert D, et al. A case matched analysis of robotic radical hysterectomy with lymphadenectomy compared with laparoscopy and laparotomy. Gynecol Oncol 2009; 113:357–361. [DOI] [PubMed] [Google Scholar]
- 18.Hou C-Y, Li X-L, Jiang F, et al. Comparative evaluation of surgical stress of laparoscopically assisted vaginal radical hysterectomy and lymphadenectomy and laparotomy for early-stage cervical cancer. Oncol Lett 2011; 2:747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michael F, Ricardo dos R, Charlotte CS, et al. Comparison of total laparoscopic and abdominal radical hysterectomy for patients with early-stage cervical cancer. Obstet Gynecol 2007; 110:96–102. [DOI] [PubMed] [Google Scholar]
- 20.Berta D-F, Antonio G-M, Marıa AP-B, et al. Sentinel lymph node identification and radical hysterectomy with lymphadenectomy in early stage cervical cancer: laparoscopy vs laparotomy. J Minim Invasive Gynecol 2008; 15:531–537. [DOI] [PubMed] [Google Scholar]
- 21.Athanasios P, Kris T, Nicola JB, et al. Total laparoscopic radical hysterectomy in the treatment of early cervical cancer. Int J Gynecol Cancer 2009; 19:712–722. [DOI] [PubMed] [Google Scholar]
- 22.Yan X, Li G, Shang H, et al. Twelve-year experience with laparoscopic radical hysterectomy and pelvic lymphadenectomy in cervical cancer. Gynecol Oncol 2011; 120:362–367. [DOI] [PubMed] [Google Scholar]
- 23.Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg 2009; 250:177–186. [DOI] [PubMed] [Google Scholar]
- 24.Yan X, Li G, Shang H, et al. Complications of laparoscopic radical hysterectomy and pelvic lymphadenectomy: experience of 117 patients. Int J Gynecol Cancer 2009; 19:963–967. [DOI] [PubMed] [Google Scholar]
- 25.Fabio G, Antonella C, Antonino D, et al. Laparoscopic vs open radical hysterectomy for stage IB2-IIB cervical cancer in the setting of neoadjuvant chemotherapy: a multi-institutional cohort study. Ann Surg Oncol 2013; 20:2007–2015. [DOI] [PubMed] [Google Scholar]


