Abstract
To evaluate the safety and efficacy of Trabectome after failed tube shunt surgery.
Twenty patients with prior failed tube shunt surgery who underwent Trabectome alone were included. All patients had at least 3 months of follow-up. Outcomes measured included intraocular pressure (IOP), glaucoma medications, and secondary glaucoma surgeries. The success for Kaplan–Meier survival analysis is defined as IOP ≤21 mm Hg, IOP reduced by at least 20% from preoperative IOP, and no secondary glaucoma surgery.
Mean preoperative IOP was 23.7 ± 6.4 mm Hg and mean number of glaucoma medications was 3.2 ± 1.5. At 12 months, IOP was reduced to 15.5 ± 3.2 mm Hg (P = 0.05) and number of medications was reduced to 2.4 ± 1.5 (P = 0.44). Survival rate at 12 months was 84% and 3 patients required additional glaucoma surgery with 15 patients reaching 12 months follow-up. Other than failure of IOP control and transient hypotony (IOP < 3 mm Hg) day 1 in 2 cases, there were no adverse events.
Trabecular bypass procedures have traditionally been considered an approach appropriate for early-to-moderate glaucoma; however, our study indicates benefit in refractory glaucoma as well. Eyes that are prone to conjunctival scarring and hypertrophic wound healing, such as those who have failed tube shunt surgery, may benefit from procedures that avoid conjunctival incision such as Trabectome. This study indicates potential benefits in this patient population.
Trabectome was safe and effective in reducing IOP at 1-year follow-up in patients with prior failed tube shunt surgery, but not effective in reducing medication reliance in these patients.
INTRODUCTION
Recent results from major clinical trials evaluating the success of tube shunt implantation for glaucoma highlight the need for alternative treatments in that the failure rates of the most commonly used implants exceed 30% at 3 years.1–3 Typically, tube shunts are reserved for refractory glaucomas that have failed prior laser or incisional procedures.4 These eyes tend to have conjunctival compromise after prior procedures resulting in conjunctival scarring and therefore have very limited treatment options as our current standard glaucoma surgical interventions rely on conjunctival tissue for aqueous drainage in the case of trabeculectomy, or coverage of devices in the case of aqueous shunts. The Trabectome is a trabecular bypass procedure that does not involve a conjunctival incision and is performed via an ab interno approach through clear cornea. In this study, we evaluate the Trabectome device as a treatment modality for refractory glaucoma eyes with failed aqueous shunt implantation.
METHODS
A total of 20 patients were included in this study. All patients had undergone Trabectome. Patients were excluded if they have less than 3 months of follow-up, had neovascular glaucoma, vision less than hand motions, Shaffer less than grade II on gonioscopy, or if they never had previous tube shunt surgery or trabeculectomy.
Data was obtained by a review of the records in an academic practice of a single surgeon (SM) with Institutional Review Board (IRB) approval, as well as by reviewing the records in the Trabectome Surgeon Database. The data in the database are submitted by Trabectome surgeons on standardized forms for the first 20 patients performed by each Trabectome surgeon. This database also has IRB approval and oversight. Data collected included pre- and postoperative intraocular pressure (IOP) measured by Goldmann applanation tonometry, visual acuity, automated Humphrey Visual Field mean deviation results, gonioscopy assessments, and patient demographics. All patients had previous failed tube shunt implantation with uncontrolled IOP on maximal tolerated medical therapy.
Details of the Trabectome surgical procedure have been previously described.5,6 First, a 1.8 mm clear corneal incision is made and the probe of the coaxial Trabectome handpiece is placed into the anterior chamber and inserted into Schlemm canal under direct gonioscopic visualization. Then, the tip of the handpiece is advanced within the canal to remove a 60–180° strip of the inner wall of Schlemm's and trabecular meshwork.
Statistical analysis was performed using R statistical software (R-Project). Comparison of preoperative and postoperative measures was done by using paired t-test. Kaplan–Meier was used for survival analysis, where success was defined as IOP less than 21 mm Hg, 20% or more reduction from a baseline IOP for any 2 consecutive visits after 3 months, and no secondary glaucoma surgery. Statistical significance was taken as P ≤ 0.05.
RESULTS
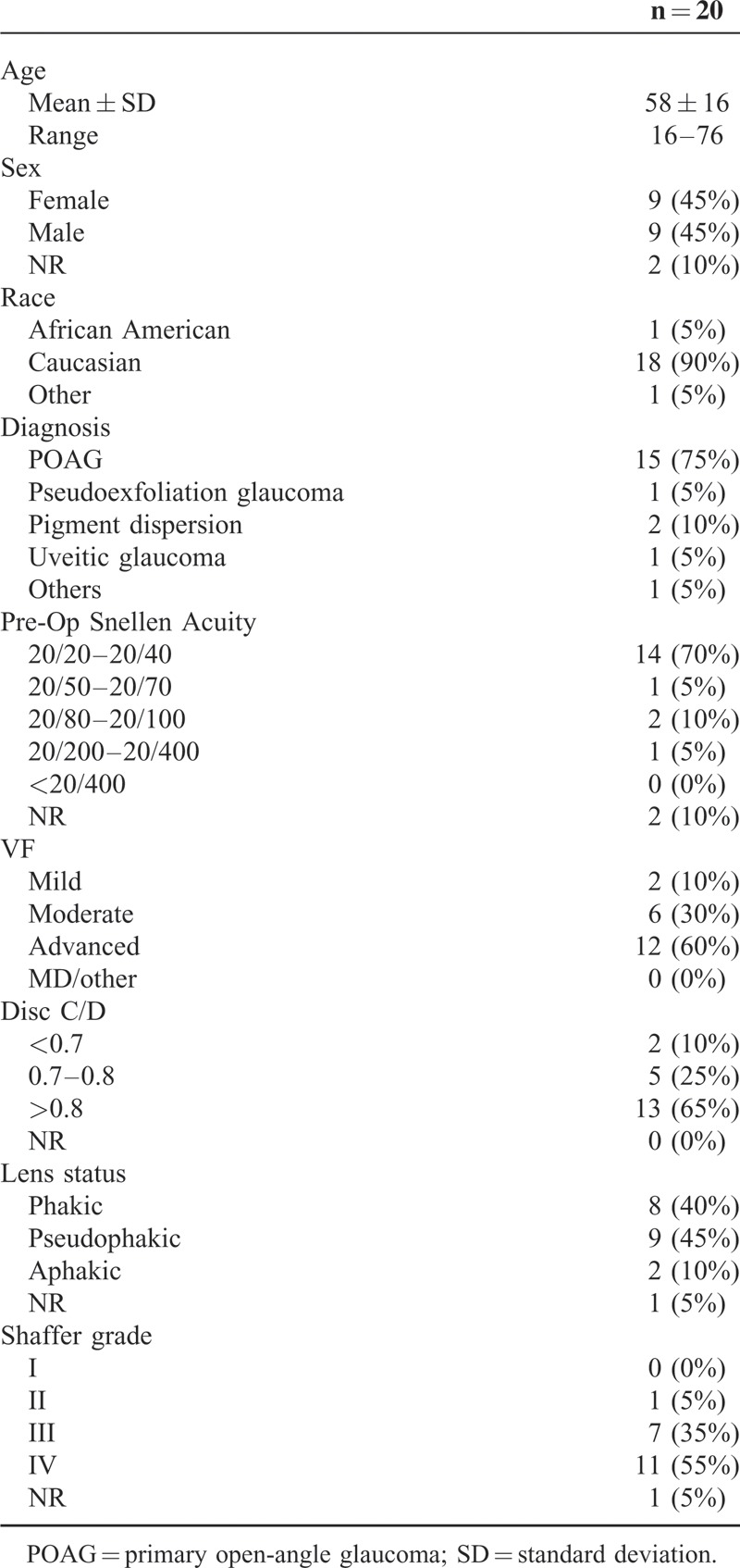
A total of 20 patients that had undergone Trabectome surgery alone were included in this study. Average age of the study group was 58 (range 16–76). Most were Caucasians (90%) and diagnosed with primary open-angle glaucoma (POAG) (75%). Table 1 shows the baseline characteristics of the study group.
TABLE 1.
Demographics
The mean preoperative IOP was 23.7 ± 6.4 mm Hg. Postoperative IOP was 15.5 ± 3.2 mm Hg (P = 0.05∗) at 12 months. The number of glaucoma medications was reduced to 2.4 ± 1.5 (P = 0.44) at 12 months from baseline of 3.2 ± 1.5. The IOP reduction was statistically significant, but the change in medication usage was not. Figures 1 and 2 show the trend of IOP and usage of glaucoma medications, respectively.
FIGURE 1.
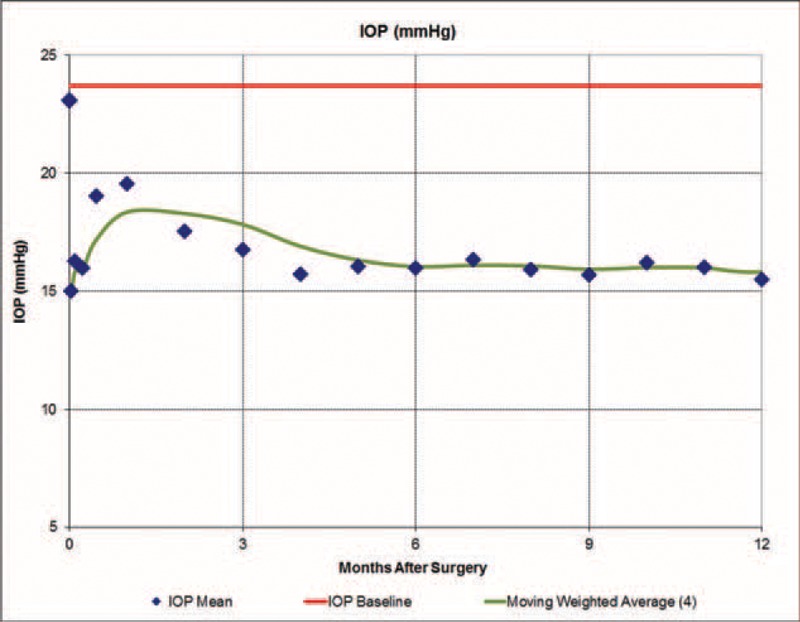
IOP trend in patients receiving Trabectome surgery after failed tube shunt procedure. IOP = intraocular pressure.
FIGURE 2.
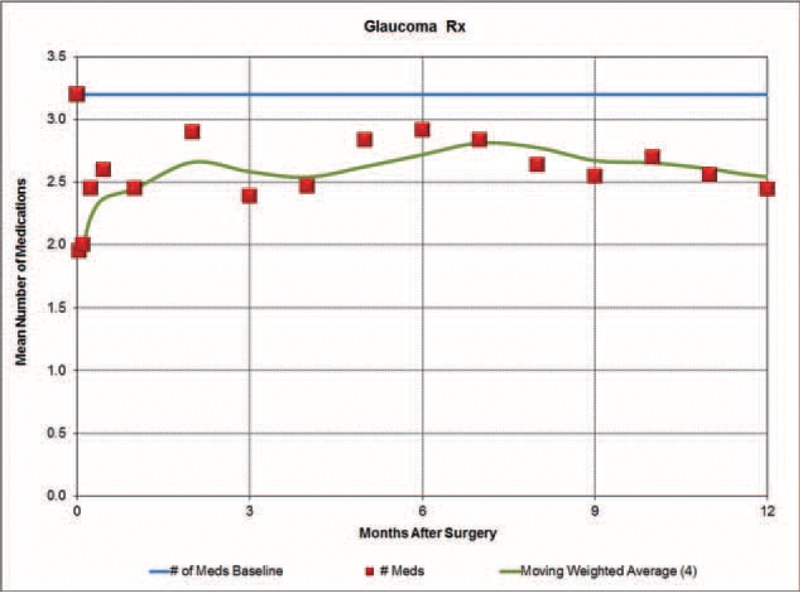
Number of glaucoma medications trend in patients receiving Trabectome surgery after failed tube shunt procedure.
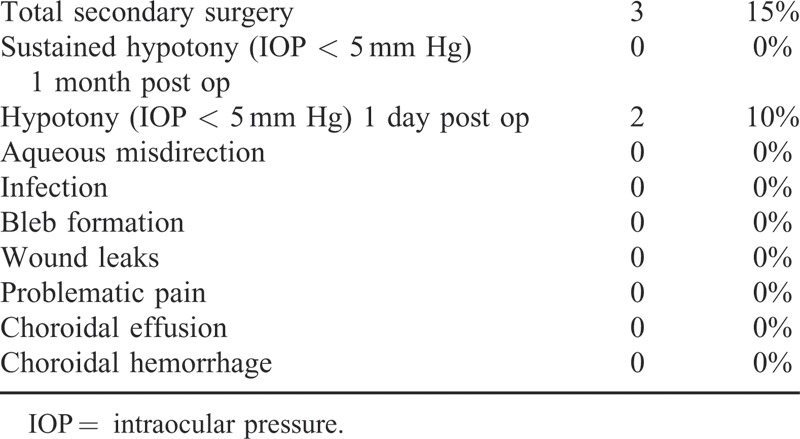
Figure 3 depicts the survival curve. The survival rate at 12 months was 84% with 12 patients reaching 12 months follow-up. Three patients required additional glaucoma surgery. Two patients were reported with hypotony at day 1, but these resolved spontaneously without long-term sequelae (Table 2). No other complications were noted.
FIGURE 3.
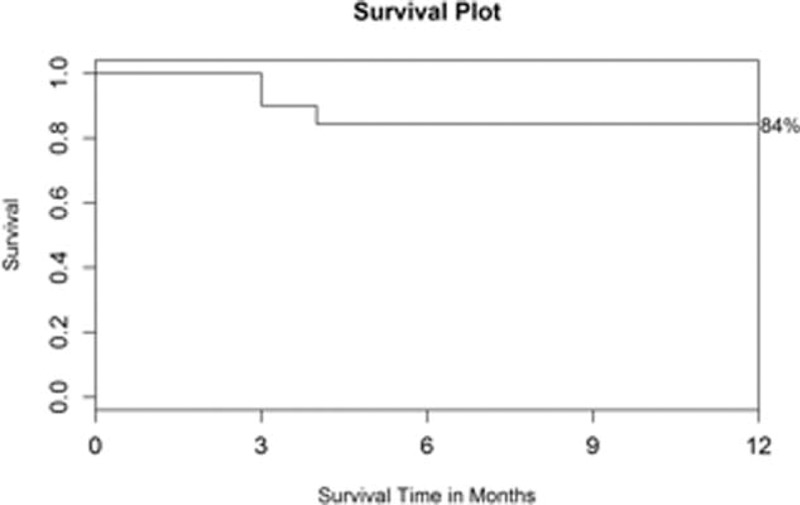
Kaplan–Meier survival plot, where success was defined as IOP less than 21 mm Hg, 20% or more reduction from a baseline IOP for any 2 consecutive visits after 3 months, and no secondary glaucoma surgery. IOP = intraocular pressure.
TABLE 2.
Postoperative Observations at 12 Months
DISCUSSION
The standard approach to managing glaucoma has traditionally been to employ medications first, followed by laser trabeculoplasty, followed by incisional surgery such as trabeculectomy, and if that fails, to proceed to tube shunt surgery.4 Recent large-scale, randomized clinical trials aimed at addressing the superiority of trabeculectomy over tube shunt implantation concluded that trabeculectomy and the Baerveldt Implant resulted in similar IOP-lowering at 5 years, but that the trabeculectomy was associated with a higher complication rate.7 These results have created a paradigm shift in that many glaucoma surgeons now consider tube shunt implantation as a primary incisional option and greater numbers of these procedures are being performed. In an attempt to determine which of the commonly implanted aqueous shunts were clinically more effective, the Ahmed Baerveldt Comparison study and the Ahmed Versus Baervledt studies were recently conducted. Both of these multicenter, randomized studies concluded that the failure rates of the Baerveldt implant exceed 30% at 3 years, and that the failure rate of the Ahmed valve was even higher, reaching 50% in the Ahmed versus Baerveldt Study.1,2 These results indicate that more options are needed to treat these refractory cases; ideally, options that do not require conjunctival tissue for success.
The Trabectome procedure is an ab interno trabecular bypass procedure that employs microbipolar elecrocautery to remove a strip of the trabecular meshwork and inner wall of Schlemm's canal. Prior published series on the Trabectome procedure have quoted success rates anywhere between 50 and 89%, but all with very low complication rates.5–11 Typical IOP following the Trabectome is in the mid teens, with patients often still requiring IOP-lowering medications to maintain this level of IOP control.5–11 Given that this is a relatively low-risk procedure, it has thus far been positioned in the treatment algorithm somewhere between laser trabeculoplasty and trabeculectomy/tube shunt implantation.
Our results indicate that a significant proportion of patients who have failed tube shunt implantation will achieve substantially improved IOP control with the Trabectome procedure. These patients often still require glaucoma medications to maintain IOP control, and our results show that there is no reduction in medication reliance in these patients.
Also, the Trabectome was notably successful in 2 aphakic patients with failed tube shunts. Although too early to conclude with only 2 aphakic patients in the study, both patients maintained a stable anterior chamber and patent tubes without any vitreous-related complications postoperatively.
There are several limitations to this study. First, this is a retrospective review, with all the inherent applicable considerations. Second, we acknowledge that the results of tube shunt implants rely somewhat on the nature of the glaucoma and inflammatory state of the eye. Therefore, patients of neovascular and inflammatory glaucoma may fail tube shunt at a higher rate than eyes with quiet, open angle glaucoma. Trabectome cannot be performed on eyes with angle closure or neovascular glaucoma, and therefore the results from this study are not applicable to these subsets of glaucoma. Also, the number of subjects in our study was small, and warrants a larger-scale investigation, ideally with longer-term follow-up than 1 year.
Patients with prior failed trabeculectomy and/or tube shunt procedures often fail these procedures as a result of exuberant wound-healing responses, and are poor candidates for further procedures that involve cooperative conjunctiva and Tenon's capsule.12,13 Our results indicate that Trabectome was safe and effective in reducing IOP at 1 year follow-up in patients with prior failed tube shunt surgery, but not effective in reducing medication reliance in these patients. Trabectome may be an appropriate treatment option in many eyes with failed tube shunts, if indicated.
Footnotes
Abbreviations: IOP = intraocular pressure, POAG = primary open-angle glaucoma.
All authors certify that this manuscript is a unique submission and is not being considered for publication by any other source in any medium. Further, the manuscript has not been published, in part or in full, in any form.
Dr. Don S Minckler has been a consultant for NeoMedix.
The other authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Barton K, Feuer WJ, Budenz DL, et al. Three-year treatment outcomes in the Ahmed Baerveldt Comparison Study. Ophthalmology 2014; 121:1547–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christakis PG, Tsai JC, Kalenak JW, et al. The Ahmed versus Baerveldt study: three-year treatment outcomes. Ophthalmology 2013; 120:2232–2240. [DOI] [PubMed] [Google Scholar]
- 3.Syed HM, Law SK, Nam SH, et al. Baerveldt-350 implant versus Ahmed valve for refractory glaucoma: a case-controlled comparison. J Glaucoma 2004; 13:38–45. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Ophtalmology Glaucoma Panel. Primary open-angel glaucoma suspect. Preferred Practice Pattern® Guidelines. San Francisco, CA: American Academy of Ophthalmology; 2010. [Google Scholar]
- 5.Minckler D, Baerveldt G, Ramirez MA, et al. Clinical results with the Trabectome, a novel surgical device for treatment of open-angle glaucoma. Trans Am Ophthalmol Soc 2006; 104:40–50. [PMC free article] [PubMed] [Google Scholar]
- 6.Minckler DS, Baerveldt G, Alfaro MR, et al. Clinical results with the Trabectome for treatment of open-angle glaucoma. Ophthalmology 2005; 112:962–967. [DOI] [PubMed] [Google Scholar]
- 7.Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in the tube versus trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol 2012; 153:789–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahuja Y, Ma Khin Pyi S, Malihi M, et al. Clinical results of ab interno trabeculotomy using the trabectome for open-angle glaucoma: the Mayo Clinic series in Rochester, Minnesota. Am J Ophthalmol 2013; 156:927–935. [DOI] [PubMed] [Google Scholar]
- 9.Francis BA, Minckler D, Dustin L, et al. Combined cataract extraction and trabeculotomy by the internal approach for coexisting cataract and open-angle glaucoma: initial results. J Cataract Refract Surg 2008; 34:1096–1103. [DOI] [PubMed] [Google Scholar]
- 10.Francis BA, See RF, Rao NA, et al. Ab interno trabeculectomy: development of a novel device (Trabectome) and surgery for open-angle glaucoma. J Glaucoma 2006; 15:68–73. [DOI] [PubMed] [Google Scholar]
- 11.Maeda M, Watanabe M, Ichikawa K. Evaluation of trabectome in open-angle glaucoma. J Glaucoma 2013; 22:205–208. [DOI] [PubMed] [Google Scholar]
- 12.Lockwood A, Brocchini S, Khaw PT. New developments in the pharmacological modulation of wound healing after glaucoma filtration surgery. Curr Opin Pharmacol 2013; 13:65–71. [DOI] [PubMed] [Google Scholar]
- 13.Seibold LK, Sherwood MB, Kahook MY. Wound modulation after filtration surgery. Surv Ophthalmol 2012; 57:530–550. [DOI] [PubMed] [Google Scholar]


