Abstract
Although the effectiveness of mass screening for gastric cancer remains controversial, several countries with a high prevalence of gastric cancer have implemented nationwide gastric cancer screening programs. This study was conducted to assess trends in the use of either upper gastrointestinal series (UGIS) or endoscopy to screen for gastric cancer, as well as to assess factors strongly associated with changes therein, over a 10-year period.
Data were obtained from the National Cancer Screening Program (NCSP) database from 2002 to 2011 in Korea. The NCSP provides biennial gastric cancer screening with either UGIS or endoscopy for men and women aged ≥40 years. Using the NCSP database, overall screening rates for gastric cancer and percentages of endoscopy use among participants were analyzed from 2002 to 2011. To estimate changes in participation rates and endoscopy use over time, we assessed the average annual percentage change (APC) by comparing the rates from 2002 and 2011 as relative rates.
Participation rates for gastric cancer screening increased 4.33% annually from 2002 to 2011. In terms of screening method, a substantial increase in endoscopy use was noted among the gastric cancer screening participants over the 10-year period. The percentage of participants who had undergone endoscopy test increased from 31.15% in 2002 to 72.55% in 2011, whereas the percentage of participants who underwent UGIS decreased tremendously. Increased endoscopy test use was greatest among participants aged 40 to 49 (APC = 4.83%) and Medical Aid Program recipients (APC = 5.73%). Overall, men, participants of ages 40 to 49 years, and National Health Insurance beneficiaries of higher socioeconomic status were more likely to undergo screening via endoscopy.
This study of nationwide empirical data from 2002 to 2011 showed that endoscopy is increasingly being used for gastric cancer screening in Korea, compared with UGIS. Nevertheless, further study of the impact of endoscopy on gastric cancer mortality is needed, and future evaluations of screening methods should take into account both cost and any associated reduction in gastric cancer mortality.
INTRODUCTION
Although the incidence of gastric cancer is declining in most developed countries, it is still the most burdensome disease in East Asian countries. About 1 million new cases of gastric cancer occurred in 2012, making it the fifth most common malignancy worldwide.1 More than 70% of these new cases occurred in developing countries, and nearly half occurred in East Asia (mainly China, Japan, and Korea).1 In the Republic of Korea, despite a decline in incidence in recent decades, gastric cancer remains the second most common cancer and the third leading cause of cancer death.2
In countries with a high prevalence of gastric cancer, such as China, Japan, and Korea, gastric cancer screening is common. Beginning in the 1960s, Japan implemented mass gastric cancer screening with photofluorography (via indirect upper gastrointestinal series [UGIS]) to facilitate early detection and, thereby, improvements in survival and cure rates.3–5 Recently, endoscopy has replaced photofluorography as an initial screening method for population-based screening in several cities in Japan, due to its high detection rate.6 Niigata City has utilized endoscopy in its population-based screening program since 2003, and a study conducted in Niigata showed that the detection of gastric cancer by endoscopy was about 2.7 to 4.6 times higher than that by photofluorography or UGIS (also called barium meal x-rays of the upper gastrointestinal tract, which are medical radiographic tests used to examine the gastrointestinal tract for abnormalities).6 In China, although gastric cancer is the second most common cancer, nationwide cancer screening programs do not exist. Nevertheless, endoscopy is widely available at outpatient clinics as part of opportunistic screening programs in major cities.7 In Korea, population-based screening for gastric cancer was implemented in 2002 as part of the National Cancer Screening Program (NCSP), based on national guidelines established in 2001. As stipulated by the NCSP, people ≥40 years are eligible for screening via UGIS or endoscopy biennially.
Although the effectiveness of mass screening for gastric cancer remains controversial, understanding individual experiences with a particular gastric cancer screening method may help when developing gastric cancer screening programs. Accordingly, we attempted to assess the rates of gastric cancer screening by either UGIS or endoscopy and outline trends in the use of the 2 gastric cancer screening procedures in Korea over a 10-year period. In addition, we also examined factors strongly associated with changes therein.
MATERIALS AND METHODS
Study Population
We performed a prospective cross-sectional study. Data from 2002 to 2011 were obtained from the NCSP database, which contains information on Medical Aid Program (MAP) recipients and on National Health Insurance (NHI) beneficiaries invited to participate in the NCSP. The NCSP provides biennial gastric cancer screening with either UGIS or endoscopy for men and women aged ≥40 years. In the NCSP, all eligible men and women biannually receive an invitation letter, along with information on screening methods and the locations of screening units, from the National Health Insurance Service (NHIS), beginning in January of each year. The letter describes which screening methods are offered by the individual screening units and provides contact information for making a reservation. Individuals invited to participate in the NCSP for gastric cancer can choose to undergo either UGIS or endoscopy screening at any one of the clinics or hospitals designated as a gastric cancer screening unit by the NHIS. Until 2007, all clinics and hospitals designated by the NHIS as a gastric cancer screening unit was required to possess both endoscopic and UGIS equipment and at least 1 full-time medical doctor trained in UGIS or endoscopy, as well as a nurse and a radiographer. However, in 2008, in an effort to improve accessibility to gastric cancer screening, the NHIS only required clinics and hospitals to have endoscopic equipment for designation as a gastric cancer screening unit. Thus, nowadays, designated gastric cancer screening units may offer either both endoscopy and UGIS or endoscopy only.
In 2002, MAP and NHI beneficiaries in the 20% income bracket were eligible for gastric cancer screening free of charge, whereas the remaining NHI beneficiaries were eligible for gastric cancer screening with a copayment of 50% of the cost of the procedure. In 2003, the NCSP expanded gastric cancer screening free of charge to NHI beneficiaries within the 30% income bracket, and in 2005, the target population was further expanded to include NHI beneficiaries in the lower 50% income bracket. Also, the NCSP reduced the copayment amount for gastric cancer screening for the upper 50% of NHI beneficiaries in 2006 from 50% to 20%, and in 2010, the copayment was further reduced to 10%. The number of people invited to participate in the NCSP was 9,586,636 in 2002, 9,769,848 in 2003, 10,307,841 in 2004, 10,519,431 in 2005, 12,409,695 in 2006, 12,180,367 in 2007, 13,336,515 in 2008, 13,083,242 in 2009, 12,703,485 in 2010, and 12,985,842 in 2011.
This study utilized data collected from the NCSP database, including demographic characteristics of individuals invited to participate in the NCSP, the test results of the gastric cancer screening participants, and written informed consent given by participants for the collection of their screening results and health data. We collected these data regularly from the NHIS. For this reason, obtaining informed consent for this specific study was waived because of the large size of the NCSP database. This study was approved by the Institutional Review Board of the National Cancer Center, Korea.
Using the NCSP database, socioeconomic status was categorized into 3 groups according to health insurance type: MAP recipients (extremely poor people who received livelihood assistance and were unable to pay for health care or insurance), NHI beneficiaries of low-income status (target population for the NCSP at free of charge), and NHI beneficiaries of high-income status (target population for the NCSP with copayment). We excluded 7431 participants (0.05% of total screening cases) because of missing information on screening method. The final number of participants comprised 709,580 for 2002, 1,024,669 for 2003, 1,218,030 for 2004, 1,861,805 for 2005, 2,854,893 for 2006, 3,341,847 for 2007, 4,242,954 for 2008, 4,715,073 for 2009, 5,038,088 for 2010, and 5,895,113 for 2011.
Statistical Analysis
Overall screening rates for gastric cancer from 2002 to 2011 were analyzed according to sex, age, and socioeconomic status based on insurance status. Percentages of endoscopy use among participants were also measured during this period. To estimate changes in participation rates and endoscopy use over time, we assessed the average annual percentage change (APC) by comparing the rates from 2002 and 2011 as relative rates. These risks are reported as the average APC ([relative risk − 1] × 100/number of years) with 95% confidence intervals (CIs).
Furthermore, we fit multivariable logistic regression models with generalized estimating equations to identify significant factors associated with choosing endoscopy over UGIS as an initial gastric cancer screening method in years 2002, 2005, 2008, and 2011 with the independent variables of sex, age, and socioeconomic status. Also, the Wald statistic was calculated to determine the P value of the heterogeneity of the odds ratios (ORs). For the pooled ORs from 2002 to 2011, we categorized the calendar year into 4 periods (2002–2004, 2005–2007, 2008–2009, and 2010–2011) to reflect changes in screening policies in Korea in multivariable logistic regression analysis. All statistical analyses were conducted using SAS statistical software (version 9.2; SAS Institute Inc., Cary, North Carolina, USA).
RESULTS
Participation Rates for Gastric Cancer Screening
Overall, gastric cancer screening rates continuously increased from 2002 to 2011 (Table 1). The participation rates increased from 7.40% in 2002 to 45.40% in 2011, for a 38% increase over the 10-year period. Overall, participation rates were higher for women than for men and highest in those aged60 to 69 years. Initially, until 2005, NHI beneficiaries of lower socioeconomic status showed the highest participation rates, after which NHI beneficiaries of higher socioeconomic status showed the highest participation rates.
TABLE 1.
Participation Rates of Gastric Cancer Screening Via the National Cancer Screening Program in Korea From 2002 to 2011
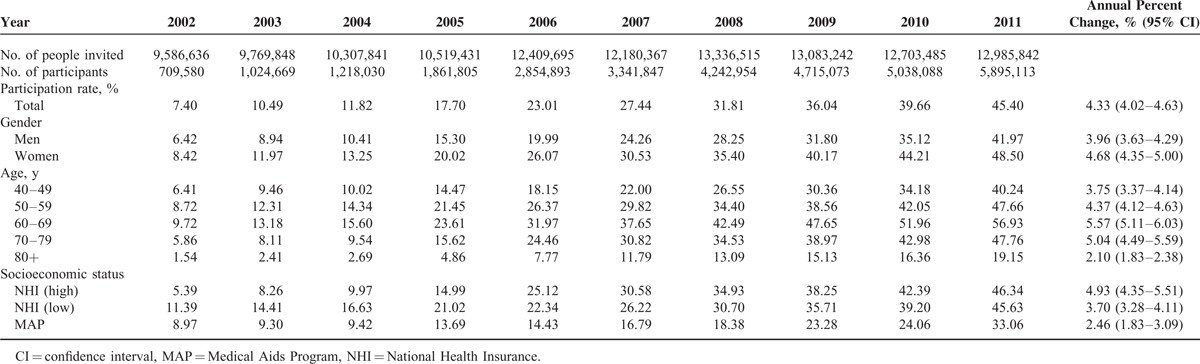
The APC in participation rates between 2002 and 2011 was 4.33% (95% CI = 4.02–4.63) (Table 1). Individuals aged 60 to 69 years showed the highest APC (5.57%) in participation rates, followed by those aged 70 to 79 (5.04%), 50 to 59 (4.37%), and 40 to 49 years (3.75%). Furthermore, female participants (APC = 4.68%) and NHI beneficiaries of higher socioeconomic status (APC = 4.93%) showed a higher APC than the average for this study.
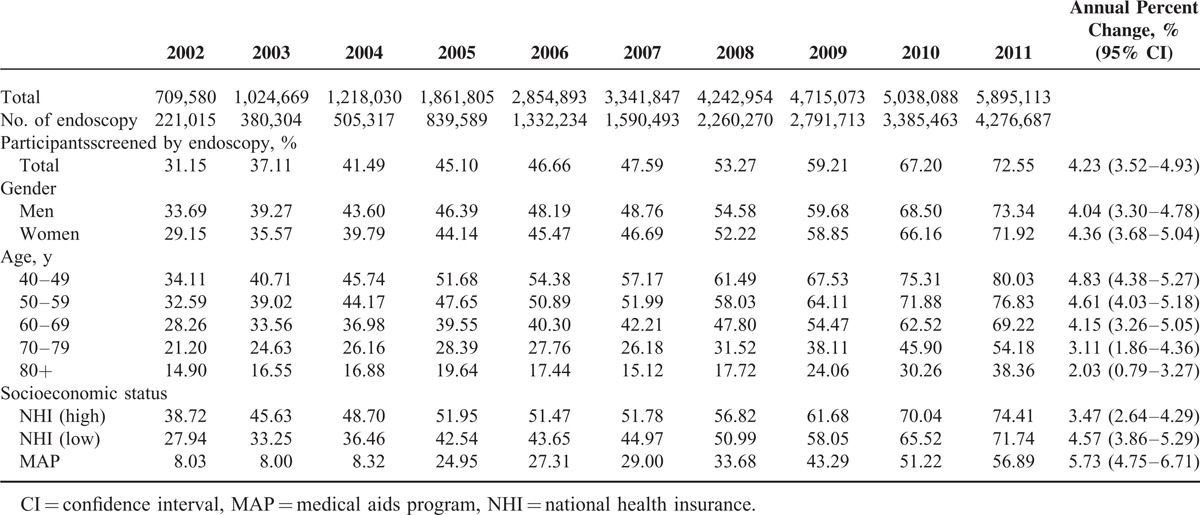
Trends of Gastric Cancer Screening Method
In addition to stable increases in gastric cancer screening rates, the percentage of participants who underwent endoscopy for gastric cancer screening dramatically increased between 2002 and 2011 (Table 2). The percentage of participants who had undergone endoscopy in 2002 was 31.15%, increasing to 72.55% in 2011. In contrast, the percentage of participants who had undergone UGIS significantly decreased (68.85% in 2002 and 32.8% in 2011). Between 2002 and 2011, the participants who had undergone endoscopy test increased by about 4.23% per year (95% CI = 3.52–4.93). The increase was greater among participants aged 40 to 49 (APC = 4.83%) and MAP recipients (APC = 5.73%). Overall, men, participants of ages 40 to 49 years, and NHI beneficiaries of higher socioeconomic status were most likely to opt for gastric cancer screening via endoscopy.
TABLE 2.
Percentage of Participants Who Underwent Endoscopy Via the National Cancer Screening Program in Korea From 2002 to 2011
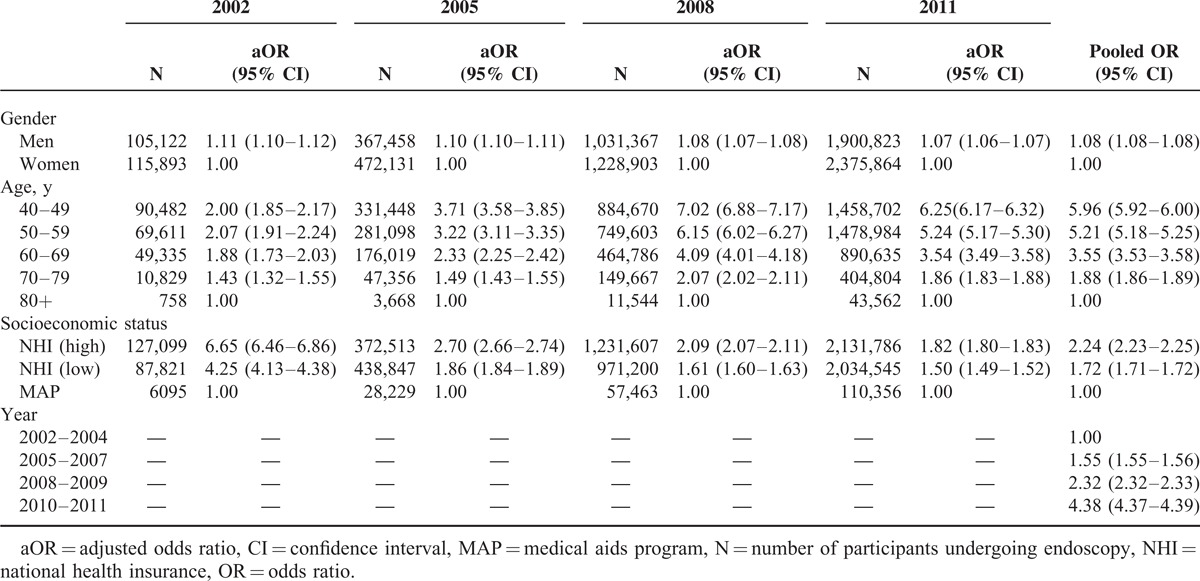
Factors Associated With Endoscopy Use
In terms of adjusted OR (95% CI) of undergoing endoscopy test among gastric cancer participants, men were slightly more likely to undergo endoscopy than women each year (Table 3). The adjusted ORs in men slightly decreased from 1.11 (95% CI = 1.10–1.12) in 2002 to 1.07 in 2011 (95% CI = 1.06–1.08). In addition, participants of younger age were significantly more likely to undergo endoscopy test than participants of older age: individuals aged 40 to 49 and 50 to 59 years showed significantly higher odds of undergoing endoscopy than those aged ≥80 years. Also, the ORs between age groups tended to increase over the 10-year period. In 2002, individuals aged 40 to 49 years were 2 times more likely to undergo endoscopy test than those aged ≥80, whereas in 2011, this likelihood increased to 6.25 times. Also, NHI beneficiaries of higher income status were more likely to undergo for gastric cancer screening via endoscopy. Nevertheless, the odds of undergoing endoscopy between individuals of differing socioeconomic status decreased significantly from 6.65 (95% CI = 6.46–6.86) in 2001 to 1.82 (95% CI = 1.80–1.83) in 2011. To reflect changes in screening policies in Korea, the adjusted ORs were computed according to 4 periods categorized according to calendar year. Taking the period of 2002 to 2004 as the reference period, the adjusted ORs were 1.55 (95% CI = 1.55–1.56) for 2005 to 2007, 2.32 (95% CI = 2.32–2.33) for 2008 to 2009, and 4.38 (95% CI = 4.37–4.39) for 2010 to 2011.
TABLE 3.
Adjusted Odds Ratio of Undergoing Endoscopy in the National Cancer Screening Program in Korea, 2002–2011
DISCUSSION
In this study, we assessed participation rates for the population-based nationwide gastric cancer screening program in Korea from 2002 to 2011. During this period, participation rates for gastric cancer screening annually increased by 4.33%. The participation rate increased the most (5.9 percentage points) between 2004 and 2005, when the target population for free-of-charge screening was expanded from NHI beneficiaries in the lower 30% income bracket to those in the lower 50% income bracket. This expansion of the target population, who were able to undergo gastric cancer screening at no charge, might have affected this increase in the overall participation rate. The current analysis also showed that the amount of copayment of the cost for undergoing gastric cancer screening might affect participation rates among NHI beneficiaries of higher socioeconomic status. Among the results of this study, participation rates increased by 10 percentage points between 2005 and 2006, when the copayment for individuals of higher socioeconomic status was reduced from 50% to 20%. These results suggest that the introduction of free gastric cancer screening and mitigation of screening costs induced a substantial increase in participation rates. Nevertheless, while overall participation rates increased annually, participation rates and APC in MAP recipients were the lowest among the 3 socioeconomic groups. This finding suggests that not only financial support but also other social support might be needed to increase participation rates among underprivileged individuals.
Along with increases in the overall participation rates of gastric cancer screening, we also noted a substantial increase in the use of endoscopy to conduct gastric cancer screening over the 10-year study period. The percentage of participants who had undergone endoscopy tests increased from 31.15% in 2002 to 72.55% in 2011, whereas the percentage of participants who underwent UGIS decreased dramatically. In a previous report in Korea, the majority of respondents preferred endoscopy for gastric cancer screening and indicated preference for endoscopy in any future gastric cancer screening that they might undergo.8 In general, individuals may show preference for a particular screening method over another based on features they deem most valuable. For example, previous studies on colorectal screening suggested that individuals showed preference for a particular method based on its accuracy or its invasiveness: individuals who chose to undergo colonoscopy reported that the accuracy of the test was the most important factor affecting their preference, whereas individuals who preferred noninvasive testing, such as fecal occult blood test, indicated that the invasiveness of the test and psychological concerns were most important.9–11 Among gastric cancer screening strategies, the same may be true. Numerous studies have examined the accuracy of endoscopy in detecting cancer.6,12–18 Recently, 2 studies compared the accuracies of radiographic tests and endoscopy, and both studies showed that endoscopic screening for gastric cancer had a higher sensitivity than radiographic screening, suggesting the greater use of endoscopy in gastric cancer screening.17,18 Thus, users concerned with accuracy may choose endoscopy over UGIS. Conversely, people who are concerned about discomfort and complications with the endoscopic procedure may still choose to undergo UGIS. According to a previous study, people who chose to undergo less invasive tests were associated with concerns for discomfort, complications, and anxiety about procedure.9 In this study, women and participants of older age were more likely to undergo UGIS than men and those of younger age.
Meanwhile, improvement in accessibility to endoscopy testing may be another possible reason for the increased use of endoscopy tests in this study. Early in the 10-year study period, the number of skilled endoscopists was not enough to cover the entire target population across the nation. However, after introduction of the nationwide gastric cancer screening program, a larger number of physicians began to perform endoscopy tests to meet the needs of endoscopic screening services. In 2008, there were >4000 board-certified endoscopic specialists in Korea, members of the Korean Society of Gastrointestinal Endoscopy, and their ranks have been increasing annually with governmental support.12 Furthermore, in 2008, to improve accessibility to gastric cancer screening, the NHIS only required clinics and hospitals to possess endoscopic equipment for designation as a gastric cancer screening unit, instead of both endoscopic and UGIS equipment. With this change, the number of gastric cancer screening units designated by the NHIS increased from 1830 in 2007 to 2418 in 2009.
Also, financial advantages for endoscopy might be associated with the increased use of endoscopy in Korea. Despite the diagnostic advantages of endoscopy, it is more expensive and requires a larger staff and greater technological expertise than radiographic testing in most countries. The cost of endoscopy is reportedly 3 to 4-fold more expensive than radiography testing (photofluorography) in Japan.6,19 However, in Korea, the cost of endoscopy is about the same as radiographic testing (UGIS) (unit costs for endoscopy and UGIS were $34.89 and $32.67, respectively, in 2008).12 Furthermore, with the NCSP, individuals can receive these tests free of charge or at a very low cost.
Also, the possibility of the need for further testing may be another possible reason why individuals choose one method over another. With the NCSP, if a suspicious lesion is detected by UGIS, an endoscopic test must be performed to biopsy the lesion. Thus, in order to avoid having to undergo 2 procedures, individuals may select endoscopy over UGIS, as biopsy can readily be performed during an initial endoscopic screening, if needed. In fact, according to studies on colorectal screening, the possibility of the need for further testing was suggested as a test-specific characteristic that could be a decisive factor in choosing one method over the another.9,10
In this study, a significantly larger number of individuals of ages 40 to 49 and 50 to 59 years underwent endoscopy test than those aged ≥80 years. Potentially, younger individuals may be less worried with the invasiveness of a test and prefer to undergo the most accurate test. In addition, positive experience with endoscopy testing might also increase preference for endoscopy in subsequent tests. A previous study reported that individuals who had received a prior endoscopy test were significantly more likely to prefer endoscopy to UGIS.8 Individuals might experience that endoscopy is less burdensome than anticipated, diminishing their psychological concerns for future tests. Thus, positive attitudes after experiencing endoscopy may bolster increased endoscopic screening rates.
Interestingly, gaps in endoscopy use according to socioeconomic status have been reduced over the past 10 years. Although MAP recipients showed the lowest gastric cancer screening rate and percentage of endoscopy use, the APC in endoscopy use among all socioeconomic status groups was the highest in MAP recipients. This result suggests that preference for endoscopy is less affected by socioeconomic status. Meanwhile, individuals of higher socioeconomic status were still more likely to prefer endoscopy to UGIS, compared with individuals of lower socioeconomic status. This suggests that individuals of higher socioeconomic status may be more knowledgeable of the advantages of endoscopy.
Our study has several limitations. The NCSP database lacks details on why a participant chose endoscopy over UGIS and geographical information. Thus, we were unable to explore the influence of other important correlates, such as test-specific characteristics (e.g., preparation, cost, and concern for discomfort, complications, and anxiety about the procedure) and geographical distribution of gastric cancer screening units, which might have affected the participants’ decisions to choose a particular screening method. Also, we could not examine regional disparity in the use of individual gastric cancer screening methods. Furthermore, this study was conducted as a cross-sectional study to examine trends in the participation rates for gastric cancer screening, and it would be impossible to infer causality therefrom. This study results might not be generalizable in other countries because of differences in health care system and cost of screening tests.
Endoscopy is widely conducted in clinical settings as a part of routine health checkups in countries with a high prevalence of gastric cancer. The results of recent studies suggest that application of endoscopy in gastric cancer screening programs is more cost effective than screening by radiographic tests in average-risk populations.6,12,20,21 Also, the general population is more likely to prefer gastric cancer screening by endoscopy.8 This study showed that endoscopy is increasingly being used for gastric cancer screening in Korea, compared with UGIS, in nationwide empirical data from 2002 to 2011. Accordingly, we suggest that endoscopy test could be considered as an initial screening method for gastric cancer screening. Nonetheless, further study of the impact of endoscopy on gastric cancer mortality is needed, and future evaluations of screening methods should take into account both cost and any associated reduction in gastric cancer mortality.
Footnotes
Abbreviations: APC = annual percentage change, MAP = Medical Aid Program, NCSP = National Cancer Screening Program, NHI = National Health Insurance, NHIS = National Health Insurance Service, UGIS = upper gastrointestinal series.
This study was supported by a Grant-in-Aid for Cancer Research and Control from the National Cancer Center, Korea (Grant numbers: 1010200 and 1310231).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. 2013; Lyon, France: International Agency for Research on Cancer, Available from: http://globocan.iarc.fr, accessed on 11/07/2014. [Google Scholar]
- 2.Jung KW, Won YJ, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat 2014; 46:109–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fukao A, Tsubono Y, Tsuji I, et al. The evaluation of screening for gastric cancer in Miyagi Prefecture, Japan: a population-based case-control study. Int J Cancer 1995; 60:45–48. [DOI] [PubMed] [Google Scholar]
- 4.Mizoue T, Yoshimura T, Tokui N, et al. Prospective study of screening for stomach cancer in Japan. Int J Cancer 2003; 106:103–107. [DOI] [PubMed] [Google Scholar]
- 5.Hisamichi S, Sugawara N, Fukao A. Effectiveness of gastric mass screening in Japan. Cancer Detect Prev 1988; 11:323–329. [PubMed] [Google Scholar]
- 6.Tashiro A, Sano M, Kinameri K, et al. Comparing mass screening techniques for gastric cancer in Japan. World J Gastroenterol 2006; 12:4873–4874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung WK, Wu MS, Kakugawa Y, et al. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol 2008; 9:279–287. [DOI] [PubMed] [Google Scholar]
- 8.Choi KS, Kwak MS, Lee HY, et al. Screening for gastric cancer in Korea: population-based preferences for endoscopy versus upper gastrointestinal series. Cancer Epidemiol Biomarkers Prev 2009; 18:1390–1398. [DOI] [PubMed] [Google Scholar]
- 9.Janz NK, Lakhani I, Vijan S, et al. Determinants of colorectal cancer screening use, attempts, and non-use. Prev Med 2007; 44:452–458. [DOI] [PubMed] [Google Scholar]
- 10.Ling BS, Moskowitz MA, Wachs D, et al. Attitudes toward colorectal cancer screening tests. J Gen Intern Med 2001; 16:822–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeBourcy AC, Lichtenberger S, Felton S, et al. Community-based preferences for stool cards versus colonoscopy in colorectal cancer.screening. J Gen Intern Med 2008; 23:169–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee HY, Park EC, Jun JK, et al. Comparing upper gastrointestinal X-ray and endoscopy for gastric cancer diagnosis in Korea. World J Gastroenterol 2010; 16:245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suzuki H, Gotoda T, Sasako M, et al. Detection of early gastric cancer: misunderstanding the role of mass screening. Gastric Cancer 2006; 9:315–319. [DOI] [PubMed] [Google Scholar]
- 14.Hosokawa O, Hattori M, Takeda T, et al. Hosokawa accuracy of endoscopy in detecting gastric cancer. Jpn J Gastroenterol Mass Survey 2004; 42:33–39. [Google Scholar]
- 15.Hosokawa O, Tsuda S, Kidani E, et al. Diagnosis of gastric cancer up to three years after negative upper gastrointestinal endoscopy. Endoscopy 1998; 30:669–674. [DOI] [PubMed] [Google Scholar]
- 16.Otsuji M, Kouno Y, Otsuji A, et al. Assessment of small diameter panendoscopy for diagnosis of gastric cancer: comparative study with follow-up survey date. Stomach Intestine 1989; 24:1291–1297. [Google Scholar]
- 17.Choi KS, Jun JK, Park EC, et al. Performance of different gastric cancer screening methods in Korea: a population-based study. PLoS One 2012; 7:e50041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamashima C, Okamoto M, Shabana M, et al. Sensitivity of endoscopic screening for gastric cancer by the incidence method. Int J Cancer 2013; 133:653–659. [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto S, Yamasaki K, Tsuji K, et al. Results of mass endoscopic examination for gastric cancer in Kamigoto Hospital, Nagasaki Prefecture. World J Gastroenterol 2007; 13:4316–4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang HS, Park EC, Chung W, et al. Comparing endoscopy and upper gastrointestinal X-ray for gastric cancer screening in South Korea: a cost-utility analysis. Asian Pac J Cancer Prev 2012; 13:2721–2728. [DOI] [PubMed] [Google Scholar]
- 21.Cho E, Kang MH, Choi KS, et al. Cost-effectiveness outcomes of the national gastric cancer screening program in South Korea. Asian Pac J Cancer Prev 2013; 14:2533–2540. [DOI] [PubMed] [Google Scholar]


