Abstract
A retrospective study to evaluate the effectiveness of 3-dimensional rapid prototyping (3DRP) technology in corrective surgery for Lenke 1 adolescent idiopathic scoliosis (AIS) patients.
3DRP technology has been widely used in medical field; however, no study has been performed on the effectiveness of 3DRP technology in corrective surgery for Lenke 1 AIS patients.
Lenke 1 AIS patients who were preparing to undergo posterior corrective surgery from a single center between January 2010 and January 2012 were included in this analysis. Patients were divided into 2 groups. In group A, 3-dimensional (3D) printing technology was used to create subject-specific spine models in the preoperative planning process. Group B underwent posterior corrective surgery as usual (by free hand without image guidance). Perioperative and postoperative clinical outcomes were compared between 2 groups, including operation time, perioperative blood loss, transfusion volume, postoperative hemoglobin (Hb), postoperative complications, and length of hospital stay. Radiological outcomes were also compared, including the assessment of screw placement, postoperative Cobb angle, coronal balance, sagittal vertical axis, thoracic kyphosis, and lumbar lordosis. Subgroup was also performed according to the preoperative Cobb angle: mean Cobb angle <50° and mean Cobb angle >50°. Besides, economic evaluation was also compared between 2 groups.
A total of 126 patients were included in this study (group A, 50 and group B, 76). Group A had significantly shorter operation time, significantly less blood loss and transfusion volume, and higher postoperative Hb (all, P < 0.001). However, no significant differences were observed in complication rate, length of hospital stay, and postoperative radiological outcomes between 2 groups (all, P>0.05). There was also no significant difference in misplacement of screws in total populations (16.90% vs 18.82%, P = 0.305), whereas a low misplacement rate of pedicle screws was observed in patients whose mean Cobb angle was >50° (9.15% vs 13.03%, P = 0.02). Besides, using 3DRP increased the economic burden of patients (157,000 ± 9948.85 Ren Min Bi (RMB) vs 152,500 ± 11,445.52 RMB, P = 0.03).
Using the 3D printing technology before posterior corrective surgery might reduce the operation time, perioperative blood loss, and transfusion volume. There did not appear to be a benefit to using this technology with respect to complication rate and postoperative radiological outcomes; however, 3D technology could reduce the misplacement rate in patients whose preoperative mean Cobb angle was >50°. Besides, it also increased the patients’ hospital cost. Therefore, future prospective studies are needed to elucidate the efficacy of this emerging technology.
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) is defined as a 3-dimensional (3D) deformity that consists of a side curve, deviation of the sagittal spinal profile, and vertebrae rotation in the transverse plane, with an overall prevalence of 0.5% to 5.2%.1 Recently, pedicle screws have become increasingly popular to correct the coronal and sagittal deformity in the surgical correction of scoliotic deformities, as pedicle screws have relatively superior major curve correction and biomechanical properties.2 However, due to the vertebrae rotation in the transverse plane, screw misplacement has been reported when pedicle screws are misplaced, with an incidence of 20% to 30%; and 1% of these patients suffered from neurovascular complications that may lead to severe consequences, such as paralysis.3,4 Although several methods and surgical techniques have been used to reduce misplacement rate and neurovascular complications, such as 3D computed tomography (CT) reconstruction of spine and increased experiences of surgeons, these techniques have had only limited effects.5
3D printing, as a new technology, which was invited by Enrico Dini, has the potential to dramatically change the field of medicine and improve patient-specific surgical planning. Recently, 3D prototyping technology has been widely used in medical field, involving in clinical practice during preoperative planning, procedure rehearsal, custom prosthetic design, and being used as an educational tool for teaching and doctor–patient communication.6–9 Gear et al10 used 3D prototyping technology and 3D printer to investigate rapid prototyping technology for the production of patient-specific, cost-effective liquid fillable phantoms directly from patient CT data, and they thought that the organ geometry showed good correspondence with anatomical references. Dankowski et al11 provided a description of 3D printing as a clinically applicable heart modeling technology for the planning of percutaneous structural heart procedures, and they thought that 3D printing was a helpful tool in individualized planning for percutaneous structural interventions. In our opinion, 3D printing could also be applied in orthopedics, such as preoperative simulation to reduce the complications and prosthetic models for joint replacement.
With regard to scoliosis, the study by Mao et al12 involved 16 cases of complex severe spinal deformity, and preoperative 3D reconstruction and rapid prototyping were applied. In their opinion, the use of computer-designed polystyrene models could provide more accurate morphometric information and facilitate surgical correction of complex severe spinal deformity. However, no studies were performed to detect the effectiveness of 3D prototyping technology in AIS patients. Therefore, we conducted this retrospective study to determine whether 3D prototyping technology could minimize the misplacement rate, reduce the neurovascular complications, and also detect the radiological and economical outcomes of AIS patients who received 3D printing before the surgery.
MATERIALS AND METHODS
This study was approved by the institutional review board of our hospital, and all patients gave written informed consent to participate. Data from 126 AIS patients who underwent posterior corrective surgery from January 2010 to January 2012 in our hospital were reviewed and collected. The inclusion criteria were as follows: patients were diagnosed as AIS who needed to receive posterior corrective surgery; the curves were all double curves (thoracic and thoracolumbar/lumbar curve), which were classified as Lenke 1. Other scoliosis, such as neuromuscular scoliosis and degenerative scoliosis, and other subtypes of AIS were excluded by medical history, physical examinations, or radiological examinations. Subjects were divided into 2 groups based on whether or not the surgery was performed with the aid of 3D printing technology. Patients in group A (n = 50) had their deformed spine prototyped with the 3D printing technology prior to undergoing posterior corrective surgery, and patients in group B (n = 76) underwent posterior corrective surgery as usual (by free hand without the use of 3D printing during preoperative period). All the surgeries were performed by a surgical team in our department, in which 3 senior and experienced surgeons were included. All patients had a minimum of 2 years follow-up.
3D prototyping was performed by creating subject-specific models on a 3D printer prior to posterior corrective surgery (Figure 1). In brief, the patients’ deformed spine was scanned using an Aquilion ONE 640 CT scanner (TOSHIBA, Japan) with a slice thickness of 0.5 mm. These images were converted to stereolithographic (STL) files by computer-aided software and reconstructed to a 3D model, which was used as a blueprint for the procedure. An STL apparatus that used selective laser sintering was used to build a computer-designed 3D polystyrene model of the spine. The final model retained all details of the internal and external spinal structure. All the surgeries were performed in both groups regarding screw placement by free hand. Moreover, these 3D models were used in the pre- and perioperative periods to aid in the operation. In particular, the models created for each subject in group A were used to plan surgical procedure by observing any complex or abnormal structures, and simulative surgery of screws implantation was also conducted.
FIGURE 1.
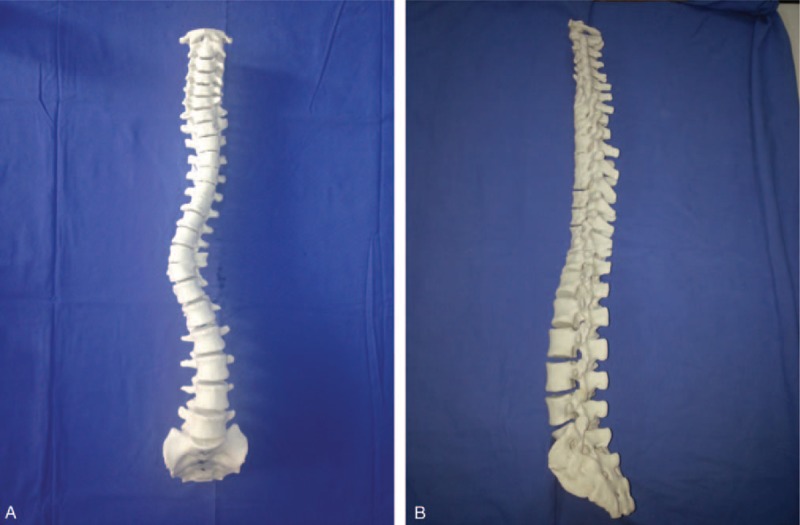
Representative spine model printed by 3D printer, (a) the coronal plane of model, (b) the sagittal plane of model. 3D = 3-dimensional.
Radiographic and clinical outcomes were collected and compared between the 2 groups preoperatively, perioperatively, and at final follow-up. Perioperative metrics included operation time, blood loss in operation, and transfusion volume, whereas postoperative hemoglobin (Hb), length of hospital stay, complications, and hospital cost were also compared between 2 groups. As to the evaluation of screw placement, a new grading system was used to assess the accuracy of screw placement through the CT scan after operation.13 The following types of misplacement were included in the analysis: medial cortical perforation (MCP), lateral cortical perforation (LCP), anterior cortical perforation (ACP), endplate perforation (EPP), and foraminal perforation (FP).14 Screws with grade 1 MCP and grade 1 LCP were regarded as screws with partial cortical perforation. Screws with grade 2 MCP, grade 2 LCP as well as screws with ACP, EPP, and FP were regarded as screws with total cortical perforation.13,14 Besides, radiological evaluations, such as mean and secondary Cobb angle, coronal balance, sagittal vertical axis (SVA), thoracic kyphosis, and lumbar lordosis were also assessed at final follow-up.
STATISTICAL ANALYSIS
Paired sample t tests were conducted to analyze the differences between preoperative and postoperative radiological parameters within groups. Independent 2-sample t tests were used to compare differences of the variables between 2 groups. Categorical variables were compared using χ2 or Fisher exact test. All statistical assessments were 2-sided, and a P value of <0.05 was considered to be significant. Statistical analyses were performed using SPSS 19.0 statistics software (SPSS Inc, Chicago, IL).
RESULTS
Group A included 50 patients (M:12, F:38) with a mean age of 12.52 ± 5.45 years, and group B included 76 patients (M:33, F:43) with a mean age of 12.11 ± 6.42 years. The average number of instrumented screws was 14.14 ± 1.96 in Group A and 13.66 ± 1.86 in Group B (P = 0.17). Patients were also divided into subgroups according to the preoperative mean Cobb angle: <50° (group A, 23; group B, 33) and <50° (group A, 27; group B, 43). There were no differences in baseline characteristics and patient demographics between groups (all, P > 0.05) (Table 1).
TABLE 1.
Patient Demographics and Characteristics at Baseline
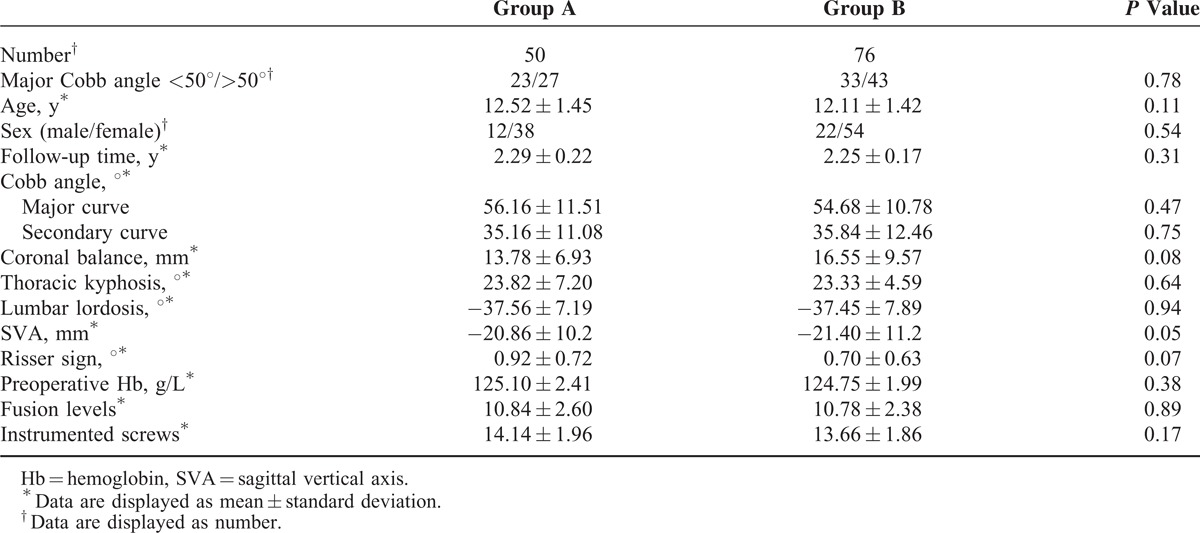
Operation time, blood loss, transfusion volume, length of hospital stay, postoperative Hb, and the complications of both groups were presented in Table 2. There were significant differences in operation time (184.32 ± 4.65 minutes vs 212.32 ± 8.17 minutes, P < 0.001), blood loss (846.68 ± 26.11 mL vs 1029.65 ± 72.18 mL, P < 0.001), transfusion volume (827.48 ± 24.67 mL vs 985.32 ± 74.34 mL, P < 0.001), and postoperative Hb (118.22 ± 3.43 g/L vs 115.15 ± 2.50 g/L, P < 0.001) between groups, with the 3D group (group A) showing a shorter operation time and less blood loss. However, no significant difference was observed in length of hospital stay (11.92 ± 1.10 days vs 12.24 ± 1.13 days, P = 0.12). Although group A showed a low incidence rate of complications than group B (8% vs 14.47%), there was no significant difference between 2 groups (P = 0.34). Furthermore, hospital cost in group A was more expensive than that in group B (157,000 ± 9948.85 Ren Min Bi (RMB) vs 152,500 ± 11,445.52 RMB, P = 0.03). Besides, the complications in group A and group B are also summarized in Table 2.
TABLE 2.
Comparability of the Operation Time, Blood Loss, Transfusion Volume, Postoperative Hb, Complications, and Hospital Cost Between 2 Groups
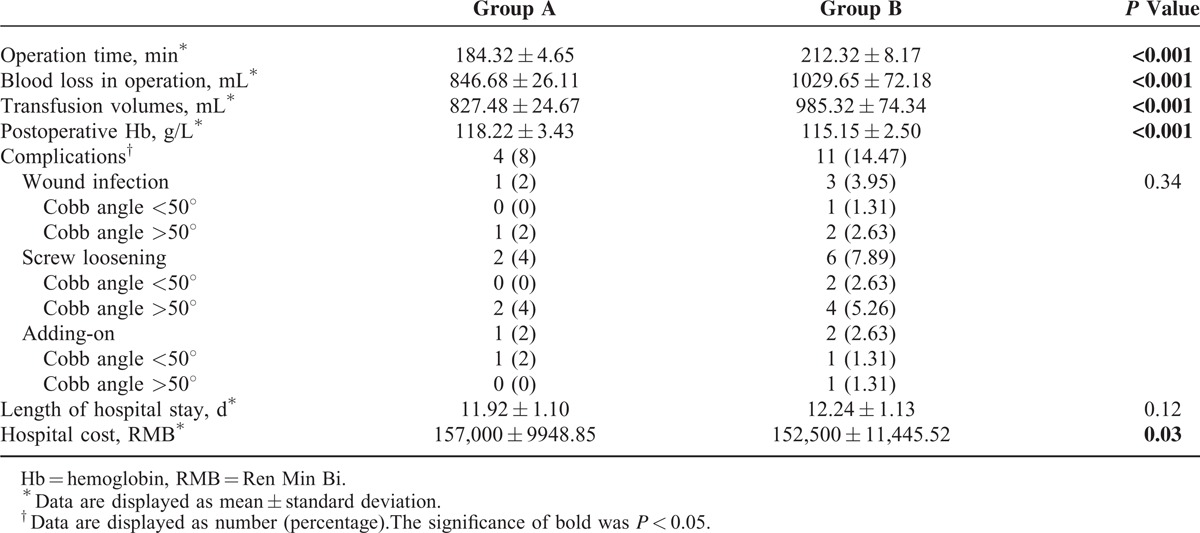
With regard to the accuracy of screw placement, the total misplacement rate of screws was 16.90% (120/710) in group A and 18.82% (195/1036) in group B, whereas no significant difference was observed between the 2 groups (P = 0.305). When stratified by mean Cobb angle, group A showed a lower misplacement rate compared with group B in patients whose mean Cobb angle was >50° (9.15% vs 13.03%, P = 0.02); however, no significant difference was observed in patients whose mean Cobb angle was <50° (8.03% vs 5.89%, P = 0.132), as shown in Table 3.
TABLE 3.
Results of the Radiological Assessment of Pedicle Screw Placement Between 2 Groups
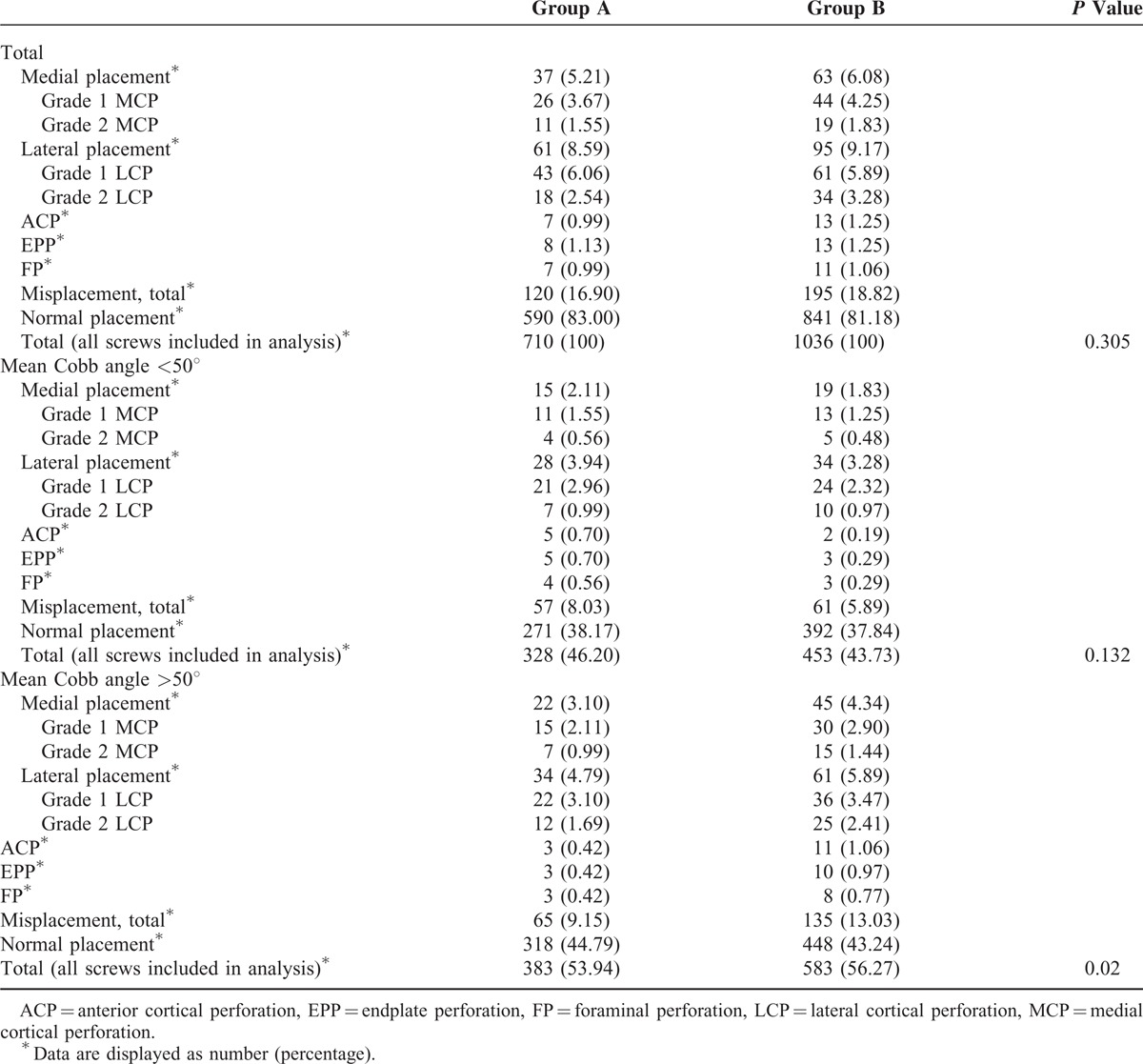
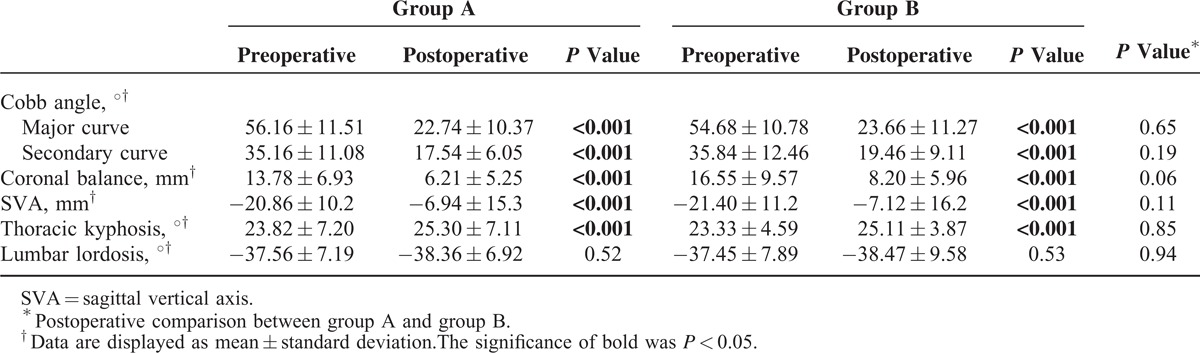
As shown in Table 4, both mean Cobb angle and secondary Cobb angle decreased significantly within 2 groups at final follow-up, respectively (all, P < 0.05); however, no significant difference was observed in either mean Cobb angle or secondary Cobb angle between the 2 groups (major curve, P = 0.65; secondary curve, P = 0.19). Coronal balance and SVA also improved significantly at final follow-up within the 2 groups (both, P < 0.001), whereas there were no significant differences between the 2 groups (P = 0.06 and P = 0.11, respectively). Thoracic kyphosis of both groups increased significantly at final follow-up (both, P < 0.001); however, no significant difference was observed between the 2 groups at final follow-up (25.30 ± 7.11° vs 25.11 ± 3.87°, P = 0.85). Besides, lumbar lordosis was slightly increased with 0.8° in group A (P = 0.52) and 1.02° in group B (P = 0.53), whereas the lumbar lordosis angle at final follow-up was not significantly different between the 2 groups (P = 0.94).
TABLE 4.
Preoperative and Postoperative Radiological Outcomes Between Group A and Group B
A typical case is shown in Figure 2.
FIGURE 2.
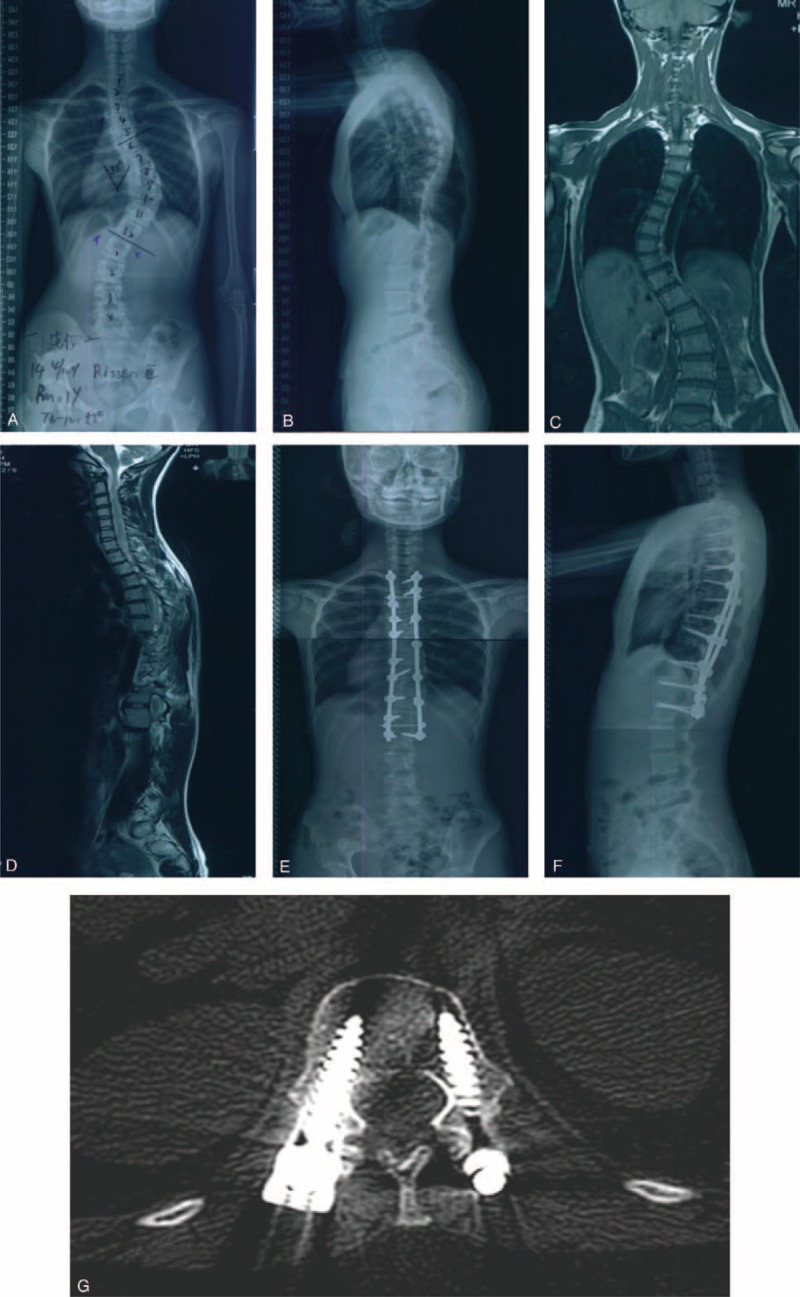
A female patient who received the 3D printing technology before the surgery. Preoperative radiographs anteroposterior (A) and lateral (B) views of a 14-year-old Lenke 1 AIS patient with a major Cobb angle of 55° and secondary Cobb angle of 38°, and the 3D prototyping technology was used before the surgery. (C) and (D) were the coronal and sagittal film of preoperative magnetic resonance imaging, showing no abnormality in spinal cord. Postoperative radiographs were shown in (E) and (F), showing the major Cobb angle and secondary Cobb angle after operation was 18° and 11°, respectively, and the correction rate was 67.27% and 71.05%, respectively. Postoperative CT scan (G) showed the accurate position of pedicle screws. 3D = 3-dimensional, AIS = adolescent idiopathic scoliosis, CT = computed tomography.
DISCUSSION
Pedicle screws in spine surgery has been trusted and applied by majority of the orthopedic surgeons and neurosurgeons; however, screw misplacement is a major concern for them due to its severe neurovascular complications,3,4 especially for AIS corrective surgery due to the complex structure of deformed spine, including the major and secondary curves, deviation of the sagittal spinal profile, and vertebrae rotation in the transverse plane. To decrease the incidence rate of misplacement and neurovascular complications, several computer imaging programs have been applied in the AIS corrective surgery, such as 3D CT reconstruction,15 intraoperative navigation systems,16 and patient-specific drill template with preplanned trajectory.17 Although 3D reconstruction was required to obtain comprehensive information about complex severe spinal deformities, CT 3D reconstruction could only be monitored on the CT working station from any direction and angle, lacking tactile view.12 Besides, the pedicle violation was also observed in 11.4% of the navigation group,16 which might lead to the controversy over the accuracy of navigation system. Therefore, more complex images should be acquired, stored, manipulated, and displayed to provide more precise information of the deformed spine for surgeons in AIS corrective surgery.
The 3D print rapid prototype technique provides detailed and subject-specific information of bony defects and osteophytes. This enhances preoperative planning and practice, and allows the surgeon to simulate surgical procedures given the person's individual anatomy. In the study by Wu et al,18 62 patients with congenital scoliosis were divided into 2 groups. One group underwent surgical correction with the assistance of intraoperative fluoroscopy, and the other group underwent surgery with the assistance of 3D rapid prototyping (3DRP). The results suggested that 70 of the 677 inserted screws were found to be misplaced, showing an overall accuracy of 89.7%, and significantly different screw misplacement rate was observed between 2 groups. These authors concluded that the rapid prototype technology reduced operation time and the lowered the risk of screw misplacement and subsequent complications. Besides, other authors also reported that the technology was beneficial in developing a surgical plan, improved intraoperative navigation, and enhanced patient education.6,7 To reduce the incidence rate of screw misplacement maximally in AIS surgery, a retrospective study was conducted to investigate the effectiveness of 3D prototyping technology in AIS surgery, and the clinical and radiological outcomes were also observed.
In our study, group A showed less operation time, blood loss, transfusion volumes, and higher postoperative Hb than group B (all, P < 0.001), whereas no significant difference in length of hospital stay was observed (P = 0.12), suggesting that using 3D prototyping technology to do the simulative surgery could save much more operation time and postoperative Hb and reduce the intraoperative blood loss and transfusion volumes. We attributed these results to simulative surgery by using 3D prototyping technology, in which simulative screw implantation were conducted, and the positions of screws could be corrected if we found the screws were in inappropriate positions. Therefore, the accuracy of screws implanting in the surgery was increased and low rate of reimplantation of pedicle screws would be reached, leading to less intraoperative blood loss and transfusion volumes. Besides, hospital cost was higher in patients who received the 3D printing before their surgeries than control subjects (P = 0.03) because they were required to pay the money of 3D prototyping models, which might lay the burden on the poor families.
As to the complications, although the incidence of complications in group B was higher than in group A (14.47% vs 8%), no significant difference was observed between the 2 groups (P = 0.34). The relatively small sample size might be an important reason. Wound infection happened in 3 patients in group B (3.95%), whereas only 1 patient suffered wound infection (2%). In our opinion, longer operation time and longer time of exposure on the bacteria environment might be an important contributor to this difference. Screw loosening is also a major concern for orthopedic surgeons, which might be related to patient's age, sex, weight bearing forces, and probably muscular forces.19 Abul-Kasim et al19 studied 81 AIS patients to evaluate the incidence of loosening (implant failure) evaluated with low-dose CT 2 years following scoliosis surgery, and their results showed that 47 of the 1666 (2.8%) screws showed evidence of loosening. However, other studies reported a wide range of incidence of screw loosening, from 7%20 to 19.5%.21 In our study, the incidence of screw loosening was 4% in group A and 7.89% in group B. Doing simulative surgery by using 3D printing technology helps the pedicle screws to be implanted into the correct position, by which great mechanic forces in the pedicle could be provided, and other factors, such as less destruction of anterior, medial, and posterior volumes of spine could also contribute to this difference. With regard to adding-on phenomenon, Wang et al22 reviewed their risk factors in their series of 278 consecutive patients with AIS, in which 45 patients suffered the adding-on phenomenon (16.19%). Cho et al23 reported that the incidence of adding-on phenomenon was 20.51% at the final follow-up (40/195). Our results showed that 3 patients suffered adding-on, and the incidence of adding-on phenomenon was 2.38%, which was less than in other studies.22,23 Short follow-up time, the correct selection of lowest instrumented vertebra (LIV), and the accuracy of screw implantation might be important contributors to our results.
As to screw misplacement, Dede et al24 studied 559 AIS patients to evaluate the incidence of screw misplacement and postoperative neurological symptoms following a free-hand pedicle screw insertion technique in AIS surgery. In their study, 481 patients with a 5923 pedicle screws met the inclusion criteria. Six patients were found to have pedicle screw malposition (1.25%) and 3 of these patients underwent revision surgery (0.62%). In the study by Abul-Kasim and Ohlin,5 5 types of misplacement were recorded in 116 AIS patients, and the results suggested that the rate of screw misplacement for the whole study was 14%, and the rate of lateral and MCP was 7% and 5%, respectively. In our study, the total misplacement rate of screws was 16.90% in group A and 18.82% in group B. This frequency was similar to the study by Abul-Kasim et al,14 whereas the total misplacement rate of screws in group B (by free hand without any guidance) is higher than the study by Lehman et al,25 in which the overall accuracy of acceptable screws using the free-hand pedicle screw placement technique in the deformed spine was 89.5%, without any neurologic, vascular, or visceral complications over an 8-year period. In our opinion, the surgical experience of the surgeons was a major contributor to this difference. Furthermore, our study showed that 3D prototyping technology could decrease the rate of screw misplacement in patients whose major Cobb angle was >50°, whereas in total population and patients whose major Cobb angle was <50°, no significant differences were observed. In our clinical experience, this higher incidence of screw misplacement in the scoliosis surgery attributed to the complex structure of deformed spine, including the vertebrae rotation in the transverse plane, the hypoplasia of pedicle screws, and spinal canal. Understanding the subject-specific and potentially abnormal anatomy in subjects undergoing scoliosis surgery might help to reduce occurrence of screw misplacement. In our study, we did not see a significant reduction in screw misplacement in our subjects whose major Cobb angle was <50°. Insignificant differences of structures of deformed spine, Cobb angle, and the vertebrae rotation in the transverse plane between AIS patients whose major Cobb angle was <50° and control subjects might be important factors to our results. In addition, the cases in which 3DRP was not used still underwent subject-specific preoperative planning with CT images, which the operating surgeons were accustomed to using during preoperative planning. However, larger Cobb angle meant more complex structures of deformed spine and more vertebrae rotation in the transverse plane, which might be important contributors to the different results in patients whose major Cobb angle was >50°. In our opinion, using 3D prototyping technology and doing simulative surgery before the scoliosis surgery to learn the accurate information about the deformed surgery could significantly decrease the rate of screw misplacement in patients whose major Cobb angle was >50°.
Major and secondary Cobb angle, coronal balance, SVA, and thoracic kyphosis improved significantly after the corrective surgeries, and no significant difference was observed in lumbar lordosis. Besides, there were no differences in these postoperative valuables between 2 groups (all, P > 0.05). This lack of difference might be attributed to the right selection of LIV and upper-instrumented vertebra and the surgeons performing the procedures. The surgeons were all experienced, senior surgeons who made accurate surgery planning and could choose the right vertebrae to implant the pedicle screws. Future studies with larger sample sizes and long follow-up times should be completed to further test the efficacy of this novel technology.
In spite of the positive results observed in our study, there are some limitations of this study that should be addressed. First, all the patients we recruited in our study were Lenke 1 AIS patients; therefore, the results concluded in our study might not represent the whole AIS patients, including Lenke 2, 3, 4, and 5 AIS patients. Second, the follow-up time in our study was relatively short, and long-term clinical and radiological outcomes should be performed. Besides, our study was a single-center study, and there were also some selection and publication bias in our research. Therefore, large-scaled and multicenter studies should be performed to evaluate the long-term effectiveness of 3DRP technology in corrective surgery for AIS patients.
CONCLUSION
Using the 3D printing technology before posterior corrective surgery might reduce the operation time, perioperative blood loss, and transfusion volume. There did not appear to be a benefit to using this technology with respect to complication rate and postoperative radiological outcomes; however, 3D technology could reduce the misplacement rate in patients whose preoperative mean Cobb angle was > 50°. Besides, it also increased the patients’ hospital cost.
Footnotes
Abbreviations: 3D = 3-dimensional, 3DRP = 3D rapid prototyping, ACP = anterior cortical perforation, AIS = adolescent idiopathic scoliosis, CT = computed tomography, EPP = endplate perforation, FP = foraminal perforation, Hb = hemoglobin, LCP = lateral cortical perforation, LIV = lowest instrumented vertebra, MCP = medial cortical perforation, STL = stereolithographic, SVA = sagittal vertical axis.
MY, CL, and YL contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Basques BA, Bohl DD, Golinvaux NS, et al. Patient factors are associated with poor short-term outcomes after posterior fusion for adolescent idiopathic scoliosis. Clin Orthop Relat Res 2015; 473:286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu T, Hai Y. Sagittal plane analysis of selective posterior thoracic spinal fusion in adolescent idiopathic scoliosis: a comparison study of all pedicle screw and hybrid instrumentation. J Spinal Disord Tech 2014; 27:277–282. [DOI] [PubMed] [Google Scholar]
- 3.Upendra BN, Meena D, Chowdhury B, et al. Outcome-based classification for assessment of thoracic pedicular screw placement. Spine 2008; 33:384–390. [DOI] [PubMed] [Google Scholar]
- 4.Di Silvestre M, Parisini P, Lolli F, et al. Complications of thoracic pedicle screws in scoliosis treatment. Spine 2007; 32:1655–1661. [DOI] [PubMed] [Google Scholar]
- 5.Abul-Kasim K, Ohlin A. The rate of screw misplacement in segmental pedicle screw fixation in adolescent idiopathic scoliosis. Acta Orthop 2011; 82:50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGurk M, Amis AA, Potamianos P, et al. Rapid prototyping techniques for anatomical modelling in medicine. Ann R Coll Surg Engl 1997; 79:169–174. [PMC free article] [PubMed] [Google Scholar]
- 7.Petzold R, Zeilhofer HF, Kalender WA. Rapid protyping technology in medicine—basics and applications. Comput Med Imag Graph 1999; 23:277–284. [DOI] [PubMed] [Google Scholar]
- 8.Hurson C, Tansey A, O’Donnchadha B, et al. Rapid prototyping in the assessment, classification and preoperative planning of acetabular fractures. Injury 2007; 38:1158–1162. [DOI] [PubMed] [Google Scholar]
- 9.Bustamante S, Bose S, Bishop P, et al. Novel application of rapid prototyping for simulation of bronchoscopic anatomy. J Cardiothorac Vasc Anesth 2014; 28:1134–1137. [DOI] [PubMed] [Google Scholar]
- 10.Gear JI, Long C, Rushforth D, et al. Development of patient-specific molecular imaging phantoms using a 3D printer. Medical physics 2014; 41:082502. [DOI] [PubMed] [Google Scholar]
- 11.Dankowski R, Baszko A, Sutherland M, et al. 3D heart model printing for preparation of percutaneous structural interventions: description of the technology and case report. Kardiol Pol 2014; 72:546–551. [DOI] [PubMed] [Google Scholar]
- 12.Mao K, Wang Y, Xiao S, et al. Clinical application of computer-designed polystyrene models in complex severe spinal deformities: a pilot study. Eur Spine J 2010; 19:797–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abul-Kasim K, Strombeck A, Ohlin A, et al. Reliability of low-radiation dose CT in the assessment of screw placement after posterior scoliosis surgery, evaluated with a new grading system. Spine 2009; 34:941–948. [DOI] [PubMed] [Google Scholar]
- 14.Abul-Kasim K, Ohlin A, Strombeck A, et al. Radiological and clinical outcome of screw placement in adolescent idiopathic scoliosis: evaluation with low-dose computed tomography. Eur Spine J 2010; 19:96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hedequist DJ, Emans JB. The correlation of preoperative three-dimensional computed tomography reconstructions with operative findings in congenital scoliosis. Spine 2003; 28:2531–2534. [DOI] [PubMed] [Google Scholar]
- 16.Sakai Y, Matsuyama Y, Nakamura H, et al. Segmental pedicle screwing for idiopathic scoliosis using computer-assisted surgery. J Spinal Disord Tech 2008; 21:181–186. [DOI] [PubMed] [Google Scholar]
- 17.Lu S, Zhang YZ, Wang Z, et al. Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Med Biol Eng Comput 2012; 50:751–758. [DOI] [PubMed] [Google Scholar]
- 18.Wu ZX, Huang LY, Sang HX, et al. Accuracy and safety assessment of pedicle screw placement using the rapid prototyping technique in severe congenital scoliosis. J Spinal Disord Tech 2011; 24:444–450. [DOI] [PubMed] [Google Scholar]
- 19.Abul-Kasim K, Ohlin A. Evaluation of implant loosening following segmental pedicle screw fixation in adolescent idiopathic scoliosis: a 2 year follow-up with low-dose CT. Scoliosis 2014; 9:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ohtori S, Inoue G, Orita S, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine 2013; 38:E487–E492. [DOI] [PubMed] [Google Scholar]
- 21.Wu ZX, Gong FT, Liu L, et al. A comparative study on screw loosening in osteoporotic lumbar spine fusion between expandable and conventional pedicle screws. Arch Orthop Trauma Surg 2012; 132:471–476. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y, Hansen ES, Hoy K, et al. Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison. Spine 2011; 36:1113–1122. [DOI] [PubMed] [Google Scholar]
- 23.Cho RH, Yaszay B, Bartley CE, et al. Which Lenke 1A curves are at the greatest risk for adding-on... and why? Spine 2012; 37:1384–1390. [DOI] [PubMed] [Google Scholar]
- 24.Dede O, Ward WT, Bosch PP, et al. Using the free hand pedicle screw placement technique in adolescent idiopathic scoliosis surgery: what is the incidence of neurologic symptoms secondary to misplaced screws? Spine 2013. [DOI] [PubMed] [Google Scholar]
- 25.Lehman RA, Jr, Lenke LG, Keeler KA, et al. Computed tomography evaluation of pedicle screws placed in the pediatric deformed spine over an 8-year period. Spine 2007; 32:2679–2684. [DOI] [PubMed] [Google Scholar]


